Abstract
Human immunodeficiency virus (HIV) and hepatitis C virus (HCV) infection are common in the criminal justice system. We offered opt-out HIV/HCV testing at the Dallas County Jail during intake from June 2015 to November 2016, after which testing was integrated into routine phlebotomy processes. The uptake of testing increased from 12.9% (118/915) in June 2015 to 80.5% (269/334) in January 2016. HIV was confirmed in 1.0% (30/3155) of inmates; 6 were new diagnoses and all were linked to care. HCV antibody positivity was found in 16.4% (500/4042) of inmates. Sixty percent (155/258) of HCV-positive inmates born between 1945 and 1965 (ie, baby boomers) were non-Hispanic black, whereas 56.2% (136/242) born after 1965 were non-Hispanic white. Testing only baby boomers would have missed approximately half of HCV infections, predominantly among young, non-Hispanic white people. Future efforts should expand HIV and HCV testing in jails, as it is feasible, acceptable, and increases prevention and engagement in care for a high-prevalence, hard-to-reach population.
Keywords: health disparities, hepatitis C virus, HIV/AIDS, incarceration, opt-out, testing
The burden of human immunodeficiency virus (HIV) and hepatitis C virus (HCV) is substantially higher among those who are incarcerated than among the general US population.1 In 2008, 1.5% of the US custody population had HIV (>3 times higher than among the general population), and 12.0% to 35.0% of the US custody population had HCV (up to 10 times higher than among the general population).2,3 Furthermore, incarcerated people are less likely than the general population to access routine medical care before or after incarceration,4,5 leading to worse individual outcomes and increased risk of HIV and HCV transmission to others. Incarceration therefore provides a unique opportunity for screening, engagement in care, treatment, and secondary prevention of these infections.
Although the Centers for Disease Control and Prevention recommends routine opt-out HIV testing in correctional facilities, only 19% of US prisons and 35% of US jails provide this service.3 Similarly, the World Health Organization recommends that all inmates be tested for HCV; however, only 17 US states perform routine HCV screening in prison.6,7 Currently, HCV screening in the United States focuses primarily on adults in the general population born between 1945 and 1965 (ie, baby boomers). Although several studies have shown the feasibility of routine testing for HIV and HCV in correctional facilities,8,9 few models for real-world implementation and acceptability of opt-out HIV or HCV screening exist.
In 2015, we initiated an opt-out HIV/HCV testing program at the Dallas County Jail. Our study objectives were to (1) describe the uptake of HIV/HCV opt-out testing for inmates entering jail, (2) determine the prevalence of HIV and HCV in this population, and (3) describe the demographic characteristics of the Dallas County Jail study sample with HIV or HCV.
Data and Methods
Opt-out HIV/HCV testing was offered to inmates entering the Dallas County Jail beginning in June 2015. Before this date, HIV testing had been offered through targeted opt-in screening by outside agencies, and HIV and HCV screening was available by inmate request. Opt-out testing was initially offered during the intake process at the same time as tuberculosis skin testing; however, in November 2015, testing was offered with any scheduled blood draw. With the implementation of this change, the study phlebotomist was integrated into the general phlebotomy team and all phlebotomists began offering HIV/HCV testing. Under this system, inmates were informed that HIV/HCV screening tests were routinely performed for all blood draws, unless the inmate declined the test (ie, opt-out method). This study was determined to be exempt by the University of Texas Southwestern Institutional Review Board.
