Abstract
Background
Community Reinforcement and Family Training (CRAFT) assists family members with a treatment-resistant loved-one. The most consistent outcome of CRAFT is increased treatment entry of the identified treatment-resistant person (IP). This led us to question whether all six components of CRAFT are necessary.
Methods
In a randomized clinical trial, 115 concerned significant others (CSOs) of an IP received 12–14 sessions of the full CRAFT intervention, 4–6 sessions focused on Treatment Entry Training (TEnT), or 12–14 sessions of Alanon/Nar-Anon Facilitation (ANF). We monitored treatment entry, attendance, and substance use of the IP and the CSO’s mood and functioning. Data were collected at baseline and 4-, 6-, and 9- months post-baseline.
Results
We found significant reductions in time to treatment entry (X2(2)=8.89, p=.01) and greater treatment entry rates for CRAFT (62%; OR=2.7, 95% CI=1.1–6.9) and TEnT (63%; OR=2.9, 95% CI=1.2–7.5) compared to ANF (37%), but CRAFT and TEnT did not differ significantly from each other (OR=1.1, 95% CI=0.4–2.7). No between-group differences in IP drug use were reported by CSOs, but days of drug use decreased over time for all groups (F(3, 277)=13.47, p<.0001). Similarly, CSO mood and functioning did not differ between the three conditions, but improved over time (p<.0001 for all significant measures).
Conclusions
We replicated the results of previous trials demonstrating that CRAFT produces greater treatment entry rates than ANF and found similar treatment entry rates for CRAFT and TEnT. This suggests that treatment entry training is sufficient for producing the best established outcome of CRAFT.
Keywords: Community Reinforcement and Family Training, concerned significant others, substance abuse, treatment entry, treatment resistance
1. Introduction
Community Reinforcement Approach and Family Training (CRAFT) is designed to help a family member or concerned significant other (CSO) of a substance-using individual who is treatment resistant. It addresses three goals: 1) engaging the identified treatment-resistant person (IP) in treatment, 2) reducing their substance use, and 3) improving the CSO’s mood and functioning. Over about 12 sessions, CSOs are trained to change their interactions with the IP to discourage continued substance use and encourage treatment entry. The six primary components of CRAFT include: 1) a functional analysis that identifies the function of the substance use and is used to develop contingency management (CM) strategies; Contingency management training, which teaches the CSO to 2) differentially reinforce the IP’s positive, sober behaviors, and 3) avoid interfering with the natural negative consequences of drug use; 4) Communication skills training, which assists the CSO in implementing CM and treatment entry training skills and in reducing conflictive and unproductive interactions; 5) Treatment entry training, which trains the CSO to recognize appropriate times and ways to suggest treatment to the IP, and also arranges rapid treatment entry for the IP; and 6) Self-care, which focuses on the CSO and involves enriching relationships and activities independent of the IP. CRAFT also includes two basic therapeutic components that are not specific to its goals: Motivation training to increase the CSO’s compliance with the intervention; and Safety training to teach the CSO to recognize precursors to physical violence and to take safety measures (Meyers et al., 1996; 1998, 1999; Meyers and Smith, 1997, Meyers and Wolf, 1998).
CRAFT was initially tested by Sisson and Azrin (1986) who randomly assigned CSOs of alcohol-dependent IPs to receive either a traditional program that provided education on the disease of addiction and a firm referral to a 12-step program for family members (i.e., Alanon; the most widely available program for helping CSOs with alcohol use disorder) or to CRAFT. None of the IPs of CSOs receiving the traditional program entered treatment, while 86% of those whose CSO received CRAFT did. Significant decreases also were seen in measures of IP drinking, even before the IP entered treatment.
In subsequent randomized trials, CRAFT has produced significantly better IP treatment entry for CSOs of problem drinkers (Miller et al., 1999; Bischof et al., 2016) and illicit drug users (Kirby et al., 1999 and Meyers et al., 2002) as compared to a 12-step group, a 12-Step facilitation intervention based on Alanon and Naranon (ANF), a waitlist, and the Johnson Intervention (Johnson, 1986; a well-known method of gathering significant others to confront the IP). Only one trial (Manuel et al., 2012) failed to show statistically significant differences in treatment entry between CSOs receiving CRAFT and those who were asked to read a CRAFT self-help book (Meyers and Wolfe, 2004); however, the trial may not have been sufficiently powered to detect the moderate effect.
Overall, when compared to a control group, CRAFT consistently produced better treatment entry of the treatment-resistant IPs, typically after 4 to 6 sessions (see Roozen et al., 2010 for a review). Also, CSOs in all of these studies reported pre- to post-intervention improvements in mood and functioning regardless of their assigned treatment condition. Unfortunately, most studies did not include a no-intervention-comparison group, so the improvements in CSO emotional wellbeing could not be attributed to the interventions per se. However, a recent study used a waitlist control and reported that CRAFT produced significant improvements in CSO mental health and relationship happiness (Bischof et al., 2016); however, these findings have not yet been replicated.
The most consistent and best supported outcome of CRAFT is increased treatment entry of the IP, which is generally achieved before all 12 CRAFT sessions have been administered. This finding led us to question whether all of the sessions are necessary or whether CRAFT could be reduced in duration and cost by focusing on fewer components. The present study conducted a component analysis of CRAFT, focusing on treatment entry training (TEnT) to determine if it alone would be sufficient to produce treatment entry rates comparable to the complete CRAFT intervention. We hypothesized that TEnT and the complete CRAFT intervention would produce similar treatment entry rates and that both would be higher compared to an ANF comparison condition. According to behavioral theory the additional components of the full intervention (e.g., contingency management training) should increase CSO sobriety support, reduce enabling, and make CRAFT more likely than TEnT or ANF to produce reductions in IP substance use (as was seen in in the initial Sisson and Azrin, 1986 study). Theoretically, both CRAFT and ANF, which contain self-care elements, should result in significant pre-to-post improvements in CSO mood and functioning compared to TEnT, which did not include self-care.
2. Material & Method
2.1 Participants, Recruitment, and Screening
CSOs were recruited through newspaper, public transportation, and radio advertisements. Institutional Review Board approval was granted by the Treatment Research Institute and the Philadelphia Department of Public Health prior to participant recruitment.
