Abstract
To evaluate the safety and efficacy of retroperitoneal laparoscopic ureterolithotomy (RLU) in the treatment of proximal ureteral stones accompanied with obstructive pyelonephritis without preoperative drainage.
We retrospectively reviewed 21 cases of proximal ureteral stones with infected kidney undergoing RLU between July 2013 and September 2016. Stone-induced obstructive infected hydronephrosis was diagnosed using blood and urine tests and imaging modalities. Empirical effective broad spectrum antibiotic therapy was initiated immediately, and then urgent RLU was performed without preoperative drainage. During the surgical procedure, infected urine was also aspirated before stone was removed. Preoperative, intraoperative, and postoperative clinical data were collected.
Operations were performed successfully without open conversion or blood transfusion. The mean operation time was 69.3 ± 12.33 minutes. For all the patients, the level of plasma procalcitonin decreased after RLU. The mean hospital stay duration was 6.4 ± 1.54 days. No septic shock or other severe complications occurred. By discharge, the body temperature and hemogram of each patient returned to normal. A 100% stone-free rate was achieved.
Our study suggests that RLU is a potentially safe and effective method to treat proximal ureteral stones accompanied with obstructive pyelonephritis without any need of preoperative drainage.
Keywords: laparoscopic ureterolithotomy, obstructive pyelonephritis, preoperative drainage, ureteral stone
1. Introduction
Obstructive pyelonephritis is a common complication caused by upper urinary tract (UUT) stones and becomes a urological emergency with a potentially lethal risk if it progresses to septic shock.[1] Extracorporeal shock-wave lithotripsy (ESWL), percutaneous nephrostolithotomy (PCNL), and ureteroscopic lithotripsy (URL) are widely used mini-invasive techniques for effective treatment of UUT stones. However, given the high risk of septic shock, pyelonephritis is a contraindication to perform endoscopic stone surgery or ESWL because of high intrarenal pressure and subsequent bacterial infection absorption into circulation. For these patients with obstructive pyelonephritis, moreover, conventional antibiotic therapy can hardly relieve symptoms, because of the scarce intake of antibiotics in the affected kidney.[2] According to the current guidelines, patients with stone-induced obstructive infected hydronephrosis should receive urgent decompression by retrograde ureteral stenting or percutaneous nephrostomy and delayed stone removal.[3–5] Several days of preoperative renal drainage until the sepsis is resolved are considered essential before endoscopic surgeries can be performed,[5,6] which will inevitably prolong the hospitalization duration and increase the risk of associated adverse events. In addition, unfortunately, despite long-term preoperative drainage and even negative reexamined urine culture, the widely used mini-invasive techniques failed to completely avoid the following urosepsis.[7,8] The treatment of UUT stones accompanied with obstructive pyelonephritis remains challenging for urologists.
Laparoscopic ureterolithotomy (LU) is an effective and safe technique to remove upper ureteral stones with a high stone-free rate and low incidence of complications.[9,10] Although it is not the 1st-line choice in guidelines, LU has advantages over PCNL and URL in some selected cases.[5] The laparoscopic approach does not increase intrarenal pressure in the absence of irrigation. In addition, aspiration of the infected urine through the ureter incision can be performed conveniently simultaneously during laparoscopic approaches. So that, decompression and stone removal can be performed within a 1-session procedure, which may significantly decrease the incidence of postoperative sepsis.[11] Considering these advantages, LU is probably a feasible alternative to endoscopic surgeries following preoperative drainage. Therefore, we attempted to evaluate the safety and efficiency of urgent retroperitoneal laparoscopic ureterolithotomy (RLU) in the treatment of obstructive pyelonephritis caused by proximal ureteral stones.
2. Methods
Twenty cases of proximal ureteral stones with infected kidney was retrospectively reviewed who were treated with urgent RLU in the Department of Urology, Tongji Hospital, Huazhong University of Science and Technology, Wuhan, China, between July 2013 and September 2016. The included patients had complaints of typical clinical symptoms of obstructive pyelonephritis such as flank pain, fever (>38 °C), and costovertebral angle tenderness when admission. The diagnosis of urinary tract infection (UTI) was based on urinalysis and bacterial culture, count of white blood cell, blood bacterial culture, and plasma procalcitonin (PCT) assay. Ureteral stones and hydronephrosis were confirmed using urinary ultrasonography, computed tomography urography (CTU), and abdominal plain radiographies of the kidney, ureter, and bladder (KUB) (Fig. 1). Empirical effective broad-spectrum antibiotic therapy with cefoperazone/tazobactam was initiated immediately just after obstructive pyelonephritis was diagnosed and microbiological sample was collected.
