Abstract
Objectives
This systematic review evaluated the evidence for use of computer technologies to assess and reduce high-risk health behaviors in emergency department (ED) patients.
Methods
A systematic search was conducted of electronic databases, references, key journals, and conference proceedings. Studies were included if they evaluated the use of computer-based technologies for ED-based screening, interventions, or referrals for high-risk health behaviors (e.g., unsafe sex, partner violence, substance abuse, depression); were published since 1990; and were in English, French, or Spanish. Study selection and assessment of methodologic quality were performed by two independent reviewers. Data extraction was performed by one reviewer and then independently checked for completeness and accuracy by a second reviewer.
Results
Of 17,744 unique articles identified by database search, 66 underwent full-text review, and 20 met inclusion criteria. The greatest number of studies targeted alcohol/substance use (n = 8, 40%), followed by intentional or unintentional injury (n = 7, 35%) and then mental health (n = 4, 20%). Ten of the studies (50%) were randomized controlled trials; the remainder were observational or feasibility studies. Overall, studies showed high acceptability and feasibility of individual computer innovations, although study quality varied greatly. Evidence for clinical efficacy across health behaviors was modest, with few studies addressing meaningful clinical outcomes. Future research should aim to establish the efficacy of computer-based technology for meaningful health outcomes and to ensure that effective interventions are both disseminable and sustainable.
Conclusions
The number of studies identified in this review reflects recent enthusiasm about the potential of computers to overcome barriers to behavioral health screening, interventions, and referrals to treatment in the ED. The available literature suggests that these types of tools will be feasible and acceptable to patients and staff.
The emergency department (ED) is well situated to play a central role in identifying and addressing critical high-risk health behaviors. ED patients are more likely than the general U.S. population to report risky health behaviors, such as use of alcohol, drugs, and tobacco; involvement in violence; and unsafe sexual behavior.1–3 Many ED patients endorse more than one of these risky behaviors, placing them at even higher risk of subsequent illness and injury.4
The Society for Academic Emergency Medicine (SAEM) has recognized that emergency care “includes preventive and educational, as well as curative, medical service.”5 However, there are attitudinal, cultural, administrative, educational, technological, and systems barriers to integrating behavioral health measures so that they become a routine part of emergency care.6 Emergency physicians receive little training in the assessment of patients’ psychosocial or behavioral health risks or in the skills needed to address these problems.7 Many EDs struggle with long wait times, high acuity, limited budgets, and insufficient staff and are challenged to add preventive programs to their scope of practice.8
One proposed solution to these relatively fixed barriers to ED behavioral health interventions is the use of computer technology. Computers offer the potential of delivering cost-effective, individually tailored, evidence-based interventions for an array of health behaviors; reducing the time and resources needed for implementation of behavioral health measures; and allowing the ED to provide such measures consistently and with uniform quality. Importantly, computer-based screening and interventions are likely to be highly acceptable to patients. In national samples, over three-fourths of American Internet users report using the Internet to access health information.9 A recent study showed that many ED patients show interest in and even preference for technology-based interventions for a wide variety of behavioral health topics.10 A meta-analysis evaluating the efficacy of computer-delivered interventions to promote healthy behaviors in outpatient (non-ED) settings concluded that participants who received these interventions improved their knowledge, attitudes, and intentions toward changing their high-risk health behavior.11
A growing number of studies are examining the use of computers for behavioral health screening or interventions in the ED setting. However, this emerging literature has not been synthesized to allow recommendations for use of technology for targeted health issues or to formulate recommendations for future directions in research. The objectives of this systematic review were to evaluate the existing evidence for use of computer technologies in addressing health behaviors in EDs, to assess the quality of the existing literature, and to identify notable gaps in research on computer technology for behavioral health efforts in the ED.
METHODS
Search Strategy
For this systematic review, the research team worked in conjunction with a medical research librarian to develop and implement a systematic search strategy. The search was conducted in 14 databases: Academic Search Premier, CINAHL, Cochrane Central Register of Controlled Trials, Cochrane Reviews, Cochrane, Database of Abstracts of Reviews of Effects, EMBASE, Grey Literature Report, Health Technology Assessments Database, Nursing at OVID, ProQuest Theses and Dissertations, PsychInfo, PubMed, and SocIndex. We also searched ClinicalTrials.gov for ongoing studies and contacted investigators of pertinent studies to determine if there were studies pending publication. Last, we hand-searched the reference sections of all included articles and related review articles to identify other potentially relevant studies. An initial search was performed in December 2010. A final search was performed in February 2011 to capture any newly published articles. Data extraction and synthesis were conducted from March to June 2011.
