Abstract
In situ ulnar nerve release has been gaining popularity as a simple, effective, and low-morbidity procedure for the treatment of cubital tunnel syndrome. One concern with the technique is how to manage the unstable ulnar nerve after release. It is unclear how much nerve subluxation will lead to problems and surprisingly there is no grading system to assess ulnar nerve instability. I propose such a grading system, as well as a new technique to stabilize the unstable ulnar nerve. The blocking flap technique consists of raising a rectangular flap off the flexor/pronator fascia and attaching it to the posterior subcutaneous flap so that it blocks the nerve from subluxation/dislocation.
Key Words: blocking flap, cubital tunnel syndrome, in situ release, ulnar nerve subluxation
Cubital tunnel syndrome (CubTS) is the second most common compressive neuropathy in the upper extremity after carpal tunnel syndrome (CTS).1–3 However, unlike CTS there are numerous surgical options to treat CubTS including simple in situ decompression, medial epicondylectomy, and various anterior transposition techniques (subcutaneous, intramuscular, submuscular).
In 1986, Amadio4 reviewed the 5 potential sites of ulnar nerve entrapment for CubTS: the Arcade of Struthers, medial intermuscular septum, medial epicondyle, cubital tunnel, and the flexor-pronator aponeurosis. Conventional wisdom followed that all 5 sites need to be addressed during routine cubital tunnel surgery to avoid inadequate release. It is valuable to note that Amadio found that the 2 most common sites of compression were at the medial epicondyle (13 cases) and the cubital tunnel (17 cases) during 41 submuscular transposition cases. Furthermore, a single compressive focus was identified in 19 patients, 2 foci in 7, and 3 foci in 2.
My experience is similar to Amadio’s, in that the majority of my patients with CubTS have had ulnar nerve pathology in the region of the medial epicondyle (retrocondylar groove) or just proximal or distal (cubital tunnel) to it. This would support in situ release as a viable option that decompresses the nerve at 1 region instead of 5. Multiple studies have also found in situ release to be as effective as other treatments.5–12
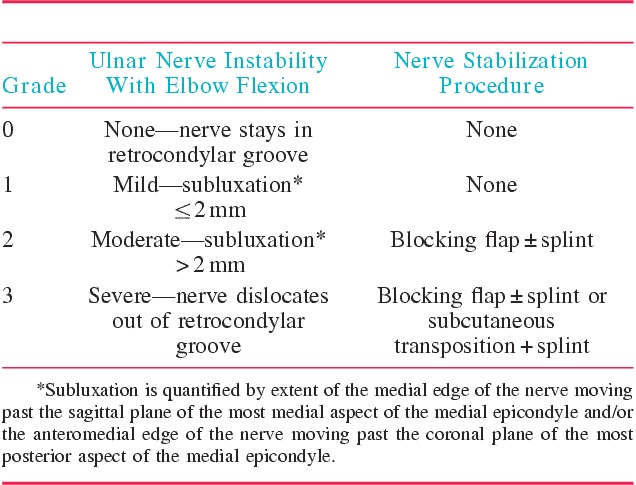
In situ decompression has been gaining in popularity.13 However, it is unclear how to manage the unstable ulnar nerve after in situ decompression. When the nerve is unstable, the literature recommends some form of transposition.14,15 Surprisingly, intraoperative ulnar nerve instability is not classified in the literature and it is unclear if mild to moderate-subluxation necessitates transposition. Motivated by a 3-fold goal of minimizing dissection of the nerve, avoiding anterior transposition, and preventing subluxation, I describe a method to stabilize the unstable nerve after an in situ release. Furthermore, I propose a grading scheme for ulnar nerve instability to help guide treatment (Table 1). Only with a classification can we speak uniformly about ulnar nerve instability to evaluate its implication on cubital tunnel release outcomes.
TABLE 1.
