Abstract
Background:
The success of hip surgery in treating acetabular retroversion depends on the severity of the structural deformity and on selecting the correct patient for open or arthroscopic procedures.
Purpose:
To compare a group of patients with retroverted hips treated successfully with hip arthroscopy with a group of patients with retroverted hips that failed arthroscopic surgery, with special emphasis on (1) patient characteristics, (2) perioperative radiographic parameters, (3) intraoperative findings and concomitant procedures, and (4) patient sex.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
We retrospectively reviewed the charts of 47 adult patients (47 hips) with acetabular retroversion who had undergone hip arthroscopy. Retroversion was based on the presence of an ischial spine sign in addition to either a crossover or posterior wall sign on a well-positioned anteroposterior pelvic radiograph. A total of 24 hips (50%) (16 females, 8 males; mean patient age, 31 years) had failed arthroscopy, defined as modified Harris Hip Score (mHHS) <80 or need for subsequent procedure. Twenty-three hips (8 females, 15 males; mean patient age, 29 years) were considered successful, defined as having no subsequent procedures and an mHHS >80 at the time of most recent follow-up. Perioperative variables, radiographic characteristics, and intraoperative findings were compared between the groups, in addition to a subgroup analysis based on sex.
Results:
The mean follow-up for successful hips was 30 months (SD, 11 months), with a mean mHHS of 95. In the failure group, 6 patients required subsequent procedures (4 anteverting periacetabular osteotomies and 2 total hip arthroplasties). The mean overall time to failure was 21 months, and the mean time to a second procedure was 24 months (total hip arthroplasty, 29.5 months; periacetabular osteotomy, 21.2 months); 18 hips failed on the basis of a low mHHS (mean, 65; range, 27-79) at last follow-up. Factors significantly different between the success and failure groups included patient sex, with males being more likely than females to have a successful outcome (P < .02), as well as undergoing femoral osteoplasty (P < .02). Intraoperative variables that were associated with worse outcome included isolated labral debridement (P < .002). In a subgroup analysis, males were more likely than their female counterparts to have a successful outcome with both isolated cam and combined cam-pincer resection (P < .05). Level of crossover correction on postoperative radiographs had no correlation with outcome.
Conclusion:
Acetabular retroversion remains a challenging pathoanatomy to treat arthroscopically. If hip arthroscopy is to be considered in select cases, we recommend labral preservation when possible. Male patients with correction of cam deformities did well, while females with significant retroversion appeared to be at greater risk for failure of arthroscopic treatment.
Keywords: hip, hip arthroscopy, FAI, retroversion
Hip arthroscopy for the treatment of acute and chronic chondrolabral pathology and femoroacetabular impingement (FAI) has gained in popularity over the past decade, providing a reliable, minimally invasive method of addressing potentially joint-threatening conditions.1 Proponents of the technique cite equivalent outcomes as compared with open procedures for the treatment of pain attributed to bony impingement,2 as well as excellent pain relief and return to function for patients treated for a variety of intra-articular conditions.3
While the correlation between acetabular retroversion and anterior impingement has been clearly described,4 the implication of hip arthroscopy in the setting of underlying dysmorphic acetabulae is not fully understood. It has been suggested that special care be taken for patients with a posterior wall sign (ie, posterior undercoverage), as anterior acetabular rim trimming causes global acetabular undercoverage that may lead to iatrogenic instability. In the presence of these radiographic findings, an anteverting periacetabular osteotomy has been recommended, with significant improvement in clinical outcomes scores.11 In addition, the structurally abnormal acetabulum may be associated with other abnormalities, such as abnormal femoral version or morphology5,6 or anterior inferior spine overhang, leading to subspine impingement that may be inadvertently overlooked as a cause of pain. Such concomitant pathology could lead to poor outcomes when arthroscopic procedures cannot address or fail to address the associated structural findings.
The success of hip surgery in treating acetabular retroversion depends on the severity of the structural deformity and relies on correct patient triage to open or arthroscopic procedures. The purpose of this study was to compare the group of hips treated with successful arthroscopy with a group of hips that failed arthroscopic surgery, with special emphasis on (1) patient characteristics, (2) perioperative radiographic parameters, (3) intraoperative findings and concomitant procedures, and (4) patient sex. We hypothesized that patients who failed hip arthroscopy will have undergone more extensive labral and acetabular resection when compared with retroverted patients with successful arthroscopic outcomes.
