Abstract
Jejunoileal bypass (JIB) was developed as a surgical treatment for morbid obesity in the early 1950s. However, this procedure is now known to be associated with multiple metabolic complications and has subsequently been abandoned as a viable bariatric procedure. Some of these known complications include renal stone formation, liver failure, migratory arthritis, fat-soluble deficiencies, blind-loop syndrome and severe diarrhea. Additionally, there have been animal models suggesting colon dysplasia after JIB. To our knowledge however, in humans, no colon cancers have been attributed to JIB in the literature. Here we report a 63-year-old morbidly obese female who had a JIB surgery in 1973 and subsequently was found to have numerous sessile colonic polyps throughout her colon and adenocarcinoma of the ascending colon without any family history of colonic polyposis syndromes or colon cancer.
INTRODUCTION
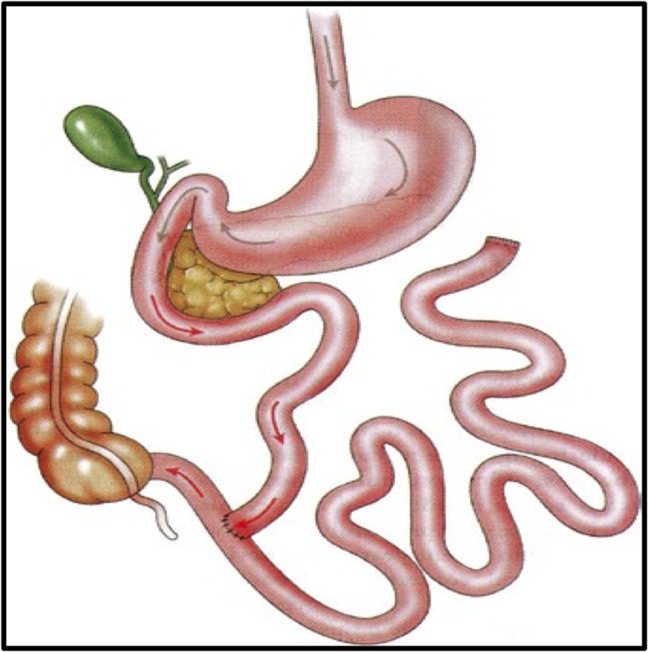
Bariatric surgery has proven to be the most efficacious treatment for morbid obesity and resolution of obesity-related comorbidities [1]. Early on in the surgical treatment of morbid obesity, the jejunoileal bypass (JIB) procedure was introduced in the 1950s in the USA [2]. The procedure created effective weight loss by producing significant calorie malabsorption as all but the distal 10 cm of ileum was bypassed (Fig. 1) [3]. This procedure was effective in producing substantial initial weight loss and achieved durable results [3–5]. However, JIB was abandoned early in the 1980s due to severe short and long-term complications, such as renal stone formation, liver failure, migratory arthritis, fat-soluble vitamin deficiencies, blind-loop syndrome and severe diarrhea [6–9]. Currently, the JIB is no longer recommended as the treatment option for morbid obesity. Today, there remains a population of patients post JIB where long-term complications are still being discovered. Herein, we report, to our best knowledge, the first case of a colon adenocarcinoma following JIB surgery in humans.
Figure 1:
Anatomy of jejunoileal bypass.
CASE REPORT
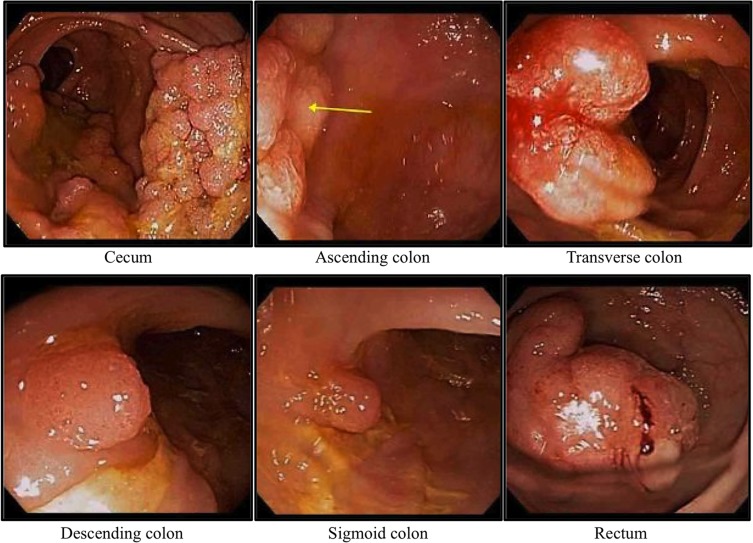
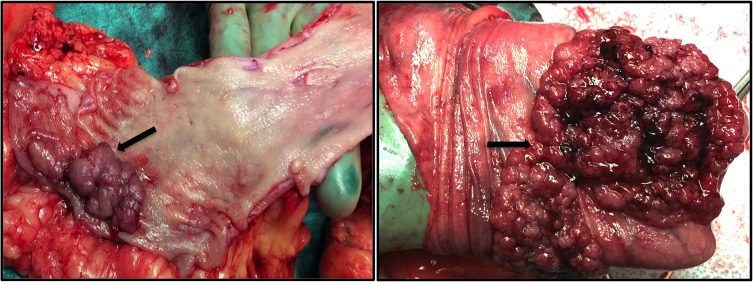
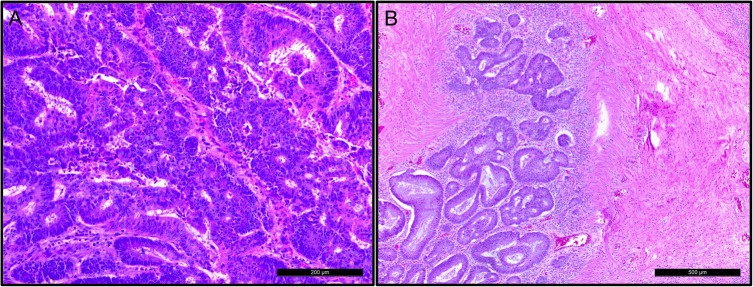
A 63-year-old morbidly obese female (BMI of 62.2 kg/m2) who underwent a JIB in 1973, presented to our surgical clinic in December of 2013 with persistent morbid obesity as well as vague gastrointestinal complaints, particularly the sensation of bloating. Her medical history includes hypertension, diabetes mellitus type 2, hyperlipidemia, chronic kidney disease, arthritis, congestive heart failure, gout, fatty liver disease, history of a deep vein thrombosis and pulmonary emboli. The patient denies any known family history of colorectal cancer or familial polyposis syndromes. During a previous screening esophagogastroduodenoscopy and colonoscopy in 2010 the patient was found to have reflux induced esophagitis with a normal stomach and