Figure 1.
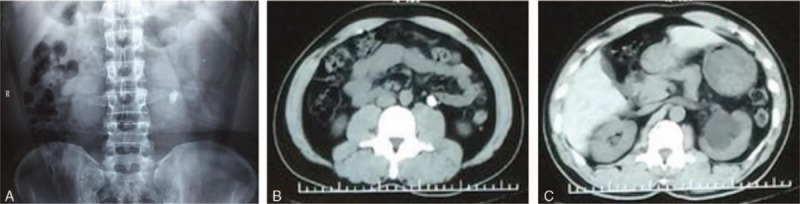
The preoperative imaging modalities of 1 patient. (A) Abdominal plain radiographies of the KUB showing the ureteral stone; (B) CTU showing the ureteral stone; and (C) CTU showing the stone-induced hydronephrosis. CTU = computed tomography urography, KUB = kidney, ureter, and bladder.
This study was approved by the ethics committees of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology. Patients were included in our case series when they met the following criteria: impacted ureteral stones of >1 cm in size, stone-induced pyelonephritis, and normal hemodynamic index. The exclusion criteria were as follows: multiple stones, sign of shock or multiple organ dysfunction syndromes, diabetes, immunocompromised status, or other diseases associated with urinary tract obstruction such as tumor, horseshoe kidneys, and ureteropelvic junction obstruction. All the patients were given a comprehensive introduction about the advantages and disadvantages of different options, including 1-session RLU and 2 weeks of nephrostomy drainage followed by PCNL or URL. Twenty-one patients selected and provided informed consent for the RUL procedures.
RLU was performed by experienced surgeons under general anesthesia, normally on the next day after the diagnosis was confirmed. The conventional 3-port standard procedure proceeded in accordance with previous reports.[12,13] To establish a working space, the fascia lumbodorsalis was divided using hemostatic forceps through a 2-cm skin incision at the subcostal posterior axillary line. The retroperitoneal space was separated by dissection of the index finger and then balloon dilatation. Another 2 ports were placed 1-cm over the iliac crest and at the subcostal anterior axillary line. After opening Gerota fascia and the perinephric fat capsule, the stone could be identified along the bulge of the ureter. The flowing infection urine was absorbed through the longitudinal ureter incision by the aspirator as much as possible before the stone was extracted (Fig. 2). After the stones were removed, a 6-Fr double J stent was inserted routinely in the pelvic and bladder, respectively.
Figure 2.
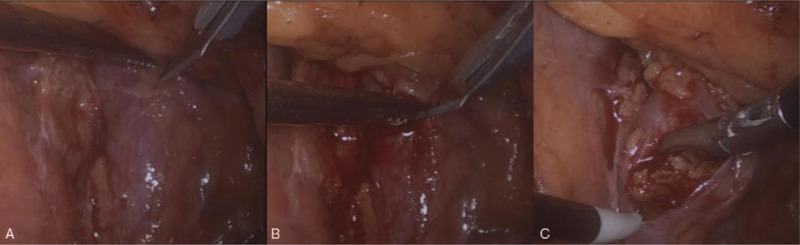
The surgical procedures. (A) Ureter dissociation and stone location identification; (B) ureter incision and urine aspiration; and (C) stone extraction.
All the patients received close postoperative surveillance. Antibiotic therapy continued until the body temperature and white blood cell returned to normal, and antibiotic species would be adjusted in accordance with the result of the bacterial culture and drug sensitivity assay. Abdominal plain radiography of the KUB and ultrasonography were performed 3 days after operation to investigate stone residuals and the position of the double J stent. The stents remained for 1 month since the date of operation. Ultrasonography or radiography of the KUB was performed 1, 3, and 6 months after operation for reexaminations.