Grading System of Ulnar Nerve Instability
ANATOMY
The ulnar nerve pierces the intermuscular septum of the arm at the Arcade of Struthers approximately 8 to 10 cm proximal to the medial epicondyle. The nerve then traverses posterior to the axis of the elbow behind the medial epicondyle in the retrocondylar groove. This retrocondylar groove is often mistaken for the cubital tunnel; the actual cubital tunnel is distal to the groove. The roof of the tunnel is formed by the Arcuate Ligament of Osborne, which spans the medial epicondyle and olecranon and is confluent with the aponeurosis of the FCU. The nerve then travels between the ulnar and humeral heads of the FCU and pierces the deep fascia of the flexor-pronator mass approximately 5 cm distal to the medial epicondyle.
INDICATIONS/CONTRAINDICATIONS
CubTS is a common diagnosis and the diagnostician should perform their standard history and physical specific to compressive neuropathies. Some major points include history of the symptoms, specifics of the symptoms, and location of the symptoms. Aggravating conditions should be recorded. Many patients report numbness, tingling, paresthesias or burning in the volar small finger and volar, ulnar ring finger. Some also report medial sided elbow pain. On inspection patients with severe CubTS may have intrinsic muscle wasting, a Wartenberg sign (abducted small finger because of an unopposed extensor digiti quinti because of weak or paralyzed palmar interossei), or an ulnar claw hand (because of weak ulnar lumbricals). The physical examination also includes sensory testing by static or moving 2-point discrimination or Semmes-Weinstein monofilament testing. Provocative maneuvers include the Tinel test, which involves percussing the ulnar nerve at the retrocondylary groove and 3 cm proximal and distal to it. The elbow flexion test with the elbow in maximum flexion and the wrist extended for 1 minute should recreate the patient’s paresthesias.16 Significant ulnar nerve compression can lead to a positive Froment sign (weak key pinch with flexion of the thumb interphalangeal joint as the flexor pollicis longus tries to compensate for a dysfunctional adductor pollicis), a positive Pollock test (weak flexor digitorum profundus of the small finger), or the inability to adduct/abduct the fingers.
Nerve conduction study/electromyography (NCS/EMG) is not a requirement because CubTS is a clinical diagnosis. However, I routinely order them to guide treatment, assess the severity of the compression, and help counsel the patient on expectations depending on the extent of nerve damage. The preoperative NCS/EMG is also helpful as a baseline study if there is any intraoperative nerve injury or the patient fails to improve after surgery. I recommend surgical treatment when the NCS/EMG shows moderate or severe compression. I also offer surgical treatment if the patient fails conservative treatment and has mild ulnar nerve compression on NCS/EMG. Lastly, patients who have a clinical diagnosis of CubTS but normal electrodiagnostic studies are offered surgery because the nerve study may be incorrect or the patient may have dynamic CubTS in which the nerve compression only manifests itself with activity. False negative electrodiagnostic studies may occur because there is variable compression of different fascicles but the intact large fibers yield normal conduction velocities.17
Nonoperative treatment is offered to those with mild nerve compression on NCS/EMG. This treatment includes activity modification (no leaning the medial elbow on firm surfaces, limit activities in elbow flexion) and night splinting (orthosis or towel) to prevent elbow flexion.
Contraindications to the blocking flap technique include a previous anterior transposition. As the nerve has already been transposed, the blocking flap would not be useful. If revision surgery is planned after a previous in situ decompression with no blocking flap, and the problem is nerve instability, the blocking flap may be useful. If, however, the problem is nerve cicatrix then the blocking flap will not be useful. The goal of the technique is to manage nerve instability.