Methods
This study was approved by an institutional review board and included the retrospective review of patients evaluated between January 2009 and February 2013 by 1 of 3 hip arthroscopy-trained surgeons (R.J.S., A.J.K., B.A.L.) at the Mayo Clinic. Included were all skeletally mature patients with acetabular retroversion, defined as the presence of an ischial spine sign, as well as a crossover sign and/or posterior wall sign on a well-centered anteroposterior pelvis radiograph with adequate tilt and rotation,8 as evaluated by 2 independent orthopaedic surgeons (K.L.P., A.J.K.). Patients were excluded if they had any radiographic evidence of dysplasia (defined by Tönnis angle >12° and lateral center-edge angle <24°), protrusio or profunda, or if they had any prior trauma or surgery to the hip. A total of 77 patients were identified. Of these, 12 were excluded because of concomitant acetabular dysplasia, 8 for prior hip surgery, 6 because of follow-up <6 months and the absence of failure, and 4 for declining to participate in research activities. The remaining 47 patients with acetabular retroversion who had undergone hip arthroscopy at our institution (46) or elsewhere (1) for treatment of hip impingement were included in this study.
Surgical Technique
Surgical technique involved standard supine positioning on a table, allowing for distraction across the hip. A standard mobile C-arm unit was used, and all images were taken by a certified radiograph technician under the direction of the operative surgeon. Preoperative views included anteroposterior pelvis and hip; 45° Dunn view; lateral, internal, and external rotation views to isolate the optimum view of the cam lesion (if applicable); and a final anteroposterior pelvis view after traction had been applied to ensure distractibility of the joint. With distraction applied, an anterolateral portal was first established under fluoroscopic guidance and a 70° arthroscope introduced. Accessory working portals were created under direct visualization dependent on the pathology to be addressed. Arthroscopic images documented the integrity of the acetabular and femoral articular cartilage and were used by the reviewers in determining the Beck cartilage classification for each case. Acetabular osteoplasty, labral debridement, and/or repair was performed as indicated, with the latter performed according to the integrity of the tissue and the size and thickness of the tear as it was assessed intraoperatively. Traction was released and the integrity of the labral seal assessed. Under fluoroscopic guidance, the cam lesion, if present, was identified and resected. The patient was placed in a hip abduction orthosis postoperatively.
Rehabilitation
Patients were treated with a comprehensive 5-phase rehabilitation protocol. Hip braces were not used postoperatively. Patients were kept partial weightbearing for 4 weeks utilizing crutches. Gentle range-of-motion exercises were initiated early in the postoperative period, and use of an exercise bike was introduced in the first 2 weeks following surgery. Patients progressed to jogging at 3 months and unrestricted activity at 6 months.
Data Collection
Patients were divided into 2 groups: success and failure. Patients were considered a “failure” if they had 1 of the following at the time of most recent follow-up: a postoperative modified Harris Hip Score (mHHS)9 <80 or a subsequent procedure (repeat hip arthroscopy, periacetabular osteotomy, or hip arthroplasty). All others were considered “success” at final follow-up.
Patient charts were reviewed for baseline characteristics and operative procedures performed. Age and sex were recorded, but body mass index and activity level were not consistently available. The intraoperative arthroscopic images were reviewed by a single reviewer, and cartilage damage was graded according to the Beck cartilage classification (grade 1, normal; grade 2, chondromalacia; grade 3, debonding; grade 4, cleavage; grade 5, full-thickness defect).19 Pre- and postarthroscopy radiographic measurements were recorded with computer-assisted calculation tools by 2 independent reviewers. These values included Tönnis grade of osteoarthritis, alpha angle, Tönnis or roof angle and lateral center-edge angle, femoral head-neck offset, crossover sign, and ischial spine signs, all per previously described methods.10,24 The change from pre- to postoperative measurements was also calculated for radiographic parameters affecting acetabular coverage (lateral center-edge and Tönnis angles).
Patients were observed until last clinical review or until a subsequent procedure was performed. An mHHS was performed on all patients at the latest follow-up to determine the degree of success of the arthroscopic procedure.