Search terms included emergencies, emergency service, emergency medicine, accident and emergency, casualty, electronic mail, Internet, computers, software, technology, wireless, mobile, laptop, and social network. The full list of search terms and a detailed search strategy can be found in Data Supplement S1 (available as supporting information in the online version of this paper). Articles selected were limited to those published in English, Spanish, or French language and those published in or after 1990.
Study Selection
Studies were included if they employed computer technology for behavioral screening, interventions, and/or referrals for patients presenting to the ED and if they used computers to address risky behaviors (e.g., unsafe sex, partner violence, substance abuse, depression). We did not use standard or uniform definitions of the individual high-risk behaviors, but accepted the authors’ definition of these behaviors. Studies were excluded if they used computers solely to improve documentation, for follow-up after general ED care, or for detection or care of chronic medical illnesses. Studies were also excluded if they used research assistants, social workers, or nurses to improve ED-based behavioral screening, interventions, or referrals, unless the key component of the intervention involved computers. Both observational and experimental studies were included. If multiple articles were published analyzing the results of a single study (e.g., a preliminary analysis followed by a final analysis), the most comprehensive or final article was retained.
One study investigator (NA) performed an initial screen of all titles to identify potentially eligible articles and to eliminate duplicates across databases. Two study investigators (EKC and MLR) repeated the screen with a sample (200 articles) from the full list of titles to verify the quality of the initial screen. EKC and MLR then independently reviewed the abstracts of each retained article. If at least one investigator felt a study was potentially eligible based on abstract review, the full manuscript was obtained. The same two study investigators (EKC and MLR) then independently performed a review of the full manuscripts to determine if the study met all of the inclusion criteria. Any discrepancies in opinion were resolved by discussion with a fourth study investigator (EDB).
Data Abstraction and Analysis
Information on each eligible study was collected using a standardized data abstraction form that captured study design, study characteristics, patient population, target behavior, description of the innovation or intervention, outcomes, and results. One reviewer (EKC or MLR) extracted data for each study, with accuracy of information confirmed by a second reviewer (EKC or MLR). Given the broad range of topics included in our search, meta-analysis of the data was not possible; studies were analyzed descriptively only.
Quality Assessment
Eligible studies were assessed for methodologic quality and risk of bias using a modification of the criteria developed by Downs and Black.12 The Downs and Black instrument uses 27 criteria assessing the quality of reporting, power, and internal and external validity of a research study. To optimize the uniformity of scoring, we simplified the two subscales with multicategorical answer options to dichotomous answer options, making the maximum score possible 27. We divided the total score into tertiles and considered scores of 19 to 27 “high quality,” scores of 10–18 “moderate quality,” and scores 9 or below “low quality.”13,14 Two investigators (EKC and MLR) independently completed quality scoring of each study; in case of discrepancy, a third investigator (EB) was involved and disagreements were resolved through consensus. Inter-rater reliability was determined by calculating a κ statistic.
RESULTS
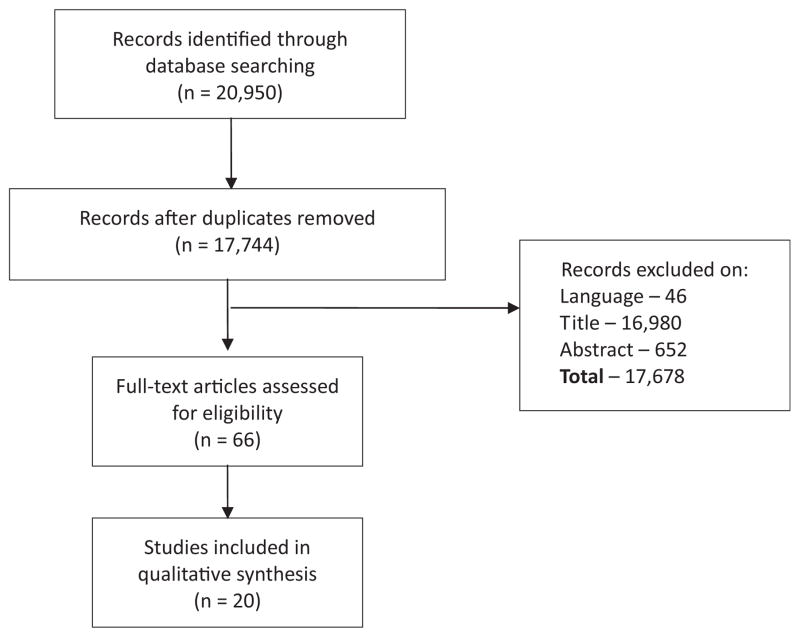
The study selection process is outlined in Figure 1. Of 685 studies retained after review of titles, 66 full-text articles were evaluated, and 20 met inclusion criteria for the review. Although the search included studies published from 1990 to the present, the eligible studies were all published since 2001. Eight (40%) of the eligible studies were federally funded; the remaining 12 studies were supported by state or provincial governments or by private corporations or foundations. The greatest number of ED-based computer studies targeted alcohol/substance use (n = 8, 40%), followed by injury (intentional or unintentional; n = 7, 35%) and then mental health (n = 4, 20%). One study15 addressed both alcohol use and violence and was counted in both categories. Most (n = 19, 95%) were conducted at a single center. Two studies (10%) included non–English-speaking populations. Table 1 summarizes the reviewed studies’ characteristics, including the behavioral target and the function or functions of the computer innovation tested.16–34
Figure 1.
