Abstract
Purpose of review
We summarized recent literature on the epidemiology and treatment of eating disorders in middle-aged and older women and men.
Recent findings
The prevalence of eating disorders according to DSM-5 criteria is around 3.5% in older (>40 years) women and around 1–2% in older men. The majority of those eating disordered persons are not in treatment. There are new terms like ‘perimenopausal eating disorders’ and ‘muscularity-oriented eating disorders’ indicating the impact of the aging process and sex-specific differences.
Summary
Disordered eating and eating disorders occur in both women and men of all ages. Medical complications because of age, the stigma of eating disorders in a still ‘untypical’ age, and the glorification of sports activity often hinder the recognition of eating disorders in midlife and older persons. Treatment approaches should consider treatment strategies tailored for older women and men, addressing the context of midlife and aging.
Keywords: eating disorders, epidemiology, midlife, older men, older women, prevalence, treatment
INTRODUCTION
Based on a small but growing literature, it has become evident that eating disorders and related body image concerns not only occur in young women (below 35 years), but also in women of middle and older age [1–4,5▪▪]. In a previous issue of this journal, we have reviewed the literature on pathological eating and body dissatisfaction in middle-aged and older women till 2014 [6]. Findings on pathological eating in older women also initiated research in older men within the last years. We searched for articles using PubMed, Ovid MEDLINE(R), EMBASE, and PsycINFO, based on terms ‘eating disorders,’ ‘eating behavior,’ disordered eating,’ ‘body image,’ ‘body shape,’ ‘body dissatisfaction,’ ‘midlife,’ ‘middle age’, ‘elderly’, ‘older age’, ‘women,’ ‘men’, ‘females,’ and ‘males’ to review the recent literature on disordered eating and eating disorders and associated features in middle-aged and older women and men between 2015 and May 2017.
Box 1.
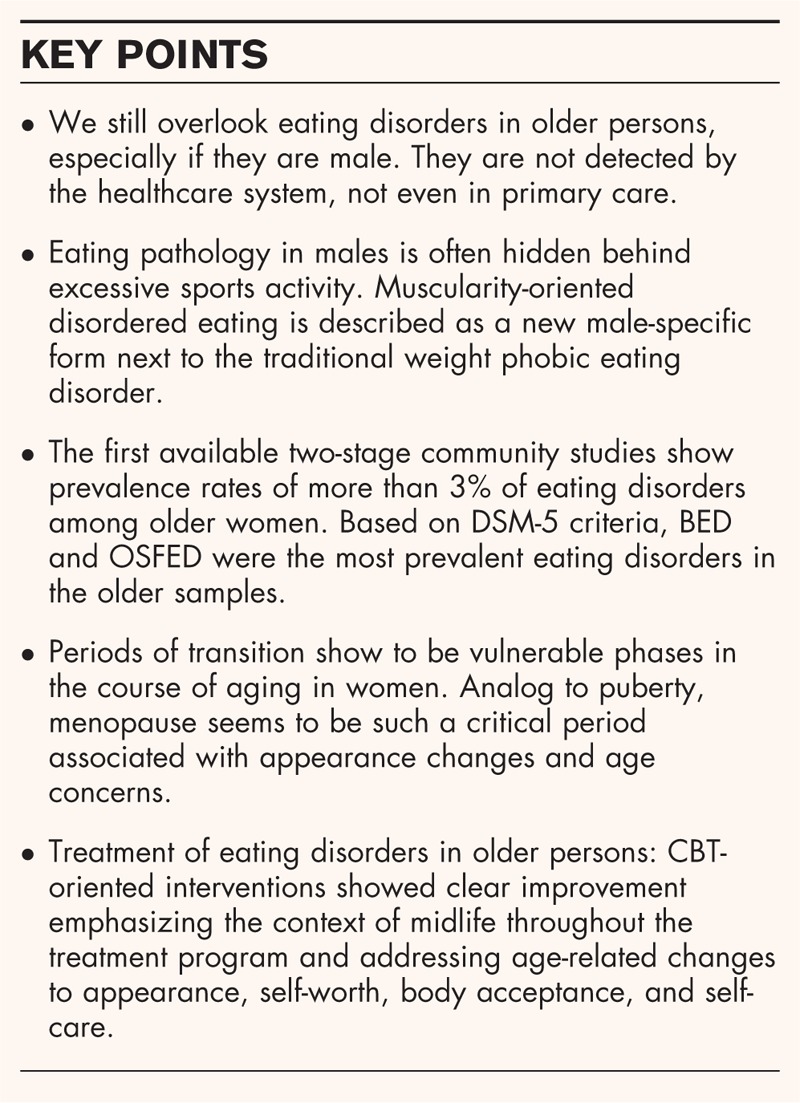
no caption available
DIAGNOSES AND ASSESSMENT
In our previous review (2014) on middle-aged and older women, the included studies were often based on broader and subthreshold criteria of disordered eating [6]. Recent studies, however, show evolvement of methodological approaches [7,8▪] using formal criteria such as DSM-5 [9] or ICD-10 [10]. In addition, there are studies that use subthreshold and simpler criteria of disordered eating, such as single core symptoms of eating disorders like low BMI, binge eating only, binge eating and purging or purging only [11,12]. Other studies have selected cases based on various standardized questionnaires or subscales to assess eating disorder [13,14] or various aspects of disordered eating [15,16]. Data on eating disorders in midlife and older persons are mostly derived from community samples or case reports rather than large clinical samples because people of concern are less often patients (both in and outpatients) who seek treatment. This is especially true for men. ‘Men aged midlife and beyond might be the most stigmatized group to suffer from an eating disorder’ [17▪▪]. Studies on eating disorders in men in general are rare [18] and still biased because of the fact of predominantly female-oriented instruments to assess eating behavior [19,20]. Research in middle-aged and older men is very limited and most studies are based on single case reports [17▪▪]. To our knowledge, there exists only one community study on disordered eating in older males [21].