All the procedures performed in the present study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
3. Results
Twenty-one patients, including 5 men and 16 women, underwent RLU to resolve ureteral stones accompanied with obstructive pyelonephritis. The mean age was 57.5 ± 8.60 years (range, 38–72 years). They had a mean body mass index of 22.5 ± 2.20 kg/m2 (range, 19.3–27.9 kg/m2). All the patients had fever and flank pain, with a mean body temperature of 38.8 ± 0.37 °C (range, 38.3–39.5 °C). The laboratory test demonstrated pyuria in all the patients as follows: 6 showed + (presence of 15–30 white cells per high-power field of urine); 8, ++ (30–45 white cells per high-power field of urine); and 7, +++ (45–60 white cells per high-power field of urine), respectively. Leukocytosis happened in all the patients as well; the mean blood white cell count increased to 17.3 ± 2.37 × 103/mm3 (range, 14.2–21.6 × 103). Ten of 21 urine cultures showed positive gram-negative bacteria, including Escherichia coli (8 cases) and Klebsiella pneumoniae (2 cases). In the blood cultures, 4 samples showed positivity for gram-negative bacteria (E coli) and 1 sample showed positivity for gram-positive bacteria (Enterococcus faecalis). Tests for preoperative plasma PCT revealed relatively high levels, with a mean of 7.6 ± 2.40 μg/L (range, 3.5–12.2 μg/L). The results of the other tests such as blood pressure, respiration, and coagulation function were normal. All stones located in the proximal ureter, including 8 on the left side and 13 on the right side. The mean stone size was 14.9 ± 1.26 mm (range, 12.6–17.2 mm).
Each of the RLU procedure was performed successfully without open conversion. The mean operation time was 69.3 ± 12.33 minutes (range, 52–95 minutes). None of the patients experienced severe bleeding during surgery and needed blood transfusion. The antibiotic protocol was converted in 4 cases because of insensitivity to cefoperazone/tazobactam according to the bacterial culture and drug resistance test results. After adjustment, the postoperative fever status lasted from 2 to 5 days (mean, 2.9 days). The PCT level was measured again on the 2nd day after operation, showing that PCT value decreased for each patient, with the mean value of 5.0 ± 2.13 μg/L (range, 1.4–9.1 μg/L). No perinephric abscess or wound infection occurred. In total, only 6 patients had flank pain (Clavien–Dindo grade I) and 1 had prolonged urine leakage, which was cured by adjusting the position of the ureteral stent under cystoscopy (Clavien–Dindo grade III). Overall, no septic shock or other severe complications occurred. None of the patients required intensive care unit admission or hemodynamic support. The mean hospital stay was 6.4 ± 1.54 days (range, 4–10 days), and by discharge, the body temperature and hemogram returned to normal in all the patients. Meanwhile, a 100% stone-free rate was achieved. None of the patients experienced readmission. Ureteral stents were removed 1 month after operation. No stone recurrence and ureter stricture occurred within our 6-month follow-up.
4. Discussion
Urolithiasis is one of the most common urological diseases, with a high prevalence of 1% to 20%.[14,15] UUT stone is one of the major causes of complicated UTI that is resistant to standard antibacterial treatment.[16] According to large cohorts in different countries, complicated UTIs account for approximately 20% to 32% of severe sepsis cases in emergency departments.[17–19] Obstruction due to UUT stones combined with UTI potentially results in septic shock, with a mortality rate of approximately 2% despite intensive treatment.[20,21] The management of obstructive pyelonephritis focuses on early recognition, immediate antibacterial therapy, and aggressive drainage.
Percutaneous nephrostomy tube insertion and retrograde ureteral stent insertion are the currently most widely used 2 options for prompt decompression.[22] However, neither of the 2 methods can get rid of interference of the collecting system. According to previous reports, for infected kidneys, retrograde ureteral stenting and percutaneous nephrostomy were associated with septic shock at incidence rates of 6% and 3.6%, respectively.[23,24] In addition, percutaneous nephrostomy procedure is associated with a notable rate of hemorrhage.[25] Moreover, placement of retrograde ureteral stent usually fails for impacted stones. Apart from complications, a standard of drainage duration and a criterion to perform operation are lacking.