duodenum. On colonoscopy, she was found to have multiple adenomatous polyps throughout the colon, without any evidence for malignancy. The patient unfortunately was lost to follow-up until she was seen in our minimally invasive general and bariatric surgery clinic in December of 2013. After our assessment, the patient was referred back to gastroenterology for further evaluation based on prior findings of multiple colonic polyps from 2010. A repeat colonoscopy in February of 2014 identified multiple tubular adenomatous and tubulovillous polyps measuring 3–30 mm in size throughout the colon (Fig. 2). Due to the extent of the colonic polyposis and persistent morbid obesity, the patient was taken to surgery for a total abdominal colectomy and low anterior resection with an end ileostomy by the colorectal surgical team, reversal of her previous JIB, and vertical sleeve gastrectomy. A total of thirteen colonic polyps were found in the resected specimen ranging in size from 1.4 to 7.6 cm. Pictures of the gross pathology for two of the larger polyps are shown in Fig. 3. Histopathologic analysis from a 1.4 cm polyp in the ascending colon revealed an invasive adenocarcinoma (Fig. 4). Twelve benign lymph nodes were also found in the resected specimen. The patient tolerated her immediate post-operative course well, however, she expired on post-operative day 67 due to septic complications including pneumonia.
Figure 2:
Colonoscopy: colonic polyposis.
Figure 3:
Surgical fragments from total colectomy with polyposis.
Figure 4:
Optical microscopic view, hematoxylin & eosin staining. Fragments from polypoid lesion with adenocarcinoma. (A) Invasive adenocarcinoma, low grade. (B) Adenocarcinoma with desmoplastic reaction.
DISCUSSION
Despite many known complications following JIB such as electrolyte imbalances, biliary and renal lithiasis, hepatic insufficiency, bone disease, renal insufficiency, gout, autoimmune diseases and various intestinal complications [10], this is to our knowledge the first report of colon cancer described in the literature.
Obesity, itself is a major risk factor for cancer development [11]. Colorectal carcinogenesis has been an area of research in post JIB patients secondary to higher amounts of bile acids in the colon, considered as a carcinogenic substance to colonic mucosa [12]. Bile acids are found to be 10 times higher from colonic stool samples of patients following JIB versus normal anatomy patients [13]. Moreover, animal studies have shown an increased risk for colon carcinoma in rats after JIB [14, 15]. Additionally, patients status-post JIB have a persistent increase in cell proliferation in the large intestine compared with patients with native anatomy, suggesting an increased risk for developing colonic cancer [16]. Despite no previous reports in the literature of colon cancer following JIB, McFarland et al. [17] did report on a patient who was found to have two tubulovillous adenomas, without signs of malignancy.
