Growing concerns about the wellbeing and stability of the biomedical research workforce are well documented. Over the last 15 years (since the end of the doubling of the NIH budget), we have observed worsening “hypercompetition” as more scientists vie for fewer available dollars (1, 2). Within this hypercompetitive environment, the research workforce is growing older at a rate that is disproportionate to the general American labor force (3). Late-career investigators have been awarded a greater proportion of available research funding, raising concerns that early-career investigators risk being crowded out of the workforce before they have a chance to launch independent scientific careers (3). Other analysts have suggested that adverse effects are also being felt by midcareer investigators (4); large numbers of meritorious investigators may achieve research independence only to lose it because they are unable to renew their one grant or obtain a second new grant.
Fig. 1.
The NIH hopes its latest initiative will improve the grant-funding prospects for early- and midcareer investigators. Image courtesy of Shutterstock/Stephen_Payne.
In our latest effort to tackle this problem, the NIH is launching the “Next Generation Researchers Initiative,” first announced in June. We believe this initiative will help ameliorate these difficult issues in a direct data-driven manner (5) by taking substantive steps to increase funding opportunities for early- and midcareer investigators.
Finding Remedies
It is not entirely clear why early- and midcareer investigators are disproportionately affected by hypercompetition. Some worry about a review bias that favors more-experienced and better-known researchers (5), making it easier for them to get their applications favorably received at peer review. Others have suggested a resiliency factor (4): experienced, well-networked scientists may hold more than one grant or have access to greater sums of grant and private money, making it easier for them to weather the effects of rejected applications. Regardless of the causes, it is clear that NIH funds are being increasingly concentrated among a smaller group of generally more-accomplished, better-recognized investigators (6).
Over the last 10–15 years, the NIH has implemented policies to provide a better chance for early-career investigators, who represent the future, to secure funding. Our previous policy, fully implemented in 2009, calls on NIH Institutes and Centers to take steps to ensure that the success rates for de novo applications are similar for new and established investigators; furthermore, half of the new investigators funded must be early-stage investigators (ESIs), investigators who are within 10 years of their terminal degree (e.g., PhD) or completion of their clinical training. Effectively, the policy has given handicaps to new and early-stage investigators. Recently published data suggest that this policy has attenuated the decline in fortunes among early-stage investigators (4, 5) but may have actually worsened outcomes for midcareer investigators.
A New Approach
The Next Generation Researchers Initiative is an effort to reverse the adverse trends seen by both ESIs and early-established investigators (EEIs), those midcareer investigators who are within 10 years of first achieving research independence as ESIs and are trying to maintain funding. This Initiative also responds to Section 2021 of the 21st Century Cures Act, which Congress passed into law in December 2016. That section calls on the NIH Director “to develop, modify, or prioritize policies … to promote opportunities for new researchers and earlier research independence, such as policies to increase opportunities for new researchers to receive funding.”
Therefore, beginning in Fiscal Year 2017, the NIH will fund greater numbers of ESI and EEIs than in years past. For ESIs, our goal for Fiscal Year 2017, and for subsequent years, is to issue competing awards to approximately 200 more than we did in Fiscal Year 2016. We will also identify EEIs, investigators who are within 10 years of receiving their first major independent NIH research award and who received their first award as an early-stage investigator. Among these investigators, we will prioritize those who are at risk of losing their only source of NIH funding despite having submitted an application that fared well on peer review, as well as
Some might worry that redirecting funds to more early-career investigators may lead to funding lower-quality science. We do not see this as a risk.
those potential rising stars who have one active award and are seeking to add a second. We will aim to issue competing awards to about 200 more such EEIs than we have in years past. Over five years (the typical length for a first NIH research grant), this policy will lead to funding of approximately 2,000 additional ESIs and EEIs who would otherwise have just missed the payline. Our targets are consistent with those suggested by a recently published NIH workforce analysis (5) that recommended the agency fund approximately 2,200 additional early-career investigators to stabilize workforce demographics.
