Abstract
Background
Community noise exposure has been shown to increase the risk of hypertension; however, the relationship between occupational noise exposure and hypertension is less clear.
Methods
Using an inception cohort of workers in a specialty metals manufacturing company, we retrospectively assessed occupational noise exposure, hearing acuity, and incident hypertension diagnoses using administrative datasets. Time-weighted average noise exposure levels were assigned to employees based on their job histories. Cox proportional hazards models were performed to determine the association of noise exposure with risk of incident hypertension.
Results
The adjusted hazard ratio (HR) of incident hypertension did not significantly differ between groups by cumulative continuous or categorized noise exposure metric.
Conclusion
We found no increased risk of incident hypertension with exposure to occupational noise among workers. Further assessment examining workers’ use of hearing protection devices is warranted.
Keywords: occupational noise, noise exposure, workplace health, hypertension, occupational health and safety
Introduction
Noise exposure has long been considered one of the most ubiquitous hazards in the workplace, with noise-induced hearing loss being its most well understood outcome. Research has also demonstrated an association between community noise exposure (e.g., exposures associated with road, rail, and air traffic) and an increase in risk of cardiovascular disease, including hypertension, myocardial infarction, stroke, and death due to coronary heart disease [Sorensen et al., 2012; Willich et al., 2006; Ndrepepa and Twadella, 2011; Babisch 2014; Hansell et al., 2013; Rosenlund et al., 2001; Eriksson et al., 2007; van Kempen and Babisch, 2012; Munzel et al., 2014]. Swinburn et al [2015] estimated that a 5-dB community noise reduction in the United States could lead to a decrease in prevalence of hypertension by 1.4% and coronary heart disease by 1.8%. However, research on the relationship between occupational noise exposure and cardiovascular outcomes is more ambiguous [van Kempen et al., 2002].
Hypertension in particular has been studied as an outcome of occupational noise exposure. Approximately one in three adults in the United States develop hypertension, making it one of the most common chronic diseases [NCHS 2014]. In response, many employers have implemented initiatives aimed at prevention and proper treatment of hypertension in order to reduce the massive economic burden of the disease, which totaled $47.5 billion in the US in 2010 alone [Go et al., 2013]. A reduction in prevalence and costs of hypertension could also have benefits beyond decreases in direct health care costs, including potential reductions in absenteeism, disability claims, and premature retirement [CDC, 2014].
Although the exact causal pathway for the potential association between occupational noise exposure and hypertension is unknown, it is most plausible that noise exposure, either through annoyance and discomfort or nervous system stimulation, activates the sympathic nervous system and endocrine system. Such reactions may result in an imbalance in homeostasis, thus promoting the development of hypertension [DEFRA, 2014; Basner et al., 2014; Babisch, 2011].
Research examining the relationship between occupational noise exposure and hypertension has largely relied on self-reported exposures, small samples sizes, and, until recently, cross sectional designs [Lang et al., 1992; Wu et al., 1987; Powazka et al., 2002; Gan et al., 2011; de Souza et al., 2015]. There has been less research using cohort designs where noise exposures are quantitatively estimated and disease status is assessed longitudinally to exclude prevalent cases. Two such studies, one of male sawmill workers and another of male aircraft manufacturing workers, reported statistically significant associations between cumulative noise exposure greater or equal to 85 dBA-years and risk of incident hypertension [Sbihi et al., 2008; Chang et al., 2013]. A meta-analysis conducted by van Kempen et al [2002] found a significant association between occupational noise exposure and hypertension; however, the authors made particular note of the contradictory nature of the studies included and warned that all studies included in that meta-analysis used a cross-sectional design. Stokholm et al [2013] followed 145,000 Danish industrial workers for 7 years and estimated their current and historical noise exposures based on a small sample of contemporary measurements. No increased risk of hypertension associated with increased noise exposure was observed among blue-collar industrial workers, though a significant difference in risk was observed between blue-collar and white-collar female workers. More recently, Liu et al [2016] examined both noise level and frequency in relation to incident hypertension and found that certain frequencies were positively and linearly associated with risk of hypertension. In addition, they detected a significant relationship between higher noise exposure levels and incident hypertension; however, the relationship lost significance after adjusting for multiple comparisons.
To help elucidate the relationship between occupational noise exposure and incident hypertension, we conducted a retrospective cohort study using quantitative noise exposure measurements, job information, and individual characteristics among white male manufacturing workers. We also controlled for baseline hearing ability, as well as annual rate of hearing loss, among cohort members in an attempt to adjust for the potential attenuation of noise exposure through hearing loss, and the effects of this attenuation on risk of incident hypertension.
