Abstract
Spontaneous pneumomediastinum is a benign, self‐limited condition that mainly affects young people. In this report, we present four cases of this uncommon condition and a review of the current literature. Two cases had no prior significant medical history: one had a history of asthma and the other underwent regular outpatient treatment for anorexia nervosa. The three patients who were not anorexic spontaneously improved within a few days. However, the patient with anorexia nervosa took 2 months to recover. It appears that spontaneous pneumomediastinum is an intractable complication of anorexia nervosa, and the improvement of nutritional status in the patient is essential to manage this condition.
Keywords: anorexia nervosa, asthma, spontaneous pneumomediastinum, young woman
1. Introduction
Spontaneous pneumomediastinum is the presence of air in the mediastinum in the absence of trauma, and it is generally benign and self‐limited.1, 2 This rare condition mainly affects young people and usually spontaneously resolves within a few days.3, 4 We present four cases of spontaneous pneumomediastinum, including a review of the current literature.
2. Case Presentation
2.1. Case 1
A 14‐year‐old girl was evaluated for sore throat and headache in the emergency room. These symptoms had appeared while she was playing basketball in her junior high school in the morning, and dyspnea and numbness of the finger tips developed in the evening. She had no prior significant medical history. On physical examination, her vital signs were stable, and she looked thin; however, her body mass index (BMI) was not recorded. Physical findings were normal. Although we found no abnormalities on chest x‐ray, chest computed tomography (CT) clearly revealed pneumomediastinum. She became asymptomatic after conservative treatment, 6 days later.
2.2. Case 2
A 15‐year‐old girl was evaluated for a 1 day history of chest pain, sore throat, and dyspnea, which occurred abruptly while she was attending class at her high school. On physical examination, her vital signs were stable, and her BMI was 18.3 kg/m2. Physical findings were normal. Her chest x‐ray showed pneumomediastinum, and chest CT revealed pneumomediastinum and subcutaneous emphysema. After conservative treatment, repeat x‐ray showed almost complete recovery of the pneumomediastinum 4 days later.
2.3. Case 3
A 22‐year‐old woman was evaluated for a 3 day history of chest pain, which had abruptly started when she strongly coughed while working in her office. She had a medical history of asthma and had experienced an asthma exacerbation episode 4 days ago. On physical examination, her vital signs were stable, and her BMI was 22.7 kg/m2. Auscultation revealed wheezing, and there was crepitus in her neck. Chest x‐ray showed only subcutaneous emphysema, but chest CT revealed subcutaneous emphysema and pneumomediastinum. After conservative treatment, repeat CT showed complete recovery of the pneumomediastinum 5 days later.
2.4. Case 4
A 16‐year‐old girl was evaluated for chest pain that had continued for 14 days. She had been hospitalized in a psychiatric ward for the treatment of anorexia nervosa and was discharged 20 days prior to her visit to our outpatient clinic. She had experienced additional weight loss after her hospital discharge. She had no laxative addiction or habitual self‐induced vomiting. On physical examination, her vital signs were stable, and her BMI was 14.0 kg/m2. There was crepitus in her neck. Chest x‐ray and chest CT revealed pneumomediastinum and subcutaneous emphysema (Figure 1). She was readmitted to the psychiatric ward of the hospital. Initially, her oral caloric intake (<500 kcal/d) was insufficient. Chest CT after 1 week revealed worsened pneumomediastinum and subcutaneous emphysema. At 1 month after admission, her oral intake was supplemented with a high‐calorie intravenous infusion, providing a total intake of 1000 kcal/d from oral and intravenous sources. The pneumomediastinum and subcutaneous emphysema got better as her nutritional state improved. Repeat CT at 2 months showed almost complete recovery of the pneumomediastinum.
Figure 1.