EPIDEMIOLOGY
Incidence and prevalence are the two principal measures of the distribution of a disorder [22,23]. In epidemiological research on eating disorders, prevalence studies vastly outnumber incidence studies. Prevalence studies of eating disorders are often conducted in high-risk populations such as schoolgirls or female college students, but recently some community studies on middle-aged and older persons have been conducted.
For prevalence studies, the method of preference has a two-stage design. In a two-stage design, the first stage involves screening a large number of individuals for suspected cases by means of an easily administered questionnaire [22]. The second stage involves (semi-structured) interviews with the screen-positive persons who are likely to have an eating disorder. Usually, a number of randomly selected screen-negative persons are also interviewed to confirm that they are not cases and thereby to validate the cutoff of the screening questionnaire. Two-stage surveys using strict diagnostic criteria reveal much lower prevalence rates than the early surveys conducted in the past century that relied exclusively on questionnaires.
WOMEN
Incidence rates
Incidence studies on eating disorders among young females have often been based on detected cases in hospital records and case registers of in and outpatients in mental healthcare facilities [23]. Incidence studies of eating disorders among older persons hardly exist. Smink et al.[7] studied incident cases with anorexia nervosa and bulimia nervosa according to DSM criteria detected in primary care in a large representative sample of 1% of the Dutch population during the 1980s, 1990s, and 2000s [7]. Combining the results of these three periods we find a low incidence rate for anorexia nervosa of 4.0 [95% confidence interval (CI): 2.4–6.5] per 100 000 females aged 35–64 years compared with an incidence rate of 85.1 (95% CI: 65.2–109.1) in the high-risk group for anorexia nervosa of females aged 15–19 years. For bulimia nervosa the yearly incidence rate is 5.9 (95% CI: 3.8–8.8) per 100 000 females aged 35–64 years compared with an incidence rate of 35.0 (95% CI: 27.9–43.3) in the high-risk group for bulimia nervosa of females aged 15–29 years. However, only a small proportion of cases of eating disorders in the community is detected by general practitioners [22,23] and this is likely to be even more true for eating disorders among older persons. Therefore, to understand more on the occurrence of eating disorders among older persons we have to rely on prevalence studies in the community.
Prevalence rates
In their reviews of eating disorder studies on older women both Mangweth-Matzek et al.[6] in 2014 and Podfigurna-Stopa et al.[24] in 2015 found very few prevalence studies, and the resulting prevalence rates were only based on questionnaires. However, two recent studies on eating disorders among older persons used more sophisticated designs with a two-stage detection strategy.