Study selection.
Table 1.
Study Characteristics
| Behavioral Target | First Author (Year) | Country | Project Purpose
|
||
|---|---|---|---|---|---|
| Screening | Interventions | Referral | |||
| Alcohol/substance use | Bendtsen (2007)16 | Sweden | X | ||
| Boudreaux (2009)17 | United States | X | X | ||
| Karlsson (2005)18 | Sweden | X | X | ||
| Maio (2005)19 | United States | X | |||
| Neumann (2006)20 | Germany | X | X | ||
| Trinks (2010)21 | Sweden | X | X | ||
| Vaca (2010)22 | United States | X | X | X | |
| Alcohol and youth violence | Walton (2010)15 | United States | X | ||
| IPV | Houry (2008)23 | United States | X | X | |
| MacMillan (2006)24 | Canada | X | |||
| Rhodes (2002)25 | United States | X | |||
| Rhodes (2006)26 | United States | X | |||
| Trautman (2007)27 | United States | X | X | ||
| Unintentional injury | Gielen (2007)28 | United States | X | X | |
| Mental health | Claassen (2005)29 | United States | X | ||
| Fein (2010)30 | United States | X | |||
| Schriger (2001)31 | United States | X | |||
| Schriger (2005)32 | United States | X | |||
| HIV risk behaviors | Merchant (2009)33 | United States | X | X | |
| Multiple health behaviors | Rhodes (2001)34 | United States | X | X | |
IPV = intimate partner violence.
Tables 2 through 5 provide further details of individual studies by topic, including data on key variables and quality assessment scores. The single paper addressing both violence and alcohol use15 is listed in Table 2. Inter-rater reliability for the quality scores was high, with 24 discrepancies out of 540 data points (96% concurrence, κ = 0.67).
Table 2.
Alcohol and Substance Use Studies
| Study Design | First Author (Year) | Target Population | Experimental Condition (Length of Participation)* | Comparison Condition(s) | Primary Outcome(s) | Sample Size† | Main Results | QAS |
|---|---|---|---|---|---|---|---|---|
| Cross-sectional | Karlsson (2005)18 | Adult (18–70) patients | Computer screening and tailored printout of advice (one time, 2 minutes) | None | Acceptability | 44 | Acceptable: most patients felt positive about ED alcohol screening and computerized screening and tailored printouts. | 11 |
| Vaca (2010)22 | Adult (≥18) patients | Bilingual computerized alcohol SBIRT kiosk (one time, 1–8 min) | None | Feasibility‡ and acceptability | 5,103 | Feasible and acceptable. Most patients reported ease of use and comfort with computers. | 15 | |
| Prospective cohort | Boudreaux (2009)17 | Adult (≥18) patients in the ED and chest pain observation unit | Computerized screen and tailored referrals regarding drugs, alcohol, tobacco (one time, median 13 minutes) | None | Feasibility and acceptability | 85 patients, 51 providers | Feasible and acceptable: high mean patient and ED and substance use provider satisfaction scores. Low use of treatment referrals. | 19 |
| Quasi-experimental | Bendtsen (2006)16 | ED nurses | Computerized screening and brief intervention of patients (eSBI) (one time) | Usual care, in period before implementation of eSBI | Feasibility and acceptability to nurses | 48 nurses | Modest acceptability to nurses; low utilization. | 10 |
| RCT | Maio (2005)19 | Adolescent (14–18) patients with minor injury | Interactive computer program (one time, mean 25 minutes) | Usual care | Alcohol misuse | 580 (at 12 months) | No effect for general study population; decreased alcohol use among subgroup of risky drinkers. | 24 |
| Neumann (2006)20 | Adult (≥18) at-risk drinkers presenting due to injury | Computerized screening and tailored feedback and advice on alcohol use (one time) | No intervention | At-risk drinking | 660 (at 12 months) | Decreased alcohol use at 12 months but proportion of at-risk drinkers did not change. | 19 | |
| Trinks (2010)21 | Adult (18–69) patients | Computerized screening and tailored, printed feedback and advice on alcohol use (one time) | Short feedback with information on risk level of drinking | Patient participation and effectiveness for reducing alcohol use at 6 months | 93 (at 6 months) | Only 41% completed the intervention and only 17% follow-up; no difference in 6-month alcohol use. | 15 | |