A relative contraindication to the technique is detected intraoperatively. After the blocking flap is placed, the elbow is flexed to determine if the nerve stays located or if the nerve continues to sublux. If there is a large subluxation tendency of the nerve, this may cause compression against the blocking flap, which may result in continued neuropathy. This may also lead to disruption of the blocking flap creating an unstable nerve. If either of these scenarios is observed, the surgeon may consider abandoning the blocking flap technique and performing a transposition. My preferred transposition is subcutaneous so the fascia raised for the blocking flap can now be converted to the Eaton fascio-dermal sling.18
SURGICAL TECHNIQUE
Setup
Surgery is usually performed with local anesthesia and sedation under tourniquet control. Alternatively, the surgery can be performed with regional anesthesia and sedation or general anesthesia. In terms of positioning, the upper extremity is centered on an arm table with the shoulder in approximately 80 to 90 degrees of abduction. In case anterior transposition is needed, the nonsterile tourniquet should be placed high into the axilla so it is at least 10 cm proximal to the medial epicondyle to allow decompression of the Arcade of Struthers which is 8 to 10 cm proximal to the medial epicondyle. If there is not enough clearance then a sterile tourniquet should be used.
The arm is fully externally rotated and the forearm is supinated. Then 2 folded towels are placed under the olecranon with the medial edge of the towels at the ulnar edge of the olecranon, which places the elbow away from the arm table to allow clearance for hand and instrument movement; this also allows the posterior soft tissue to fall away from the incision which helps with visualization. Then sufficient towels are placed under the proximal forearm to put the elbow in about 30 degrees of flexion. Then a mark is placed on the medial epicondyle and then a 4 to 5 cm curvilinear incision is made in line with the course of the ulnar nerve 5 mm posterior to the medial epicondyle with the proximal/distal extent centered on the medial epicondyle. The incision marking is made with the elbow in the position it will be during the procedure because any change in arm positioning will change the relationship of the skin and the nerve. Local anesthetic is injected at the incision and proximal and distal to it. An esmarch is used to exsanguinate and the tourniquet is inflated. Then the arm is placed back on the towels in the same position and the same amount of flexion as when the incision markings were made (Fig. 1).
FIGURE 1.

Upper extremity positioning on arm table for cubital tunnel surgery. The shoulder is abducted 80 to 90 degrees. The arm is fully externally rotated and the forearm is supinated. Two towels are folded and placed under the olecranon. Enough towels are placed under the proximal forearm to put the elbow in 30 degrees of flexion.
Superficial Exposure
The skin is incised and scissors are used to dissect to the fascial layer. Within the subcutaneous layer, branches of the medial antebrachial cutaneous (MABC) nerve are identified and protected. The MABC branches can be in any location but typically, the branches will travel proximal, anterior to distal, posterior. Subcutaneous flaps are elevated off the fascia in all directions (proximal, distal, anterior, and posterior). If this is done, good visualization will be achieved, which can help avoid nerve injury. This will also allow mobility of the skin and adipose layer so that the “incision window” may be moved to see different aspects of the deep incision. The medial epicondyle is identified and marked at its most medial point which is not at the center of the medial epicondyle but is located proximally and slightly posterior. Some patients have a large adipose layer so it may be difficult to find the level of the fascia. If one is unclear about their position about the elbow, palpate the medial epicondyle and direct the dissection to that location. The incision may also be lengthened if visualization is an issue.
Deep Exposure
The ulnar nerve is palpated in the retrocondylar groove. The fascia over the nerve is opened at a spot where there is good visualization. This release is continued 3 to 4 cm proximal and distal to the medial epicondyle or until the surgeon is satisfied. The flimsy perineural tissue around and deep to the nerve may or may not be divided. Dividing this superficial tissue but leaving the tissue deep to the nerve may facilitate the next step, which is inspection of the nerve. The nerve is evaluated for a focal area of thickening or hyperemia of the nerve, as well as normal-appearing nerve proximal and distal to the abnormal segment, to confirm that the pathologic site has been released (Figs. 2, 3).
FIGURE 2.
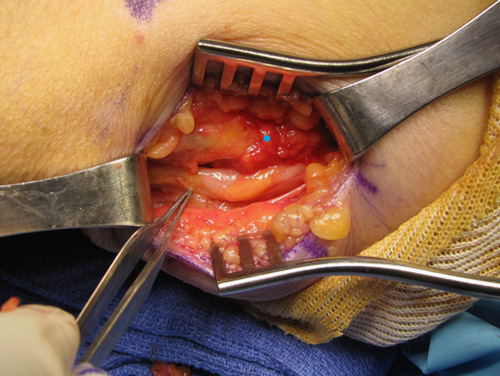
Right ulnar nerve after in situ release with forceps pointing to normal diameter nerve with swelling of the nerve 5 mm proximal to it.