Testing was performed using a fourth-generation antigen/antibody test for HIV (LabCorp Laboratories, Redmond, WA) and an HCV antibody assay (BioRad Laboratories, Hercules, CA). The rate of uptake (ie, the number of tests completed divided by the number of tests offered) was recorded from June 2015, when the testing program began, through January 2016, when the number of tests offered was no longer recorded. All other data were collected from June 2015 through June 2016. We calculated the positivity rate (ie, the number of positive tests divided by the number of tests completed) and tabulated data on demographic characteristics (sex, race/ethnicity, and age) from information in electronic health records. For those who tested positive for HIV, we assessed the risk factors for HIV acquisition, engagement in care (defined as being seen by an HIV provider in the 6 months before incarceration), reengagement in care (defined as receipt of HIV care during incarceration), and whether the person was newly or previously diagnosed with HIV. In addition, we determined from medical records whether or not the patient had been prescribed antiretroviral therapy and if the patient had an undetectable HIV ribonucleic acid viral load (<200 copies/mL). For all those testing HCV antibody positive, we determined prior seropositivity by chart review. We examined cross-tabular frequencies to explore differences between age groups and racial/ethnic groups. We used SAS version 9.4 for all analyses.10
Results
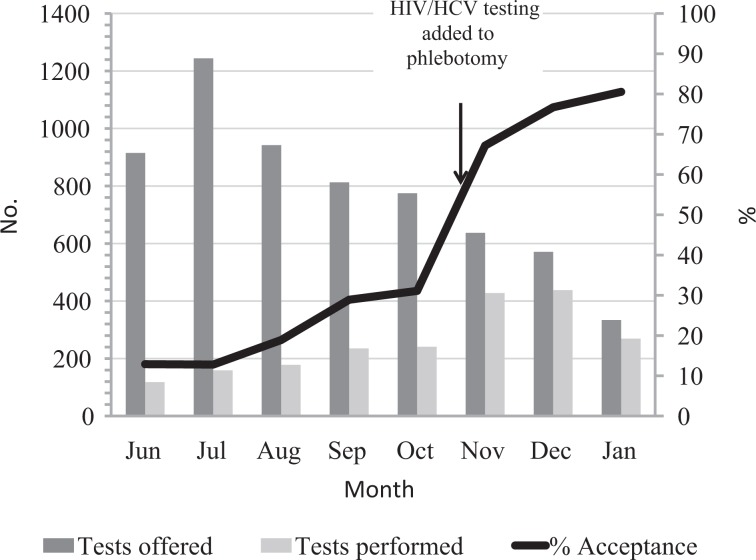
The acceptance rate of HIV/HCV testing increased from 12.9% (118 tests completed of 915 tests offered) in June 2015 to 80.5% (269 tests completed of 334 tests offered) in January 2016. Although the number of inmates who were offered testing declined over time, from a mean of 1033 per month in June 2015 to 514 per month in January 2016, the number of tests performed increased from a mean of 151 tests per month (during June–August 2015) to 378 tests per month (from November 2015 through January 2016) (Figure 1). Most inmates (3042/3155, 96.4%) accepted testing for both HIV and HCV; 45 of 3155 (1.4%) declined HCV testing because they already knew their HCV status, and an additional 68 of 3155 (2.1%) were not offered HCV testing because the test was not available at that time.
Figure 1.
Number of human immunodeficiency virus (HIV) and hepatitis C virus (HCV) tests offered and completed among inmates at the Dallas County Jail, June 2015 to January 2016.
During the study period, of 3155 HIV screening tests performed, 41 inmates (1.3%) tested positive. Of these, 11 were false positives (positive fourth-generation antigen/antibody test and negative HIV-1/HIV-2 antibody differentiation assay): 8 had a negative HIV nucleic acid amplification test and 3 had an insufficient sample to be tested. Of the 30 true positives, 6 were newly diagnosed, and all 30 inmates were linked to care during and after incarceration. Of the 6 newly diagnosed inmates, the median (standard deviation) age was 27 (10.4), all were men, 4 were non-Hispanic black, and 4 reported heterosexual risk only (Table). Among the 24 inmates previously known to have HIV infection who were retested during this study, 6 were not engaged in care before incarceration, but 18 were linked back to care during incarceration and treated with antiretroviral therapy. Of the 18 linked back to care, 6 were released before the jail clinic appointment.