Conceição et al.[8▪] recently examined the point prevalence of eating disorders in 342 women on the Azores (Portugal) aged 65–94 years using a two-stage approach. In stage 1, women were screened for various symptoms of disordered eating and in stage 2, 118 women were interviewed using the eating disorder examination [25]. The authors found 12 eating disorder cases, corresponding to a prevalence rate of 3.5% (95% CI: 2.0–6.1%), which was comparable with that in young Portuguese women [26], however, in a different diagnostic distribution. Based on DSM-5 criteria, binge eating disorder (BED) was the most prevalent eating disorder in the described elderly women (1.7%), followed by other specified feeding and eating disorders (OSFED; 1.5%), and bulimia nervosa (0.3%); no cases of anorexia nervosa or night eating syndrome were identified. Binge eating episodes (without fulfilling the criteria for BED) were reported by 5.6% of women. The strengths of this study are the examination of an older sample, the two-stage design, and the use of face-to-face interviews.
In another recently published two-stage study, Micali et al.[5▪▪] reported the lifetime and 12-month prevalence of eating disorders in a large sample of 5658 midlife women from the United Kingdom. Women who screened positive in phase one were selected for interviews in phase two using the Structured Clinical Interview for DSM Disorders (SCID-1) based on DSM-5, supplemented with behavioral data. With regard to the 12-month prevalence, 3.6% (95% CI: 3.0–4.4%) of the 40–50-year-old women were identified with eating disorders, displaying OSFED as the most prevalent one (1.7%), followed by BED (1.0%), bulimia nervosa (0.4%), and anorexia nervosa (0.2%). These women reported an overall lifetime prevalence of eating disorders of 15.3% (95% CI: 13.5–17.4%) showing OSFED as the most prevalent diagnosis (7.6%), followed by anorexia nervosa (3.6%), bulimia nervosa (2.2%), and BED (2.0%). The study by Micali et al.[5▪▪] was nested in a longitudinal study of a large community-based sample of women in the United Kingdom in which they also studied risk factors. Childhood sexual abuse was associated with all disorders with binge eating behaviors (anorexia nervosa binge-purge, bulimia nervosa, BED, and subthreshold bulimia nervosa and BED) among midlife women. This is in line with the results of a recent meta-analysis that showed that childhood maltreatment, regardless of type, is associated with the presence of all types of eating disorders, and with severity parameters that characterize these illnesses in a dose-dependent manner [27].
Baker & Runfola [28▪▪] introduced a new term ‘perimenopausal eating disorder’ indicating the affliction of eating disorders and critical hormonal changes in women. The authors strongly believe in an endocrinological cause of eating disorders and encourage further research in this field that was first described by Mangweth-Matzek et al.[29], showing significantly higher eating disorder prevalence rates in perimenopausal women as compared with pre- and postmenopausal women. Baker et al.[30▪] examined the association between bulimic symptoms and hormone concentrations (reproductive/appetite) in premenopausal versus perimenopausal women. They found a positive association between leptin and binge eating, but none with regard to reproductive hormones [30▪].
Treatment
So far there are almost no publications on treatment studies focusing on middle-aged or older patients with eating disorders. Micali et al.[5▪▪] reported in their two-phase prevalence study that only a 27.4% minority of midlife women who met criteria for DSM-5 eating disorders received treatment or sought help at any time in life. The general practitioner was the most common healthcare provider (8.2%) and 1.2% of the women reported having received inpatient treatment. Podfigurna-Stopa et al.[24] pointed out that in all eating disorders the interference with medical complications because of age were the most challenging part of treatment (e.g., osteoporosis). A study by Gaudiani et al.[31▪] was the first to compare age groups on the acuity of clinical characteristics and on medical outcomes of short inpatient refeeding treatment in patients with severe anorexia nervosa. Among the 142 patients examined (mostly female), in the age range of 17–65 years, 46% were 30 years or older (25% above 40 years). Those patients above 30 years did not differ from the younger ones with regard to the degree of profound underweight and prevalence of medical complications. Their progression through medical stabilization worked as well as in younger patients (achievement of BMI of 14).
The focus of a review by Lewis-Smith et al.[32▪▪] was to identify interventions for women in midlife that aim to improve body image and disordered eating. Three effective interventions were found, two were based on CBT and one pilot study used acceptance and commitment therapy. In the study by McLean et al.[33] a cognitive behavioral therapy (CBT)-based intervention for body image and disordered eating showed clear improvements in women of midlife; they emphasized the context of midlife throughout the treatment program and addressed age-related changes to appearance, self-worth, body acceptance, and self-care.