Methods
Study Population
We selected an inception cohort consisting of hourly white, male employees at sixteen geographically diverse specialty metal manufacturing plants belonging to a single corporation in the United States. Manufacturing processes occurring at the plants included aluminum smelting, aluminum forging and casting, and the fabrication of aluminum and other light metals. An employee was included in the cohort if he was hired on or after January 1, 1996 (the date when data become available to the investigators), was employed for at least 2 years, and was in a job that required both noise exposure monitoring and regular audiometric testing. At least two audiograms were required during follow-up to assess both baseline hearing status and change in hearing status. Follow-up ended on December 31, 2012.
Data Sources
The present study is part of a longstanding relationship between the company and Yale and Stanford Universities, the goal of which is to improve health and safety outcomes for the workforce. Data were merged from several datasets annually received as part of this collaboration.
The human resources dataset provides date of birth, sex, ethnicity, plant location, hire date, termination date, job and department titles, as well as all dates pertinent to job changes, leave of absence, disability, layoff and retirement. With this data, we constructed job histories for each worker and calculated active person-time by job. Because of the large number of job titles used in the human resources database, the researchers (with guidance from a company industrial hygienist) collapsed similar jobs together into standardized job categories. This process allowed us to meaningfully account for task and physical demands of jobs that would not otherwise be captured [Taiwo et al., 2009; Cantley et al., 2016].
Personal dosimetry measurements are collected for each job for employees included in the noise surveillance program. The industrial hygiene dataset provides personal noise measurement data on all jobs for which exposures ever equal or exceed an 8-hour time-weighted average (TWA) of 82 dBA measured using the following criteria: 85 dBA TWA corporate exposure limit, 5 dB time-intensity exchange rate (i.e., the change in average exposure level required to halve or double the allowable exposure duration), SLOW time constant (i.e., 1-sec time weighting to smooth variability), and 80 dBA threshold (below which noise levels do not contribute to accumulate dose). Note that the exchange rate, time constant, and threshold are specified by the Occupational Safety and Health Administration (OSHA), and that the corporate exposure limit is identical to the OSHA Action Level for noise [Occupational Safety and Health Administration, 1983].
Using the standardized job categories, we matched employees in the human resources dataset to jobs present in the industrial hygiene dataset. With 9367 noise samples from 191 plant-job combinations that represented at least 75% of the job’s shift length, we calculated time-weighted noise exposure levels for each standardized job category in which the employee worked. To take into account any temporal changes in noise level by job, a regression line was fitted for each standardized job category for each year of the study. Noise level by year was assigned to each job based on the predicted value. Average noise levels (LOSHA) were calculated as follows:
where t is the time period for each of the n standardized job categories in which the employee worked, LA is the predicted noise level for the standardized job category for that time period, and T is the total duration worked. Exposure was considered as both a continuous and categorical measure; categories were designated as <82 dBA (referent), 82–84.99 dBA, 85–87.99 dBA, and >88 dBA. While the exchange rate used to measure noise exposures for this study was 5 dB (as specified by the corporate exposure limit and the OSHA Action Level), here we present results in 3 dB bins, where 3 dB step is equivalent to a doubling of noise intensity.
All employees in jobs where noise sampling occurs are automatically enrolled in the company’s hearing conservation program and receive periodic pure tone air conduction audiometric threshold testing at 0.5, 1, 2, 3, 4, and 6 kHz. Audiometric surveillance data were provided to us through the company’s occupational health database, which also includes employee body mass index (BMI) and smoking history. BMI was categorized as <25 (Normal), 25–29.9 (Overweight), and >30 (Obese). Hearing threshold levels were calculated by using the binaural average of hearing thresholds at the frequencies of 3 kHz, 4 kHz, and 6 kHz. Average annual rate of hearing threshold change and baseline hearing threshold values were included in the analysis. Hearing health questions asked during audiometric testing were also included in our analysis. These include: “Have you ever had noise in your ears?”, “Have you ever had noisy hobbies?”, “Did you ever shoot or hunt?”, “Do you presently have another noisy job?”, and “Have you ever had a noisy job?”.
Finally, medical claims are received annually from the company’s central data processing vendor for all employees participating in the company’s preferred provider insurance organization (>90% of the workforce). Data include International Classification of Diseases (ICD-9) codes for disease diagnosis and National Drug Codes (NDC) for prescription information. Fields include date of service, provider type, and provider location. A case was defined as anyone free of disease for at least the first two years of employment who was subsequently diagnosed with hypertension during an outpatient physician visit, emergency room visit, or inpatient admission. The ICD-9 codes used to define hypertension included 401: essential hypertension, 402: hypertensive heart disease, 403: hypertensive renal disease, and 404: hypertensive heart and renal disease.
Databases were linked using an encrypted unique identifier to ensure human subject protection, as we have done in previous analyses [Taiwo et al., 2009; Cantley et al., 2016; Pollack et al., 2007]. The Institutional Review Boards of Yale University and Stanford University approved the study protocols and written consent was waived as the research involved no more than minimal risk.
