Abstract
Objective
To examine the cancer information seeking behaviors and preferences of cancer survivors.
Methods
This cross sectional study used the National Cancer Institute’s 2003 Health Information National Trends Survey data to evaluate 619 cancer survivors.
Results
Two thirds (67.5%, n=418) of the survivors sought cancer information (InfoSeek) and 32.5% (n=201) did not (NoInfoSeek). Significant predictors of cancer information seeking included age (less than 65), gender (female), income (>$25,000/yr) and having a regular HCP.
Conclusion
Not all survivors actively look for cancer information. Although most survivors prefer receiving cancer information from their HCP, many turn to a variety of other sources, primarily the internet.
Practice Implications
HCPs should periodically assess information seeking behaviors and preferences of cancer survivors and actively refer patients to the Internet as an extension of and enhancement to their patient interactions. Credible and useful websites could be identified and recommended by the HCP as a means to address some of the barriers identified by survivors.
Keywords: cancer survivors, information seeking, internet, coping, information avoiders
1. Introduction
When confronted with a potentially life threatening illness such as cancer, information may provide needed knowledge about the disease, treatment, and self-care management. It may also facilitiate coping by mediating uncertainty and anxiety and by providing social support [1-6]. Information seeking is the purposive acquistion of information from selected information carriers [7].1 Exploring the factors that influence individuals’ cancer information seeking (or avoiding) behaviors or actions is important when developing cancer communication interventions.
The information needs of cancer survivors were first documented by Cassileth [8] in a study of 256 recently diagnosed cancer patients. Cancer patients desired information about diagnosis (type, stage, location), treatment and treatment goals, side effects, and impact on quality of life. Information preferences were associated with age, education, race, and medical status. Since that seminal study, a number of others have explored the information needs of cancer survivors [5, 11-19]. These studies identified other patient factors that influenced information needs including gender, employment status, coping style, type of cancer, and time since diagnosis. Many of these studies documented the now prevailing paradigm: the majority of cancer survivors desire as much information as possible about their disease and treatment [8, 14, 16]. However, not all survivors want that much information. The amount and timing of information desired varied in those with a blunting style (avoiding threatening information) or for those trying to maintain hope [5, 11, 12, 18, 20-24].
Information source preferences among cancer survivors have been explored in a number of studies [17, 25-28]. The preferred source of information has been identified in most of these studies as interpersonal communication with the physician or health care provider. Other mediated sources, including the Internet, used alone or in combination, were also selected.
A number of literature reviews were conducted regarding cancer information seeking behaviors among cancer patients and their families [4, 10, 29-31]. With few exceptions, most studies included in these reviews were descriptive and cross-sectional in design and reported information needs and behaviors from relatively newly diagnosed cancer patients (first year or two).
Many health behavior models include beliefs and knowledge as important variables in understanding and promoting behavior change. The comprehensive model of information seeking (CMIS) is a conceptual model linking information seeking with health behavior models and has three major components: antecedents; information carrier factors; and information seeking which may then act together with other health behavior models. [7] Antecedent factors include demographics (gender, age, race/ethnicity, education, and socioeconomic status), direct experience (including personal and social networks), salience (perceived applicability to the problem at hand) and beliefs (about lack of knowledge, self-efficacy, cancer). These antecedent factors influence the need for information and the information channel preferences. Information carrier factors relate to channel selection, either interpersonal (health care providers, family, friends) or mediated (print, electronic, mass media), and channel usage. The utility or usefulness of the channel selection is related to the information seeker’s needs, expectations, and accessibility. Information seeking actions may be passive or active, seeking or avoiding [24, 32]. These actions may then interact with or become part of other health behavior models. Health information seeking or avoidance has the potential to moderate perceived health threats (severity and susceptibility), provide cues to action, and influence psychological and behavioral outcomes [4, 7, 9, 33]. This may be useful when designing interventions to promote healthy lifestyle behaviors in cancer survivors. For example, Perry and Bauer (2001), using the Health Belief Model and stages of change, developed and tested compuer generated printed tailored messages regarding vegetable intake for breast cancer survivors. The experimental group improved vegetable consumption and moved forward in their stage of change.
The purpose of this study was to examine the antecendent and information carrier factors associated with different information seeking behaviors or actions of cancer survivors. This is a secondary data analysis utilizing the National Cancer Institute’s (NCI) Health Information National Trends Survey I (HINTS I), a national survey about the public’s use of cancer-related information [34]. Specific research questions for this study are:
-
∎
What are the differences between survivors who do and do not seek cancer information?
-
∎
What are the preferred sources of information of cancer survivors who do or do not seek cancer information?
2. Methods
This is a cross sectional, correlational study using the NCI’s 2003 HINTS I database. [35] HINTS was designed to collect nationally representative data every two years focused on cancer communications, cancer information seeking preferences and behaviors, knowledge about cancer, perceived susceptibility, severity, benefits and barriers, cancer-related behaviors, risk reduction, screening behaviors, general health, and data on personal cancer experience [35]. The first wave of HINTS data was collected in 2003, HINTS 1.