Ariel and Perri [34] examined the effect of dose of behavioral treatment for obesity on binge eating severity in 572 adults (79% females) with a mean age of 53 years. Study participants showed best effects in reduction of binge eating severity at 6 months after moderate and high-dose behavioral treatment (16 or 24 weekly sessions) as compared to low dose or nutritional control group (both 8 weekly sessions). Improvement of binge eating severity was correlated with dietary self-monitoring and weight loss.
There are no data with regard to long-term recovery rates in middle and older patients with eating disorders.
MEN
Prevalence rates
Raevuori et al.[18] summarized data on eating disorder in males in their 2014 review, including lifetime prevalence rates of anorexia nervosa = 0.2–0.3%, of bulimia nervosa = 0.1–0.5%, and of BED = 1.1–3.1% and characteristics in core symptoms that did not differ from women. However, data were based predominately on younger men.
The review of Reas and Stedal [17▪▪] published in 2015 recapped data on eating disorders of men aged more than 40 years based on very few studies. Lifetime prevalence rates based on supplemental data from the US National Comorbidity survey were 0.0, 1.3, and 2.7% for anorexia nervosa, bulimia nervosa, and BED, respectively in 45–59-year-old men, and for men aged at least 60 years they were less than 1% in all three diagnostic groups (0.3, 0.3, and 0.9%, respectively). The 12-month prevalence rate for eating disorders in midlife for older males was estimated between 0.2 and 1.6%. Overall, they described an increase over time both in binge eating behavior and in purging behavior in men aged 45 years or older.
So far no community studies have been reported on middle-aged and older men using two-stage methodological approaches including ICD or DSM criteria.
Mangweth-Matzek et al.[21] surveyed 470 men of Innsbruck (Austria) aged 40–75 years, mostly randomly selected from Census Bureau data using an anonymous questionnaire on eating disorder symptoms (based on either BMI <18.5, binge eating only, binge eating and purging or purging only), the eating disorder examination questionnaire [35], body image, and exercise activity including exercise addiction [36,37]. In total, 6.8% of the men met criteria of disordered eating and also showed a significantly higher eating disorder examination questionnaire score as compared with normal eating men. In the context of binge eating excessive exercise was the most frequently used inappropriate compensatory behavior. Furthermore, the eating disordered men displayed significantly more exercise addiction behavior than the control group based on the Exercise Addiction Inventory [37]. The authors concluded that evolvement of sportive behavior most often hinders recognition of disorder. Thus further research is needed.
Disordered eating was also assessed in a sample of older veterans (N = 642 males, N = 55 females, aged on average 62.99, SD ± 12.03) who were selected based on reported trauma exposure from an earlier study [13]. Of the male veterans 0.1% displayed anorexia nervosa, 2.8% bulimia nervosa, 2.5% BED based on DSM-5 criteria. Posttraumatic Stress Disorder was significantly associated with disordered eating in males using the Eating Disorder Diagnostic Scale [38] and with food addiction. Eating disorder symptoms were discussed as mediating factors for coping with negative effects and emotion regulations.
Dieting and body image concerns
Slof-Op‘t Landt et al.[16] examined the prevalence of dieting and fear of weight gain across ages in 31 636 participants (age 13–98 years; 39.8% men) of the Netherlands Twin Register. They found that the majority of men in the Netherlands did not diet: men aged 45–65 years reported the highest rates of dieting (32%). The rates for men were lower than those for women: 35–65 year old women reported the highest (57–63%) rates of dieting. Fear of weight gain was described by 25–46% of the men and by 39–44% of the women in the various age groups [16].
Drive for muscularity and muscle dysmorphia were studied as essential aspects of eating disorders in an Australian sample of men aged 19–84 years [39▪▪]. The authors found that there are three types of men: those with high muscularity concern, high shape and weight concerns, and high dieting and exercise dependence; those with moderate shape and weight concerns, moderate muscularity concerns, and high dieting; and those with low to moderate scores across all measures. Risk for eating disorders was high in the first two groups. ‘Fat-Talk’ as an aspect closely related to body dissatisfaction was found also in men (N = 819) across the whole lifespan [15] unlike women who showed this association primarily in younger ages. Fat-talk was closely related to disordered eating both in women and men.
Cottrell and Williams [40] in their recent review on the importance of recognition of eating disorders in men focused in primary care providers when evaluating their complaints. Body image issues, especially drive for muscularity expressed by exercise routines have to be included in medical assessment.