| Walton (2010)15 | Adolescent (14–18) patients | Computerized brief intervention for violence and alcohol (one time, mean 35 minutes) | Control (brochure with community resources) or therapist brief intervention | Self-reported peer violence and alcohol use and related consequences | 726 | Decreased alcohol consequences at 6 months. No decrease in self-reported alcohol use and involvement in violence. | 22 |
QAS = quality assessment score; SBIRT = Screening, Brief Intervention and Referral to Treatment.
If duration of intervention is not provided, it was not mentioned in the article.
Sample size reported was that used in the main analysis. In general, sample at final follow-up was used, unless authors reported intention-to-treat analysis, in which case the number of all participants randomized to treatment was used.
The definition of feasibility, and measures used to assess it, varied from study to study.
Table 5.
Other Studies
| Study Design | First Author (Year) | Target Population | Experimental Condition (Length of Participation)* | Comparison Condition(s) | Primary Outcome(s) | Sample Size† | Main Results | QAS |
|---|---|---|---|---|---|---|---|---|
| Quasi-experimental | Rhodes (2001)34 | Adult (18–65) patients | Computerized survey and tailored printout of recommendations regarding a variety of behavioral risk factors (one time, mean 18 minutes) | Usual care | Feasibility‡ and acceptability; recall of health information | 454 | Feasible and acceptable; increased recall of receiving health information. | 17 |
| RCT | Merchant (2009)33 | Adult (18–64) patients | Computerized screening and tailored feedback regarding HIV risk behaviors with feedback (one time, 10–15 minutes) | Screening only | Self-perceived risk for current HIV infection | 566 | Screening alone significantly increased self-perceived HIV risk; no significant increase for screening and feedback. | 21 |
RCT = randomized controlled trial; QAS = quality assessment score.
If duration of intervention is not provided, it was not mentioned in the article.
Sample size reported was that used in the main analysis. In general, sample at final follow-up was used, unless authors reported intention-to-treat analysis, in which case the number of all participants randomized to treatment was used.
The definition of feasibility, and measures used to assess it, varied from study to study.
Computer-based ED Alcohol and Substance Use Innovations
Among the eight studies addressing alcohol and substance use (Table 2),15–22 four (50%) were randomized controlled trials (RCTs) that employed computer technology to deliver interventions aimed at reducing risky drinking,15,19–21 with measured outcomes of alcohol consumption. The remaining studies’ outcomes measured intervention feasibility and acceptability for patients and/or providers. Many of these studies used the standard ED care as a control group (30%) or had no comparison condition (25%). Clinical outcomes for the four RCTs included alcohol use; one study15 additionally measured negative social consequences of alcohol use (e.g., missed school, trouble getting along with friends). Overall, the studies showed acceptability and feasibility and some evidence of efficacy in reducing high-risk alcohol use.
Computer-based ED Violence and Unintentional Injury Interventions
Of the seven studies that addressed violence or unintentional injury in the ED23–28 (Table 3 and Walton et al.15), five23–27 targeted intimate partner violence (IPV). The IPV studies largely focused on screening, with limited interventions. Most of the outcomes measured were proximal, occurring within the initial ED visit, such as detected prevalence of IPV, physician documentation, and provision of referrals to services. Only Houry et al.23 measured occurrence of IPV after the ED visit. The study by MacMillan et al.24 was the only one to provide a comparison with an alternative, nontechnological means of identifying IPV. Overall, these studies showed high feasibility and acceptability of computerized screening and few negative consequences.