CRAFT is a clinically appropriate treatment for people who currently are in a close, established relationship with a treatment-resistant IP. It is not recommended when there is minimal contact between the CSO and IP or if the CSO has a substance use problem. To verify that the IP was treatment-resistant, potential participants were asked to invite the IP to accompany them to their first appointment. Those who attended an appointment with their IP became ineligible if the IP accepted a referral and attended treatment. Also, CSOs who reported < 12 days per month face-to-face contact with the IP or met diagnostic criteria for a substance use disorder during the past two years were not eligible. They also had to report IP substance use consistent with a diagnosis of abuse or dependence (First et al., 1995). CSOs also had to: a) be an adult parent, partner/spouse, close relative or friend of an adult IP who was using alcohol, stimulants, or opiates; b) agree not to receive outside counseling related to the IP’s substance use during the intervention and c) report no significant domestic violence in the relationship with the IP as measured by the Conflict Tactics Scale-2 (Straus et al., 2003). Finally, CSOs could be excluded if they had significant clinical mental health needs that required treatment (e.g., severe depression, suicidality). Ineligible CSOs were given a referral for services tailored to their needs.
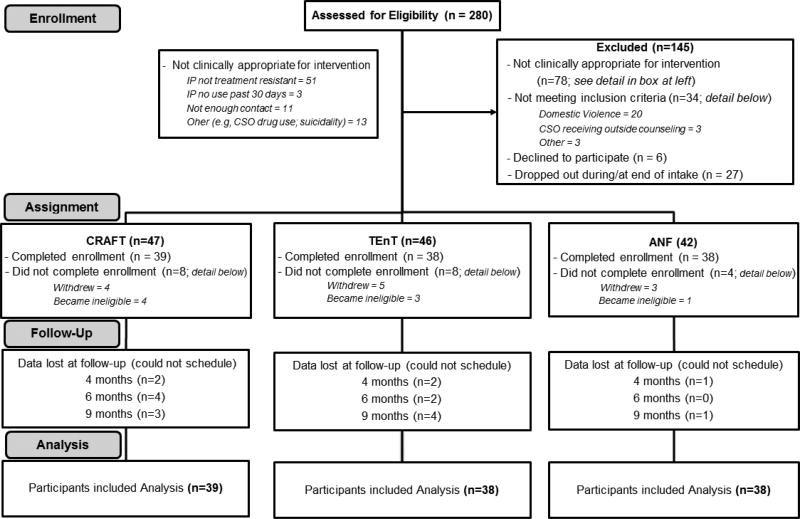
Eligible CSOs provided informed consent, completed an intake assessment, and then began their assigned intervention. A simple randomization procedure was used to assign CSOs to one of three manual-directed interventions immediately before receiving their first session (see Figure 1). Participants could become ineligible after random assignment (e.g., if domestic violence was discovered).
Figure 1.
2.2 Introductory Sessions
In order to increase participation and ensure participants safety, all participants received an introductory session and safety-training. During the introductory session, the counselor built motivation to participate in the intervention by highlighting the benefits that could be expected from it. The safety session addressed how to recognize, minimize, and respond to conflict. All sessions in all conditions were fifty minutes in duration. CSOs met with their counselor to complete all the sessions scheduled (see below), even if their IP had already entered treatment.
2.3 Interventions
2.3.1 Community Reinforcement and Family Training (CRAFT; 12–14 sessions)
trained the CSO in all CRAFT components. Therapists checked homework completion, provided instruction regarding the skill covered during that session, and engaged in role-plays using modeling, practice, and feedback until the CSO mastered it or the session was nearly over. CSOs were assigned homework to practice the skill between sessions. The CRAFT manual developed by Smith and Meyers (2004) served as the foundation for this intervention.
2.3.2 Treatment Entry Training (TEnT; 4–6 sessions)
focused on training the CSO to identify times when the IP may be more amenable to the suggestion that s/he enter treatment. Because suggesting treatment entry requires communication between the CSO and IP, communication training was included but abbreviated and focused only on treatment entry - they were not applied to other issues (e.g., substance use, relationship difficulties). The sessions followed the same structure as for CRAFT. The TEnT manual was derived from the full CRAFT manual and reviewed by Dr. Meyers.
2.3.3 Al-/Nar-Anon Facilitation (ANF; 12–14 sessions)
educated CSOs about the steps, principles, and philosophies associated with Al-Anon/Nar-Anon. The counselor provided information about 12-step philosophy and concepts, and guidance, support, and active encouragement to engage in a 12-step group. The intervention was based on a manual used in prior randomized clinical trials of CRAFT (Nowinski et al., 1992). We considered several options for the active control comparison condition, but chose ANF because it controlled for non-specific intervention factors (e.g., attention, credibility) and because previous studies showed minimal effect on the primary outcome of treatment entry when compared with CRAFT (Meyers et al., 2002; Miller et al., 1999).
2.4 IP Brief Treatment and Referral Procedure
At any point in the study, IPs from any of the three groups who expressed interest in entering treatment were offered brief motivational enhancement therapy and treatment referral at our clinic. Brief treatment consisted of one to four sessions with the goal of building the IP’s motivation for treatment and making a referral to services in the community.
In accordance with CRAFT procedures, participants assigned to CRAFT and TEnT also received rapid treatment entry, which offered an appointment within 24 hours. Participants in the ANF group received appointments according to usual practice (typically within one week)
2.5 Counselors, Training, and Clinical Supervision
Three counselors blind to the research hypotheses implemented the interventions. All had master’s degrees and at least two years of clinical experience. Counselors met 80% content criterion and had good quality ratings on module-specific checklists as assessed by doctoral-level supervisors (MLK, LAB). To control for non-specific counselor variables (e.g., credibility and competence), the same counselors administered all three interventions (cf. Behar and Borkovec, 2003). Sessions were videotaped and selectively reviewed in weekly supervision.