FIGURE 3.
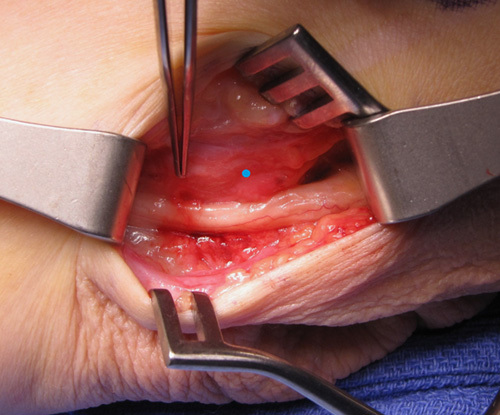
Left ulnar nerve after in situ release with forceps pointing to area of hyperemia. The blue dot in this picture and all the pictures in this manuscript, is the most medial aspect of the medial epicondyle.
Once the nerve is completely released, the elbow is flexed to evaluate for ulnar nerve instability. If the nerve is going to sublux or dislocate, it is better to know intraoperatively so it can addressed. The nerve can also be manually displaced out of the retrocondylar groove as the elbow is flexed to see if the nerve stays dislocated. Interestingly, some patient’s anatomy causes the ulnar nerve to reduce deeper into the retrocondylar groove with elbow flexion making the nerve actually more stable with elbow flexion; these patients do not need a blocking flap. If the nerve does not subluxate (Grade 0 instability, Table 1) then the procedure is complete (Fig. 4).
FIGURE 4.
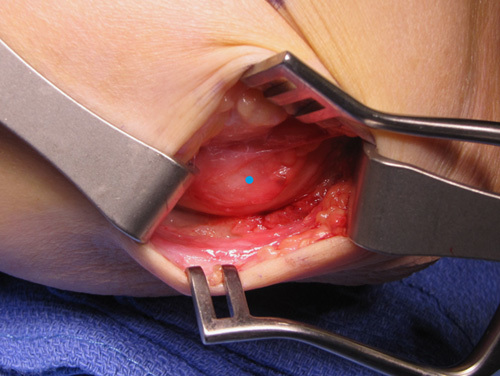
Same case as in Figure 3. With elbow flexion this ulnar nerve falls deeper into the retrocondylar groove. According to the ulnar nerve instability grading system, this is Grade 0 instability.
Reconstruction
The nerve instability should be quantified. I recommend measuring how much the medial edge of the nerve translates past the sagittal plane of the most medial aspect of the medial epicondyle, and/or the anteromedial edge of the nerve translates past the coronal plane of the most posterior aspect of the medial epicondyle. If there is ≤2 mm subluxation (Grade 1), I believe there is no need for nerve stabilization (Fig. 5). If there is >2 mm subluxation (Grade 2) but without frank dislocation, I recommend the blocking flap technique (Figs. 6A,B). This entails raising a modified Eaton fascio-dermal sling, which has been described for subcutaneous transposition.18 The original design of the sling is 3 sides of an 1 cm square with the medial side left attached to the medial epicondyle. In a subcutaneous transposition, this fascia is elevated and sutured to the anterior subcutaneous adipose layer posterior to the transposed ulnar nerve to maintain the nerve’s new location. In contrast, the blocking flap is designed as a rectangle measuring 2.5 cm in length and 1 cm in width, which is elevated from the middle third of the flexor-pronator fascia which originates from the medial epicondyle. The medial side is also left attached like the Eaton sling but the fascia is turned posteriorly on its medial attachment and sutured with 2.0 Vicryl to the subcutaneous adipose of the posterior skin flap so that it “blocks” ulnar nerve subluxation (Figs. 7–10). This does not cause a site of compression because the flap is not placed circumferentially around the nerve, nor is it sutured to a firm structure creating a circumferential enclosure. The technique simply provides a barrier to medial and anterior subluxation/dislocation.