Statistical Analysis
Statistical analyses were performed using SAS version 9.3. (SAS Institute, Inc., Cary, NC). Descriptive statistics were calculated for the full cohort and by hypertensive disease status. Cox proportional hazards models were performed to determine the association of noise exposure with risk of incident hypertension. In order to ensure the proportionality assumption necessary to the Cox model, we constructed log-log survival plots. We first ran bivariate models assessing the impact of individual covariates on the risk of hypertension. Variables were carried into the final adjusted model if significance reached p≤0.10; noise exposure categories were forced into the model despite a lack of significance in the bivariate analysis. The final multivariate model was adjusted for age at baseline, body mass index, smoking history, baseline hearing threshold, average annual loss in hearing threshold, and annual wages. Random effects for job-within-plant and plant were included to account for clustering of workers and unmeasured factors within-job and within-plant. Interactions between noise exposure category and plant type (smelter vs fabrication) were explored, and a multivariate model including annual hearing loss as the primary predictor variable was also investigated. All p values were two sided and a value of less than α=0.05 was considered statistically significant.
Results
Among the 2052 employees identified as meeting the criteria for the inception cohort, there were 244 cases of incident hypertension over the study period, or 13.5% of the total cohort. Table 1 displays descriptive statistics for the cohort at baseline. The hypertension cases were older (39 vs 36 years), more likely to be overweight and obese (43% vs 39% and 48% vs 35%, respectively), and more likely to have ever smoked (48% vs 43%). Mean follow-up time was slightly longer for the cohort as a whole compared to cases (6.6 vs 5.9 years). Noise exposures between groups were similar in the reference and highest noise categories, higher for cases in the 82–84.99 dBA category, and lower for cases in the 85–87.99 dBA category. Baseline hearing threshold levels and annual rate of hearing loss were greater for cases. Figure 1 illustrates the variability of noise exposure by plant. Average noise exposure by job ranged from 54 to 97dBA.
Table 1.
Characteristics of inception cohort by disease status, 1996–2012
| Total Cohort N=2052 |
Cases of Hypertension n=244 |
|||||||
|---|---|---|---|---|---|---|---|---|
| N | % | Mean | SD | N | % | Mean | SD | |
| Age at baseline | 35.8 | 8.5 | 39.1 | 8.4 | ||||
| Follow-up time in years | 6.5 | 3.6 | 5.9 | 3.1 | ||||
| Body mass index, kg/m2 | ||||||||
| < 25 | 389 | 19.0 | 18 | 7.4 | ||||
| 25–29.9 | 801 | 39.0 | 106 | 43.4 | ||||
| >30 | 723 | 35.2 | 116 | 47.5 | ||||
| Unknown | 139 | 6.8 | 4 | 1.6 | ||||
| Smoking Status | ||||||||
| Ever | 890 | 43.4 | 117 | 48.0 | ||||
| Never | 658 | 32.1 | 80 | 32.8 | ||||
| Unknown | 504 | 24.6 | 47 | 19.3 | ||||
| Noise exposure (continuous) | 82.7 | 4.8 | 82.6 | 4.3 | ||||
| Noise exposure (categorized) | ||||||||
| < 82 dBA | 950 | 46.3 | 115 | 47.1 | ||||
| 82–84.99 dBA | 522 | 25.4 | 68 | 27.9 | ||||
| 85–87.99 dBA | 341 | 16.6 | 33 | 13.5 | ||||
| ≥ 88 dBA | 239 | 11.7 | 28 | 11.5 | ||||
| Baseline hearing threshold at 3, 4, 6 Khz | 18.0 | 14.6 | 22.4 | 16.5 | ||||
| Average loss in hearing threshold at 3, 4, 6 kHz by year (continuous) | 0.5 | 1.1 | 0.7 | 1.0 | ||||
| Annual wages in USD | 51047.3 | 13791.3 | 50734.9 | 12426.6 | ||||
| History of noise in ears | 544 | 27.8 | 75 | 30.7 | ||||
| History of noisy hobbies | 930 | 47.6 | 122 | 500 | ||||
| History of shooting or hunting | 1067 | 54.6 | 133 | 54.5 | ||||
| Currently has another noisy job | 621 | 31.7 | 72 | 29.5 | ||||
| Previously had a noisy job | 1067 | 53.8 | 153 | 62.7 | ||||
| Smelter | 731 | 35.6 | 78 | 32.0 | ||||
Figure 1.