2.6 Intervention Integrity
A web-based one-minute interval coding system was developed to measure the dosage of specific treatment components and to check for between-intervention content contamination (e.g., ANF content appearing in a CRAFT session). Nine raters blind to the research hypotheses, experimental condition, and intervention components coded all of the sessions for 20% of the CSO participants. We coded a randomly selected subset of participants, rather than a subset of sessions because we wanted to verify that the amount of treatment entry training was constant across CRAFT and TEnT. This way if there were any treatment entry differences between the two groups, they could be attributed to the additional components of the CRAFT intervention and not to differences in the total amount of treatment entry training received over the course of the CRAFT versus TEnT interventions. Inter-rater agreement was calculated for 20% of the coded tapes and was acceptable (kappa=.91, range=0.65–1.0).
To assess contamination among the interventions, we calculated the number of sessions and total session minutes that contained elements of a different intervention than that assigned. We also assessed whether the three interventions were similar in perceived quality and credibility via the Working Alliance Inventory (Horvath and Greenberg, 1989) global scale and the task, bond, and goal subscales, and the credibility subscale of the Expectancy and Credibility Questionnaire (Devilly and Borkovec, 2000).
2.7 Assessments
Assessments were conducted by hypothesis-blinded research assistants at study intake, four months post-intake (approximate endpoint of the intervention), and 6- and 9-months post-intake follow-up. A modified Treatment Services Review-6 (TSR-6; Cacciola et al., 2008) measured IP treatment entry, time to IP treatment entry, and IP treatment transfer as reported by CSOs at each session and follow-up assessment. Initial treatment entry was operationalized as entry either to brief treatment at our clinic (see section 2.4) or directly to treatment independently provided by a community program (bypassing our clinic). Time to treatment entry was measured by counting the days between the CSO’s first session to initial treatment entry of the IP. Treatment referral occurred when IPs attending brief treatment at our program accepted a referral for continued treatment in a community program. Community treatment entry occurred when an IP who accepted a referral entered a community treatment program. Finally, community treatment attendance referred to the mean number of days that the IPs attended treatment in a community program.
The Form-90-Collateral (Miller, 1996; Scheurich et al., 2005; Westerberg et al., 1998) measured days of IP alcohol and drug use during the past 30 days as reported by the CSO. CSO mood and functioning were measured by the Beck Depression Inventory-II (BDI-II; Beck et al., 1996), the state version of the State-Trait Anxiety Inventory-State version (STAI-S-Form Y; Spielberger, 1983), the Anger Expression Index of the State-Trait Anger Expression Inventory-2 (STAXI-2; Spielberger, 1999) and by the Significant Other Survey – Self-Report (SOS-SR; Benishek et al., 2012). The latter assesses CSO problems in seven life domains (emotional, relationship, family, financial, physical violence, legal, health). CSO sobriety support and enabling were assessed at baseline and 4 months using the Sobriety Support Subscale (SSS) of the Spouse Sobriety Influence Inventory (SSII; Yoshioka et al., 1992) and the Enabling Behaviors Subscale of the Behavior Enabling Scale (EBS; Rotunda et al., 2004).
2.9 Data Analysis
As a check on randomization, we conducted chi-square analyses or analyses of variance (ANOVAs) to compare the three groups on categorical or continuous variables, respectively. We considered including baseline variables as covariates in our analyses where possible; however there were no statistically significant differences in baseline characteristics between groups. We used a logistic regression analysis to determine group differences in treatment entry rates and a Kaplan-Meier Survival Analysis to compare the groups on time to treatment entry. Clients who did not enter treatment were right censored (i.e., coded as no treatment entry and 271 days to event, which corresponded to the last day of study participation). A mixed effects model was used to examine group differences in days of IP drug use across the four assessment points. We included terms for study group and time (0, 4-, 6-, or 9-month assessment) in the model. Finally, a series of mixed effects models were used to compare the three groups on CSO sobriety support and enabling, as well as mood and functioning. Models included terms for group, time, and the group by time interaction. The models specified a compound symmetry covariance structure.
3. Results
3.1 Participant Characteristics
One hundred and thirty-five participants were randomized to an intervention. Similar numbers of participants in each condition dropped out or withdrew (CRAFT and TEnT=4; ANF=3), and several became ineligible before beginning the intervention. This resulted in 115 participants completing enrollment, beginning their assigned intervention, and being included in the analyses.
Participant demographics and intake characteristics for CSOs and their IPs are presented in Tables 1 and 2. There were no significant differences between groups.
Table 1.
Descriptive Characteristics of Concerned Significant Others (CSOs)
| CRAFT | TEnT | ANF | Total | p-value | |
|---|---|---|---|---|---|
| N | 39 | 38 | 38 | 115 | |
| Female Gender | 71.8% | 76.3% | 84.2% | 77.4% | .420 |
| Race | .243 | ||||
| Black | 35.9% | 29.0% | 52.6% | 39.1% | |
| White | 61.5% | 65.8% | 42.1% | 56.5% | |
| Other | 2.6% | 5.3% | 5.3% | 4.4% | |
| Employed (Currently) | 84.6% | 71.1% | 73.7% | 76.5% | .329 |
| Marital Status | .168 | ||||
| Married | 53.9% | 68.4% | 44.7% | 55.7% | |
| Never Married | 15.4% | 10.5% | 29.0% | 18.3% | |
| Other | 30.8% | 21.1% | 26.3% | 26.0% | |
| Mean Age (SD) | 50.6 (10.4) | 50.0 (10.9) | 49.8 (12.9) | 50.1 (11.3) | .958 |
| Mean Years of Education (SD) | 15.5 (2.7) | 15.0 (2.9) | 15.3 (2.5) | 15.3 (2.7) | .705 |
| Relationship to IP | .179 | ||||
| Parent | 23.1% | 29.0% | 26.3% | 26.1% | |
| Spouse/Partner | 59.0% | 57.9% | 39.5% | 52.2% | |
| Other | 18.0% | 13.2% | 34.1% | 21.7% | |
| Living with IP | 74.4% | 68.4% | 55.3% | 66.1% | .195 |
| Mean Days of Contact with IP Out of the Past 90 (SD) | 79.7 (19.5) | 80.2 (19.0) | 73.6 (23.9) | 77.8 (20.9) | .314 |
Table 2.