Table.
Demographic and clinical characteristics of HIV-infected inmates (n = 30) identified through opt-out HIV testing at Dallas County Jail, June 2015 to July 2016
| Characteristic | New Diagnosis (n = 6) | Previously Known Diagnosisa (n = 24) |
|---|---|---|
| Age, mean (SD) | 27.0 (10.4) | 38.9 (12) |
| Sex | ||
| Male | 6 | 21 |
| Female | 0 | 3 |
| Race/ethnicity | ||
| Non-Hispanic white | 1 | 4 |
| Non-Hispanic black | 4 | 17 |
| Hispanic | 1 | 3 |
| Risk factorb | ||
| Injection drug use | 0 | 2 |
| Heterosexual | 4 | 14 |
| Men who have sex with men | 2 | 13 |
| Unknown | — | 1 |
| Undetectable viral loadc | ||
| Yes | 0 | 6 |
| No | 6 | 15 |
| Unknown | — | 3 |
| Using antiretroviral therapyd | ||
| Yes | 3 | 18 |
| No | 3 | 5 |
| Unknown | — | 1 |
| HCV antibody positive | ||
| Yes | 0 | 6 |
| No | 6 | 16 |
| Unknown | — | 2 |
| Engaged in care before incarceratione | ||
| Yes | — | 14 |
| No | — | 6 |
| Unknown | — | 4 |
| Engaged in care during incarceratione | ||
| Yes | 6 | 18 |
| No | 0 | 6 |
| Unknown | — | — |
| Engaged in care after incarceratione | ||
| Yes | 6 | 9 |
| No | 0 | 8 |
| Unknown | — | 7f |
Abbreviations: —, no data were collected; HCV, hepatitis C virus; HIV, human immunodeficiency virus.
aA known diagnosis is a previously documented HIV infection in jail electronic medical records.
bInmates could report multiple risk factors.
c<200 copies/mL.
dAntiretroviral therapy was initiated, continued, or restarted while incarcerated.
eEngagement in care is any clinic visit with a medical provider during a 6-month period.
fSix patients were scheduled to follow up with clinics outside the jail system.
In addition, 3042 inmates were tested for HCV, and 500 (16.4%) inmates had a positive HCV antibody screening test; of these, 215 (43.0%) were non-Hispanic white, 210 (42.0%) were non-Hispanic black, and 75 (15.0%) were Hispanic. HCV prevalence differed by race/ethnicity: of inmates who tested HCV antibody positive, 210 of 937 (22.4%) were non-Hispanic white, 210 of 1527 (13.8%) were non-Hispanic black, and 80 of 578 (13.8%) were Hispanic. Of the 500 inmates who tested HCV antibody positive, the mean age was 49, 402 (80.4%) were men, 177 (35.4%) had previously documented HCV antibody positivity, and 258 (51.6%) were baby boomers.