Sample
Of the 6,369 participants included in HINTS 1, 9.7% (n= 619) identified themselves as cancer survivors2. Of these cancer survivors, 67.5% (n=418) had personally sought cancer information (InfoSeek) and 32.5% (n=201) had not (NoInfoSeek). The most commonly reported cancers were breast, cervical, prostate, melanoma, colorectal and endometrial cancers; 9.5% reported having more than one type of cancer.
Measures
An expert advisory committee guided NCI personnel in the development of the HINTS I survey [35]. Established criteria for scientific validity, utility and implementation experience served as the basis for inclusion of survey items [35]. After expert review, cognitive interviewing, and national field testing, the final survey consisted of questions regarding cancer communication (35 items), cancer history and general cancer knowledge (16 items), cancer specific personal risk and screening questions (54 items), primary cancer risk behaviors (29 items), and health status and demographics (14 items) [35]. The English and Spanish versions of the HINTS I survey instrument can be obtained at http://cancercontrol.cancer.gov/hints.
HINTS 1 Procedures
Once approved by the NIH IRB, national data were collected in English and Spanish from October 2002 through May 2003 using a list-assisted random-digit-dial (RDD) sampling method [36]. One English or Spanish speaking adult (≥18 years) was selected within each household to be interviewed by phone [34]. To obtain adequate minority representation, special efforts were made to oversample telephone exchanges for African-Americans and Hispanics. The survey was administered following the best practices identified by the American Association for Public Opinion Research [37] to minimize bias from coverage, sampling, and nonresponse and measurement error [35]. Telephone interviewers reached 19,509 households; 55% completed the screening interview and 62.8% of those who completed the screener completed the extended interview with a final total HINTS sample of 6,369. The average interview length was 30 minutes.
For the current study, an IRB exemption was granted and, after registering for access at NCI for this secondary data analysis, the HINTS I SAS files and codebooks were obtained from the HINTS website (http://hints.matthewsgroup.com/register.asp).
Statistical analysis
This secondary data analysis used a variety of analytical approaches to address each of the research questions [38, 39]. Replicate weights, provided by the NCI, were used to compute jackknife variance estimations, adjust for nonresponse, and calibrate or weight for gender, age, race and ethnicity, and education [40]. All sample sizes are reported as unweighted and all percentages are weighted which allows for the adjusted sample data to be representative of US population estimates. Comparisons were made between cancer survivors who did (InfoSeek) and did not (NoInfoSeek) seek cancer information. Information carrier factors related to channel selection are described; Preferred and trusted sources of information were also tested by time since diagnosis (≤1 year, 2-5 years, 6-10 years, and ≥ 11 years). Descriptive statistics, presented as proportions or means, were calculated for responses related to information seeking behaviors and preferences and demographic variables. Categorical variables were compared using cross-tabulations and chi-square tests, continuous data were compared using means and t-tests were conducted. To identify antecedent factors that were independently associated with information seeking behaviors among cancer survivors, demographic and experience variables (p<.10) from the univariate analysis were entered in a multiple logistic regression analysis with information seeking (yes, no) as the dependent variable. Variables included age (<65, ≥ 65 years of age), education (≤ high school, high school, > high school), income (<$25K, ≥ $25k), employment status (employed or not), marital status (married/partnered or not), having a child ≤ 18 years of age in household (yes/no), having a regular health care provider (HCP) (yes, no), having health insurance (yes, no), and internet access (yes, no). Although gender and race groups (Caucasian, black, other) were not significantly different, they were entered into the logistic regression since they have been found to be important in other studies of information seeking. Variables that were not significant were then dropped from the model in stages. SAS version 9.0 (Cary, NC) and SUDAAN SAS 9.1 Callable version (RTI, Research Triangle Park, NC) were used for all analyses [41, 42]. Using the comprehensive model of information seeking, antecedent factors results are presented first followed by information carrier factors results.
3. Results
Antecedent Factors
Differences Between Information Seekers And Nonseekers. The typical cancer survivor was Caucasian, employed, married, and female, had at least a high school education, a regular health care provider and health insurance (table 1). The mean time since a cancer diagnosis was 10.5 years for InfoSeek and 12.5 years for NoInfoSeek (p=.05). These groups were, however, significantly different (p < .05) on a number of factors. The NoInfoSeek group was older (p <.001), had less education (p<.001) and income (p<.001). They also had a smaller proportion reported being married (p=.02), having children in their household (p =.001), working (p <.001), having a regular health care provider (p=.003), having someone else look for cancer information for them (p<.001), and having Internet access (p<.001). There were some differences in types of cancer (p =.04) between the two groups: the NoInfoSeek had more breast and prostate cancer and less endometrial and lung cancer than the InfoSeek group. In the final logistic regression model, four variables were significant (p<.05) predictors of information seeking. Information seekers were more likely to be: ‘younger’ (< 65 years of age) (odds ratio (OR) 4.8 with 95% confidence interval (CI) 2.9-8.2); female (OR 1.7, CI 1.1-2.7); having greater income (OR 3.4, CI 2.1-5.6); and having a regular health care provider (OR 3.5, CI 1.7-7.4). Income and education were positively associated with each other (p <.001). Education and Internet were also positively associated with each other (<.001).
