Abstract
Background:
Dural arteriovenous fistulas (DAVF) are unusual intracranial vascular malformations consisting of anomalous connections between meningeal arteries and dural sinuses or the veins that pass through them. They have variable clinical presentation and prognosis, which depend on their location and venous hemodynamics. Treatment is based on the closure of the abnormal connections, which is usually conducted via arterial and/or transvenous endovascular techniques.
Case Description:
We present a male patient who complained of headaches and left-sided pulsatile tinnitus due to DAVF from the external carotid artery branches draining directly into the ipsilateral sigmoid sinus. Embolization with Onyx® was successful, obtaining angiographic occlusion and symptom remission. However, on postoperative day 4, the patient presented with left facial palsy and spontaneous regression.
Conclusion:
Although embolization is an effective and safe procedure, complications may occur. Reflux of the embolic agent to the vasa nervorum of the cranial nerve may lead to ischemic neuropathy. Here, we reported a case of embolized DAVF presenting with a postoperative peripheral facial palsy where the two embolized pedicles were branches of the middle meningeal and occipital arteries involved in the vascularization of the extratemporal segment of the facial nerve. We discuss the etiopathogenic, anatomical, and pathophysiological aspects of this complication.
Keywords: Arteriovenous fistula, central nervous system vascular malformations, facial paralysis, intracranial arteriovenous malformations, therapeutic embolization, vasa nervorum
INTRODUCTION
Dural arteriovenous fistulas (DAVF) consist of abnormal connections between vascular structures within the dural space. These fistulas are uncommon, representing only 10–15% of intracranial cerebral vascular malformations.[3,6] Embolization with sclerosing material of DAVF is a well-established procedure that facilitates surgery by reducing blood flow and may lead to complete healing.[3] The aim of this report was to present a case of DAVF treated with embolization by Onyx® (EV3, Irvine, CA, USA), a nonadhesive blend of an ethylene-vinyl alcohol copolymer with a solvent, dimethyl sulfoxide, plus a radiopaque contrast agent (tantalum powder), who developed transient facial paralysis, as well as to review the literature and discuss the neuroanatomical etiology and pathophysiology of this complication.
CASE REPORT
A 57-year-old male presented with 3 months of left pulsatile tinnitus and hemicranial headache without any other neurological deficits. He had no history of head trauma or central nervous system infections. Digital subtraction angiography revealed DAVF with afferents from the left external carotid artery (LECA), notably with the occipital and middle meningeal arteries draining into the ipsilateral sigmoid sinus, without leptomeningeal cortical retrograde venous drainage, and grade I of the Cognard classification [Figure 1].
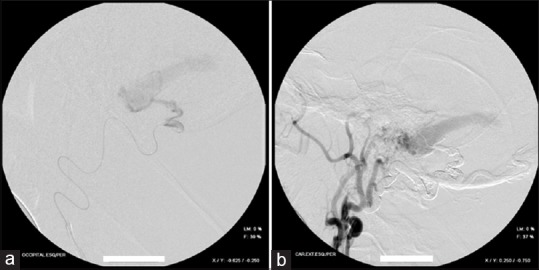
Figure 1.

DSA profile view showing FAVD supplied by branches of the LECA and direct drainage into the sigmoid sinus
The transvenous approach was chosen, together with closure of the affected sinus using coils, but the surgical team experienced difficulties when passing the microcatheter from the transverse to the sigmoid sinus, which was likely isolated. Thus, two sessions of transarterial embolization were performed 2 months apart [Figure 2]. During the first session, the fistulous branch of the left occipital artery was occluded with Onyx® [Figure 3a and b]. The patient recovered uneventfully and tinnitus decreased, although headaches persisted. During the second session conducted with Onyx®, the feeder branch of the left middle meningeal artery was occluded [Figure 4a and b]. Angiography revealed complete exclusion of the fistula and successful embolization [Figure 5]. On the first day postoperatively, the patient presented with ipsilateral peripheral facial palsy, House Brackmann grade 4 [Figure 6], and no other physical or neurological signs. Tomography showed no ischemic or hemorrhagic complications [Figure 7]. The patient received 4 mg of intravenous dexamethasone every 6 h and showed progressive improvement with complete recovery in 4 days [Figure 8]. After 4 months, the patient remains under our care, with no complaints of headache or tinnitus. A follow-up appointment is scheduled for 6 months after his last session.
Figure 2.