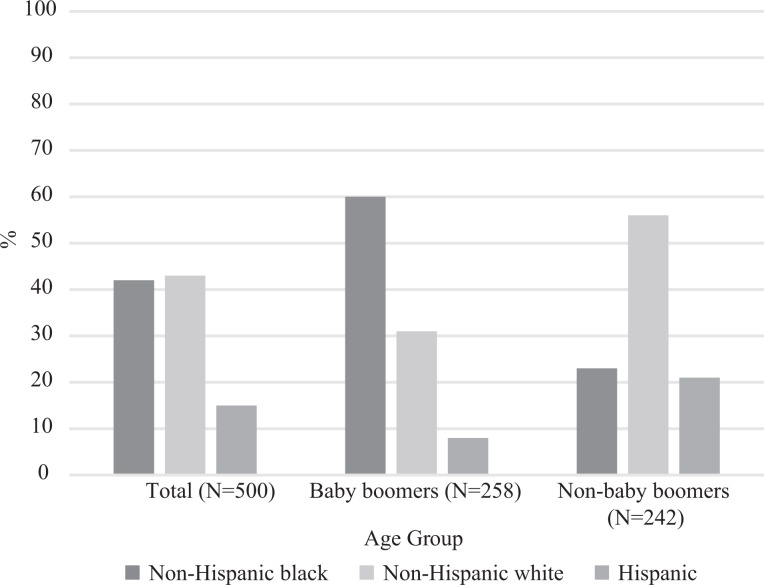
The HCV antibody positivity rate among baby boomers was 40.6% (258/636) and among non–baby boomers was 10.1% (242/2406). More patients in the non–baby boomer cohort than in the baby boomer cohort were tested for HCV (2406 vs 636). When stratified by age and race/ethnicity, 60.0% (155/258) of those who were HCV antibody positive in the baby boomer cohort were non-Hispanic black, whereas 56.2% (136/242) of those who were HCV antibody positive in the non–baby boomer cohort were non-Hispanic white (Figure 2). Similarly, when comparing baby boomers with non–baby boomers, the prevalence of HCV antibody positivity varied by race/ethnicity: 39.9% (155/388) versus 4.8% (55/1139), respectively, among non-Hispanic black inmates, 44.7% (80/179) versus 17.2% (130/758) among non-Hispanic white inmates, and 33.3% (23/69) versus 11.2% (57/509) among Hispanic inmates.
Figure 2.
Hepatitis C antibody-positive inmates, by racial/ethnic group and age cohort, Dallas County Jail, June 2015 to January 2016. Baby boomers are those born between 1945 and 1965. Non–baby boomers are those born before 1945 or after 1965.
Discussion
We describe one of the first studies of an opt-out HIV/HCV testing program in a jail setting. We observed a 6-fold increase in uptake of HIV/HCV testing when it was integrated into routine phlebotomy processes. We also detected few cases of newly diagnosed HIV infection and found high rates of HCV antibody positivity. Nearly half of the inmates who were HCV antibody positive were born after the baby boomer cohort, and these younger, HCV-positive inmates were predominantly non-Hispanic white.
Uptake increased substantially when HIV and HCV testing was offered with scheduled blood draws rather than immediately at jail intake. Potential barriers to screening for infectious diseases in correctional facilities include stigma, competing medical priorities, and strict security protocols. The intake process can be chaotic, with logistical barriers (ie, the need to complete paperwork and assign housing, lack of dedicated space, and reduced security staff members) and individual barriers (ie, incoming inmates may be intoxicated, fatigued, or upset about incarceration) to conducting testing. Aligning priorities and leveraging resources by integrating the study phlebotomist into the jail phlebotomist pool and bundling opt-out HIV/HCV testing with scheduled blood draws increased both the uptake and the number of tests performed monthly. Opt-out testing, which makes testing a routine process rather than one that requires multiple steps or individual requests, may decrease the stigma of being tested for infections such as HIV and HCV. Also, the finding that combining screening for various conditions increases testing uptake was shown during outbreak investigations in the criminal justice system when screening for HIV and tuberculosis was combined.11,12
Although our study found few new HIV diagnoses, our findings on new HIV diagnoses were similar to those in reports on the population in correctional facilities.9 Furthermore, the prevalence of HIV diagnoses (1.0%) found in our study matched the threshold for testing recommended by the Centers for Disease Control and Prevention (0.1% prevalence).13,14 Consistent with national trends,5,15 we identified new HIV infections primarily among young men from racial/ethnic minority groups, and linkage to care while incarcerated was high. In addition, we reconfirmed HIV infection in 24 inmates, 6 of whom had not been engaged in HIV care before entering jail. Similar to the experience in a large urban emergency department in Houston, Texas, where an opt-out HIV testing program significantly increased engagement in HIV care from 41% in 2008 to 59% in 2012 among previously diagnosed people,16 HIV testing in jail provides a critical opportunity to identify and reengage HIV-infected inmates who have been lost to care.