Statistical Analysis
The analysis focused on comparing the cohort of 24 patients who underwent hip arthroscopy and failed (failure defined by a subsequent procedure or low functional outcome) with a cohort of 23 patients who underwent hip arthroscopy with a minimum follow-up of 1 year and were considered successful. Patient outcomes included a comparison of pre- and postoperative radiographic parameters, as well as intraoperative findings and procedures performed. Patient demographics, baseline clinical data, surgical factors, and patient outcomes that are measured on a continuous scale, such as time from injury to surgery, length of procedure, and months to failure, were compared with 2-sample t tests or nonparametric Wilcoxon rank-sum tests. Demographics, baseline and surgical data, and outcomes defined as binary or multilevel categorical variables, such as type of surgery, change in radiographic measurements, procedure performed, and intraoperative complications, were evaluated with chi-square tests. If differences in patient demographics, baseline data, or surgical factors were identified, the study outcomes were analyzed with multivariable models to adjust for the between-groups differences. All statistical tests were 2-sided, and P values <.05 were considered significant.
Results
There was no baseline difference in age (mean, 30.4 years; range, 14-57 years) between the groups; however, there were more females in the failure group (16 vs 8) (P < .02).
Of the 47 hips included in the study, 24 (51%) were considered failures. Of these, 6 patients required subsequent procedures (4 anteverting periacetabular osteotomies and 2 total hip arthroplasties). The mean overall time to failure was 21 months (range, 11-48 months). The mean time to a second procedure was 24 months (29.5 months to total hip arthroplasty and 21.2 months to periacetabular osteotomy). Eighteen hips failed on the basis of a low mHHS (mean, 65; range, 27-79) but no subsequent procedure at last follow-up. The mean follow-up for the success group was 30 months (range, 12-47 months), and the mean mHHS at most recent follow-up was 95 (range, 81-100).
Radiographic Measurements
Preoperative radiographic measurements showed the mean alpha, neck-shaft, and center-edge angles were similar between the groups. Although the difference did not reach statistical difference, successful patients had larger preoperative Tönnis angles (6.5° vs 4.9°, P = .083), although all the angles were very similar. All patients with a preoperative crossover sign had one postoperatively as well. Postoperatively, there was no difference in mean alpha, center-edge, or Tönnis angle (Table 1). When the difference between pre- and postoperative measurements was compared, there was a larger decrease in center-edge angle in the failures (–3.1° vs –2.1° for successes), although this again did not reach statistical significance (P = .086).
TABLE 1.
Pre- and Postoperative Radiographic Parametersa
| Preoperative | Postoperative | |||||
|---|---|---|---|---|---|---|
| Failure (n = 24) | Success (n = 23) | P Value | Failure (n = 24) | Success (n = 23) | P Value | |
| Alpha angle, deg | .3052b | .9624c | ||||
| Mean ± SD | 61.8 ± 12.6 | 62.0 ± 11.2 | 53.8 ± 16.2 | 58.2 ± 11.1 | ||
| Range | 34.0-94.5 | 39.9-85.0 | 30.0-78.0 | 38.0-77.0 | ||
| Femoral neck shaft angle, deg | .6938b | |||||
| Mean ± SD | 133.6 ± 5.7 | 132.9 ± 5.3 | ||||
| Range | 120.0-144.0 | 124.0-141.4 | ||||
| Positive sign, No. (%) | ||||||
| Posterior wall | 10 (41.67) | 14 (58.33) | .1880c | |||
| Ischial spine | 24 (51.06) | 23 (48.94) | NA | |||
| Crossover | 20 (50.00) | 20 (50.00) | >.999b | 20 (50.00) | 20 (50.00) | >.999b |
| Center-edge angle, deg | .2041b | .5103c | ||||
| Mean ± SD | 32.6 ± 5.5 | 30.4 ± 6.0 | 29.5 ± 6.0 | 28.3 ± 5.9 | ||
| Range | 25.0-43.1 | 24.0-43.0 | 18.0-41.0 | 17.0-38.0 | ||
| Tönnis angle, deg | .0828b | .0088c | ||||
| Mean ± SD | 4.9 ± 3.3 | 6.5 ± 2.7 | 4.4 ± 4.4 | 7.8 ± 4.2 | ||
| Range | 0.0-10.8 | 1.9-11.0 | 0.0-19.0 | 0.0-15.0 | ||
aReport generated on March 20, 2015. NA, not applicable.
bFisher exact test.
cUnequal variance t test.