FIGURE 5.
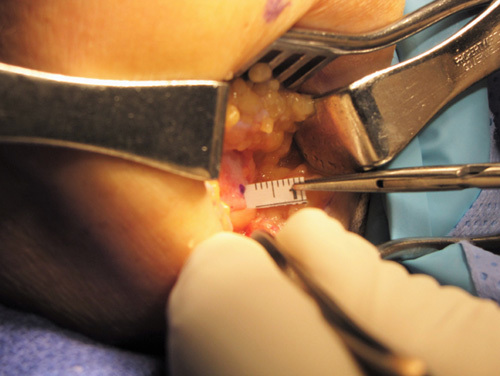
Oblique picture of right ulnar nerve release demonstrating medial translation of the nerve. Purple dot near the tip of the ruler is the most medial aspect of the medial epicondyle. Ulnar nerve is just below the ruler and shows it breaking the sagittal plane of the most medial aspect of the medial epicondyle, that is, the nerve is subluxing medial to the epicondyle. As the subluxation is <2 mm, this is Grade 1 instability.
FIGURE 6.
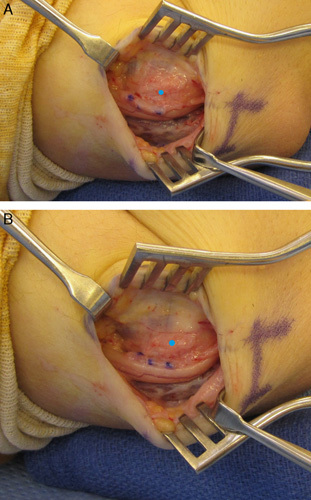
Left ulnar nerve after in situ release with the elbow in 30 degrees of flexion which shows no subluxation (A). When the elbow is flexed the ulnar nerve subluxes > 2 mm medially which is rated as Grade 2 instability (B). The degree of subluxation may be easier to assess with a finger on the medial epicondyle palpating the nerve as it subluxes, than by visualization.
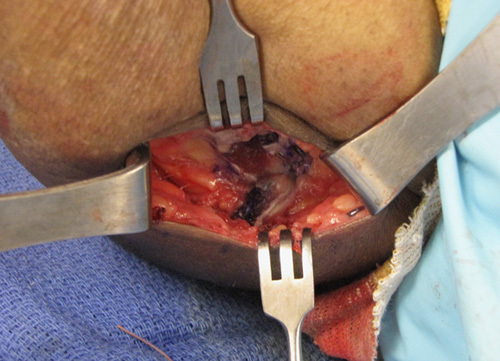
FIGURE 7.

This patient has Grade 3 instability with a nerve that dislocates out of the retrocondylar groove. The blocking flap has been raised from the flexor-pronator fascia with the medial side attached. The forceps is holding the fascia. The swollen ulnar nerve is in the inferior part of the wound out of the retrocondylar groove with a branch of the MABC laying on top of it.
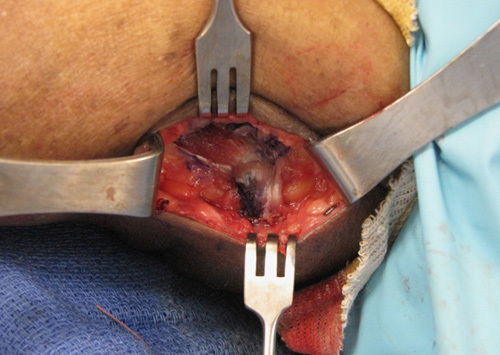
FIGURE 10.
After the flap has been sutured the elbow is taken into flexion to evaluate if the nerve is kept contained by the blocking flap. The nerve is also evaluated for other areas of compression such as the triceps, that could excessively compress the nerve anteriorly and cause disruption of the blocking flap.