The proportion of inmates with a positive HCV antibody test was 16% in our study, approximately 9 times higher than in the general population in Texas (1.8%).17 However, our results are consistent with other studies in the correctional setting that report an HCV prevalence ranging from 12% to 35%.2,18 One-third of inmates testing positive for HCV had evidence of previous HCV infection in their jail electronic medical record. Although repeat testing may be an opportunity for education and discussion of treatment options, future efforts could improve detection of new infections by pre-screening jail electronic medical records for previous HCV results. Testing only baby boomers would have missed approximately half of HCV infections, predominantly among non-Hispanic white inmates, reflecting national demographic trends in injection drug use and HCV prevalence. From October 2006 to March 2008, of 804 inmates in Massachusetts who reported HCV infection, 67.3% were born after 1965.19 Moreover, among people aged 15-24 in Massachusetts with newly identified HCV during 2002-2006, 78% (1052/1357) were white and 72% (860/1196) reported a history of injection drug use.20 Nationally, acute hepatitis C infection among people aged <30 is associated with rising injection drug use, particularly in nonurban areas.21 Monitoring HCV trends, especially in heavily affected populations such as substance users and incarcerated people, will not only enhance knowledge of the epidemiology of drug use and HCV, but also help direct harm reduction, addiction services, and HCV treatment to those areas that are most affected.
Limitations
Our study had several limitations. First, not all inmates were offered screening; therefore, our results may not reflect the true prevalence of HIV and HCV in the Dallas County Jail. However, the demographic characteristics of our study sample matched the demographic characteristics of the general Dallas County Jail population. Second, we did not perform tests of HCV viral load to confirm HCV antibody results; therefore, a proportion of those who tested positive for HCV antibody may not have had chronic HCV. The next stage of this project includes a reflex test for HCV ribonucleic acid for all positive HCV antibody tests. Third, this study was performed at a single jail; as such, our findings may not be generalizable to other jails. However, the Dallas County Jail is 1 of the 10 largest jails in the country, and our findings reflect real-world implementation of opt-out HIV/HCV testing.
Conclusions
HIV testing identified a small number of new HIV diagnoses, predominantly among young non-Hispanic black men, and rates of linkage to HIV care in the jail were high. Opt-out HIV and HCV testing was feasible and acceptable in the Dallas County Jail, especially when integrated into existing processes. Testing only baby boomers would have missed approximately half of HCV infections, predominantly among non-Hispanic white inmates. Thus, HCV testing should be offered to all inmates, regardless of age. Future efforts should focus on ribonucleic acid testing to confirm HCV infection and link infected people to HCV treatment after release from jail.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was funded by the Gilead FOCUS program. A.E.N. is supported by funding from the National Institute of Allergy and Infectious Diseases (K23 AI 112477). The authors would like to acknowledge the efforts of all the opt-out HIV/HCV project staff members at the Dallas County Jail.