Table 1.
2003 HINTS Cancer Survivor Characteristics (n= 619)
| InfoSeeker (n= 418, 67.5%) | NoInfoSeek (n=201, 32.5%) | p-value | |
|---|---|---|---|
| Age (mean years) | 54 | 66 | <.0001 |
| Gender (% female) | 67.8 | 60.7 | .1 |
| Marital Status | .02 | ||
| Married/partnered | 70.7% | 55.7% | |
| Divorced/separated | 12.1% | 13.3% | |
| Widowed | 10.3% | 24.9% | |
| Never married | 7.1% | 6% | |
| Race | |||
| Caucasian | 84.5% | 74.1% | .3 |
| Black | 7.8% | 9.9% | |
| Hispanic | 3.7% | 6.9% | |
| Other | 4% | 9.2% | |
| Education | <.0001 | ||
| < High School | 10.9% | 32.7% | |
| High School | 37.5% | 38.6% | |
| > High School | 51.6% | 27.7% | |
| Employment status | <.0001 | ||
| Full-time/self-employed | 47.2% | 21.8% | |
| Retired | 25.8% | 54.4% | |
| Not able to work | 10.8% | 12.1% | |
| Homemaker | InfoSeeker | NoInfoSeek | |
| Out of work | 8.2% | 6.3% | |
| Student | 5% | 2.7% | |
| 2.1% | 2.8% | ||
| Household income | |||
| <$25,000/yr | 24.7% | 48.1% | <.0001 |
| $25,000-<35,000 | 15% | 7.5% | |
| $35,000-<50,000 | 17.4% | 11.6% | |
| $50,000-<75,000 | 13% | 8.4$ | |
| ≥$75,000 | 19.6% | 7.3% | |
| Missing | 10.3% | 17% | |
| Child <18 years of age in household | 34.2% | 16.3% | .0003 |
| Have regular health care provider | 86.7% | 71.1% | .003 |
| Have health insurance | 93.6% | 90.4% | .4 |
| General health status | .8 | ||
| Excellent | 11% | 8.7% | |
| Very Good | 25.7% | 24.2% | |
| Good | 28.2% | 29% | |
| Fair | 23.4% | 28.7% | |
| Poor | 11.8% | 9.5% | |
| Years since diagnosis (mean years) | 10.5 | 12.5 | .05 |
| Type of cancer (n) | |||
| Breast (119) | 16.3% | 18.9% | .04 |
| Cervical (94) | 15.8% | 11.7% | |
| Prostate (62) | 10.2% | 15% | |
| Melanoma (61) | 10.7% | 10% | |
| Colorectal (49) | 7.6% | 7.7% | |
| Endometrial (39) | 7.3% | 4.3% | |
| Lymphoma (21) | 5.5% | 1.7% | |
| Eleven others (combined1) (159) | 25.1% | 30.4% | |
| More than one cancer (59) | 67.8% | 32.2% | |
| Family member has had cancer | 70.3% | 66% | .6 |
| Other person looked for cancer information | 52.9% | 12.1% | <.0001 |
| Have Internet access | 61.2% | 24% | <.001 |
| Type of Access | |||
| Telephone | 71.2% | 81.8% | |
| Broadband (cable, DSL) | 26.4% | 13.8% | |
| Other | 1.7% | 4.4% |
None of the eleven cancers accounted for ≥4%.
Respondents were asked about their beliefs regarding trusted sources of cancer information. When asked how much they trusted different sources of information (from 1 = a lot to 4 = not at all), significant differences were found in all sources between the InfoSeek and NoInfoSeek groups. The NoInfoSeek group ranked their trust in all sources lower than the InfoSeek group (p values range by source from .04 to<.001) (figure 1).
Figure 1.