Surgical Procedures
With regard to procedures performed at the time of surgery, patients who failed were more likely to undergo labral debridement (P < .002), either in isolation or in combination with other procedures. However, when this was separated into patients who underwent isolated labral debridement (no acetabular bony work and no labral repair), the difference between the groups did not reach statistical significance. Those with successful outcomes were also more likely to undergo femoral osteoplasty (58% success vs 41% fail) (P < .02), either in isolation or in combination with other labral procedures. There was no difference between groups with regard to labral repairs, acetabular osteoplasty, or whether a psoas release was performed (Table 2).
TABLE 2.
Surgical Procedures Performeda
| Failure (n = 24) | Success (n = 23) | P Value | |
|---|---|---|---|
| Labral debridement | .0022b | ||
| No | 7 (29.17) | 17 (70.83) | |
| Yes | 17 (73.91) | 6 (26.09) | |
| Labral repair | .7918b | ||
| No | 6 (54.55) | 5 (45.45) | |
| Yes | 18 (50.00) | 18 (50.00) | |
| Femoral osteoplasty | .0197b | ||
| No | 9 (81.82) | 2 (18.18) | |
| Yes | 15 (41.67) | 21 (58.33) | |
| Acetabular chondroplasty | .0959b | ||
| No | 19 (59.38) | 13 (40.63) | |
| Yes | 5 (33.33) | 10 (66.67) | |
| Femoral chondroplasty | .6662c | ||
| No | 22 (52.38) | 20 (47.62) | |
| Yes | 2 (40.00) | 3 (60.00) | |
| Acetabular osteoplasty | .0918b | ||
| No | 12 (66.67) | 6 (33.33) | |
| Yes | 12 (41.38) | 17 (58.62) | |
| Psoas | .6662c | ||
| No | 22 (52.38) | 20 (47.62) | |
| Yes | 2 (40.00) | 3 (60.00) |
aReport generated on March 20, 2015. Values are presented as No. (%).
bChi-square test.
cFisher exact test.
Cartilage Damage
Grading of the acetabular cartilage according to the Beck cartilage classification at the time of arthroscopy showed no statistically significant differences between the groups with regard to mean score and to those with a score ≥4 versus ≤3 (P > .3).
Sex-Based Differences
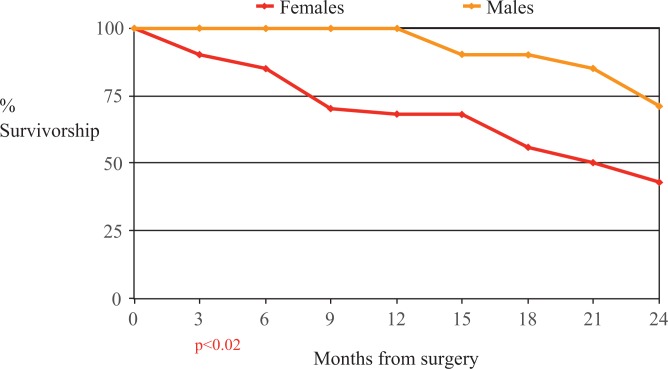
A subgroup analysis based on patient sex found no difference in the percentage of males treated with femoral osteoplasty for cam lesions (19 of 23, 82%) when compared with females (19 of 24, 79%). However, males who underwent femoral osteoplasty did significantly better than females undergoing femoral osteoplasty (79% success vs 43% success) (P < .05). Additionally, of the 11 males and 12 females who underwent both femoral osteoplasty and acetabular osteoplasty, 90% of males were considered a success versus only 40% of females (P < .03). There was no significant difference in the number of males or females undergoing acetabular osteoplasty or in their outcomes (Table 3). A Kaplan-Meier analysis showed increased survivorship among males at both 1 year (100% vs 68%) and 2 years (72% vs 44%) postoperatively (P < .02) (Figure 1).
TABLE 3.