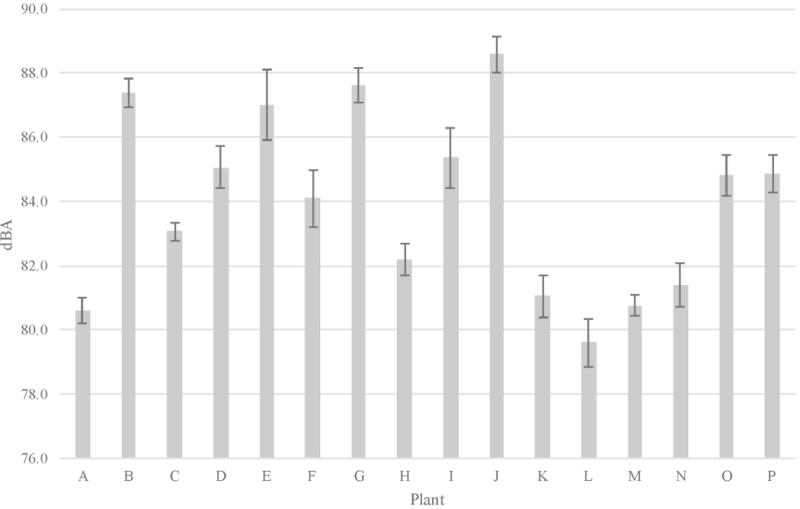
Average noise levels by plant with 95% CI
The adjusted hazard ratio (HR) of incident hypertension did not significantly differ between groups by cumulative continuous or categorized noise exposure metric (Model 1, Table 2). Increasing age and BMI were associated with greater HRs. Baseline hearing threshold and annual rate of hearing loss failed to emerge as predictors of hypertension despite early evidence of an effect in the bivariate analysis. Likewise, hearing health questions answered by each worker were not associated with any increases in HR for incident hypertension. An adjusted model exploring the possibility of hearing loss as an alternative and potentially more accurate estimate of in-ear noise exposure was performed (Model 2, Table 2). This model did not include noise exposure levels, but rather tested whether or not hearing loss may act as a proxy for noise exposure in a setting where adjustment for hearing protection was not possible. Hearing loss quintiles were not significantly associated with risk of hypertension. Additional adjustment for an interaction term between facility type and noise exposure showed no significant effect, nor did an adjusted model incorporating continuous noise exposure (data not shown).
Table 2.
Unadjusted and adjusted hazard ratios for risk of incident hypertension
| Bivariate Model | Adjusted Model 1a | Adjusted Model 2 a | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Age | 1.05 | 1.04–1.07 | 1.04 | 1.03–1.06 | 1.04 | 1.02–1.06 |
| Body mass index (<25=reference) | ||||||
| 25–29.9 | 2.81 | 1.71–4.64 | 2.79 | 1.68–4.61 | 2.79 | 1.69–4.63 |
| >30 | 4.08 | 2.49–6.71 | 4.36 | 2.63–7.22 | 4.34 | 2.62–7.19 |
| Unknown | 1.72 | 0.58–5.10 | 1.11 | 0.35–3.47 | 1.04 | 0.33–3.27 |
| Smoking Status (Never=reference) | ||||||
| Ever | 1.22 | 0.92–1.62 | 1.25 | 0.93–1.67 | 1.20 | 0.89–1.61 |
| Unknown | 1.46 | 1.01–2.11 | 1.53 | 1.03–2.29 | 1.48 | 0.99–2.21 |
| Noise exposure (continuous) | 1.00 | 0.98–1.03 | – | – | ||
| Noise exposure (< 82dBA=reference) | ||||||
| 82–84.99 dBA | 1.02 | 0.76–1.38 | 1.01 | 0.70–1.45 | – | |
| 85–87.99 dBA | 0.97 | 0.66–1.43 | 1.01 | 0.63–1.61 | – | |
| ≥ 88 dBA | 0.95 | 0.63–1.44 | 0.98 | 0.58–1.65 | – | |
| Baseline average hearing threshold at 3, 4, 6 kHz | 1.02 | 1.01–1.02 | 1.01 | 1.00–1.02 | 1.01 | 1.00–1.01 |
| Average annual loss in hearing threshold at 3, 4, 6 kHz | 1.21 | 1.07–1.37 | 1.09 | 0.94–1.26 | – | |
| Average annual loss in hearing threshold at 3, 4, 6 kHz categorized (Quintile 1=reference) | ||||||
| Quintile 2 | 0.81 | 0.51–1.28 | – | 0.75 | 0.47–1.20 | |
| Quintile 3 | 0.92 | 0.59–1.43 | – | 0.91 | 0.58–1.44 | |
| Quintile 4 | 0.83 | 0.52–1.31 | – | 0.68 | 0.43–1.10 | |
| Quintile 5 | 1.82 | 1.20–2.77 | – | 1.35 | 0.87–2.10 | |
| Annual wages, per 10,000 USD | 0.88 | 0.79–0.99 | 0.83 | 0.73–0.93 | 0.83 | 0.73–0.93 |
| History of noise in ears | 0.89 | 0.68–1.17 | – | – | ||
| History of noisy hobbies | 1.11 | 0.86–1.43 | – | – | ||
| History of shooting or hunting | 0.94 | 0.73–1.22 | – | – | ||
| Currently has another noisy job | 0.93 | 0.71–1.23 | – | – | ||
| Previously had a noisy job | 1.17 | 0.89–1.52 | – | – | ||
| Worked in smelter | 0.93 | 0.71–1.22 | – | – | ||
Random effects included for job category and plant location
Discussion
We found no association between occupational noise exposure and risk of incident hypertension in an inception cohort of white male manufacturing workers employed by a single US company. In addition, our final multivariate model failed to show an association between either baseline hearing threshold level or annual change in hearing threshold level and the risk of hypertension, although it might reasonably be expected that reduced noise exposures resulting from hearing loss could influence risk of hypertension. To this end, we modeled the risk of hypertension excluding noise exposure but including hearing loss as our primary predictor while also adjusting for all demographic and job level variables; this analysis also showed no association with risk of hypertension.