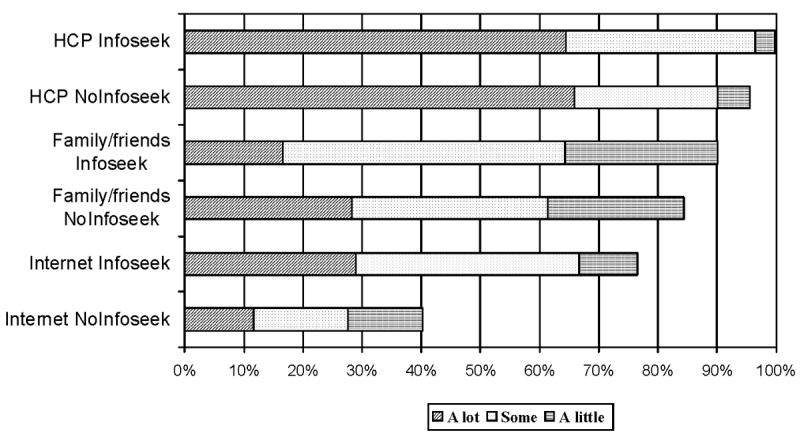
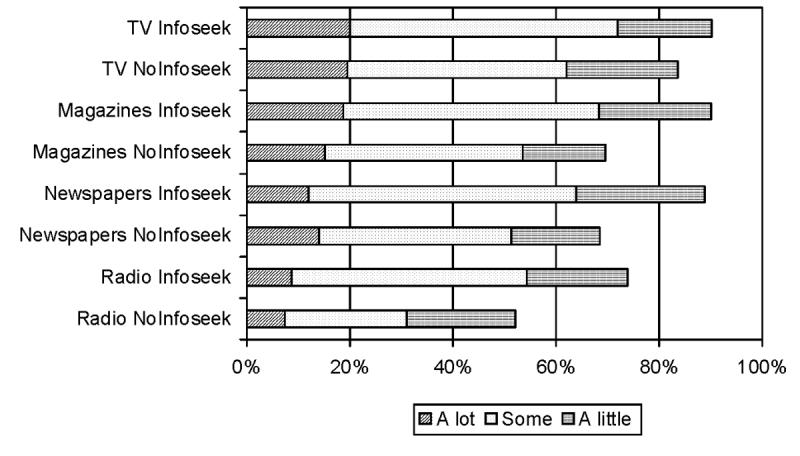
InfoSeek and NoInfoSeek: Trust in Information Source or Channel
Information Carriers
InfoSeek (n=408) were asked to describe where they looked for cancer information most recently. The two most commonly cited sources were the Internet (35.4%) and health care providers (19.4%) followed by books (12.9%). No significant differences were found in either group for source of information used by time since diagnosis (≤1 year, 2-5 years, 6-10 years, and ≥ 11 years). Information seekers were also more likely to have had someone else (usually a family member) look for cancer information for them (p<.001).
Even though 83% (343/409) of InfoSeek agreed that they were satisfied with the information they obtained, a number of barriers were identified. They included: 25% being concerned about the quality of the information; 15% wanting more information but not finding it; 16% being frustrated trying to find information; 14% not having enough time to get information; 16% taking a lot of effort to find the information, and 13% finding it too hard to understand.
As noted, Internet access was significantly higher for InfoSeek (61.2%, 256/418) compared to the NoInfoSeek group (24%, 48/201, p<.0001). Of the InfoSeek with Internet access, 67% sought cancer information online. The most frequently cited reasons that InfoSeek used the Internet for cancer information included convenience (28%), amount of available information (23%), immediacy of access (15%), and provided more current and reliable information (4%). Almost all (91%) found the online cancer information somewhat or very useful. Most InfoSeek using the Internet for cancer information (71%) reported finding the online sites by using Internet search engines.
Reasons cited for not using the Internet were similar for both InfoSeek and the NoInfoSeek groups and included: too complicated (40% and 56% respectively), not interested (38 % and 43%), costs too much (34% and 38%), and not useful (14% and 23%). Of note, only 26% of InfoSeek and 14% NoInfoSeek reported hi-speed (broadband/cable modem or DSL) access to the Internet (NS), the rest had telephone access.
Cancer survivors were asked where they would first look for cancer information if it was needed in the future (figure 2). When asked what they would use if available and free, both groups listed their health care provider first followed by the Internet regardless of time since diagnosis. All other interpersonal and mediated sources of information were cited much less frequently. They were also asked what sources of information they would like to use. InfoSeek consistently selected more information sources than the NoInfoSeek group (figure 3). While they had different levels of endorsement, the majority in both groups was willing to read personalized materials if offered.
Figure 2.
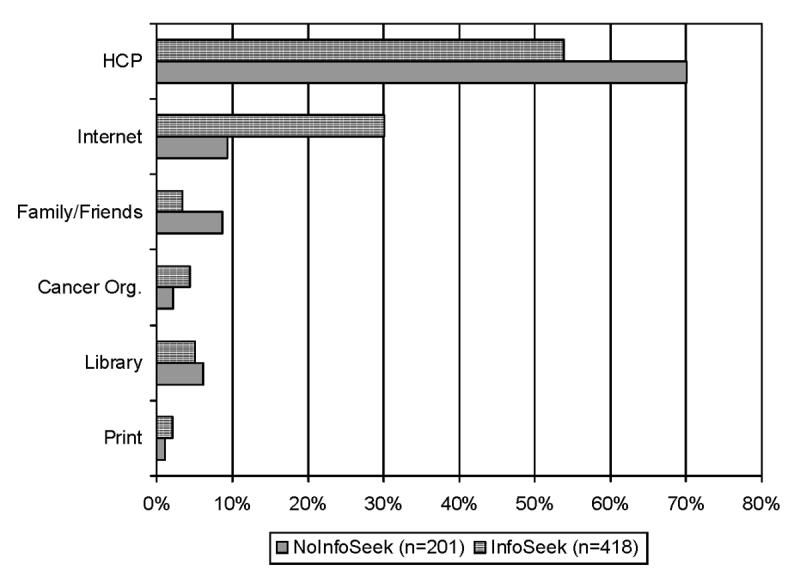
Cancer Survivors’ Preferred Sources of Information (p <.001)
Figure 3.