Despite growing evidence for a cause and effect relationship of the JIB to initiate colonic neoplasia, other etiologies exist as the cause for colon cancer in this particular case. Although our patient denied any family history of colon cancer or familial intestinal polyposis syndromes, sporadic polyposis syndromes cannot be completely excluded as a cause. Sporadic polyposis syndromes have been shown to occur in 20–40% of patients with colonic polyposis [18, 19].
In conclusion, we report here a case of colon cancer in a patient 30 years following JIB surgery. Patients who have had a JIB procedure are now becoming more rare, however, physicians who encounter these patients should ensure proper colon cancer screening. Mechanisms at the cellular level are largely still unknown but this report may offer some direction into further research.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Kissler HJ, Settmacher U. Bariatric surgery to treat obesity. Semin Nephrol 2013;33:75–89. [DOI] [PubMed] [Google Scholar]
- 2. Kremen AJ, Linner JH, Nelson CH. An experimental evaluation of the nutritional importance of proximal and distal small intestine. Ann Surg 1954;140:439–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Griffen WO Jr., Bivins BA, Bell RM. The decline and fall of the jejunoileal bypass. Surg Gynecol Obstet 1983;157:301–8. [PubMed] [Google Scholar]
- 4. Deitel M, Shahi B, Anand PK, Deitel FH, Cardinell DL. Long-term outcome in a series of jejunoileal bypass patients. Obes Surg 1993;3:247–52. [DOI] [PubMed] [Google Scholar]
- 5. Vage V, Solhaug JH, Berstad A, Svanes K, Viste A. Jejunoileal bypass in the treatment of morbid obesity: a 25-year follow-up study of 36 patients. Obes Surg 2002;12:312–8. [DOI] [PubMed] [Google Scholar]
- 6. Cannova JV, Krummen DM, Schreiber H, Schaefer IK. An approach to the treatment of recurring polyarthralgia after jejunoileal bypass. Obes Surg 1997;7:215–7; discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 7. Lowell JA, Shenoy S, Ghalib R, Caldwell C, White FV, Peters M, et al. Liver transplantation after jejunoileal bypass for morbid obesity. J Am Coll Surg 1997;185:123–7. [DOI] [PubMed] [Google Scholar]
- 8. Mole DR, Tomson CR, Mortensen N, Winearls CG. Renal complications of jejuno-ileal bypass for obesity. QJM 2001;94:69–77. [DOI] [PubMed] [Google Scholar]
- 9. Sorenson HA, Frendsen NJ, Hyldstrup L. Late calcium metabolic consequences of jejuno-ileal bypass. Obes Surg 1992;2:219–23. [DOI] [PubMed] [Google Scholar]
- 10. Singh D, Laya AS, Clarkston WK, Allen MJ. Jejunoileal bypass: a surgery of the past and a review of its complications. World J Gastroenterol 2009;15:2277–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 2003;348:1625–38. [DOI] [PubMed] [Google Scholar]
- 12. Farhana L, Nangia-Makker P, Arbit E, Shango K, Sarkar S, Mahmud H, et al. Bile acid: a potential inducer of colon cancer stem cells. Stem Cell Res Ther 2016;7:181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Koivisto P, Miettinen TA. Adaptation of cholesterol and bile acid metabolism and vitamin B12 absorption in the long-term follow-up after partial ileal bypass. Gastroenterology 1986;90:984–90. [DOI] [PubMed] [Google Scholar]
- 14. Bristol JB, Wells M, Williamson RC. Adaptation to jejunoileal bypass promotes experimental colorectal carcinogenesis. Br J Surg 1984;71:123–6. [DOI] [PubMed] [Google Scholar]
- 15. Rainey JB, Davies PW, Williamson RC. Relative effects of ileal resection and bypass on intestinal adaptation and carcinogenesis. Br J Surg 1984;71:197–202. [DOI] [PubMed] [Google Scholar]
- 16. Appleton GV, Wheeler EE, Al-Mufti R, Challacombe DN, Williamson RC. Rectal hyperplasia after jejunoileal bypass for morbid obesity. Gut 1988;29:1544–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McFarland RJ, Talbot RW, Woolf N, Gazet JC. Dysplasia of the colon after jejuno-ileal bypass. Br J Surg 1987;74:21–2. [DOI] [PubMed] [Google Scholar]
- 18. Heinimann K, Thompson A, Locher A, Furlanetto T, Bader E, Wolf A, et al. Nontruncating APC germ-line mutations and mismatch repair deficiency play a minor role in APC mutation-negative polyposis. Cancer Res 2001;61:7616–22. [PubMed] [Google Scholar]
- 19. Truta B, Allen BA, Conrad PG, Weinberg V, Miller GA, Pomponio R, et al. A comparison of the phenotype and genotype in adenomatous polyposis patients with and without a family history. Fam Cancer 2005;4:127–33. [DOI] [PubMed] [Google Scholar]