Table 3.
Injury Studies
| Study Design | First Author (Year) | Target Population | Experimental Condition (Length of Participation)* | Comparison Condition(s) | Primary Outcome(s) | Sample Size† | Main Results | QAS |
|---|---|---|---|---|---|---|---|---|
| IPV | ||||||||
| Cross-sectional | Rhodes (2002)25 | Adult (18–65) patients | Computerized screening and tailored printed recommendations (one time, mean 17 minutes) | Usual care | Feasibility,‡ acceptability, IPV detection rates | 470 | Higher physician documentation of IPV in computer-screened group. | 16 |
| Prospective cohort | Houry (2008)23 | Adult (18–55) patients | Computerized screening and referrals (one time) | N/A | Safety and use of referrals | 3,083 (in ED); 1,037 (9-1-1 call follow-up); 131 (at 3 months) | No significant safety issues; reduced 9-1-1 calls; relatively high use of resources at 3-month follow-up. | 17 |
| Quasi-experimental | Trautman (2007)27 | Female adult (≥18) patients | Computerized screening (one time, mean 6 minutes) | Computerized health survey without IPV questions | Screening, detection, referral, and services for IPV | 1,005 | Higher completion of screening, higher detection of IPV, and higher receipt of referrals and services. | 18 |
| RCT | MacMillan (2006)24 | Female adult (18–64) patients | Computerized screening (one time) | Face-to-face interview or written self-completed questionnaire | Acceptability and detection of IPV | 768§ | Acceptable to patients. Computer did not detect higher prevalence of IPV. | 18 |
| Rhodes (2006)26 | Female adult (18–65) patients | Computerized screening (one time, mean 18 min) | Usual care | IPV disclosure to and discussion with providers; receipt of services | 871 | Rates of IPV discussion, disclosure, and referral to services. | 23 | |
| Pediatric injury prevention | ||||||||
| Gielen (2007)28 | Parents of pediatric ED patients (4–66 months) | Computerized tailored injury prevention intervention (one time) | Report on unrelated child health topics | Safety knowledge and behaviors regarding car seat, smoke alarm, poison storage safety | 901 | Higher safety knowledge, higher use of child safety seats. | 23 | |
IPV = intimate partner violence; QAS = quality assessment score.
Sample size reported was that used in the main analysis. In general, sample at final follow-up was used, unless authors reported intention-to-treat analysis, in which case the number of all participants randomized to treatment was used.
If duration of intervention is not provided, it was not mentioned in the article.
The definition of feasibility, and measures used to assess it, varied from study to study.
Study was conducted in multiple sites; number listed represents size of subsample recruited from the ED.
Computer-based ED Mental Health Interventions
As with the injury studies, the mental health studies (Table 4) focused primarily on patient screening.29–32 Two studies (50%) were RCTs31,32 of a computer-based screening program that included physician notification of the results of the mental health screen. Outcomes included rate of detection of occult psychiatric problems, referrals, and receipt of services; none of the studies measured clinical outcomes related to the psychiatric conditions. None of the studies compared the technological innovation with a non–technology-based process. Overall, these studies showed high acceptability and feasibility of screening, but limited clinical outcomes.
Table 4.
Mental Health Studies
| Study Design | First Author (Year) | Target Population | Experimental Condition (Length of Participation)* | Comparison Condition(s) | Primary Outcome(s) | Sample Size† | Main Results | QAS |
|---|---|---|---|---|---|---|---|---|
| Cross-sectional | Claassen (2005)29 | Adult (≥18) patients with nonpsychiatric chief complaints | Computerized bilingual mental health screening (one time, 6 minutes) | N/A | Feasibility‡ and detection | 1,590 | Feasible to administer; high levels of occult suicidality compared with existing literature. | 9 |
| Fein (2010)30 | Adolescents (14–18) presenting to the ED with nonpsychiatric complaints | Brief computerized mental health screen (one time, 10 minutes) | Usual care, in the 19 months prior to implementation | Feasibility, detection, and social worker or psychiatrist assessment | 11,201 | Feasible; small but significantly increased identification and assessment of patients with psychiatric problems. | 17 | |
| RCT | Schriger (2001)31 | Adult (≥18) patients with diffuse or unusual complaints/behavior | Computerized psychiatric screening interview (one time, 5–10 minutes) with physician notification | Physician not notified of screening results | Detection, consultation or referral | 190 | No difference between groups in psychiatric diagnosis, consultation or referral. | 20 |
| Schriger (2005)32 | Adult (≥18) ED patients with “nonspecific somatic complaints” | Computerized psychiatric screen (one time, 2–35 minutes) with patient and physician notification | Screening only, or screening plus notification of patients only | Acceptability, detection and use of referrals | 95 | High acceptability; high rates of occult mental illness; trend toward increased referral with patient and physician notification. | 14 |
QAS = quality assessment score.