Unsuccessfully attempt of embolization through transvenous approach due to left sigmoid sinus isolated
Figure 3.
(a) Selective micro catheterization of the left occipital artery showing the fistulous point. (b) Final control of the first session, after embolization of the left occipital artery
Figure 4.
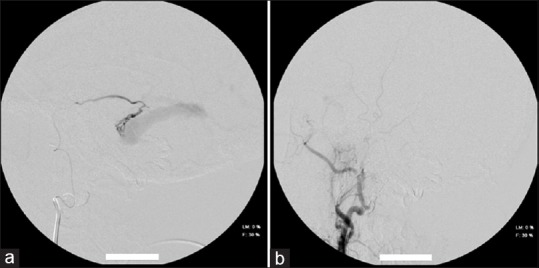
(a) Selective micro catheterization of the left middle meningeal artery showing the fistulous point. (b) Final control of the second session, after embolization of the left middle meningeal artery
Figure 5.
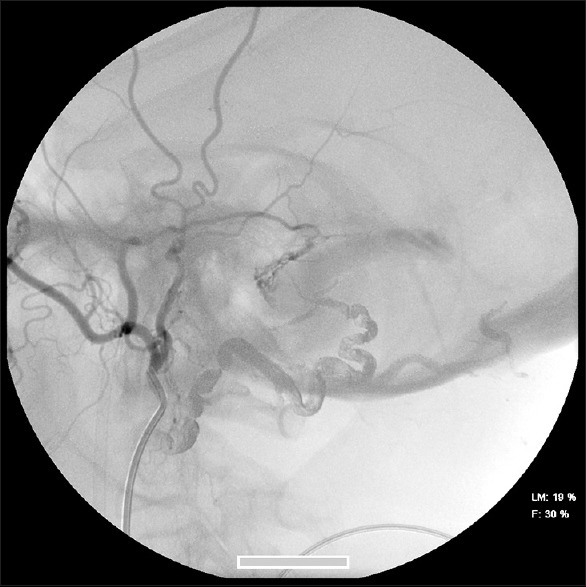
DSA final control, showing complete closure of FAVD by Onyx
Figure 6.

Left peripheral facial palsy House-Brackmann grade 4 on the first postoperative day
Figure 7.

Computed tomography image (axial view) showing large amount of artifact corresponding to Onyx in the embolized vessels in close proximity to the facial nerve route (opacities at the left side)
Figure 8.