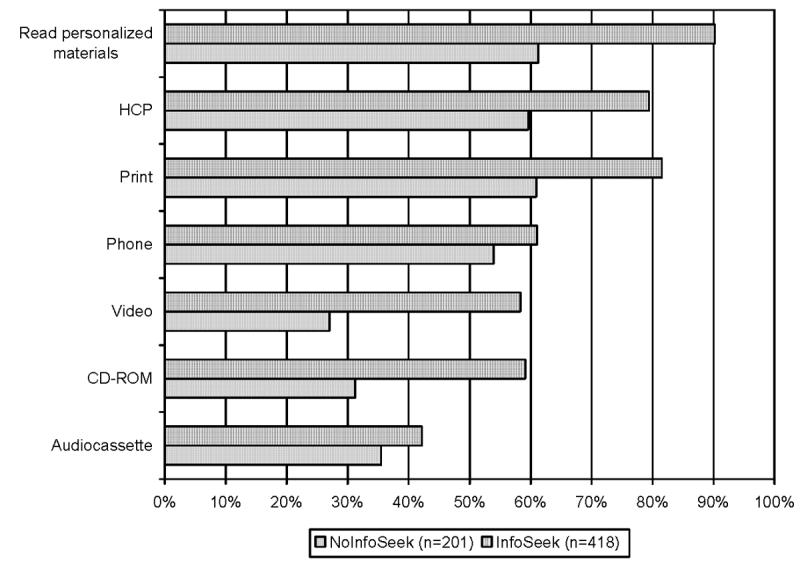
Cancer Survivors Would Use These Information Carriers or Channels
Despite these differences, when asked to rank their level of confidence in their ability to find cancer information, if needed, both groups rated themselves as confident-very confident (InfoSeek mean 1.4 and NoInfoSeek mean 1.5 on a very confident =1 to not at all confident = 4 scale). These findings were not significantly different by group or time since diagnosis.
4. Discussion and Conclusion
4.1 Discussion
The comprehensive model of information seeking provided a conceptual model to explore information seeking behaviors of cancer survivors and associated antecedents and information carrier factors of survivors who did and did not seek cancer information. Two out of three cancer survivors sought cancer information in an analysis of 619 cancer survivors. Differences were found between those who did and did not seek information in both antecedent and information carrier factors. Age, gender, income, and having a regular provider were predictors for information seeking. While other studies identified education and health status as additional antecedent factors [8, 13, 31, 43-45], these factors did not contribute to our model of information seeking. Income, however, may be a proxy for education. A recent survey from the Health on the Net Foundation found the education gap for using the Internet was narrowing between those with a college education and those with high school or less; non-university educated respondents were increasingly using the Internet for health information [46]. One factor that was more consistent with other information seeking studies was being ‘younger’ (less than 65 years old) and may reflect the general health evolution from more passive to active participation in health care. Thus, age may not remain an important variable as ‘boomers’ get older since they bring a more active approach to their health care [47].
Similar to other studies, we found that most survivors would prefer to get their health information from their health care providers [19, 26, 28, 31, 45, 48]. Our study found that information seekers were more likely to have others look for cancer information for them. These data did not provide insight as to the interactions between survivors and others helping to look for information but this relationship should be explored further. Other, more passive sources of information may also be useful in reaching the nonseeker group [49]. Information seekers identified a willingness to use a wider variety of mediated information carriers or sources than participants who did not seek cancer information. In a recent study by Basch and colleagues [25], 85% of Internet users also used other print sources of information.
Even though both groups preferred receiving information from their health care providers, information seekers used the Internet more often than they consulted their HCP because it was convenient, had a lot of information, and was available when needed. Internet use also improves users’ understanding of health issues and enhances patient-physician communication, and for some, led to enhanced coping and lessened anxiety [43, 46, 48, 50]. The Internet has become an important channel for the exchange of cancer information and support [28, 30, 48, 51, 52, 52]. In this study, 61% of information seekers had access to the Internet but only 60% of those actually used this channel to look for cancer information. For many cancer survivors, the Internet remains difficult to access and complicated to use. This is despite the fact that Internet access has steadily been increasing for Americans; according to the October 2005 Pew Internet & American Life Project, 68% of adults now have access. Barriers regarding finding websites and their ease of use can be addressed by developing better websites (see www.usability.gov) and not relying just on search engines as a hit or miss approach to finding a credible site for cancer information. Even those who access information from the Internet preferred interpersonal information sources, primarily from their health care provider, and sought other mediated sources when needed. This personal and trusted interaction between health care provider and patient tailors information to the patient’s needs. While more easily accessed than health care providers, Internet sources of information have yet to deliver the personalized and tailored information that survivors may seek. In a recent Health on the Net survey [46], 90% of patients would like their health care providers to recommend trustworthy websites. This combination approach may be more effective in meeting survivors’ information needs.