If duration of intervention is not provided, it was not mentioned in the article.
Sample size reported was that used in the main analysis. In general, sample at final follow-up was used, unless authors reported intention-to-treat analysis, in which case the number of all participants randomized to treatment was used.
The definition of feasibility, and measures used to assess it, varied from study to study.
Other Computer-based ED Interventions
Of the remaining two studies (Table 5), one34 used a computerized survey to screen for a variety of health behaviors, including drug and alcohol use, cardiovascular health risk behaviors, high-risk sexual behaviors, depression, and other “injury-prone behaviors.” This study measured acceptability, feasibility, and knowledge retention, but not actual behavior change. Merchant et al.33 used audio computer-assisted self-interview technology to increase ED patient attitudes to their own HIV risk; however, actual risk behaviors were not measured.
DISCUSSION
There are many barriers to implementing interventions for behavioral health issues in the ED setting. ED clinicians work in a high-volume, high-acuity setting with significant time constraints and receive little training in providing assessments or interventions for common problems such as substance abuse, smoking cessation, involvement in violence, or HIV risk. The institutional resources available for management of these issues are highly variable but generally insufficient for the large number of patients who might benefit from them.35,36 Studied behavioral interventions in the ED setting are often performed by social workers or case managers, yet the lack of availability of these resources, especially in remote or small EDs,37 limits the dissemination of treatments designed to be performed by these individuals. At the same time, many ED patients lack a consistent source of follow-up care, so failing to address these health issues during the visit may mean failing to take advantage of individuals’ sole point of contact with health care.
Computer technology-based screening, interventions, and referrals have several clinical advantages that make them potentially advantageous for use in the ED setting. 38 They provide a sense of anonymity and privacy and may increase reporting of unhealthy behaviors.26,39 They require little direct clinician involvement. They can be adapted to be culturally and linguistically specific, and audio capabilities allow them to be used among low-literacy individuals. They can provide individualized health information to participants immediately and in an engaging manner. They are able to store information so that progress over time can be accurately monitored and reviewed with the participant during follow-up after the ED visit. They minimize the bias that can arise in clinical relationships. An intervention, if proven effective, may be able to be disseminated while maintaining treatment fidelity among clinical sites.
This review supports the promise of computer-based technology as a means to filling a recognized health care gap in the ED. All the studies we identified were published within the past 10 years, reflecting the surge of interest and investment in applying emerging technologies to behavioral health problems. The broad range of health issues studied within a relatively short time period speaks to the many areas ED clinicians are eager to address—and likely feel constrained from addressing—in their current practice. While screening is arguably the simplest, and perhaps the most obvious, use of technology in the ED, a number of studies used computers in more core patient care functions, such as creating personalized referrals to treatment services or providing interactive interventions.
However, this literature review also identifies many areas for growth in the research on technology use for behavioral change in the ED. First, there are notable gaps in the types of risky health behaviors addressed by studied technologies. Most of the existing studies addressed alcohol or substance abuse; within this category, there was only one study examining drug use and no studies addressing tobacco use. Most of the computer-based work on violence examined IPV, with little directed toward youth violence and nothing directed toward other types of community violence, elder violence, or child abuse. Only one study addressed unintentional injuries, and only one addressed high-risk sexual behaviors. Walton’s intervention for alcohol use and violence among adolescents was the sole study to acknowledge the importance of addressing co-occurring high-risk behaviors together.
Some studies identified clinical or behavioral outcomes: four of the substance use intervention studies measured alcohol use before and after the ED intervention, with one measuring negative social consequences of alcohol use. One violence-related study measured occurrence of IPV—not just use of resources—after the ED visit. However, the majority of the studies, even the experimental studies, lacked patient-related outcomes. Many lacked comparison against valid nontechnological interventions and instead used “usual care” as the comparison group, presuming that the only option to technology-based interventions is no treatment at all. In some cases, this may be attributable to the lack of current nontechnological evidence-based practices, such as in the treatment of IPV or mental health problems identified in the ED setting. In other cases, this shortcoming reflects the early stage of research on implementing computer-based technologies into the ED setting. Feasibility and acceptability were still the primary questions for many researchers, as demonstrated by the 55% of studies in our review that focused on these topics.