References
- 1. Rich JD, Beckwith CG, Macmadu A, et al. Clinical care of incarcerated people with HIV, viral hepatitis, or tuberculosis. Lancet. 2016;388(10049):1103–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gough E, Kempf MC, Graham L, et al. HIV and hepatitis B and C incidence rates in US correctional populations and high risk groups: a systematic review and meta-analysis. BMC Public Health. 2010;10:777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Solomon L, Montague BT, Beckwith CG, et al. Survey finds that many prisons and jails have room to improve HIV testing and coordination of postrelease treatment. Health Aff (Millwood). 2014;33(3):434–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chodos AH, Ahalt C, Cenzer IS, Myers J, Goldenson J, Williams BA. Older jail inmates and community acute care use. Am J Public Health. 2014;104(9):1728–1733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Iroh PA, Mayo H, Nijhawan AE. The HIV care cascade before, during, and after incarceration: a systematic review and data synthesis. Am J Public Health. 2015;105(7):e5–e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Beckman AL, Bilinski A, Boyko R, et al. New hepatitis C drugs are very costly and unavailable to many state prisoners. Health Aff (Millwood). 2016;35(10):1893–1901. [DOI] [PubMed] [Google Scholar]
- 7. Lucas KD, Eckert V, Behrends CN, Wheeler C, MacGowan RJ, Mohle-Boetani JC. Evaluation of routine HIV opt-out screening and continuum of care services following entry into eight prison reception centers—California, 2012. MMWR Morb Mortal Wkly Rep. 2016;65(7):178–181. [DOI] [PubMed] [Google Scholar]
- 8. Schoenbachler BT, Smith BD, Sena AC, et al. Hepatitis C virus testing and linkage to care in North Carolina and South Carolina jails, 2012-2014. Public Health Rep. 2016;131(suppl 2):98–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Paltiel AD, Weinstein MC, Kimmel AD, et al. Expanded screening for HIV in the United States—an analysis of cost-effectiveness. N Engl J Med. 2005;352(6):586–595. [DOI] [PubMed] [Google Scholar]
- 10. SAS Institute, Inc SAS Version 9.4. Cary, NC: SAS Institute, Inc; 2013. [Google Scholar]
- 11. Stout JE, Katrak S, Goswami ND, et al. Integrated screening for tuberculosis and HIV in tuberculosis contact investigations: lessons learned in North Carolina. Public Health Rep. 2014;129(suppl 1):21–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Person AK, Goswami ND, Bissette DJ, et al. Pairing QuantiFERON gold in-tube with opt-out HIV testing in a tuberculosis contact investigation in the southeastern United States. AIDS Patient Care STDs. 2010;24(9):539–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Janssen RS, Onorato IM, Valdiserri RO, et al. Advancing HIV prevention: new strategies for a changing epidemic—United States, 2003. MMWR Morb Mortal Wkly Rep. 2003;52(15):329–332. [PubMed] [Google Scholar]
- 14. Divine BT, Greby SSM, Hunt KV, Kamb ML, Steketee RW, Warner L. Revised guidelines for HIV counseling, testing, and referral. MMWR Recomm Rep. 2001;50(RR-19):1–57. [PubMed] [Google Scholar]
- 15. Centers for Disease Control and Prevention. Prevalence and awareness of HIV infection among men who have sex with men—21 cities, United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(37):1201–1207. [PubMed] [Google Scholar]
- 16. Flash CA, Pasalar S, Hemmige V, et al. Benefits of a routine opt-out HIV testing and linkage to care program for previously diagnosed patients in publicly funded emergency departments in Houston, TX. J Acquir Immune Defic Syndr. 2015;69(suppl 1):S8–S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yalamanchili K, Saadeh S, Lepe R, Davis GL. The prevalence of hepatitis C virus infection in Texas: implications for future health care. Proc (Bayl Univ Med Cent). 2005;18(1):3–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Akiyama MJ, Kaba F, Rosner Z, Alper H, Holzman RS, MacDonald R. Hepatitis C screening of the “birth cohort” (born 1945-1965) and younger inmates of New York City jails. Am J Public Health. 2016;106(7):1276–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kim AY, Nagami EH, Birch CE, Bowen MJ, Lauer GM, McGovern BH. A simple strategy to identify acute hepatitis C virus infection among newly incarcerated injection drug users. Hepatology. 2013;57(3):944–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Onofrey S, Kludt P, DeMaria A, et al. Hepatitis C virus infection among adolescents and young adults: Massachusetts, 2002-2009. MMWR Morb Mortal Wkly Rep. 2011;60(17):537–541. [PubMed] [Google Scholar]
- 21. Zibbell JE, Iqbal K, Patel RC, et al. ; Centers for Disease Control and Prevention. Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years—Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR Morb Mortal Wkly Rep. 2015;64(17):453–458. [PMC free article] [PubMed] [Google Scholar]