This study had a number of strengths. Our unique access to both individual- and job-level variables allowed us to construct a job-weighted noise exposure metric while also controlling for known risk factors of hypertension, including age, body mass index, economic status, and job category. We have previously shown that a single medical claim for hypertension is a highly specific measure of case ascertainment [Tessier-Sherman et al., 2013]. Further, by excluding medication usage from our case definition, we limited the likelihood of disease misclassification, as the medications used to treat hypertension are widely used in cardiac care. Finally, by restricting our analysis to a single company with well-established occupational health and medical data collection procedures, we minimized the likelihood of potential biases in such data due to between-company differences.
The research on occupational noise exposure and risk of hypertension, much of which has been cross-sectional in nature, has yielded inconsistent results [Lang et al., 1992; de Souza et al., 2015; Chang et al., 2003; Lusk et al., 2004]. Two recent longitudinal studies found conflicting results: Chang et al [2013] conducted a prospective cohort study in 578 male Taiwanese aircraft manufacturing employees where hypertension was defined using physician diagnoses and blood pressure measurements. When all cases of hypertension were analyzed together, they found a dose-response relationship between noise and hypertension; however, when looking only at those cases defined as hypertensive through physician records, a statistically significant association was not found. The large prospective cohort study by Stokholm [2013] used a cohort of both industrial and financial sector employees and found no effect of noise on hypertension in men, though an effect was noted between white collar and blue collar women.
Conversely, the research examining community noise exposure and hypertension has largely shown a positive association, whether the source of the noise is an airport or road traffic [Ndrepepa and Twardella, 2011; Babisch and Kamp, 2009; Gan et al., 2012]. In light of this incongruence, it seems plausible that community noise and occupational noise may have inherently different effects on our bodies. The primary biologic mechanism espoused for the posited relationship between noise and hypertension is the stimulation of the sympathic nervous system and the resulting loss of equilibrium. However, one of the primary theorized triggers for this biologic response is disturbance and annoyance during sleep, the time when the body recovers from the mental and physical burden of the day. If this is accurate, then ambient noise may only have a pathophysiologic effect during times of rest, rather than during the typical demands of work life [van Kempen, 2002].
There are a number of limitations to this study. First, despite the potentially important effects of hearing protection devices (HPDs) on noise-related health outcomes, we did not have individual-level information regarding the use of HPDs, and therefore had no ability to account for or estimate any HPD-related attenuation of noise exposure [Lusk et al., 2012]. If employees in the highest noise exposure category used HPDs more often than those in lower noise categories, an increased hazard ratio might be expected among workers in lower exposure groups. Such an increase was seen in previous work investigating the relationship between hearing loss and occupational noise exposure in a similar cohort [Rabinowitz et al., 2007]. Our findings did not show a relationship between noise exposure and hypertension among any of the noise exposure groups, suggesting either that use of hearing protection may not be an effect modifier, or that there is such substantial misclassification of exposures due to lack of information on HPD use that our statistical power to detect an association is significantly degraded, or that use of HPDs was sufficient in all exposure groups to reduce in-ear exposure to a level low enough to avoid any cardiovascular effects of noise.