Additionally, while many of the studies we reviewed reported their technological innovation to be feasible and acceptable, and a few reported efficacy in reducing harmful behaviors, none as yet have addressed how sustainable these innovations will be. Can these technologies truly be disseminated to resource-poor areas? Can they be implemented in places that do not have significant resources of institutional support and information technology specialization? Technology-based interventions may be a solution to resource and time limitations in the ED, but they have high start-up costs and a commitment to maintenance. ED staff must be trained to use the technological program, device, or software. Hardware and software can break, malfunction, become outdated, or be vandalized or stolen; they must be replaced or updated on a regular basis. Commercial products are rapidly becoming available that may allow researchers and hospitals to develop computer-based resources with increasing ease and affordability; however, few studies in our review comment on the cost-effectiveness of their innovations or other practical potential limitations to long-term and wide-spread use of technologies. Most studies were single-center, making it as yet difficult to imagine how these innovations would function outside of the specific environment in which they were developed.
These are all challenges that surely accompany any major innovation in the systems we use to deliver health care. However, they bear recognition, lest our enthusiasm for incorporating computers to fill the gaps in emergency services prevent us from anticipating and addressing the challenges and costs specific to technology-based interventions.
Finally, most of the studies we identified used computers in the ED for fairly “traditional” functions, such as administering patient surveys or providing static health information. We anticipate that upcoming research will examine newer computer applications, such as social networking or telehealth applications, and employ computer technology for more advanced and complex functions, including delivering interactive and highly tailored ED-based interventions, performing patient boosters or follow-ups after the ED visit, and providing dynamic linkages to needed services.
LIMITATIONS
First, it is possible that we failed to include relevant studies, whether because we missed them in the initial search or erroneously excluded them when reviewing studies by title or abstract. Any studies published since our final review (in February 2011) would also not be included in this review. Our determinations of study quality were also subject to the biases of the study investigators.
We did take a number of steps to ensure that all eligible studies were included and that our assessments of quality were objective. We made our search as comprehensive as possible by including multiple, diverse, and redundant databases. We also had two investigators independently review abstracts and articles for inclusion and used a standardized process for achieving consensus to avoid reviewer fatigue and subjectivity and to minimize error. Nevertheless, a systematic review is ultimately a subjective process, and the possibility for error or bias remains.
Well-validated quality assessment instruments for both randomized and nonrandomized studies are lacking. Therefore, the process of quality scoring adds to the subjective nature of systematic review. Although Downs and Black has come to be accepted as a standard for assessing quality of studies and is commonly used in the medical literature, it is an unvalidated measure, and categorization into “high,” “moderate,” and “low” quality categories remains an imperfect and somewhat arbitrary process. This is all the more true given that we used a modified version of the scale to optimize its precision. We included the Downs and Black instrument to include some objective measure of the likelihood of bias and to put study findings in context of their methodologic rigor; however, judgment of the quality of individual studies should be moderated by an acknowledgement of the limitations of the scale itself.
While the studies we reviewed supported the feasibility of computer-based interventions, there are two caveats to this statement. First, there was wide variation in the criteria authors used to define feasibility, ranging from patient willingness to participate to the ability to incorporate the technology into existing ED functions; this discrepancy is reflected in the contradiction between the number of studies asserting feasibility and the lack of information provided on the technical and financial aspects of implementing these interventions. Second, it is likely that some researchers attempted technological innovations for health behaviors, but failed to initiate or completely implement them due to some of the potential barriers discussed. Such failures would not be represented in the published literature. Additionally, computer-based applications for behavioral modification that are commercially or privately developed are typically not formally tested in a clinical setting, so this study cannot begin to comment on their appropriateness or effectiveness for our population. While missing unpublished studies or unstudied technologies is not a flaw of our research methods, it is important to acknowledge that our review may disproportionately represent the successes and therefore paint a misleadingly rosy picture of these technologies.
CONCLUSIONS
Computerized tools hold great potential for overcoming the multiple barriers to behavioral health screening, interventions, and referrals to treatment in the ED. We identified 20 studies that examined the feasibility, acceptability, or efficacy of using computer technology in the ED to provide screening or services for a wide variety of common high-risk health behaviors. While initial findings suggest that these types of tools will be feasible and acceptable, further research is needed to establish their efficacy for meaningful health outcomes and to identify approaches to overcoming barriers to dissemination and sustainability.