Spontaneous resolution of peripheral facial paralysis after 4 days of embolization
DISCUSSION
Understanding the facial nerve's vascularization is essential for understanding the current case report. The facial nerve (cranial nerve VII) is a mixed nerve with predominantly motor fibers that divide into supranuclear, nuclear, and infranuclear paths.[7]
Infranuclearly, vascularization is provided by the carotid and vertebrobasilar arterial systems.[7] In the internal auditory canal, the meatal segment is fed by the labyrinthine branch terminals of the anterior inferior cerebellar artery. Thus, the six infranuclear segments receive irrigation from the following arteries:
Petrous artery: branch of the middle meningeal artery that penetrates the temporal bone, irrigating the region of the geniculate ganglion, tympanic segment, and part of the labyrinth;
Stylomastoid artery: usually a branch of the occipital artery. It enters the stylomastoid foramen upwardly and is responsible for supplying this region's mastoid segment and facial nerve branches, thus contributing to the vascularization of the tympanic segment.[5,7]
In this report, we presented a case of DAVF treated with embolization by Onyx® who developed transient facial paralysis. It should be noted that in the present case, the DAVF received afferents from the LECA, especially the middle and occipital meningeal arteries. The most likely cause of the facial palsy was Onyx®'s unintended penetration of the vasa nervorum of the facial nerve, yet without irreversible disruption of the vascularization.
Partial or even complete deficits of the cranial nerve are expected to occur following the use of temporary embolic agents such as polyvinyl alcohol or Gelfoam.[1] More durable materials such as cyanoacrylate derivatives may cause permanent dysfunction. Because Onyx® is a permanent embolic agent with a low recanalization rate, cranial nerve deficits caused by its use have a poorer prognosis than those caused by temporary embolic agents.[1]
Six different published case reports of facial paralysis following transarterial embolization with Onyx® support this observation.[1,2,3,4,5,6]
In one of these case studies, magnetic resonance imaging and histopathology revealed the presence of Onyx® in the intramastoidal facial canal, with obliteration of the lumen of the vasa nervorum and necrosis of the vessel wall.[3] In another case, the patient experienced contralateral facial palsy after embolization, and the presence of Onyx® was detected through intraoperative tomography. Also, electromyography showed a loss of facial nerve function. In both cases, paralysis was permanent, even after surgical decompression.[6]
CONCLUSION
Embolization of dural arteriovenous fistulas with Onyx® is an effective and safe procedure. However, it requires good knowledge of neuroanatomical vascularization of the cranial nerves, as well as the utmost care during the procedure. Although rare, an inadvertent penetration of the embolic agent into the surrounding vessels of the facial nerve sheath can cause ischemia and direct nerve compression.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Luana Antunes Maranha Gatto, Email: luanamaranha@yahoo.com.br.
Fernando Saurin, Email: ferando_saurin@live.com.
Gelson Luis Koppe, Email: koppe@bighost.com.
Zeferino Demartini, Junior, Email: demartiniz@gmail.com.
REFERENCES
- 1.Gartrell BC, Hansen MR, Gantz BJ, Gluth MB, Mowry SE, Aagaard-Kienitz BL, et al. Facial and lower cranial neuropathies after preoperative embolization of jugular foramen lesions with ethylene vinyl alcohol. Otol Neurotol. 2012;33:1270–5. doi: 10.1097/MAO.0b013e31825f2365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gaynor BG, Elhammady MS, Jethanamest D, Angeli SI, Aziz-Sultan MA. Incidence of cranial nerve palsy after preoperative embolization of glomus jugulare tumors using Onyx. J Neurosurg. 2014;120:377–81. doi: 10.3171/2013.10.JNS13354. [DOI] [PubMed] [Google Scholar]
- 3.Kupfer TJ, Aumann K, Laszig R, Meckel S. Periphere Fazialisparese nach Onyx®-Embolisation einer duralen arteriovenösen Fistel. HNO. 2011;59:465–9. doi: 10.1007/s00106-011-2297-9. [DOI] [PubMed] [Google Scholar]
- 4.Lv X, Jiang C, Zhang J, Li Y, Wu Z. Complications related to percutaneous transarterial embolization of intracranial dural arteriovenous fistulas in 40 patients. AJNR Am J Neuroradiol. 2009;30:462–8. doi: 10.3174/ajnr.A1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ozanne A, Pereira V, Krings T, Toulgoat F, Lasjaunias P. Arterial vascularization of the cranial nerves. Neuroimaging Clin N Am. 2008;18:431–9. doi: 10.1016/j.nic.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 6.Ozluoglu LN, Koycu A, Jafarov S, Hizal E, Boyvat F. Facial palsy following embolization of a dural arteriovenous fistula. Eur Arch Otorhinolaryngol. 2016;273:2843–6. doi: 10.1007/s00405-015-3772-9. [DOI] [PubMed] [Google Scholar]
- 7.Tobin CE. Injection method to demonstrate blood supply of nerves. Anat Rec. 1943;87:341–4. [Google Scholar]