Sex-Based Differencesa
| Male (n = 23) | Female (n = 24) | P Valueb | |
|---|---|---|---|
| Femoral osteoplasty | .317 | ||
| Yes | 19 (82) | 16 (66) | |
| No | 4 (17) | 8 (33) | |
| Outcome femoral osteoplasty | .042 | ||
| No. | 19 | 16 | |
| Success | 15 (79) | 7 (43) | |
| Fail | 4 (21) | 9 (56) | |
| Femoral + acetabular osteoplasty | >.999 | ||
| Yes | 11 (47) | 12 (50) | |
| No | 12 (52) | 12 (50) | |
| Outcome femoral + acetabular osteoplasty | .027 | ||
| No. | 11 | 12 | |
| Success | 10 (90) | 5 (41) | |
| Fail | 1 (10) | 7 (58) | |
| Mixed | 0 (0.00) | 1 (100.00) |
aReport generated on March 20, 2015. Values are presented as No. (%).
bFisher exact test.
Figure 1.
Kaplan-Meier survivorship analysis by sex for all procedures.
Discussion
Based on its less invasive nature, hip arthroscopy is often better accepted by patients and surgeons over open procedures when attempting to address the symptoms of FAI.18 However, hip arthroscopy has significant limitations and is often unable to address all the potential variables associated with the structural deformity. Still, many patients with acetabular retroversion and posterior undercoverage undergo successful hip arthroscopy, which suggests that certain patient characteristics may be associated with better outcomes. We found that males with cam pathology were more likely than their female counterparts to have a successful outcome in the setting of acetabular retroversion.
In our consecutive series, 50% of patients with acetabular retroversion were considered failures. While these data were coming from a tertiary referral center, only 1 patient had the index hip arthroscopy at an outside facility; therefore, this remains an unacceptably high failure rate. Nearly half of patients (24 of 47) met the criteria for an anteverting periacetabular osteotomy as described by Siebenrock et al23—a procedure with documented favorable long-term follow-up—yet all were first referred for arthroscopy. This led us to question which quantifiable variables could be identified preoperatively to guide the surgeon toward the most appropriate treatment. Unfortunately, no significant differences were seen in radiographic parameters, either preoperatively or postoperatively, suggesting that radiographic analysis alone is not sufficient to determine outcome. However, those with a successful outcome were more likely to undergo cam resection, and of those, males were more likely to have a successful outcome. When contrasted with the equivocal outcome among patients undergoing isolated pincer resection, this may suggest that resecting the cam can decompress the anterior hip, thereby decreasing the need for rim resection, which leads to successful results, particularly in males.
Overall, this series showed fairly poor results for the arthroscopic treatment of patients with acetabular retroversion. A previous study suggested satisfactory short- and midterm outcomes with the arthroscopic treatment of FAI.23 While these authors included patients with acetabular retroversion as an underlying source of pincer impingement, they lacked subset analysis of their individual performance. A study that focused on the implications of version reported less significant improvements in mHHS with femoral, not acetabular, retroversion.6 Others have warned against the arthroscopic management of acetabular retroversion in the setting of concomitant dysplasia,7,20 citing the potential for iatrogenic instability.
Sex-based differences in FAI have been well documented in the literature, in terms of pathoanatomy and patient outcomes,12,13 with cam lesions being more common in athletic males14 and symptomatic pincer lesions (largely those attributed to protrusio) thought to be more common in middle-aged women.15 None of the patients in our study had radiographic evidence of protrusio, suggesting that all pincer lesions came from anterosuperior overcoverage because of retroversion. A recent computed tomography study of 878 acetabulae in males and females showed no difference in the prevalence of retroversion or anterior overcoverage in females,21 suggesting that the symptomatology of FAI, not the actual underlying structural deformity, may be what drives these sex-based differences. Similarly, Hetsroni et al12 performed a retrospective computed tomography study of 249 hips with symptomatic FAI and found that females had more anteverted acetabulae and smaller alpha angles than their male counterparts. Our results showed that while the numbers of males and females undergoing isolated cam or combined cam-pincer resections were not significantly different, males were more likely to have a successful outcome with both procedures and had longer 2-year survival. Several variables not included in the analysis could have influenced the failure rates, including femoral version, overall laxity, and subclinical instability. Indeed, female sex has been associated with higher rates of ligamentous laxity and instability after hip arthroscopy for FAI.26
Interestingly, the status of the cartilage at the time of arthroscopy did not affect the ultimate outcome, which contrasts with previously reported studies on the significance of acetabular chondral defects and their association with inferior outcomes.25 Note, however, that all patients had preserved joint space with Tönnis arthritis grade 0-1 and thus remained candidates for hip arthroscopy. Longer term follow-up would more adequately determine the significance of these cartilage lesions. Also, the Beck classification includes chondrolabral delamination, and the presence of a cam lesion causing chondrolabral delamination was a positive variable in this study and therefore may be a confounding factor.