FIGURE 8.

The blocking flap has been flipped posteriorly over the ulnar nerve to its intended docking site on the subcutaneous adipose layer of the posterior skin flap.
FIGURE 9.
The blocking flap has been sutured to the subcutaneous adipose layer with 2.0 Vicryl. The nerve is visible distal and proximal to the flap.
If there is gross instability of the nerve, which is defined as the nerve dislocating out of the retrocondylar groove (Grade 3), I usually perform the blocking flap technique. However, I may switch to a subcutaneous transposition for Grade 3 instability if the blocking flap cannot control the nerve instability. If the nerve is significantly pushed out of the retrocondylar groove, by the triceps for example, this may cause compression of the nerve against the blocking flap or lead to disruption of the flap. I perform a subcutaneous transposition by extending the incision (8 cm proximal and 6 cm distal to the medial epicondyle) and completely releasing the ulnar nerve as well as resecting the medial intermuscular septum. The sutures between the blocking flap and the posterior subcutaneous adipose are removed and the flap is converted to the Eaton fascio-dermal sling and sutured to the anterior subcutaneous adipose tissue, posterior to the transposed nerve.18
After securing the blocking flap, the elbow is then flexed and extended to verify that the nerve is stable without iatrogenic compression by the blocking flap or triceps. The tourniquet is released and hemostasis is obtained. The typical tourniquet time with placement of the blocking flap is 20 minutes; without the blocking flap, it takes less time.
Closure
The skin is then closed with 4-0 nylon sutures. For Grades 0 and 1 instability, a soft dressing is placed. For Grade 2 with a blocking flap, I do not splint. For Grade 3 instability with a blocking flap, I would consider a splint because the flap should be allowed to heal with the elbow immobilized because it will prevent gross dislocation of the nerve though, I have been splinting cases of Grade 3 instability less frequently because the blocking flap has successfully stabilized the nerve and there have not been any instances of dislocating nerves postoperatively. For a subcutaneous transposition, I routinely splint because of the amount of soft tissue dissection and to allow the fascio-dermal sling to heal.
Rehabilitation
Patients with a soft dressing are to keep the dressing on and the incision dry for 7 days. After 7 days, the patient is instructed that the incision may get wet in a shower and band-aids are placed. The sutures are then removed at the 10 to 14 day postoperative office visit. For an in situ release with a blocking flap, if a splint was placed it is kept on and dry until the 10 to 14 day postoperative visit. At the first postoperative visit, the splint is removed and no other immobilization is applied. Sutures are removed and scar massage is instructed to be performed for 10 minutes twice a day. The patient is taught gentle range of motion exercises of the elbow. Occupational therapy is not usually prescribed unless there is significant elbow stiffness which is not typical. All patients can increase activities as tolerated except the patients with Grade 3 instability who were treated with a blocking flap or a subcutaneous transposition; they are advised to avoid heavy (>50 lbs) lifting for another 4 weeks.
Expected Outcomes
The advantage of the blocking flap technique is it controls ulnar nerve instability in the setting of in situ decompression. In situ decompression has been shown to be as equally effective as other techniques in treating CubTS, but is a less invasive procedure with less morbidity.
Complications
The complications of the procedure include the usual ones encountered in cubital tunnel surgery including injury to the MABC and the ulnar nerve. A specific complication relating to the blocking flap would include failure/disruption of the flap so that ulnar nerve instability ensues. I have not seen this complication but I will not be surprised when it happens. To manage this problem, I would recommend a subcutaneous transposition unless the cause of failure is due to a technical flaw that would not be repeated.