Descriptive Characteristics of the Identified Treatment-Resistant Person (IP)
| CRAFT | TEnT | ANF | Total | p-value | |
|---|---|---|---|---|---|
| N | 39 | 38 | 38 | 115 | |
| Female Gender | 41.0% | 23.7% | 47.4% | 37.4% | .087 |
| Race | .454 | ||||
| Black | 30.8% | 28.9% | 47.4% | 35.7% | |
| White | 59.0% | 63.2% | 47.41% | 56.5% | |
| Other | 10.3% | 7.9% | 5.3% | 7.8% | |
| Currently Employed | 56.4% | 60.5% | 55.3% | 57.4% | .887 |
| Marital Status | .913 | ||||
| Married | 51.3% | 57.9% | 47.4% | 52.2% | |
| Never Married | 35.9% | 28.9% | 36.8% | 33.9% | |
| Other | 12.8% | 13.2% | 15.8% | 13.9% | |
| Mean Age (SD) | 43.0 (11.4) | 44.6 (12.5) | 45.0 (14.3) | 44.2 (12.7) | .769 |
| Mean Years of Education (SD) | 13.9 (2.5) | 13.7 (2.4) | 13.3 (2.1) | 13.5 (2.6) | .291 |
| Primary Drug of Abuse | |||||
| Alcohol | 64.1% | 68.4% | 44.7% | 59.1% | .082 |
| Stimulants | 28.2% | 18.4% | 42.1% | 29.6% | |
| Opiates | 7.7% | 10.5% | 5.3% | 7.8% | |
| Other | 0% | 2.6% | 7.9% | 3.5% | |
| Mean Days Used Drugs in Past 90 (SD) | 75.4 (21.9) | 77.6 (22.6) | 73.2 (23.2) | 75.4 (22.4) | .698 |
3.2 Intervention Exposure, Fidelity, and Integrity
An average of 9.56 sessions (SD=3.20) were completed for CRAFT, 9.79 sessions (SD=2.58) for ANF, and 4.82 sessions (SD=1.39) for TEnT. Six (3.2%) of the 184 sessions coded for intervention integrity contained instances of content from a different intervention (two per condition) and there were 40 minutes of intervention contamination out of 9,451 minutes of coded session time (0.42%). As expected, the mean amount of time spent in Treatment Entry Training did not differ significantly between CRAFT and TEnT conditions (t(14)=.99, p=.34) and significantly less time (t(14)=5.55, p<.001) was spent on communication training in TEnT (2.13 minutes, SD=6.01 vs 50.40 minutes, SD=23.90 in CRAFT).
3.3 Working Alliance and Intervention Credibility
There were no significant between group differences (F(2,109)=0.54, p=.582) for working alliance on the global scale, but there was an overall effect of time on the bond subscale with higher scores following the completion of the intervention than after the first session (F(1,109)=16.27, p=.0001). The ANF group had significantly higher scores on intervention credibility (F(2,111)=6.66, p=.0019) than the CRAFT and TEnT groups at the beginning of the intervention (M=25.34, SD=2.18 vs. M=23.38, SD=3.21 and M=23.42, SD=3.41, respectively). That credibility is higher in ANF is not surprising since the 12-step approach is the most widely used program used in the United States and much better known than CRAFT or TEnT. ANF credibility scores were significantly higher scores than the TEnT group following the completion of the intervention (M=25.61, SD=2.49 vs. M=23.30, SD=4.45). There were no significant differences between CRAFT (M=23.92, SD=4.40) and either TEnT or ANF post-intervention. Overall differences in credibility scores among the groups were small and a bias favoring ANF suggests that any differences in intervention outcomes were not due to poor credibility of the ANF control comparison condition.
3.4 IP Treatment Entry
3.4.1 Initial Treatment Entry
rates were 62% (n=24) and 63% (n=24) in the CRAFT and TEnT conditions, respectively, and 37% (n=14) in the ANF condition. A logistic regression analysis indicated this was a significant difference (X2(2)=6.5, p=.04), with the CRAFT (OR=2.7, 95% CI=1.1–6.9) and TEnT (OR=2.9, 95% CI=1.2–7.5) groups having significantly higher rates than ANF. CRAFT and TEnT groups did not differ from each other (OR=1.1, 95% CI=0.4–2.7).
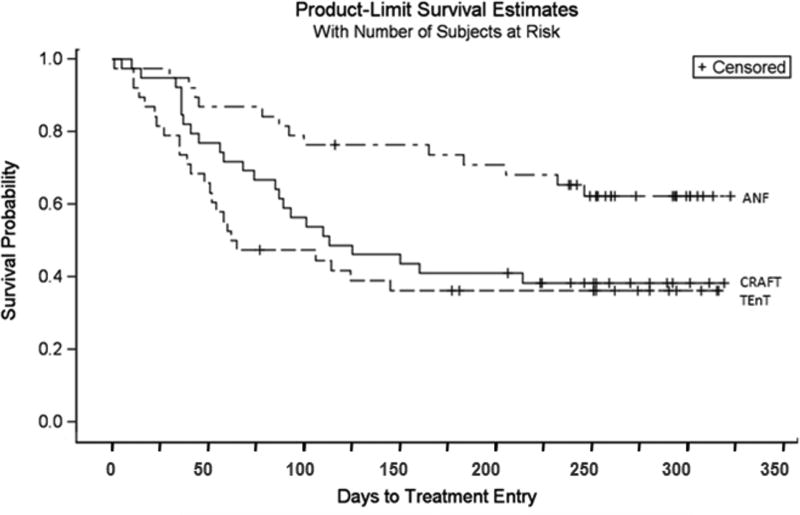
3.4.2 Time to Treatment Entry
Figure 2 shows the percentage of IPs remaining out-of-treatment each day after the CSO’s first treatment session. A downward drop is created each time an IP enters treatment. The mean days from first session to treatment entry among the three groups were 130.31 (SE=12.50) days for CRAFT, 85.25 (SE=8.97) for TEnT, and 196.00 (SE=13.53) for ANF. The Kaplan-Meier survival analysis indicated these were significant differences (X2(2)=8.89, p=.01). Post hoc tests showed that relative to ANF, both CRAFT (X2(1)=5.59, p=.02; HR=2.12, 95% CI=1.12–4.22) and TEnT (X2(1)=8.08, p=.005; HR=2.54, 95% CI=1.31–4.93) had less time to treatment entry. Overall there were no differences between CRAFT and TEnT groups (X2(1)=0.61, p=.43).