It is not clear whether access to health information (either by HCP or Internet) or coping style influences information seeking behaviors. Information seeking or avoidance as a coping style was not assessed in this study, leaving the question unanswered as to whether lack of access or intentional avoidance were factors for those who did not seek information. Avoiding or limiting information may be a method to decrease distress, manage ambiguity, and foster hope [2, 5, 11, 12, 18, 53]. In studies of other cancer survivors, information avoiders or ‘blunters’ were found to be less distressed than ‘monitors’ or information seekers [5]. Among studies of women with multiple sclerosis [20, 21], the amount and timing of desired information differed between monitors and blunters; blunters wanted more general information than monitors and at later time points across the illness trajectory. We do not know if similar patterns would be seen in cancer survivors or how information needs or behaviors would change over time.
Health information seeking behaviors have the potential to influence behavioral and psychological outcomes [4, 7, 9, 33]. Changes in our health care system have put more responsibility on patients to be active participants in decision making, self-care, and disease management. Active participation presumes the person will have the necessary information. It is not known what happens to cancer survivors if they do not want to be active participants who seek information or do not have the needed information.
4.2 Conclusion
Regardless of time since diagnosis, all cancer survivors preferred to get their cancer information from their health care provider. Most, however, turned to other sources, primarily the Internet, when seeking cancer information. While two thirds of cancer survivors in this study personally sought cancer information, one third did not. Age, gender, income and having a regular health care provider were all predictors of cancer information seeking behaviors.
4.3 Practice Implications
Although cancer information seeking has become the prevailing paradigm for cancer survivors, a group of survivors may not actively seek cancer information. Health care providers should assess or elicit information seeking behaviors and preferences from cancer survivors. Information avoiders could be assessed as to their barriers (literacy, Internet access) or coping style (‘monitors’ or ‘blunters’). Given that most survivors are willing to turn to the Internet, the quality and accessibility of the websites that are consulted are important determinants in its usefulness.3 Health care providers might want to harness the connection between themselves and the Internet and consider its’ use as an extension and enhancement to their patient interactions. Health care providers can screen existing websites for credibility and make specific recommendations to their patients. Likewise, providers can be instrumental in developing, contributing to, and evaluating trustworthy health or cancer-related websites. Research is needed related to how cancer information needs change over time in longitudinal studies of survivors and the impact of matching information seeking style and preferences with information delivery on psychological and behavioral outcomes.
Acknowledgements
D. Mayer was the recipient of doctoral scholarships from the American Cancer Society and ONS Foundation and a National Service Research Award from the National Institute of Nursing Research and was partially funded by NCI training grant R25 CA093831 (Kathi Mooney, PI). The authors thank Dr. Richard Moser and Dr. Bradford Hesse of the National Cancer Institute for their expert assistance with the HINTS database, Robert Rosofsky for programming assistance, Kathy Pikosky and Stefanie Jeruss for assistance with manuscript preparation.
Footnotes
Information seeking has been associated with the desire to participate in decision making but is a separate health behavior; one can desire information and not want to be an active participant in decision making and visa versa. [8-11] The focus of this paper is on information seeking.
Excluding non-melanoma skin cancers unless included another cancer in the ‘more than one cancer’ group
High quality and useful websites have greater availability of information, ease of finding information/navigation, trustworthiness/credibility, and accuracy. [46] The reader is referred to the principles set forth by the Health on the Net Foundation http://www.hon.ch/, Trust-e http://www.truste.org/, Internet Healthcare Coalition http://www.ihealthcoalition.org/, and URAChttp://www.urac.org/ to assess trustworthiness of health related websites.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Afifi WA, Weiner JL. Toward a theory of motivated information management. Commun Theory. 2004;12:167–90. [Google Scholar]
- 2.Brashers DE, Goldsmith DJ, Hsieh E. Information seeking and avoiding in health contexts. Hum Commun Res. 2002;28:258–71. [Google Scholar]
- 3.Derdiarian A. Informational needs of recently diagnosed cancer patients. A theoretical framework. Part I. Cancer Nurs. 1987;10:107–15. [PubMed] [Google Scholar]
- 4.Kreps G, Massimilia D. Cancer communications research and health outcomes: review and challenge. Comm Studies. 2002;53:318–36. [Google Scholar]
- 5.Miller SM. Monitoring versus blunting styles of coping with cancer influence the information patients want and need about their disease. Implications for cancer screening and management. Cancer. 1995;76:167–77. doi: 10.1002/1097-0142(19950715)76:2<167::aid-cncr2820760203>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 6.Wenzel L, Glanz K, Lerman C. Stress, Coping and Health Behavior. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education. Theory, Research, and Practice. 3rd Edn. Josey Bass; San Francisco,CA: 2002. pp. 210–39. [Google Scholar]