The second limitation relates to the nature of the exposure metric and the limited follow-up period. Because only 20% of our cohort had mean noise exposures ≥85dBA, it is possible that if a relationship between occupational noise and hypertension exists, our exposures were not high enough to detect such an effect. Davies reported an association only for those exposed to >92dBA [Davies et al., 2005]. It is also possible that the cumulative average exposure modeled for workers in this study did not adequately capture the variable nature of occupational noise in the facilities studied. If cardiovascular effects of occupational noise are related to stress and annoyance, the temporal and spatial variability of noise exposure could be an important factor in determining risk of hypertension. In this case, estimation of peak exposures, or of intermittency of exposures – measures not available in the dataset used for this analysis, but proposed for use in epidemiological studies [Seixas et al., 2005] – could have yielded different results. Further, because we chose an inception cohort with the intent of limiting the healthy worker survivor effect, our mean follow-up period was 6.5 years. Two studies that reported positive associations between noise exposure levels and hypertension may have benefitted from employment durations between 8 and 15 years [Chang et al., 2013; Liu et al., 2016].
The third limitation of the study is the potential for survivor bias. We considered whether or not survivor bias could have a role in our results as those most sensitive to noise and thus susceptible to disease may have either changed jobs or left the company within our 2 year washout period. We examined the employee population excluded from our cohort and compared them to those who remained. Mean hearing loss levels were comparable between groups, suggesting that the likelihood of this type of bias was low.
The final limitation relates to our ability to control for other factors known to be associated with risk of hypertension. We did not have information available on our participants regarding participation in regular exercise, salt intake, or other factors that increase the risk of developing hypertension. We were able to control for annual income, which may have partially controlled for socioeconomic status and, by proxy, some of these risk factors. However, it is possible that the potential confounding effects of some of these other unmeasured risk factors influenced our results.
Conclusions
To our knowledge, this is the first study investigating the relationship between occupational noise and hypertension that used hypertension incidence rather than prevalence and that had access to a substantial database of quantitative noise exposure measurements. For workers with similar occupational noise exposures and follow-up, our findings suggest that such exposure is not associated with the risk of hypertension, with the important caveat that use of HPDs, an important factor in estimating exposures to noise, could not be considered in our models.
Acknowledgments
Funding: This research was funded by grants from the National Institute on Aging (Disease, Disability and Death in an Aging Workforce, NIH/NIA, 1 R01 AG026291-06 - Current): BTS, LFC, DG, MRC; National Institute for Occupational Health and Safety (Assessing hearing conservation effectiveness, 1 R01 OH010132-01 - Past): LFC, DG, PMR, RLN; and a contract with Alcoa Inc (Current at the time this research was initiated).
Footnotes
Authors’ contributions: In the preparation of this manuscript, BTS, RLN, and PMR conceived of and developed the study design. DG and BTS conducted the data analysis, and BTS, LFC, RLN, MRC and PMR participated in data interpretation and drafting the final paper. All authors are accountable for all aspects of the research presenting in this manuscript.
Institution and Ethics approval and informed consent: The work presented in this manuscript was conducted at the Yale University School of Medicine, with approval from the Yale University School of Medicine Human Investigations Committee. Informed consent was waived as the research involved no more than minimal risk.
Disclosure (Authors): Until spring 2016, BTS, LFC, DG, and MRC received a portion of their compensation at Yale and Stanford through a long-standing contractual agreement with Alcoa, Inc. None of the funding sources had any decision-making authority over the design, analysis, written description or publication with regard to the study described in this manuscript.
Disclaimer: None
Data sharing: As an alternative to providing a de-identified data set to the public domain, we allow access for the purpose of re-analyses or appropriate “follow-on” analyses by any qualified investigator willing to sign a contractual covenant with the host Institution limiting use of data to a specific agreed upon purpose.
References
- Babisch W, van Kamp I. Exposure-Response Relationship of the Association between Aircraft Noise and the Risk of Hypertension. Noise Health. 2009;11(44):161–168. doi: 10.4103/1463-1741.53363. [DOI] [PubMed] [Google Scholar]
- Babisch W. Cardiovascular Effects of Noise. Noise Health. 2011;13(52):201–204. doi: 10.4103/1463-1741.80148. [DOI] [PubMed] [Google Scholar]
- Babisch W. Updated Exposure-Response Relationship between Road Traffic Noise and Coronary Heart Diseases: A Meta-Analysis. Noise Health. 2014;16(68):1–9. doi: 10.4103/1463-1741.127847. [DOI] [PubMed] [Google Scholar]
- Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. Auditory and Non-Auditory Effects of Noise on Health. Lancet. 2014;383(9925):1325–1332. doi: 10.1016/S0140-6736(13)61613-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantley LF, Tessier-Sherman B, Slade MD, Galusha D, Cullen MR. Expert Ratings of Job Demand and Job Control as Predictors of Injury and Musculoskeletal Disorder Risk in a Manufacturing Cohort. Occup Environ Med. 2016;73:229–236. doi: 10.1136/oemed-2015-102831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Workplace Health Promotion: Blood Pressure Screening and Control [Internet] Atlanta, GA. [updated 2014 Feb 27; cited 2016 Mar 9]. Available from: http://www.cdc.gov/workplacehealthpromotion/evaluation/topics/blood-pressure.html.