Figure 2.
The percentage of IPs not entering treatment each day after the CSO’s first intervention session.
3.4.3 Treatment Referral and Community Treatment Entry
Forty-two IPs (CRAFT=18; TEnT=20; ANF=4) received brief treatment and referral at our clinic. About half (n=22; 52%) accepted a community treatment referral (see Table 3). Due to the low number of participants in the ANF group, it was dropped from statistical comparisons on this variable. A comparison of CRAFT and TEnT showed no significant differences between groups (X2(1)=1.69, p=.194). Although 22 participants accepted a community treatment referral, only 12 of them actually entered community treatment (29% of the 42 attending brief treatment).
Table 3.
Treatment Entry Outcomes for Identified Treatment-Resistant Person (IP)
| Outcome | n | CRAFT | TEnT | ANF | p |
|---|---|---|---|---|---|
| Initial Treatment Entry % (N) | 115 | 39 | 38 | 38 | |
| 61.5 (24)a | 63.2 (24)a | 36.8 (14)b | .039 | ||
| Days of Community Treatment Attendance M (SD) | 10.1 (27.3) | 9.1 (24.0) | 4.7 (10.7) | .530 | |
|
| |||||
| Initial Treatment Entry Breakdown: | 62 | 24 | 24 | 14 | |
| Direct to Community Program % (N) | 25.0 (6) | 16.7 (4) | 71.4 (10) | -- † | |
| Brief Treatment % (N) | 75.0 (18) | 83.3 (20) | 28.6 (4) | -- † | |
| % Accepted Treatment Referral, of those entering Brief Treatment (N) | 42 | 18 | 20 | 4 | |
| 38.9 (7) | 60.0 (12) | 75.0 (3) | .194* | ||
| % Community Treatment Entry, of those Accepting Referral (N) | 22 | 7 | 12 | 3 | |
| 28.6 (2) | 58.3 (7) | 100.0 (3) | -- † | ||
Notes. Post hoc test results shown in superscripts (non-matching letters indicate a significant difference between values);
=ANF group not included in chi-square analysis due to small n;
= No statistical analyses conducted.
Definitions:
Initial Treatment Entry = entry to either brief treatment at our clinic or directly to community program
Brief Treatment = 1–4 sessions of MET at our clinic
Community Treatment Attendance = only attendance at a community treatment program; brief treatment attendance at our clinic excluded
Direct to Community Program = Entry to community program bypassing brief treatment at our program
Treatment Referral = Attended brief treatment and accepted community treatment referral
Community Treatment Entry = Accepted a treatment referral and entered community treatment
3.4.4 Community Treatment Attendance
The mean number of days that the IPs attended treatment is presented in Table 3. On average, IPs whose CSOs received CRAFT or TEnT attended about twice as many sessions as IPs whose CSO received ANF, but a non-parametric Kruskal-Wallis test comparing the rank sums of participants in the three groups indicated no significant between group differences (X2(2)=1.27, p=.53).
3.5 IP Substance Use
CSOs reported higher rates of primary substance use for their IP at intake than at any of the follow-up points (F(3,277)=13.47, p<.0001; see Table 4). There were no significant differences between intervention groups (F(2,111)=0.40, p=.67) and no group by time interaction. A secondary analysis comparing substance use outcomes of IPs who did and did not achieve initial treatment entry indicated a main effect with those initially entering treatment having fewer days of drug use than those who did not (F(1,112)=2.39, p=.02, d=.38). However, the interaction with condition and time was not significant (F(3, 280)=1.09, p=.35).
Table 4.
Results of Mixed Effects Models
| Outcome | Group | Baseline n=113 (M/SD) |
4-Months n=94 (M/SD) |
6-Months n=99 (M/SD) |
9-Months n=94 (M/SD) |
p |
|---|---|---|---|---|---|---|
| Identified Treatment-Resistant Person (IP) Drug Use | ||||||
| Past 90 Day Drug Use M (SD) | CRAFT | 72.2(23.8)a | 56.2b (28.7) | 55.9b (32.0) | 62.9b (27.7) | < .0001* |
| TEnT | 68.4(26.5)a | 63.2b (26.0) | 55.9b (29.7) | 54.6b (34.1) | ||
| ANF | 66.8 (27.2)a | 55.4b (30.9) | 56.0b (31.6) | 57.2b (31.1) | ||
|
| ||||||
| Concerned Significant Other (CSO) Behavior Toward IP | ||||||
| Sobriety Support | CRAFT | 3.82a (1.44) | 4.14a (1.32) | -- | -- | .026** |
| TEnT | 3.76a (1.52) | 3.57a (1.63) | -- | -- | ||
| ANF | 3.69a (1.53) | 3.28b (1.43) | -- | -- | ||
| Behavior Enabling | CRAFT | 1.86a (0.44) | 1.77b (0.41) | -- | -- | < .0001* |
| TEnT | 1.94a (0.52) | 1.69b (0.44) | -- | -- | ||
| ANF | 2.00a (0.52) | 1.55b (0.38) | -- | -- | ||
Note. Post hoc test results shown in superscripts (non-matching letters indicate a significant difference between values).
= Main effect of time only significant effect;
= Significant interaction effect only, no main effect of time or between-group differences.
3.6 CSO Mood and Functioning
CSO mood and functioning showed no significant between group or interaction effects. However, depression (F(3,304)=29.13, p< .0001), anxiety (F(3,306)=11.06, p<.0001), and anger expression (F(3,304)=7.44, p< .0001) decreased over time, indicating improvement in all three groups. Similarly, CSO problems decreased over time for frequency and severity, respectively for emotional (F(3,307)=24.98, p<.0001; F(3,307)=11.96, p< .0001), relationship (F(3,307)=52.24, p< .0001; F(3,307)=37.60, p< .0001), and family problems (F(3,307)=53.30, p<.0001; F(3,307)=34.05, p< .0001). The other four life areas measured by the SOS were not analyzed because of low frequencies and non-normal distributions.