‘Men, muscles, and eating disorders’ is the content of another recent review on males by Lavender et al.[41▪]. They introduced a new term: ‘muscularity-oriented disordered eating’ based on a body image that differs from the traditional, female weight phobic attitudes by a dual focus of leanness (low body fat) and muscularity. The authors describe various disorders as to body image, eating behavior, and drug use to reach the body ideal. With regard to eating disorder, terms like ‘bulk and cut dietary practices’ [41▪] are used explaining ‘periodic oscillation in dietary practices’ [41▪], resulting in overregulation of protein consumption aiming increase of muscularity, versus restriction of dietary energy aiming reduction in body fat.
Treatment studies in older males are limited to case reports as shown in the review of Reas and Stedal [17▪▪]. Like in older women, health issues because of age often hinder the recognition of eating disorder. Data on onset and course are therefore not available.
CONCLUSION
Based on current research eating disorders do occur above 40 years of age both in women and men. Recent two-stage epidemiological studies show that the overall prevalence of eating disorders according to DSM-5 criteria is around 3–4% among women and 1–2% in males of middle and older age. Although the occurrence of eating disorders (especially of anorexia nervosa) is lower among older women than among the highest-risk group of young females, healthcare providers should consider the possibility of an eating disorder also among older people. This is challenging because of age-dependent symptomatology, the patients’ underreport of eating disorder symptomatology because of shame, the stigmatization of psychiatric disorders also from the doctor's side, and the fact that eating disorder is often hidden behind excessive sports activity.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Harris M, Cumella EJ. Eating disorders across the life span. J Psychosoc Nurs Ment Health Serv 2006; 44:20–26. [DOI] [PubMed] [Google Scholar]
- 2.Gadalla TM. Eating disorders and associated psychiatric comorbidity in elderly Canadian women. Arch Womens Ment Health 2008; 11:357–362. [DOI] [PubMed] [Google Scholar]
- 3.Mangweth-Matzek B, Rupp CI, Hausmann A, et al. Never too old for eating disorders or body dissatisfaction: a community study of elderly women. Int J Eat Disord 2006; 39:583–586. [DOI] [PubMed] [Google Scholar]
- 4.Lapid MI, Prom MC, Burton MC, et al. Eating disorders in the elderly. Int Psychogeriatr 2010; 22:523–536. [DOI] [PubMed] [Google Scholar]
- 5▪▪.Micali N, Martini MG, Thomas JJ, et al. Lifetime and 12-month prevalence of eating disorders amongst women in mid-life: a population-based study of diagnoses and risk factors. BMC Med 2017; 15:12. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study examined the lifetime and 12-month prevalence of eating disorders in a large sample of 5658 midlife women from the United Kingdom based on a two-stage methodological approach. The authors found a 12-month prevalence rate of eating disorders of 3.6% (3.0–4.4%, 95% CI) in the 40–50-year-old women, displaying OSFED as the most prevalent one (1.7%). These women reported an overall lifetime prevalence of eating disorders of 15.3% (13.5–17.4%, 95% CI).
- 6.Mangweth-Matzek B, Hoek HW, Pope HG., Jr Pathological eating and body dissatisfaction in middle-aged and older women. Curr Opin Psychiatry 2014; 27:431–435. [DOI] [PubMed] [Google Scholar]
- 7.Smink FR, van Hoeken D, Donker GA, et al. Three decades of eating disorders in Dutch primary care: decreasing incidence of bulimia nervosa but not of anorexia nervosa. Psychol Med 2016; 46:1189–1196. [DOI] [PubMed] [Google Scholar]
- 8▪.Conceição EM, Gomes FV, Vaz AR, et al. Prevalence of eating disorders and picking/nibbling in elderly women. Int J Eat Disord 2017; 50:793–800. [DOI] [PubMed] [Google Scholar]; In this study, the point prevalence of eating disorders in 342 women on the Azores (Portugal) aged 65–94 years was examined based on a two-stage approach using a questionnaire for various symptoms of disordered eating in stage 1, and the eating disorder examination interview in stage 2. The authors found an eating disorder prevalence rate of 3.5% (2.0–6.1, 95% CI) which was comparable with that in young Portuguese women, however, in a different diagnostic distribution.