- Chang T-Y, Jain R-M, Wang C-S, Chan C-C. Effects of Occupational Noise Exposure on Blood Pressure. J Occup Environ Med. 2003;45(12):1289–1296. doi: 10.1097/01.jom.0000100003.59731.3d. [DOI] [PubMed] [Google Scholar]
- Chang T-Y, Hwang BF, Liu CS, Chen RY, Wang VS, Bao BY, et al. Occupational Noise Exposure and Incident Hypertension in Men: A Prospective Cohort Study. Am J Epidemiol. 2013;177(8):818–825. doi: 10.1093/aje/kws300. [DOI] [PubMed] [Google Scholar]
- Davies HW, Teschke K, Kennedy SM, Hodgson MR, Hertzman C, Demers PA. Occupational Exposure to Noise and Mortality From Acute Myocardial Infarction. Epidemiology. 2005;16(1):25–32. doi: 10.1097/01.ede.0000147121.13399.bf. [DOI] [PubMed] [Google Scholar]
- DEFRA (Department of Environment, Food and Rural Affairs) Environmental Noise:Valuing Impacts on: Sleep Disturbance, Annoyance, Hypertension, Productivity and Quiet. 2014 [cited 2016 Mar 9]. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/380852/environmental-noise-valuing-imapcts-PB14227.pdf.
- de Souza TCF, Périssé ARS, Moura M. Noise Exposure and Hypertension: Investigation of a Silent Relationship. BMC Public Health. 2015;15:328. doi: 10.1186/s12889-015-1671-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eriksson C, Rosenlund M, Pershagen G, Hilding A, Östenson CG, Bluhm G. Aircraft Noise and Incidence of Hypertension. Epidemiology. 2007;18(6):716–721. doi: 10.1097/EDE.0b013e3181567e77. [DOI] [PubMed] [Google Scholar]
- Gan WQ, Davies HW, Demers PA. Exposure to Occupational Noise and Cardiovascular Disease in the United States: The National Health and Nutrition Examination Survey 1999–2004. Occup Environ Med. 2011;68(3):183–190. doi: 10.1136/oem.2010.055269. [DOI] [PubMed] [Google Scholar]
- Gan WQ, Davies HW, Koehoorn M, Brauer M. Association of Long-Term Exposure to Community Noise and Traffic-Related Air Pollution With Coronary Heart Disease Mortality. Am J Epidemiol. 2012;175(9):898–906. doi: 10.1093/aje/kwr424. [DOI] [PubMed] [Google Scholar]
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart Disease and Stroke Statistics—2013 Update A Report From the American Heart Association. Circulation. 2013;127(1):e6–245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansell AL, Blangiardo M, Fortunato L, Floud S, de Hoogh K, Fecht D, et al. Aircraft Noise and Cardiovascular Disease near Heathrow Airport in London: Small Area Study. BMJ. 2013;347:f5432. doi: 10.1136/bmj.f5432. [DOI] [PubMed] [Google Scholar]
- Lang T, Fouriaud C, Jacquinet-Salord M-C. Length of Occupational Noise Exposure and Blood Pressure. Int Arch Occ Env Hea. 1992;63(6):369–372. doi: 10.1007/BF00386929. [DOI] [PubMed] [Google Scholar]
- Liu CS, Young LH, Yu TY, Bao BY, Chang TY. Occupational Noise Frequencies and the Incidence of Hypertension in a Retrospective Cohort Study. American Journal of Epidemiology. 2016;184(2):120–8. doi: 10.1093/aje/kwv333. [DOI] [PubMed] [Google Scholar]
- Lusk SL, Gillespie B, Hagerty BM, Ziemba RA. Acute Effects of Noise on Blood Pressure and Heart Rate. Arch Environ Health. 2004;59(8):392–99. doi: 10.3200/AEOH.59.8.392-399. [DOI] [PubMed] [Google Scholar]
- Lusk SL, Hagerty BM, Gillespie B, Caruso CC. Chronic Effects of Workplace Noise on Blood Pressure and Heart Rate. Arch Environ Health. 2012;57(4):273–281. doi: 10.1080/00039890209601410. [DOI] [PubMed] [Google Scholar]
- Münzel T, Gori T, Babisch W, Basner M. Cardiovascular effects of environmental noise exposure. European heart journal. 2014;35(13):829–36. doi: 10.1093/eurheartj/ehu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2014: With Special Feature on Adults Aged 55–64. 2015 Hyattsville, MD. [cited 2016 Mar 9]. Available from: http://www.cdc.gov/nchs/data/hus/hus14.pdf#059. [PubMed]
- Ndrepepa A, Twardella D. Relationship between Noise Annoyance from Road Traffic Noise and Cardiovascular Diseases: A Meta-Analysis. Noise Health. 2011;13(52):251–259. doi: 10.4103/1463-1741.80163. [DOI] [PubMed] [Google Scholar]