Surgical management of ureteral stones with complicated UTI remains challenging. Normally, the size of stones that cause urinary tract obstruction is relatively larger. For treating large stones, ESWL is less effective. Single-session ESWL would hardly achieve satisfying stone clearance, whereas repeated ESWL is associated with significantly higher risk of deterioration, even death.[26] Endoscopic treatment, including URL and PCNL, is much more effective than ESWL. However, the irrigation significantly increases the intrarenal pressure, which leads to intrarenal, pyelovenous, and pyelolymphatic bacterial infection absorption. In Kanno et al's study,[7] although all patients with obstructive pyelonephritis experienced 7 days of preoperative drainage, the incidence of sepsis was still up to 8% after URL. In another study, patients underwent flexible ureteroscopy after percutaneous nephrostomy tube placement, while the postoperative sepsis rate was up to 10%.[27] Stone clearance efficiency is also a concern. Currently, either URL or PCNL can hardly achieve 100% clearance within a 1-session approach.[28] As mentioned earlier, secondary or complementary management would provide UTI another chance to develop to bacteremia.
Unlike endoscopic surgery, the laparoscopic approach has minimal impact on intrarenal pressure. In addition, aspiration through the proximal ureter incision can play the role of prompt decompression. Thus, theoretically, preoperative drainage is not necessary for a secure RLU. On the contrary, 1 randomized controlled trial showed that preoperative ureter stenting significantly increased the rate of UTI after RLU.[29] When symptoms are not significant or pyuria is not detected because of the obstruction of impacted stone, UTI might be missed. Nevertheless, for incident concurrent UTI, on the basis of our previous experience and other reports, RLU is a safe option for obstructive upper ureteral stones, even for those without preoperative indwelling drainage tubes,[12,30] indicating the security of RLU. In our present study, all the patients received complete stone clearance, without any occurrence of severe sepsis or other severe complications, and without requiring transfusion or open conversion. Finally, ureteral stent insertion and stone removal were accomplished in a single-session procedure, instead of the usual 2 sessions in previous cases. Given all the benefits, if the condition allows, urgent RUL is a rational consideration as a safe and effective option to manage ureteral stones combined with obstructive pyelonephritis, especially for patients who reject traditional preoperative drainage because of the time-consuming procedure and associated morbidities.
Although LU and open surgical stone removal are not strongly recommended in accordance with the current guidelines, they may be considered in cases for which URL, PCNL, or ESWL is risky or unlikely to be successful.[5] Compared with open surgery, laparoscopic operation is more complex and requires more surgical skills. However, it should be the preferred option before proceeding to open surgery, when performed by experienced surgeons.[5] Generally, both transperitoneal and RLU are effective, safe, and feasible. However, in the presence of UTI, the retroperitoneal approach is considered superior to the transperitoneal approach because the transperitoneal approach is associated with more gastrointestinal damage and higher risks of acute peritonitis once the infected urine passes into peritoneal cavity.
To confirm the safety of our novel approach, patients’ status must be carefully evaluated before operation to ensure that the patients could endure the adverse effects of general anesthesia and laparoscopic procedure. The appearance of septic shock or multiple organ dysfunction syndrome is a contraindication; in that case, urgent decompression is still necessary for symptom relief. On the other hand, RLU is suitable when the stone mass is centrally located so that clearance can be surely achieved within a 1-session procedure. Otherwise, for example, in case of multiple stones, initial decompression would be preferred. Besides general physical and laboratory tests, researchers also did much effort to identify risk factors that correlate with urosepsis and found that PCT level was an important predictor for monitoring the severity of bacterial infections.[31–33] In our study, preoperative PCT level indicated mild to moderate sepsis, and decreasing postoperative PCT levels confirmed improvement of the condition.
In our case series, the promising results showed that patients with obstructive pyelonephritis benefited from RUL without preoperative drainage. However, we must admit that the concept is still controversial and our study has inherent limitations. The retrospective nature and small number of patients in a single institute should be mentioned. Owing to insufficient clinical data, a comprehensive comparison of RLU with traditional protocols was not applicable. Only the single arm of RLU was reported. Moreover, not all the stones were analyzed after removal for financial reasons. Further prospective, randomized comparative trials with larger sample sizes should be undertaken to confirm our findings.
5. Conclusion
On the basis of our experience, in the absence of preoperative drainage, RUL seems to be a safe and effective option in the treatment of ureteral stones for patients with obstructive pyelonephritis, providing a low risk of septic shock and a high stone-free rate.
Acknowledgments
The authors thank National Natural Science Foundation of China (No.81500534), The National Research Foundation for the Doctoral Program of Higher Education of China (No.20130142120072), and Innovation Foundation of Huazhong University of Science and Technology (No.1802030) for the support.