- 9.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed.Arlington: American Psychiatric Association; 2013. [Google Scholar]
- 10.World Health Organization. The ICD-10 classification of mental and behavioral disorders. Genova: World Health Organization; 1992. [Google Scholar]
- 11.Gagne DA, Von Holle A, Brownley KA, et al. Eating disorder symptoms and weight shape concerns in a large web-based convenience sample of women ages 50 and above: results of the gender and body image (GABI) study. Int J Eat Disord 2012; 45:832–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mangweth-Matzek B, Hoek HW, Rupp CI, et al. Prevalence of eating disorders in middle-aged women. Int J Eat Disord 2014; 47:320–324. [DOI] [PubMed] [Google Scholar]
- 13.Mitchell KS, Wolf EJ. PTSD, food addiction, and disordered eating in a sample of primarily older veterans: the mediating role of emotion regulation. Psychiatry Res 2016; 243:23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eik-Nes T, Romild U, Guzey I, et al. Women's weight and disordered eating in a large Norwegian community sample: the Nord-Trøndelag Health Study (HUNT). BMJ Open 2015; 5:e008125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tzoneva M, Forney KJ, Keel PK. The influence of gender and age on the association between ‘fat-talk’ and disordered eating: an examination in men and women from their 20s to their 50s. Eat Disord 2015; 23:439–454. [DOI] [PubMed] [Google Scholar]
- 16.Slof-Op ’t Landt MC, van Furth EF, van Beijsterveldt CE, et al. Prevalence of dieting and fear of weight gain across ages: a community sample from adolescents to the elderly. Int J Public Health 2017; doi: 10.1007/s00038-017-0948-7. [DOI] [PubMed] [Google Scholar]
- 17▪▪.Reas DL, Stedal K. Eating disorders in men aged midlife and beyond. Maturitas 2015; 81:248–255. [DOI] [PubMed] [Google Scholar]; The review was based on 16 case reports of eating disorders in males aged 40–81 years describing mostly an early onset, variable courses of illness, and diagnostic crossovers. Lifetime prevalence rates were reported ranging from 0% to 2.7%. The 12-month prevalence rate was estimated between 0.2 and 1.6%.
- 18.Raevuori A, Keski-Rahkonen A, Hoek HW. A review of eating disorders in males. Curr Opin Psychiatry 2014; 27:426–430. [DOI] [PubMed] [Google Scholar]
- 19.Darcy AM, Lin IH. Are we asking the right questions? A review of assessment of males with eating disorders. Eat Disord 2012; 20:418–426. [DOI] [PubMed] [Google Scholar]
- 20.Strother E, Lemberg R, Stanford SC, Turberville D. Eating disorders in men: underdiagnosed, undertreated and misunderstood. Eat Disord 2012; 20:346–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mangweth-Matzek B, Kummer KK, Pope HG. Eating disorder symptoms in middle-aged and older men. Int J Eat Disord 2016; 49:953–957. [DOI] [PubMed] [Google Scholar]
- 22.Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and other eating disorders. Curr Opin Psychiatry 2006; 19:389–394. [DOI] [PubMed] [Google Scholar]
- 23.Hoek HW. Brownell KD, Walsh B. Epidemiology of eating disorders. Eating disorders and obesity: a comprehensive handbook 3rd ed.New York: Guilford Press; 2017. 237–242. [Google Scholar]
- 24.Podfigurna-Stopa A, Czyzyk A, Katulski K, et al. Eating disorders in older women. Maturitas 2015; 82:146–152. [DOI] [PubMed] [Google Scholar]
- 25.Fairburn CG, Cooper Z, O’Connor M. Fairburn CG. Eating Disorder Examination (16. 0D). Guilford Press, Cognitive behavior therapy and eating disorders. New York:2008. [Google Scholar]
- 26.Machado PPP, Machado BC, Gonçalves S, Hoek HW. The prevalence of eating disorders not otherwise specified. Int J Eat Disord 2007; 40:212–217. [DOI] [PubMed] [Google Scholar]
- 27.Molendijk ML, Hoek HW, Brewerton TD, Elzinga BM. Childhood maltreatment and eating disorder pathology: a systematic review and dose-response meta-analysis. Psychol Med 2017; 19:1–15. [DOI] [PubMed] [Google Scholar]
- 28▪▪.Baker JH, Runfola CD. Eating disorders in midlife women: a perimenopausal eating disorder? Maturitas 2016; 85:112–116. [DOI] [PubMed] [Google Scholar]; In the review, a new term ‘perimenopausal eating disorder’ was introduced, indicating the affliction of eating disorders and critical hormonal changes in women. The authors believe in an endocrinological cause of eating disorders.