3.7 CSO Enabling and Sobriety Support
There was a significant group by time interaction for CSO sobriety support (F(2,101)=3.79, p=.026) such that CSOs in the ANF group were less likely to report engaging in sobriety support behaviors after receiving the intervention (d=−.27). There were no statistically significant changes for those receiving CRAFT or TEnT (d ’s=.21 and −.10, respectively). Also, CSOs in all three groups were less likely to report enabling behaviors after receiving the intervention (F(1,104)=57.71, p< .0001; see Table 4).
4. Discussion
4.1 Treatment Entry
This study replicated previous findings in that CRAFT produced treatment entry among treatment-resistant individuals at about three times the rate of ANF. It also showed that the TEnT component of CRAFT is sufficient to produce treatment entry at rates comparable to those found with the complete CRAFT intervention in fewer sessions and at less cost. Despite the fact that TEnT focused immediately on treatment entry, it did not result in the IP entering treatment significantly sooner compared to the full CRAFT intervention that addressed other behaviors first. However, it is worth noting that during the first 60 days of the intervention the slope of the survival curve appeared steeper (i.e., more people entered treatment) in TEnT relative to both CRAFT and ANF. A larger study might have sufficient power to detect statistically significant differences. Since faster treatment entry is important to family members, especially when there is risk of overdose, even small differences could be clinically meaningful.
Although CRAFT and TEnT produced high levels of brief treatment entry at our clinic, rates of transferring IPs to longer-term community treatment were less impressive. Overall, only 29% of the IPs entering brief treatment at our clinic were successfully transferred to treatment in the community. Although the differences between groups in the proportion of IPs transferring to community treatment were large, they were not statistically significant. Research with larger numbers of IPs is needed, but it may be that CRAFT and TEnT are best delivered in the context of a treatment program that offers full services to IPs, making transfer to community services unnecessary. Others have reported limited success executing similar transfers of substance using populations (about 10% to 20%; Chutaupe et al., 2001; Kimber et al., 2008; McCusker et al., 1995). The rates of transfer that we achieved are similar to those in studies of Screening, Brief Intervention and Referral to Treatment (SBIRT; Babor et al., 2007). For example, Krupski et al. (2010) reported transfer rates of 33.8% overall, but had less success with patients who had not previously received specialty treatment (26.6%). Although the mean number of community treatment sessions attended was about twice as high in CRAFT and TEnT as in ANF, these differences were not statistically significant. Thus, once the IP entered treatment in the community, there were no apparent differences in retention as a function of the intervention.
4.2 Substance Use
Even though initial treatment entry predicted lower drug use overall, our mixed effects model analysis did not show differences in substance use between groups over time. This is contrary to what behavioral theory would predict as CRAFT trains CSOs to provide contingent reinforcement for abstinence whereas TEnT and ANF do not. The lack of differences between CRAFT and ANF is similar to previous CRAFT randomized trials. There are several possible explanations for these results. First, since all groups showed significant decreases in drug use over time, it is possible that the reductions in the CRAFT group were due to CSOs providing positive reinforcement for abstinence, and that the similar reductions in the TEnT and ANF groups occurred due to other mechanisms. As in previous CRAFT trials, it is impossible to know whether the interventions were responsible for the reductions in drug use because a no-treatment control or waitlist comparison group was not included.
Perhaps a more likely explanation is that CSOs were not providing contingent reinforcement for IP drug abstinence at home or that they did so ineffectively, as CRAFT does not train CSOs to directly reinforce urinalysis-verified drug abstinence as is the case in empirically-supported applications of abstinence reinforcement (Lussier et al., 2006; Prendergast et al., 2006). In addition, CRAFT does not necessarily provide clear advanced specification of consequences, it uses social versus tangible reinforcers, and it may use less effective reinforcement schedules.
4.3 CSO Mood and Functioning
Also contrary to what theory would predict, there were no differences between groups in improvements of CSO mood and functioning even though CRAFT and ANF encouraged self-care while TEnT did not. It is possible that entering into any type of supportive counseling relationship or taking any steps to address IP behavior reduces these problems for CSOs. Once again, we cannot make firm conclusions about the effects of the interventions on CSO mood and functioning because of the absence of a no-treatment comparison; however, some support for this explanation comes from Bischof et al. (2016), which found improvements in CSO mental health in CRAFT group compared to a waitlist control.
The changes in CSO behavior enabling were also different than expected. There were significant decreases in behavior enabling in all three groups, not just in the CRAFT and ANF groups where this behavior was directly addressed. It is not clear why decreases occurred in the TEnT group, and it may be that the small reductions in all three groups were not clinically meaningful. The measure may not adequately track changes that occur in CSO behavior as a function of the interventions, or more likely, CSOs may not make large changes in the behaviors trained in the interventions. It is possible that the only CSO behavior that reliably changes is suggesting treatment entry for CSOs receiving CRAFT or TEnT. Some support for this is suggested in the SSS data, which indicated that the CRAFT group did not report significant increases in behaviors that would support sobriety in their IPs over time. Although it is worth noting that the CRAFT group showed small nonsignificant increases in SSS, while there were significant decreases in this measure for the ANF group. This is consistent with the fact that ANF did not specifically address sobriety support. Al-Anon and Nar-Anon groups do place considerable emphasis on reducing enabling behaviors and perhaps this focus in the absence of discussing sobriety support results in family members reducing positive reinforcement, even when their IP is sober.
4.4 Limitations
A limitation of this study is that, similar to prior CRAFT studies, data on the IP treatment attendance and drug use were collected from the CSOs, rather than directly from the IPs. Although we asked IPs to have their treatment program verify session attendance, they very rarely provided permission. It is not clear how accurately CSOs in this study reported on their IP’s substance use, although significant correlations on frequency of target drug use have been reported (r=0.73, p < .01; Meyers et al., 2002). Still, we cannot be sure that the significant decreases in substance use from baseline to follow-up assessments were actual or merely perceived on the part of the CSO. Obtaining biological verification of substance use from the IPs would have been preferable, but with treatment-resistant IPs, collecting these data for all participants is not possible.