The Next Generation Researchers Initiative effectively mandates that NIH redistribute some funds to approximately 400 ESIs and EEIs each year. We estimate that in Fiscal Year 2017 these redirected funds will add up to about $210 million. As we roll out the initiative over the next five years, we will reach a steady state of roughly $1.1 billion (5).
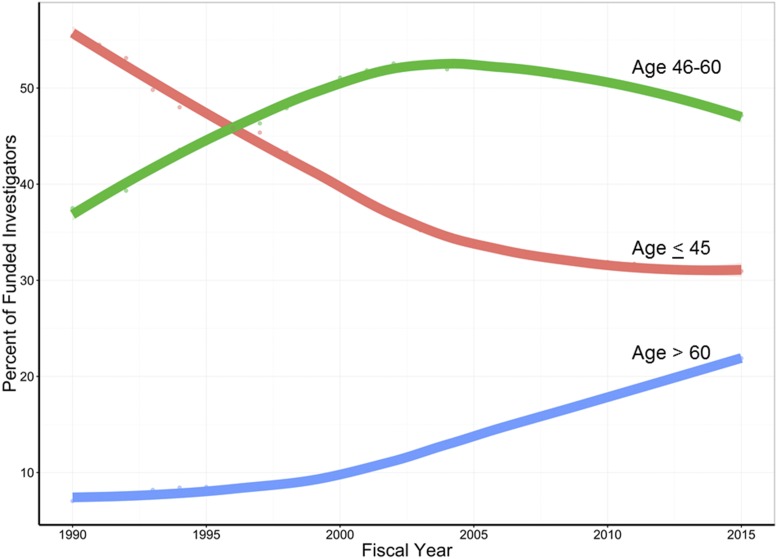
Fig. 2.
Since the late 1990s, the percentage of NIH-funded investigators over the age of 60 years—those earning research-project and other substantive NIH awards—has risen significantly compared with other age groups. The curves are drawn by locally weighted scatterplot smoothing.
Funding Sources
An obvious question is where these monies will come from. Earlier this year, we took note of published findings showing diminishing marginal returns as individual researchers’ levels of funding increase (7, 8). We were able to replicate those findings for NIH-funded scientists with the highest level of support and therefore proposed a possible funding cap of the equivalent of three R01 grants per investigator at any given time. After hearing extensive feedback from the community, we concluded that to apply such a formula across the board was inconsistent with longstanding NIH principles of considering the individual merits of each and every application and investigator, taking into account peer review assessments and agency strategic goals and objectives. We also realized that our initial attempts at creating a metric to describe current funding support did not adequately take into account the complexities of “team science.”
Assisted by a Working Group of the Advisory Committee to the NIH Director, we will continue to explore the use of productivity metrics that can be applied, ideally on an individual basis, to guide NIH funding decisions. The Working Group, which is already engaged in deliberations, will consider productivity metrics beyond publication and citation counts. One possible framework might be “PQRST” for productivity, quality, reproducibility, sharing, and translation, respectively (9). We anticipate interim reports in upcoming public meetings of the Advisory Committee of the Director.
For now, each NIH Institute and Center will take steps to reprioritize funds according to its specific programmatic goals and objectives, while meeting the mandate to increase funding opportunities for new researchers seeking to obtain and maintain earlier research independence. Monies may come from recent Congressional budget increases, from lower allocations to institute-initiated research programs, from selected decisions to reduce increments in funding for investigators who are already well funded, and from greater allocations to certain targeted programs (such as the R35 early-investigator–focused programs of the National Institutes of General Medical Sciences, the National Cancer Institute, and the National Heart, Lung, and Blood Institute).
Some might worry that redirecting funds to more early-career investigators may lead to funding lower-quality science. We do not see this as a risk. Recent data show that there is at most a weak association between age and outcome on individual applications (4, 10), arguing against concerns that early-career investigators are writing lower-quality grants. Other data show that there is no clear-cut association between career stage and research impact (11, 12); early-career researchers do not appear to be less creative or capable (5). Current NIH paylines are well below those seen at the time of the NIH doubling, yet follow-up analyses have suggested essentially equivalent productivity of NIH grants that received peer review scores near the top of the fundable range during those more-favorable times (13, 14). We know that in the current hypercompetitive environment many outstanding early-career investigators are left out in the cold. We risk fostering a research environment in which society will, in the years ahead, expect crucial cures from a less-experienced, poorly funded, and dwindling cohort of investigators.