- 7.Johnson JD. Cancer-related information seeking (Health Communication) Hampton Press, Inc.; Cresskill, N.J.: 1997. [Google Scholar]
- 8.Cassileth BR, Zupkis RV, Sutton-Smith K, March V. Information and participation preferences among cancer patients. Ann Intern Med. 1980;92:832–6. doi: 10.7326/0003-4819-92-6-832. [DOI] [PubMed] [Google Scholar]
- 9.Czaja R, Manfredi C, Price J. The determinants and consequences of information seeking among cancer patients. J Health Commun. 2003;8:529–62. doi: 10.1080/716100418. [DOI] [PubMed] [Google Scholar]
- 10.Harris KA. The informational needs of patients with cancer and their families. Cancer Pract. 1998;6:39–46. doi: 10.1046/j.1523-5394.1998.1998006039.x. [DOI] [PubMed] [Google Scholar]
- 11.Manfredi C, Czaja R, Price J, Buis M, Janiszewski R. Cancer patients′ search for information. J Natl Cancer Inst Monogr. 1993:93–104. [PubMed] [Google Scholar]
- 12.Bennenbroek FT, Buunk BP, van der Zee KI, Grol B. Social comparison and patient information: what do cancer patients want? Patient Educ Couns. 2002;47:5–12. doi: 10.1016/s0738-3991(02)00018-6. [DOI] [PubMed] [Google Scholar]
- 13.Boudioni M, McPherson K, Moynihan C, Melia J, Boulton M, Leydon G, Mossman J. Do men with prostate or colorectal cancer seek different information and Rport from women with cancer? Br J Cancer. 2001;85:641–8. doi: 10.1054/bjoc.2001.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Derdiarian AK. Informational needs of recently diagnosed cancer patients. Nurs Res. 1986;35:276–81. [PubMed] [Google Scholar]
- 15.Fallowfield L, Ford S, Lewis S. No news is not good news: information preferences of patients with cancer. Psychooncology. 1995;4:197–202. doi: 10.1002/pon.2960040305. [DOI] [PubMed] [Google Scholar]
- 16.James C, James N, Davies D, Harvey P, Tweddle S. Preferences for different sources of information about cancer. Patient Educ Couns. 1999;37:273–82. doi: 10.1016/s0738-3991(99)00031-2. [DOI] [PubMed] [Google Scholar]
- 17.Luker KA, Beaver K, Leinster SJ, Owens RG. Information needs and sources of information for women with breast cancer: a follow-up study. J Adv Nurs. 1996;23:487–95. doi: 10.1111/j.1365-2648.1996.tb00010.x. [DOI] [PubMed] [Google Scholar]
- 18.Leydon GM, Boulton M, Moynihan C, Jones A, Mossman J, Boudioni M, McPherson K. Cancer patients′ information needs and information seeking behaviour: in depth interview study. BRIT MED J. 2000;320:909–13. doi: 10.1136/bmj.320.7239.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rees CE, Bath PA. The information needs and source preferences of women with breast cancer and their family members: a review of the literature published between 1988 and 1998. J Adv Nurs. 2000;31:833–41. doi: 10.1046/j.1365-2648.2000.01341.x. [DOI] [PubMed] [Google Scholar]
- 20.Baker LM. Monitors and blunters: patient health information seeking from a different perspective. Bibliotheca Medica Canadiana. 1994;16:60–3. [Google Scholar]
- 21.Baker LM. A new method for studying patient information needs and information-seeking patterns. Top Health Inf Manage. 1995;16:19–28. [PubMed] [Google Scholar]
- 22.Baker LM, Pettigrew KE. Theories for practitioners: two frameworks for studying consumer health information-seeking behavior. Bull Med Libr Assoc. 1999;87:444–50. [PMC free article] [PubMed] [Google Scholar]
- 23.Matthews AK, Sellergren SA, Manfredi C, Williams M. Factors influencing medical information seeking among African American cancer patients. J Health Commun. 2002;7:205–19. doi: 10.1080/10810730290088094. [DOI] [PubMed] [Google Scholar]
- 24.Case DO, Andrews JE, Johnson JD, Allard SL. Avoiding versus seeking: the relationship of information seeking to avoidance, blunting, coping, dissonance, and related concepts. J Med Libr Assoc. 2005;93:353–62. [PMC free article] [PubMed] [Google Scholar]
- 25.Basch EM, Thaler HT, Shi W, Yakren S, Schrag D. Use of information resources by patients with cancer and their companions. Cancer. 2004;100:2476–83. doi: 10.1002/cncr.20261. [DOI] [PubMed] [Google Scholar]
- 26.Guidry JJ, Aday LA, Zhang D, Winn RJ. Information sources and barriers to cancer treatment by racial/ethnic minority status of patients. J Cancer Educ. 1998;13:43–8. doi: 10.1080/08858199809528511. [DOI] [PubMed] [Google Scholar]
- 27.Gray RE, Fitch M, Greenberg M, Hampson A, Doherty M, Labrecque M. The information needs of well, longer-term survivors of breast cancer. Patient Educ Couns. 1998;33:245–55. doi: 10.1016/s0738-3991(98)00024-x. [DOI] [PubMed] [Google Scholar]
- 28.Mills ME, Davidson R. Cancer patients′ sources of information: use and quality issues. Psychooncology. 2002;11:371–8. doi: 10.1002/pon.584. [DOI] [PubMed] [Google Scholar]
- 29.Chapman K, Rush K. Patient and family satisfaction with cancer information: pamphlet evaluation. Can Oncol Nurs J. 2003;13:164–75. doi: 10.5737/1181912x133164175. [DOI] [PubMed] [Google Scholar]
- 30.Cline RJ, Haynes KM. Consumer health information seeking on the Internet: the state of the art. Health Educ Res. 2001;16:671–92. doi: 10.1093/her/16.6.671. [DOI] [PubMed] [Google Scholar]
- 31.Finney Rutten L, Arora N, Bakos A, Aziz N, Roland J. Information needs and sources of information among cancer patients: a systematic review of research (1980-2003) Patient Educ Couns. 2005;57:250–61. doi: 10.1016/j.pec.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 32.Järvelin K, Wilson TD. On conceptual models for information seeking and retrieval research. Information Research. 2003;9 paper 163. [Google Scholar]
- 33.Dutta-Bergman MJ. Health Attitudes, Health Cognitions, and Health Behaviors among Internet Health Information Seekers: Population-Based Survey. J Med Internet Res. 2004;6:E15. doi: 10.2196/jmir.6.2.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Cancer Institute HINTS 1 Final Report. 2003. http://cancercontrol.cancer.gov/hints/docs/final_report.pdf.