The strength of this study includes its very strict definition of failure, including mHHS <80, and comparison of 2 groups of patients. Recently published literature suggests that an mHHS of 74 at 1 year from arthroscopic surgery for FAI correlated with a patient-perceived “satisfactory outcome” as it related to one’s daily function, pain, and return to activity.22 Nonetheless, this study was not without limitations. First, this was a retrospective review subject to the availability of documentation. Given that the operative reports did not consistently document closure of the capsulotomy (as was not the practice at the time), this variable was omitted from analysis and may have played a significant role in patient outcome. This may also contribute to the increased failure seen in patients with labral debridement, as patients—particularly females with baseline soft tissue laxity—may have been better served by procedures to improve the soft tissue stability around the hip.16,17 In addition, the retrospective nature did not allow for preoperative baseline scores. Therefore, we did not have the change in pre- to postoperative scores for this patient population. Finally, while a number of radiographic parameters were included, calculation of the retroversion index could have quantified the proportion of retroversion as a percentage26 and further enhanced understanding of the implications of severity of retroversion as it related to outcomes. Ultimately, owing to the retrospective nature of the study and the limitations in statistical analysis, no definite recommendations can be made based on the outcomes presented. Rather, we present these data to contribute to the overall understanding of the implications of retroversion on outcomes in hip arthroscopy.
Conclusion
Hip pain in the context of FAI with acetabular retroversion remains a complex entity. While our results suggest that males, particularly those with FAI containing a significant cam component, do better than their female counterparts, a host of corresponding variables must ultimately be considered, including femoral version, pelvic parameters, preoperative symptomatology, and surgeon skill.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the Mayo Clinic Institutional Review Board (application 14-003899).
References
- 1. Aprato A, Jayasekera N, Villar RN. Does the modified Harris Hip Score reflect patient satisfaction after hip arthroscopy? Am J Sports Med. 2012;40(11):2557–2560. [DOI] [PubMed] [Google Scholar]
- 2. Büchler L, Neumann M, Schwab JM, Iselin L, Tannast M, Beck M. Arthroscopic versus open cam resection in the treatment of femoroacetabular impingement. Arthroscopy. 2013;29(4):653–660. [DOI] [PubMed] [Google Scholar]
- 3. Chahal J, Van Thiel GS, Mather RC, 3rd, et al. The patient acceptable symptomatic state for the modified Harris Hip Score and Hip Outcome Score among patients undergoing surgical treatment for femoroacetabular impingement. Am J Sports Med. 2015;42(8):1844–1849. [DOI] [PubMed] [Google Scholar]
- 4. Clohisy JC, Baca G, Beaulé PE, et al. ; ANCHOR Study Group. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med. 2013;41(6):1348–1356. [DOI] [PubMed] [Google Scholar]
- 5. Clohisy JC, Carlisle JC, Beaulé PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(suppl 4):47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Crockarell J, Jr, Trousdale RT, Cabanela ME, Berry DJ. Early experience and results with the periacetabular osteotomy: the Mayo Clinic experience. Clin Orthop Relat Res. 1999;(363):45–53. [PubMed] [Google Scholar]
- 7. Domb BG, Philippon MJ, Giordano BD. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: relation to atraumatic instability. Arthroscopy. 2013;29(1):162–173. [DOI] [PubMed] [Google Scholar]
- 8. Fabricant PD, Fields KG, Taylor SA, Magennis E, Bedi A, Kelly BT. The effect of femoral and acetabular version on clinical outcomes after arthroscopic femoroacetabular impingement surgery. J Bone Joint Surg Am. 2015;97(7):537–543. [DOI] [PubMed] [Google Scholar]