CASE SERIES
I have performed 20 of these procedures in 14 patients. The average age of the patient at the time of their first surgery was 62.5 years. There was equal number of left and right elbows. In terms of severity of their CubTS, there were 9 severe, 2 moderate to severe, 4 moderate, 2 mild, 1 normal nerve study, and 1 unrated. All these patients had CTS: 9 severe, 10 moderate, and 1 mild to moderate. Intraoperatively, 14 elbows had Grade 3 instability and 6 had Grade 2. Average office visit follow-up was 1.5 months (I often discharge surgically-treated compressive neuropathy patients at the 6 wk time point). Average phone call follow-up was 4.8 months. The follow-up time period is short because 5 of these cases were done April of 2017 at the time of this writing. I am in the process of doing a formal evaluation of these patients for a case series report. Twelve of 14 patients had improvement in their subjective numbness/tingling or improvement in their ulnar nerve distributed 2-point discrimination. Of the remaining 2 patients, who did not report improvement, one patient did not remember her preoperative numbness (she had mild dementia) and the other had severe CubTS with significant intrinsic atrophy and ulnar clawing of the hand. None of the patients experienced ulnar nerve instability. On the basis of this case series I have been quite satisfied with the outcomes of this technique.
DISCUSSION
Despite being the second most common compressive neuropathy of the upper extremity, we seem to know little about the pathophysiology of CubTS, which explains our multitude of management options. It is uncommon to encounter thick compressive fascia causing an hourglass deformity of the ulnar nerve as in CTS. The cause of CubTS may be traction/tension because of its unique location posterior to the medial epicondyle/elbow. This theory would support transposition as the correct solution. However, in situ release has proven to be as effective as other techniques.5–12 The in situ release of the fascial covering of the ulnar nerve may decrease the amount nerve tension in elbow flexion, by allowing a mini-transposition of the nerve medial or anterior to the medial epicondyle, which may explain its successful outcomes. The blocking flap may allow this mini-transposition but prevents the nerve from full dislocation, which may cause nerve irritation. The flap is not sutured to a firm, immobile structure but rather to the mobile posterior subcutaneous tissue so it should not be a site of compression.
In contrast, Lane and Greenberg19 recreate the fascia covering of the nerve in a case report. These authors elevated a similar fascial flap from the flexor-pronator fascia but their flap was not from the middle third of the flexor-pronator fascia but the posterior half. The flap is also rotated posteriorly but then sutured to the medial side of the olecranon posterior to the nerve. With their design, an axilla is created between the medial epicondyle and the flap where the nerve can fall into with elbow flexion. To prevent this, the authors place sutures between the rotated fascia and the adjacent medial epicondyle. This technique also will prevent nerve subluxation/dislocation but I am concerned that this could be a potential site of compression, though the authors allow space between the flap and nerve. I was unaware of this case report, which was published in the fall of 2015 until one of the reviewers of this paper brought it to my attention. My first permutation of the blocking flap was done on February 13, 2015 and the first case of the technique described in this monogram was performed on November 16, 2015.
In summary, there are varying degrees of ulnar nerve instability after in situ release and it is unclear at what point the instability needs to be addressed. The grading scheme described in this paper is a useful way to communicate uniformly about ulnar nerve instability as none exists in the literature. The blocking flap technique is 1 method to prevent ulnar nerve subluxation/dislocation and I recommend its use for Grades 2 and 3 ulnar nerve instability. If the blocking flap does not seem to be adequate then some version of an anterior transposition can be performed.
Footnotes
Conflicts of Interest and Source of Funding: The author report no conflicts of interest and no source of funding.