5. Conclusion
This study provides the first component analysis of CRAFT. The finding that the treatment entry training component produces results similar to the full CRAFT intervention suggests that the main benefits of CRAFT may be realized with half as many sessions, saving time and costs. However, it is possible that there are differences in outcomes that were not measured in this study (e.g., relationship satisfaction, family conflict), so further research is needed to explore other possible differences in CSO and IP outcomes. It also will be important to assess the replicability of our findings using larger sample sizes and to compare CRAFT and TEnT on IP treatment entry when the IP is offered treatment in-house versus referral to an outside treatment program. Furthermore, we should note that the treatment entry module of CRAFT is actually comprised of two procedures; training CSOs to suggest treatment entry and arranging rapid treatment entry. Additional analyses would be needed to understand the relative contributions of these procedures. Finally, future studies should consider including a wait list condition. Bischof et al.’s (2016) inclusion of this condition suggested that CRAFT may contribute to improvements in CSO mental health. It would be useful to determine if reductions in substance use and CSO mood and functioning seen in CRAFT, TEnT, and ANF are due to similar or nonspecific treatment effects across interventions, or simply represent a regression toward the mean.
Acknowledgments
The authors would like to acknowledge contributions of the research staff (Cassandra Allen, Venice Anderson, Deborah Black, Meridith Carter, Laura Del Fra, Alicia Janik, Tisha Miller, Beth Rosenwasser, Kristin Salber-Black, Stephanie Shealy, Danette Wright-Lee) and the integrity raters (Lindsay Anmuth, Caitlin Kelly, Stephanie Kerrigan, Yong Lee, Scott List, Kelly MacKenzie, Matt Parke, Debbie Stevenson). Thanks also to Dr. Thomas Borkovec for providing consultation on the development of the integrity measures and research design.
Role of Funding Source
This research was supported by the National Institutes of Health – National Institute on Drug Abuse/NIDA [R01 DA018696, P50 DA027841]. NIDA had no role in the study design; in the collection, analysis, and interpretation of the data; in the writing of the manuscript; or in the decision to submit the manuscript for publication.
Footnotes
Contributors
Kimberly C. Kirby (principal investigator) was primarily responsible for designing the study, attaining funding, conducting the trial and writing and revising the manuscript. Lois A. Benishek, MaryLouise E.Kerwin, and Robert J. Meyers conceptualized and oversaw the interventions and provided clinical training and supervision to counselors. Lois A. Benishek, Karen L. Dugosh, and Carolyn M. Carpenedo assisted with writing sections of the manuscript. James A. Haugh trained and supervised staff responsible for assessing intervention fidelity. Carolyn M. Carpenedo was responsible for data management/cleaning and assisted with statistical analyses. Karen L. Dugosh took primary responsibility for data analysis. All authors provided substantive feedback on drafts of the paper and approved the submitted manuscript.
Conflict of Interest
No conflict declared.
Prior Dissemination
Some of the data presented in this manuscript were presented in a poster presentation at an annual meeting of the College on Problems of Drug Dependence and at invited meetings sponsored by the National Institute on Drug Abuse. Data were also presented to local organizations and community groups.
References
- Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT): toward a public health approach to the management of substance abuse. Substance Abuse. 2007;28:7–30. doi: 10.1300/J465v28n03_03. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Behar E, Borkovec TD. Between group psychotherapy outcome research. In: Schinka JA, Velicer W, editors. Comprehensive Handbook of Psychotherapy: Vol. 2. Research Methods. New York, NY: Wiley; 2003. pp. 213–241. [Google Scholar]
- Benishek LA, Carter M, Clements NT, Allen C, Salber KE, Dugosh KL, Kirby KC. Psychometric assessment of a self-administered version of the Significant Other Survey. Psychology of Addictive Behaviors. 2012;26:986–993. doi: 10.1037/a0030378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischof G, Iwen J, Freyer-Adam J, Rumpf H. Efficacy of the Community Reinforcement and Family Training for concerned significant others of treatment-refusing individuals with alcohol dependence: a randomized controlled trial. Drug and Alcohol Dependence. 2016;163:179–185. doi: 10.1016/j.drugalcdep.2016.04.015. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Alterman AI, Lynch KG, Martin JM, Beauchamp ML, McLellan AT. Initial reliability and validity studies of the revised Treatment Services Review (TSR-6) Drug and Alcohol Dependence. 2008;92:37–47. doi: 10.1016/j.drugalcdep.2007.06.004. [DOI] [PubMed] [Google Scholar]
- Chutuape MA, Katz EC, Stitzer ML. Methods for enhancing transition of substance dependent patients from inpatient to outpatient treatment. Drug and Alcohol Dependence. 2001;61:137–43. doi: 10.1016/S0376-8716(00)00133-2. [DOI] [PubMed] [Google Scholar]
- Devilly GJ, Borkovec TD. Psychometric properties of the Credibility/Expectancy Questionnaire. Journal of Behavior Therapy and Experimental Psychiatry. 2000;31:73–86. doi: 10.1016/S0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer L, Gibbon M, Williams J. Structural Clinical Interview for Axis I DSM-IV disorders (SCID) Washington, D.C: American Psychiatric Association; 1995. [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36:223–233. doi: 10.1080/10503300500352500. [DOI] [Google Scholar]
- Johnson VE. Intervention: How to Help Those Who Don't Want Help. Minneapolis, MN: Johnson Institute; 1986. [Google Scholar]
- Kimber J, Mattick RP, Kaldor J, van Beek I, Gilmour S, Rance JA. Process and predictors of drug treatment referral and referral up-take at the Sydney Medically Supervised Injecting Centre. Drug and Alcohol Review. 2008;27:602–612. doi: 10.1080/09595230801995668. [DOI] [PubMed] [Google Scholar]