- 29.Mangweth-Matzek B, Hoek HW, Rupp CI, et al. The menopausal transition: a possible window of vulnerability for eating pathology. Int J Eat Disord 2013; 46:609–616. [DOI] [PubMed] [Google Scholar]
- 30▪.Baker JH, Peterson CM, Thornton LM, et al. Reproductive and appetite hormones and bulimic symptoms during midlife. Eur Eat Disord Rev 2017; 25:188–194. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study examined the association between bulimic symptoms and hormone concentrations (reproductive/appetite) in premenopausal versus perimenopausal women. No association was found between reproductive hormones and binge eating.
- 31▪.Gaudiani JL, Brinton JT, Sabel AL, et al. Medical outcomes for adults hospitalized with severe anorexia nervosa: an analysis by age group. Int J Eat Disord 2016; 49:378–385. [DOI] [PubMed] [Google Scholar]; In this study clinical characteristics and medical outcomes of short inpatient refeeding treatment in patients (aged range of 17–65 years) with severe anorexia nervosa were examined. In total, 46% of the 142 patients examined, were 30 years or older. Those patients above 30 years did not differ from the younger ones with regard to underweight and medical complications and positive treatment outcome.
- 32▪▪.Lewis-Smith H, Diedrichs PC, Rumsey N, Harcourt D. A systematic review of interventions on body image and disordered eating outcomes among women in midlife. Int J Eat Disord 2016; 49:5–18. [DOI] [PubMed] [Google Scholar]; The review examined research on interventions among midlife women on body image and disordered eating outcome. Three effective interventions were found, two were based on CBT and acceptance and commitment therapy.
- 33.McLean SA, Paxton SJ, Wertheim EH. A body image and disordered eating intervention for women in midlife: a randomized controlled trial. J Consult Clin Psychol 2011; 79:751–758. [DOI] [PubMed] [Google Scholar]
- 34.Ariel AH, Perri MG. Effect of dose of behavioral treatment for obesity on binge eating severity. Eat Behav 2016; 22:55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hilbert A, Tuschen-Caffier B. Eating Disorder Examination – Questionnaire. Deutschsprachige Übersetzung, 1. Auflage. Münster: Verlag für Psychotherapie, PAG Institut für Psychologie AG; 2006. http://www.vfp-muenster.de/publikationen/online/EDE-Q_VfP_2.pdf. [Google Scholar]
- 36.Ziemainz H, Stoll O, Drescher A, et al. Die Gefährdung zur Sportsucht in Ausdauersportarten. Dtsch Z Sportmed 2013; 64:57–64. [Google Scholar]
- 37.Terry A, Szabo A, Griffiths M. The exercise addiction inventory: a new brief screening tool. Addict Res Theory 2004; 12:489–499. [Google Scholar]
- 38.Stice E, Telch CF, Rizvi SL. Development and validation of the eating disorder diagnostic scale: a brief self-report measure of anorexia nervosa, bulimia, and binge eating disorder. Psychol Assess 2000; 12:123–131. [DOI] [PubMed] [Google Scholar]
- 39▪▪.Hughes EK, Dean C, Allen JS. Measures of eating disorder symptoms, drive for muscularity, and muscle dysmorphia: norms and typologies of Australian men. Aust J Psychol 2016; 68:270–280. [Google Scholar]; Drive for muscularity and muscle dysmorphia were studied as essential aspects of eating disorders in an Australian sample of men aged 19–84 years. The authors found three types of men differing on muscularity concern, shape and weight concern, and dieting behavior.
- 40.Cottrell DB, Williams J. Eating disorders in men. Nurse Pract 2016; 41:49–55. [DOI] [PubMed] [Google Scholar]
- 41▪.Lavender JM, Brown TA, Murray SB. Men, muscles, and eating disorders: an overview of traditional and muscularity-oriented disordered eating. Curr Psychiatry Rep 2017; 19:32. [DOI] [PMC free article] [PubMed] [Google Scholar]; The authors focus specifically on the male-specific characteristics of eating disorders. They introduced a new term ‘muscularity-oriented disordered eating’ based on a body image that differs from the traditional, female weight phobic attitudes by a dual focus of leanness (low body fat) and muscularity.