- 9. Frank RM, Lee S, Bush-Joseph CA, Kelly BT, Salata MJ, Nho SJ. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42(11):2634–2642. [DOI] [PubMed] [Google Scholar]
- 10. Gupta A, Redmond JM, Stake CE, Dunne KF, Domb BG. Does primary hip arthroscopy result in improved clinical outcomes? 2-year clinical follow-up on a mixed group of 738 consecutive primary hip arthroscopies performed at a high-volume referral center. Am J Sports Med. 2016;44(1):74–82. [DOI] [PubMed] [Google Scholar]
- 11. Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92(14):2436–2444. [DOI] [PubMed] [Google Scholar]
- 12. Hetsroni I, Dela Torre K, Duke G, Lyman S, Kelly BT. Sex differences of hip morphology in young adults with hip pain and labral tears. Arthroscopy. 2013;29(1):54–63. [DOI] [PubMed] [Google Scholar]
- 13. Jackson TJ, Lindner D, El-Bitar YF, Domb BG. Effect of femoral anteversion on clinical outcomes after hip arthroscopy. Arthroscopy. 2015;31(1):35–41. [DOI] [PubMed] [Google Scholar]
- 14. Joseph R, Pan X, Cenkus K, Brown L, Ellis T, Di Stasi S. Sex differences in self-reported hip function up to 2 years after arthroscopic surgery for femoroacetabular impingement. Am J Sports Med. 2016;44(1):54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kahn M, Habib A, de Sa D, et al. Arthroscopy up to date: hip femoroacetabular impingement. Arthroscopy. 2016;32(1):177–189. [DOI] [PubMed] [Google Scholar]
- 16. Montgomery SR, Ngo SS, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. 2013;29(4):661–665. [DOI] [PubMed] [Google Scholar]
- 17. Nehme A, Trousdale R, Tannous Z, Maalouf G, Puget J, Telmont N. Developmental dysplasia of the hip: is acetabular retroversion a crucial factor? Orthop Traumatol Surg Res. 2009;95(7):511–519. [DOI] [PubMed] [Google Scholar]
- 18. Nepple JJ, Larson CM, Smith MV, et al. The reliability of arthroscopic classification of acetabular rim labrochondral disease. Am J Sports Med. 2012;40(10):2224–2229. [DOI] [PubMed] [Google Scholar]
- 19. Peters CL, Erickson JA, Anderson L, Anderson AA, Weiss J. Hip-preserving surgery: understanding complex pathomorphology. J Bone Joint Surg Am. 2009;91(suppl 6):42–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Poh SY, Hube R, Dienst M. Arthroscopic treatment of femoroacetabular pincer impingement. Oper Orthop Traumatol. 2015;27(6):536–552. [DOI] [PubMed] [Google Scholar]
- 21. Saadat E, Martin SD, Thornhill TS, Brownlee SA, Losina E, Katz JN. Factors associated with the failure of surgical treatment for femoroacetabular impingement: review of the literature. Am J Sports Med. 2014;42(6):1487–1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Siebenrock KA, Schaller C, Tannast M, Keel M, Büchler L. Anteverting periacetabular osteotomy for symptomatic acetabular retroversion: results at ten years. J Bone Joint Surg Am. 2014;96(21):1785–1792. [DOI] [PubMed] [Google Scholar]
- 23. Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion: treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85(2):278–286. [DOI] [PubMed] [Google Scholar]
- 24. Tannast M, Hanke MS, Zheng G, Steppacher SD, Siebenrock KA. What are the radiographic reference values for acetabular under- and overcoverage? Clin Orthop Relat Res. 2015;473(4):1234–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tannenbaum EP, Zhang P, Maratt JD, et al. A computed tomograph study of gender differences in acetabular version and morphology: implications for femoroacetabular impingement. Arthroscopy. 2015;21(7):124–154. [DOI] [PubMed] [Google Scholar]
- 26. Yeung M, Memon M, Simunovic N, Belzile E, Philippon MJ, Ayeni OR. Gross instability after hip arthroscopy: an analysis of case reports evaluating surgical and patient factors. Arthroscopy. 2016;32(6):1196–1204.e1. [DOI] [PubMed] [Google Scholar]