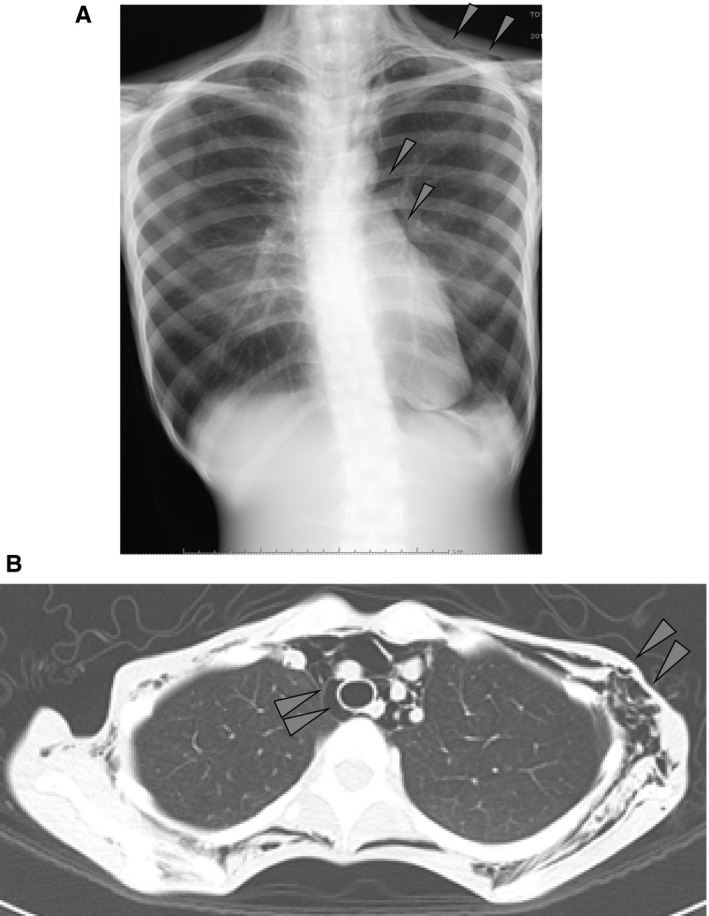
(A) Chest x‐ray film in posteroanterior projection showing pneumomediastinum and subcutaneous emphysema. (B) Chest CT scan showing pneumomediastinum and subcutaneous emphysema
3. Discussion
Spontaneous pneumomediastinum occurs mainly in lean, young men. The main symptoms include chest pain, cervical pain, dyspnea, and dysphagia. It usually resolves spontaneously within a few days.3, 4
The characteristics of our four patients are summarized in Table 1. They had some common characteristics: they were all young, thin females, in contrast to the male predominance reported in the literature.
Table 1.
Characteristics of cases
| Case | Sex | Age (y) | BMI | Trigger for pneumomediastinum | Medical history | Time for recovery |
|---|---|---|---|---|---|---|
| 1 | Female | 14 | ‐ | Exercise (basketball) | None | 6 d |
| 2 | Female | 15 | 18.3 | None | None | 4 d |
| 3 | Female | 22 | 22.7 | Asthma exacerbation | Asthma | 5 d |
| 4 | Female | 16 | 14.0 | None | Anorexia nervosa | 2 mo |
BMI, body mass index.
The notable difference is their hospitalization period. Three of the four cases recovered within a few days of conservative treatment. In contrast, case 4 with anorexia nervosa took 2 months to be cured. There are several reports on anorexia nervosa with spontaneous pneumomediastinum, and they showed a similar tendency.5, 6 According to these reports, anorexia patients needed 7‐27 days to recover, significantly longer than that needed for nonanorexic patients.7, 8
Although the details are unknown, the fragility of the alveolar tissue due to malnutrition can be the clue to understand the refractory nature.9, 10 Massaro et al. revealed that calorie restriction leads to loss of alveoli, fall in gas exchange tissue, and thinner alveolar walls in animal experiments.11 Winick also reported that atrophic tissue, including alveoli walls, was found in the victims of the Jewish Ghetto who were suffering from chronic starvation.12 Therefore, it is necessary to provide not only rest and supportive care alone but also treatment for the malnutrition due to anorexia nervosa to cure the pneumomediastinum in these patients. In case 4, the patient needed prolonged hospitalization, longer than previous records, probably because a severe malnourished condition had persisted for a long time. Her mediastinal emphysema improved as her nutritional condition was sufficiently improved.