We look forward to working with the extramural scientific community, Congress, and all interested stakeholders as we roll out the Next Generation Researchers Initiative. We recognize that our steps to fund more early-career investigators and rescue vulnerable early-established investigators will have far-reaching effects not only for the investigators but also for universities, research staff, administrators, scientific journals, and all investigators receiving (or seeking to receive) NIH funds. We plan to collect and follow all relevant data, including data on the numbers, characteristics, scientific interests, and research productivity of investigators funded through the Initiative and of all investigators in the NIH portfolio. We will analyze and report these data to minimize the risk of unintended adverse consequences and to ensure that the Initiative is achieving its goal of enabling a brighter future for the next generation of biomedical researchers in the United States.
Footnotes
The authors declare no conflict of interest.
Any opinions, findings, conclusions, or recommendations expressed in this work are those of the authors and have not been endorsed by the National Academy of Sciences.
References
- 1.Kimble J, et al. Strategies from UW-Madison for rescuing biomedical research in the US. Elife. 2015;4:e09305. doi: 10.7554/eLife.09305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alberts B, Kirschner MW, Tilghman S, Varmus H. Rescuing US biomedical research from its systemic flaws. Proc Natl Acad Sci USA. 2014;111:5773–5777. doi: 10.1073/pnas.1404402111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blau DM, Weinberg BA. Why the US science and engineering workforce is aging rapidly. Proc Natl Acad Sci USA. 2017;114:3879–3884. doi: 10.1073/pnas.1611748114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Charette MF, et al. Shifting demographics among research project grant awardees at the National Heart, Lung, and Blood Institute (NHLBI) PLoS One. 2016;11:e0168511. doi: 10.1371/journal.pone.0168511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levitt M, Levitt JM. Future of fundamental discovery in US biomedical research. Proc Natl Acad Sci USA. 2017;114:6498–6503. doi: 10.1073/pnas.1609996114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katz Y, Matter U. 2017 On the biomedical elite: Inequality and stasis in scientific knowledge production. Available at nrs.harvard.edu/urn-3:HUL.InstRepos:33373356. Accessed September 27, 2017.
- 7.Fortin JM, Currie DJ. Big science vs. little science: How scientific impact scales with funding. PLoS One. 2013;8:e65263. doi: 10.1371/journal.pone.0065263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mongeon P, Brodeur C, Beaudry C, Larivière V. Concentration of research funding leads to decreasing marginal returns. Res Eval. 2016;25:396–404. [Google Scholar]
- 9.Ioannidis JP, Khoury MJ. Assessing value in biomedical research: the PQRST of appraisal and reward. JAMA. 2014;312:483–484. doi: 10.1001/jama.2014.6932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eblen MK, Wagner RM, RoyChowdhury D, Patel KC, Pearson K. How criterion scores predict the overall impact score and funding outcomes for National Institutes of Health peer-reviewed applications. PLoS One. 2016;11:e0155060. doi: 10.1371/journal.pone.0155060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sinatra R, Wang D, Deville P, Song C, Barabási AL. Quantifying the evolution of individual scientific impact. Science. 2016;354:aaf5239. doi: 10.1126/science.aaf5239. [DOI] [PubMed] [Google Scholar]
- 12.Clauset A, Larremore DB, Sinatra R. Data-driven predictions in the science of science. Science. 2017;355:477–480. doi: 10.1126/science.aal4217. [DOI] [PubMed] [Google Scholar]
- 13.Doyle JM, et al. Association of percentile ranking with citation impact and productivity in a large cohort of de novo NIMH-funded R01 grants. Mol Psychiatry. 2015;20:1030–1036. doi: 10.1038/mp.2015.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fang FC, Bowen A, Casadevall A. NIH peer review percentile scores are poorly predictive of grant productivity. Elife. 2016;5:e13323. doi: 10.7554/eLife.13323. [DOI] [PMC free article] [PubMed] [Google Scholar]