- Occupational Safety and Health Administration. Occupational Noise Exposure; Hearing Conservation Amendment. Fed Regist. 1983;48(46):9738–9783. [Google Scholar]
- Pollack KM, Sorock GS, Slade MD, Cantley LF, Sircar K, Taiwo O, et al. Association between Body Mass Index and Acute Traumatic Workplace Injury in Hourly Manufacturing Employees. Am J Epidemiol. 2007;166(2):204–11. doi: 10.1093/aje/kwm058. [DOI] [PubMed] [Google Scholar]
- Powazka E, Pawlas K, Zahorska-Markiewicz B, Zejda JE. A Cross-Sectional Study of Occupational Noise Exposure and Blood Pressure in Steelworkers. Noise Health. 2002;5(17):15–22. [PubMed] [Google Scholar]
- Rabinowitz PM, Galusha D, Dixon‐Ernst C, Slade MD, Cullen MR. Do Ambient Noise Exposure Levels Predict Hearing Loss in a Modern Industrial Cohort? Occup Environ Med. 2007;64(1):53–59. doi: 10.1136/oem.2005.025924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenlund M, Berglind N, Pershagen G, Järup L, Bluhm G. Increased Prevalence of Hypertension in a Population Exposed to Aircraft Noise. Occup Environ Med. 2001;58(12):769–773. doi: 10.1136/oem.58.12.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sbihi H, Davies HW, Demers PA. Hypertension in Noise-Exposed Sawmill Workers: A Cohort Study. Occup Environ Med. 2008;65(9):643–646. doi: 10.1136/oem.2007.035709. [DOI] [PubMed] [Google Scholar]
- Seixas N, Neitzel R, Sheppard L, Goldman B. Alternative Metrics for Noise Exposure Construction Workers. Ann Occup Hyg. 2005;49(6):493–502. doi: 10.1093/annhyg/mei009. [DOI] [PubMed] [Google Scholar]
- Sørensen M, Andersen ZJ, Nordsborg RB, Jensen SS, Lillelund KG, Beelen R, et al. Road Traffic Noise and Incident Myocardial Infarction: A Prospective Cohort Study. PLoS ONE. 2012;7(6):e39283. doi: 10.1371/journal.pone.0039283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokholm ZA, Bonde JP, Christensen KL, Hansen AM, Kolstad HA. Occupational Noise Exposure and the Risk of Hypertension. Epidemiology. 2013;24(1):135–142. doi: 10.1097/EDE.0b013e31826b7f76. [DOI] [PubMed] [Google Scholar]
- Swinburn TK, Hammer MS, Neitzel RL. Valuing Quiet: An Economic Assessment of U.S. Environmental Noise as a Cardiovascular Health Hazard. Am J Prev Med. 2015;49(3):345–353. doi: 10.1016/j.amepre.2015.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taiwo OA, Cantley LF, Slade MD, Pollack KM, Vegso S, Fiellin MG, et al. Sex Differences in Injury Patterns Among Workers in Heavy Manufacturing. Am J Epidemiol. 2009;169(2):161–166. doi: 10.1093/aje/kwn304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tessier-Sherman B, Galusha D, Taiwo O, Cantley LF, Slade MD, Kirsche SL, et al. Further Validation That Claims Data Are a Useful Tool for Epidemiologic Research on Hypertension. BMC Public Health. 2013;13:51. doi: 10.1186/1471-2458-13-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Kempen E, Kruize H, Boshuizen HC, Ameling CB, Staatsen BAM, de Hollander AEM. The Association between Noise Exposure and Blood Pressure and Ischemic Heart Disease: A Meta-Analysis. Environ Health Persp. 2002;110(3):307–317. doi: 10.1289/ehp.02110307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Kempen E, Babisch W. The Quantitative Relationship between Road Traffic Noise and Hypertension: A Meta-Analysis. J Hypertens. 2012;30(6):1075–1086. doi: 10.1097/HJH.0b013e328352ac54. [DOI] [PubMed] [Google Scholar]
- Willich SN, Wegscheider K, Stallmann M, Keil T. Noise Burden and the Risk of Myocardial Infarction. Eur Heart J. 2006;27(3):276–282. doi: 10.1093/eurheartj/ehi658. [DOI] [PubMed] [Google Scholar]
- Wu T-N, Ko Y-C, Chang P-Y. Study of Noise Exposure and High Blood Pressure in Shipyard Workers. Am Ind Med. 1987;12(4):431–438. doi: 10.1002/ajim.4700120408. [DOI] [PubMed] [Google Scholar]