Plain CT is superior to make a definitive diagnosis. One of the four cases (Case 1) showed no findings of spontaneous pneumomediastinum on chest x‐ray; the diagnosis was made using chest CT. Kaneki et al. reported that 30% cases of spontaneous pneumomediastinum were missed on chest x‐ray and were diagnosed only using chest CT.13 CT should therefore be considered to rule out the condition, even if there is no apparent abnormality on chest x‐ray.
4. Conclusion
Although the prognosis of spontaneous pneumomediastinum was favorable, it is an intractable complication of anorexia. Improvement of nutritional status is essential to manage this condition in anorexic patients.
Conflict of Interest
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Kuroiwa M, Kita K, Wakakuri A, et al. Spontaneous pneumomediastinum in young women: Comparison between anorexia nervosa and nonanorexic patients. J Gen Fam Med. 2017;18:268–270. https://doi.org/10.1002/jgf2.43
Reference
- 1. Versteegh FGA, Broeders IAJM. Spontaneous pneumomediastinum in children. Eur J Pediatr. 1991;131:304–7. [DOI] [PubMed] [Google Scholar]
- 2. Hamman L. Spontaneous mediastinal emphysema. Bull J Hopkins Hosp. 1939;64:1–21. [Google Scholar]
- 3. Yellin A, Gapany‐Gapanavicius M, Lieberman Y. Spontaneous pneumomediastinum: is it a rare cause of chest pain? Thorax. 1983;38:383–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dekel B, Paret G, Szeinberg A, et al. Spontaneous pneumomediastinum in children: clinical and natural history. Eur J Pediatr. 1996;155:695–7. [DOI] [PubMed] [Google Scholar]
- 5. Veelen IV, Hogeman PHG, Elburg AV, et al. Pneumomediastinum: a rare complication of anorexia nervosa in children and adolescents. A case study and review of the literature. Eur J Pediatr. 2008;167:171–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lee KJ, Yum HK, Park IN. Spontaneous pneumomediastinum: an unusual pulmonary complication in anorexia nervosa. Tuberc Respir Dis. 2015;78:360–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Danzer G, Mulzer J, Weber G, et al. Advanced anorexia nervosa, associated with pneumomediastinum, pneumothorax, and soft‐tissue emphysema without esophageal lesion. Int J Eat Disord. 2005;38:281–4. [DOI] [PubMed] [Google Scholar]
- 8. Cho H, Hasegawa S, Omasa M, et al. A case of spontaneous mediastinal, pericardial, and retroperitoneal emphysema associated with anorexia nervosa. J Japan Soc Bronchol. 2002;24:332–5. [Google Scholar]
- 9. Overby KJ, Litt IF. Mediastinal emphysema in an adolescent with anorexia nervosa and self‐induced emesis. Pediatrics. 1988;81:134–6. [PubMed] [Google Scholar]
- 10. Isizawa T, Sakamoto N, Yoshiuchi K, et al. A case of anorexia nervosa with subcutaneous emphysema and pneumomediastinum. Psychosom Med. 2004;8:358–62. [Google Scholar]
- 11. Massaro D, Massaro GD, Baras A, et al. Calorie‐related rapid onset of alveolar loss, regeneration, and changes in mouse lung gene expression. Am J Physiol Lung Cell Mol Physiol. 2004;286:896–906. [DOI] [PubMed] [Google Scholar]
- 12. Winick M. Hunger disease: studies by the Jewish physicians in the Warsaw Ghetto. New York: Wiley; 1979; p. 221–3. [Google Scholar]
- 13. Kaneki T, Kubo K, Kawashima A, et al. Spontaneous pneumomediastinum in 33 patients: yield of chest computed tomography for the diagnosis of the mild type. Respiration. 2000;67:408–11. [DOI] [PubMed] [Google Scholar]