Footnotes
Abbreviations: ESWL = extracorporeal shock-wave lithotripsy, KUB = kidney, ureter, and bladder, LU = laparoscopic ureterolithotomy, PCNL = percutaneous nephrostolithotomy, PCT = procalcitonin, RLU = retroperitoneal laparoscopic ureterolithotomy, URL = ureteroscopic lithotripsy, UTI = urinary tract infection, UUT = upper urinary tract.
Funding/support: This present study was supported by National Natural Science Foundation of China (No.81500534), The National Research Foundation for the Doctoral Program of Higher Education of China (No.20130142120072), and Innovation Foundation of Huazhong University of Science and Technology (No.1802030).
The authors have no conflicts of interest to disclose.
References
- [1].Hsu CY, Fang HC, Chou KJ, et al. The clinical impact of bacteremia in complicated acute pyelonephritis. Am J Med Sci 2006;332:175–80. [DOI] [PubMed] [Google Scholar]
- [2].Marien T, Mass AY, Shah O. Antimicrobial resistance patterns in cases of obstructive pyelonephritis secondary to stones. Urology 2015;85:64–8. [DOI] [PubMed] [Google Scholar]
- [3].Assimos D, Krambeck A, Miller NL, et al. Surgical management of stones: American Urological Association/Endourological Society Guideline, Part I. J Urol 2016;196:1153–60. [DOI] [PubMed] [Google Scholar]
- [4].Assimos D, Krambeck A, Miller NL, et al. Surgical management of stones: American Urological Association/Endourological Society Guideline, Part II. J Urol 2016;196:1161–9. [DOI] [PubMed] [Google Scholar]
- [5].Türk C, Knoll T, Petrik A, et al. Guidelines on Urolithiasis 2016. European Association of Urology 2017. [Google Scholar]
- [6].Ramsey S, Robertson A, Ablett MJ, et al. Evidence-based drainage of infected hydronephrosis secondary to ureteric calculi. J Endourol 2010;24:185–9. [DOI] [PubMed] [Google Scholar]
- [7].Kanno T, Matsuda A, Sakamoto H, et al. Safety and efficacy of ureteroscopy after obstructive pyelonephritis treatment. Int J Urol 2013;20:917–22. [DOI] [PubMed] [Google Scholar]
- [8].Shoshany O, Margel D, Finz C, et al. Percutaneous nephrolithotomy for infection stones: what is the risk for postoperative sepsis? A retrospective cohort study. Urolithiasis 2015;43:237–42. [DOI] [PubMed] [Google Scholar]
- [9].Shao Y, Wang DW, Lu GL, et al. Retroperitoneal laparoscopic ureterolithotomy in comparison with ureteroscopic lithotripsy in the management of impacted upper ureteral stones larger than 12 mm. World J Urol 2015;33:1841–5. [DOI] [PubMed] [Google Scholar]
- [10].Zhao C, Yang H, Tang K, et al. Comparison of laparoscopic stone surgery and percutaneous nephrolithotomy in the management of large upper urinary stones: a meta-analysis. Urolithiasis 2016;44:479–90. [DOI] [PubMed] [Google Scholar]
- [11].Fan T, Xian P, Yang L, et al. Experience and learning curve of retroperitoneal laparoscopic ureterolithotomy for upper ureteral calculi. J Endourol 2009;23:1867–70. [DOI] [PubMed] [Google Scholar]
- [12].Zhang X, Zhu Q, Ma X, et al. Retroperitoneoscopic ureterolithotomy (The experience of 26 cases). J Clin Urol (Chinese) 2003;18:327–9. [Google Scholar]
- [13].Hemal AK, Goel A, Goel R. Minimally invasive retroperitoneoscopic ureterolithotomy. J Urol 2003;169:480–2. [DOI] [PubMed] [Google Scholar]
- [14].Hesse A, Brandle E, Wilbert D, et al. Study on the prevalence and incidence of urolithiasis in Germany comparing the years 1979 vs. 2000. Eur Urol 2003;44:709–13. [DOI] [PubMed] [Google Scholar]
- [15].Stamatelou KK, Francis ME, Jones CA, et al. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int 2003;63:1817–23. [DOI] [PubMed] [Google Scholar]
- [16].Mazzulli T. Diagnosis and management of simple and complicated urinary tract infections (UTIs). Can J Urol 2012;19(Suppl 1):42–8. [PubMed] [Google Scholar]