- 35.Nelson D, Rimer B, Kreps G, Hesse B, Viswanath K, Croyle R, Willis G, Arora N, Weinstein N, Alden W. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun. 2004;9:443–60. doi: 10.1080/10810730490504233. [DOI] [PubMed] [Google Scholar]
- 36.Groves R, Biemer P, Lyberg L, Massey J, Nicholls W, Waksberg J. Telephone Survey Methodology. John Wiley & Sons, Inc.; New York: 1988. [Google Scholar]
- 37.American Association for Public Opinion Research Standard Definitions: Final dispositions of case codes and outcome rates for surveys. 2004. http://www.apor.org.
- 38.Kiecolt KJ, Nathan LE. Secondary Analysis of Survey Data (Quantitative Applications in the Social Sciences) Sage Publications; Beverly Hills: 1985. [Google Scholar]
- 39.Kerlinger F, Lee H. Foundations of Behavioral Research. Harcourt College Publisher; Phildelphia: 2000. [Google Scholar]
- 40.Rizzo L. NCI HINTS sample design and weighting plan. Washington,D.C.: 2003. http://cancercontrol.cancer.gov/hints/docs/sampling_plan_final.pdf. [Google Scholar]
- 41.SAS Institute . SAS Version 9.1. SAS; Cary, North Carolina: 2004. [Google Scholar]
- 42.RTI International . SUDAAN Statistical Software, SAS 9-Callable. RTI; Research Triangle Park, N.C.: 2005. [Google Scholar]
- 43.Baker L, Wagner TH, Singer S, Bundorf MK. Use of the Internet and e-mail for health care information: results from a national survey. J AMER MED ASSOC. 2003;289:2400–6. doi: 10.1001/jama.289.18.2400. [DOI] [PubMed] [Google Scholar]
- 44.Carlsson M. Cancer patients seeking information from sources outside the health care system. Support Care Cancer. 2000;8:453–7. doi: 10.1007/s005200000166. [DOI] [PubMed] [Google Scholar]
- 45.Cotton A, Kaye LW, Downey R, Butler S. An early intervention model of caregiver services in rural primary care practices. Geriatr Nurs. 2004;25:240–1. doi: 10.1016/j.gerinurse.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 46.Health on the Net Foundation Analysis of 9th HON Survey of Health and Medical Internet Users. 2005. http://www.hon.ch/Survey/Survey2005/res.html.
- 47.Hesse BW, Nelson DE, Kreps GL, Croyle RT, Arora NK, Rimer BK. Trust and sources of health information. Arch Intern Med. 2005;165:1–7. doi: 10.1001/archinte.165.22.2618. [DOI] [PubMed] [Google Scholar]
- 48.Warner DA, Procaccino JD. Toward wellness: women seeking health information. J Am Soc Infor Sci Technol. 2004;55:709–30. [Google Scholar]
- 49.Dutta-Bergman MJ. Primary sources of health information: comparisons in the domain of health attitudes, health cognitions, and health behaviors. Health Commun. 2004;16:273–88. doi: 10.1207/S15327027HC1603_1. [DOI] [PubMed] [Google Scholar]
- 50.LaCoursiere SP, Knobf MT, McCorkle R. Cancer patients′ self-reported attitudes about the Internet. J Med Internet Res. 2005;7:e22. doi: 10.2196/jmir.7.3.e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rimer BK, Lyons EJ, Ribisl KM, et al. How new subscribers use cancer-related online mailing lists. J Med Internet Res. 2005;7:e32. doi: 10.2196/jmir.7.3.e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ziebland S, Chapple A, Dumelow C, Evans J, Prinjha S, Rozmovits L. How the internet affects patients′ experience of cancer: a qualitative study. BRIT MED J. 2004;328:564. doi: 10.1136/bmj.328.7439.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.van der Molen B, Hutchison G. Learning to live with cancer: the UK experience of a European patient education and Rport programme. Eur J Cancer Care (Engl) 1999;8:170–3. doi: 10.1046/j.1365-2354.1999.00158.x. [DOI] [PubMed] [Google Scholar]