- Kirby KC, Marlowe DB, Festinger DS, Garvey KA, LaMonaca V. Community reinforcement training for family and significant others of drug abusers: a unilateral intervention to increase treatment entry of drug users. Drug and Alcohol Dependence. 1999;56:85–96. doi: 10.1016/S0376-8716(99)00022-8. [DOI] [PubMed] [Google Scholar]
- Krupski A, Sears JM, Joesch JM, Estee S, He L, Dunn C, Ries R. Impact of brief interventions and brief treatment on admissions to chemical dependency treatment. Drug and Alcohol Dependence. 2010;110:126–3. doi: 10.1016/j.drugalcdep.2010.02.018. [DOI] [PubMed] [Google Scholar]
- Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311. [DOI] [PubMed] [Google Scholar]
- Manuel JK, Austin JL, Miller WR, McCrady BS, Tonigan JS, Meyers RJ, Bogenschutz MP. Community Reinforcement and Family Training: a pilot comparison of group and self-directed delivery. Journal of Substance Abuse Treatment. 2012;43:129–136. doi: 10.1016/j.jsat.2011.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCusker J, Bigelow C, Luippold R, Zorn M, Lewis BF. Outcomes of a 21-day drug detoxification program: retention, transfer to further treatment, and HIV risk reduction. American Journal of Drug and Alcohol Abuse. 1995;21:1–16. doi: 10.1016/j.jsat.2010.08.007. [DOI] [PubMed] [Google Scholar]
- Meyers RJ, Dominguez T, Smith JE. Community reinforcement training with concerned others. In: Hasselt VB, Hersen M, editors. Source of Psychological Treatment Manuals for Adult Disorders. New York, NY: Plenum Press; 1996. pp. 257–294. [Google Scholar]
- Meyers RJ, Miller WR, Hill DE, Tonigan JS. Community Reinforcement and Family Training (CRAFT): engaging unmotivated drug users in treatment. Journal of Substance Abuse. 1999;10:291–308. doi: 10.1016/S0899-3289(99)00003-6. [DOI] [PubMed] [Google Scholar]
- Meyers RJ, Miller WR, Smith JE, Tonigan J. A randomized trial of two methods for engaging treatment-refusing drug users through concerned significant others. Journal of Consulting and Clinical Psychology. 2002;70:1182–1185. doi: 10.1037//0022-006X.70.5.1182. [DOI] [PubMed] [Google Scholar]
- Meyers RJ, Smith JE. Getting off the fence: procedures to engage treatment resistant drinkers. Journal of Substance Abuse Treatment. 1997;14:467–472. doi: 10.1016/S0740-5472(97)00122-0. [DOI] [PubMed] [Google Scholar]
- Meyers RJ, Smith JE, Miller EJ. Working through the concerned significant other: Community Reinforcement and Family Training. In: Miller WR, Heather N, editors. Treating Addictive Behaviors: Processes of Change. 2. New York, NY: Plenum Press; 1998. pp. 141–161. [Google Scholar]
- Meyers RJ, Wolfe BL. Community Reinforcement and Family Training for families of substance abusers. The Counselor. 1998:24–29. [Google Scholar]
- Meyers RJ, Wolfe BL. Getting Your Loved One Sober: Alternatives to Nagging, Pleading, and Threatening. Center City, MN: Hazelden; 2004. [Google Scholar]
- Miller WR. Form 90: a structured assessment interview for drinking and related behaviors. In: Mattson ME, Marshall LA, editors. Project MATCH Monograph Series. Vol. 5. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1996. [Google Scholar]
- Miller WR, Meyers RJ, Tonigan J. Engaging the unmotivated in treatment for alcohol problems: a comparison of three strategies for intervention through family members. Journal of Consulting and Clinical Psychology. 1999;67:688–697. doi: 10.1037//0022-006X.67.5.688. [DOI] [PubMed] [Google Scholar]
- Nowinski J, Baker S, Carroll K. 12-step therapist facilitation manual: a clinical research guide for therapists treating individuals with alcohol abuse and dependence. Vol. 1. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 1992. [Google Scholar]
- Prendergast M, Podus D, Finney J, Greenwell L, Roll J. Contingency management for treatment of substance use disorders: a meta-analysis. Addiction. 2006;101:1546–1560. doi: 10.1111/j.1360-0443.2006.01581. [DOI] [PubMed] [Google Scholar]
- Roozen HG, de Waart R, van der Kroft P. Community Reinforcement and Family Training: an effective option to engage treatment-resistant substance-abusing individuals in treatment. Addiction. 2010;105:1729–1738. doi: 10.1111/j.1360-0443.2010.03016.x. [DOI] [PubMed] [Google Scholar]
- Rotunda RJ, West L, O’Farrell TJ. Enabling behavior in a clinical sample of alcohol-dependent clients and their partners. Journal of Substance Abuse Treatment. 2004;26:269–76. doi: 10.1016/j.jsat.2004.01.007. [DOI] [PubMed] [Google Scholar]
- Scheurich A, Muller MJ, Anghelescue I, Lorch B, Dreher M, Hautziger M, Szegedi A. Reliability and validity of the Form-90 interview. European Addiction Research. 2005;11:50–56. doi: 10.1159/000081417. [DOI] [PubMed] [Google Scholar]
- Sisson RW, Azrin NH. Family-member involvement to initiate and promote treatment of problem drinkers. Journal of Behavior Therapy and Experimental Psychiatry. 1986;17:15–21. doi: 10.1016/0005-7916(86)90005-4. [DOI] [PubMed] [Google Scholar]
- Smith JE, Meyers RJ. Motivating Substance Abusers to Enter Treatment: Working With Family Members. New York, NY: Guilford Press; 2004. [Google Scholar]
- Spielberger CD. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychology Press; 1983. [Google Scholar]
- Spielberger CD. State-Trait Anger Expression Inventory-2: professional manual. Odessa, TX: Psychological Assessment Resources; 1999. [Google Scholar]
- Straus MA, Hamby SL, Warren WL. The Conflict Tactics Scales Handbook. Los Angeles, CA: Western Psychological Services; 2003. [Google Scholar]
- Westerberg VS, Tonigan JS, Miller WR. Reliability of the Form-90D: an instrument for quantifying drug use. Substance Abuse. 1998;19:179–189. doi: 10.1023/A:1021429429459. [DOI] [PubMed] [Google Scholar]
- Yoshioka MR, Thomas ED, Ager RD. Nagging and other drinking control efforts of spouses of uncooperative alcohol abusers: assessment and modification. Journal of Substance Abuse. 1992;4:309–318. doi: 10.1016/0899-3289(92)90038-Y. [DOI] [PubMed] [Google Scholar]