- [17].Pro CI, Yealy DM, Kellum JA, et al. A randomized trial of protocol-based care for early septic shock. N Engl J Med 2014;370:1683–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Mouncey PR, Osborn TM, Power GS, et al. Trial of early, goal-directed resuscitation for septic shock. N Engl J Med 2015;372:1301–11. [DOI] [PubMed] [Google Scholar]
- [19].Kao CH, Kuo YC, Chen CC, et al. Isolated pathogens and clinical outcomes of adult bacteremia in the emergency department: a retrospective study in a tertiary Referral Center. J Microbiol Immunol Infect 2011;44:215–21. [DOI] [PubMed] [Google Scholar]
- [20].Yoshimura K, Utsunomiya N, Ichioka K, et al. Emergency drainage for urosepsis associated with upper urinary tract calculi. J Urol 2005;173:458–62. [DOI] [PubMed] [Google Scholar]
- [21].Reyner K, Heffner AC, Karvetski CH. Urinary obstruction is an important complicating factor in patients with septic shock due to urinary infection. Am J Emerg Med 2016;34:694–6. [DOI] [PubMed] [Google Scholar]
- [22].Pearle MS, Pierce HL, Miller GL, et al. Optimal method of urgent decompression of the collecting system for obstruction and infection due to ureteral calculi. J Urol 1998;160:1260–4. [PubMed] [Google Scholar]
- [23].Lee WJ, Patel U, Patel S, et al. Emergency percutaneous nephrostomy: results and complications. J Vasc Interv Radiol 1994;5:135–9. [DOI] [PubMed] [Google Scholar]
- [24].Flukes S, Hayne D, Kuan M, et al. Retrograde ureteric stent insertion in the management of infected obstructed kidneys. BJU Int 2015;115(Suppl 5):31–4. [DOI] [PubMed] [Google Scholar]
- [25].Millward SF. Percutaneous nephrostomy: a practical approach. J Vasc Interv Radiol 2000;11:955–64. [DOI] [PubMed] [Google Scholar]
- [26].Oh MM, Kim JW, Kim JW, et al. Bacterial sepsis after extracorporeal shock-wave lithotripsy (ESWL) of calyceal diverticular stone. Urolithiasis 2013;41:95–7. [DOI] [PubMed] [Google Scholar]
- [27].Sahin S, Resorlu B, Eksi M, et al. Flexible ureteroscopy versus laparoscopy for the treatment of patients who initially presented with obstructive pyelonephritis. Pak J Med Sci 2016;32:570–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Desai M, Sun Y, Buchholz N, et al. Treatment selection for urolithiasis: percutaneous nephrolithomy, ureteroscopy, shock wave lithotripsy, and active monitoring. World J Urol 2017;35:1395–9. [DOI] [PubMed] [Google Scholar]
- [29].Chander J, Dangi AD, Gupta N, et al. Evaluation of the role of preoperative Double-J ureteral stenting in retroperitoneal laparoscopic pyelolithotomy. Surg Endosc 2010;24:1722–6. [DOI] [PubMed] [Google Scholar]
- [30].Jiang JT, Li WG, Zhu YP, et al. Comparison of the clinical efficacy and safety of retroperitoneal laparoscopic ureterolithotomy and ureteroscopic holmium laser lithotripsy in the treatment of obstructive upper ureteral calculi with concurrent urinary tract infections. Lasers Med Sci 2016;31:915–20. [DOI] [PubMed] [Google Scholar]
- [31].Zheng J, Li Q, Fu W, et al. Procalcitonin as an early diagnostic and monitoring tool in urosepsis following percutaneous nephrolithotomy. Urolithiasis 2015;43:41–7. [DOI] [PubMed] [Google Scholar]
- [32].van Nieuwkoop C, Bonten TN, van’t Wout JW, et al. Procalcitonin reflects bacteremia and bacterial load in urosepsis syndrome: a prospective observational study. Crit Care 2010;14:R206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Singh S, Chatterji T, Sen M, et al. Serum procalcitonin levels in combination with (1)H NMR spectroscopy: a rapid indicator for differentiation of urosepsis. Clin Chim Acta 2016;453:205–14. [DOI] [PubMed] [Google Scholar]