REFERENCES
- 1.Bozentka DJ. Cubital tunnel syndrome pathophysiology. Clin Orthop Relat Res. 1998;351:90–94. [PubMed] [Google Scholar]
- 2.Coppieters MW, Bartholomeeusen KE, Stappaerts KH. Incorporating nerve-gliding techniques in the conservative treatment of cubital tunnel syndrome. J Manipulative Physiol Ther. 2004;27:560–568. [DOI] [PubMed] [Google Scholar]
- 3.Robertson C, Saratsiotis J. A review of compressive ulnar neuropathy at the elbow. J Manipulative Physiol Ther. 2005;28:345e1–345e18. [DOI] [PubMed] [Google Scholar]
- 4.Amadio P. Anatomical basis for a technique of ulnar nerve transposition. Surg Radiol Anat. 1986;8:155–161. [DOI] [PubMed] [Google Scholar]
- 5.Geutjens GG, Langstaff RJ, Smith NJ, et al. Medial epicondylectomy or ulnar-nerve transposition for ulnar neuropathy at the elbow? J Bone Joint Surg Br. 1996;78:777–779. [PubMed] [Google Scholar]
- 6.Gervasio O, Gambardella G, Zaccone C, et al. Simple decompression versus anterior submuscular transposition of the ulnar nerve in severe cubital tunnel syndrome: a prospective randomized study. Neurosurgery. 2005;56:108–117. [DOI] [PubMed] [Google Scholar]
- 7.Bartels RH, Verhagen WI, van der Wilt GJ, et al. Prospective randomized controlled study comparing simple decompression versus anterior subcutaneous transposition for idiopathic neuropathy of the ulnar nerve at the elbow: Part 1. Neurosurgery. 2005;56:522–530. [DOI] [PubMed] [Google Scholar]
- 8.Nabhan A, Ahlhelm F, Kelm J, et al. Simple decompression or subcutaneous anterior transposition of the ulnar nerve for cubital tunnel syndrome. J Hand Surg Eur Vol. 2005;30:521–524. [DOI] [PubMed] [Google Scholar]
- 9.Biggs M, Curtis JA. Randomized, prospective study comparing ulnar neurolysis in situ with submuscular transposition. Neurosurgery. 2006;58:296–304. [DOI] [PubMed] [Google Scholar]
- 10.Zlowodzki M, Chan S, Bhandari M, et al. Anterior transposition compared with simple decompression for treatment of cubital tunnel syndrome: a meta-analysis of randomized, controlled trails. J Bone Joint Surg Am. 2007;89A:2591–2598. [DOI] [PubMed] [Google Scholar]
- 11.Macadam S, Ghandhi R, Bezuhly M, et al. Simple decompression versus anterior subcutaneous and submuscular transposition of the ulnar nerve for cubital tunnel syndrome: a meta-analysis. J Hand Surg. 2008;33A:1314–1324. [DOI] [PubMed] [Google Scholar]
- 12.Caliandro P, La Torre G, Padua R, et al. Treatment for ulnar neuropathy at the elbow. Cochrane Database Syst Rev. 2012;7:Cd006839. [DOI] [PubMed] [Google Scholar]
- 13.Soltani AM, Best MJ, Francis CS, et al. Trends in the surgical treatment of cubital tunnel syndrome: an analysis of the national survey of ambulatory surgery database. J Hand Surg Am. 2013;38:1551–1556. [DOI] [PubMed] [Google Scholar]
- 14.Matzon J, Lutsky K, Hoffler E, et al. Risk factors for ulnar nerve instability resulting in transposition in patients with cubital tunnel syndrome. J Hand Surg Am. 2016;41:180–183. [DOI] [PubMed] [Google Scholar]
- 15.Boone S, Gelberman R, Calfee R. The management of cubital tunnel syndrome. J Hand Surg Am. 2015;40:1897–1904. [DOI] [PubMed] [Google Scholar]
- 16.Buehler M, Thayer DT. The elbow flexion test: a clinical test for the cubital tunnel syndrome. Clin Orthop. 1988;233:213–216. [PubMed] [Google Scholar]
- 17.Tapadia M, Mozaffar T, Gupta R. Compressive neuropathies of the upper extremity: update on pathophysiology, classification, and electrodiagnostic findings. J Hand Surg Am. 2010;35:668–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eaton RG, Crowe JF, Parkes JC., III Anterior transposition of the ulnar nerve using a non-compressing fasciodermal sling. J Bone Joint Surg. 1980;62:820–825. [PubMed] [Google Scholar]
- 19.Lane LB, Greenberg AS. Use of a fascial flap to stabilize an unstable ulnar nerve in its bed during in situ decompression. J Surg Orthop Adv. 2015;24:193–197. [PubMed] [Google Scholar]