Supplementary Material
Footnotes
The authors have no relevant financial information or potential conflicts of interest to disclose.
Supporting Information:
The following supporting information is available in the online version of this paper:
Data Supplement S1. Final search strategy.
The document is in PDF format.
Please note: Wiley Periodicals Inc. is not responsible for the content or functionality of any supporting information supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- 1.U.S. Preventive Services Task Force. Guide to Clinical Preventive Services. 2. Baltimore, MD: Williams & Wilkins; 1996. [Google Scholar]
- 2.Hirshon JM, Morris DM. Emergency medicine and the health of the public: the critical role of emergency departments in US public health. Emerg Med Clin North Am. 2006;24:815–9. doi: 10.1016/j.emc.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 3.Clancy CM, Eisenberg JM. Emergency medicine in population-based systems of care. Ann Emerg Med. 1997;30:800–3. doi: 10.1016/s0196-0644(97)70052-0. [DOI] [PubMed] [Google Scholar]
- 4.Bernstein SL. The clinical impact of health behaviors on emergency department visits. Acad Emerg Med. 2009;16:1054–9. doi: 10.1111/j.1553-2712.2009.00564.x. [DOI] [PubMed] [Google Scholar]
- 5.Bernstein E, Goldfrank LR, Kellerman AL, et al. A public health approach to emergency medicine: preparing for the twenty-first century. Acad Emerg Med. 1994;1:277–86. doi: 10.1111/j.1553-2712.1994.tb02446.x. [DOI] [PubMed] [Google Scholar]
- 6.McKay MP, Vaca FE, Field C, Rhodes K. Public health in the emergency department: overcoming barriers to implementation and dissemination. Acad Emerg Med. 2009;16:1132–7. doi: 10.1111/j.1553-2712.2009.00547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rhodes KV, Pollock DA. The future of emergency medicine public health research. Emerg Med Clin North Am. 2006;24:1053–73. doi: 10.1016/j.emc.2006.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rhodes KV, Gordon JA, Lowe RA. Preventive care in the emergency department, Part I: Clinical preventive services–are they relevant to emergency medicine? Society for Academic Emergency Medicine Public Health and Education Task Force Preventive Services Work Group. Acad Emerg Med. 2000;7:1036–41. doi: 10.1111/j.1553-2712.2000.tb02097.x. [DOI] [PubMed] [Google Scholar]
- 9.Fox S. Health Topics. Washington, DC: Pew Research Center; 2011. [Google Scholar]
- 10.Ranney M, Choo E, Wang Y, Baum A, Clark M, Mello M. Emergency department patient preferences for technology-based behavioral interventions [abstract] Acad Emerg Med. 2011;18(Suppl 1):10. doi: 10.1016/j.annemergmed.2012.02.026. [DOI] [PubMed] [Google Scholar]
- 11.Portnoy DB, Scott-Sheldon LA, Johnson BT, Carey MP. Computer-delivered interventions for health promotion and behavioral risk reduction: a meta-analysis of 75 randomized controlled trials, 1988–2007. Prev Med. 2008;47:3–16. doi: 10.1016/j.ypmed.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Comm Health. 1998;52:377–84. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Newton AS, Hamm MP, Bethell J, et al. Pediatric suicide-related presentations: a systematic review of mental health care in the emergency department. Ann Emerg Med. 2010;56:649–59. doi: 10.1016/j.annemergmed.2010.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Newton AS, Zou B, Hamm MP, et al. Improving child protection in the emergency department: a systematic review of professional interventions for health care providers. Acad Emerg Med. 2010;17:117–25. doi: 10.1111/j.1553-2712.2009.00640.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walton MA, Chermack ST, Shope JT, et al. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. JAMA. 2010;304:527–35. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bendtsen P, Holmqvist M, Johansson K. Implementation of computerized alcohol screening and advice in an emergency department–a nursing staff perspective. Accid Emerg Nurs. 2007;15:3–9. doi: 10.1016/j.aaen.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 17.Boudreaux ED, Bedek KL, Gilles D, et al. The Dynamic Assessment and Referral System for Substance Abuse (DARSSA): development, functionality, and end-user satisfaction. Drug Alcohol Depend. 2009;99:37–46. doi: 10.1016/j.drugalcdep.2008.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karlsson A, Bendtsen P. Acceptability of a computerized alcohol screening and advice routine in an emergency department setting–a patient perspective. Addict Behav. 2005;30:767–76. doi: 10.1016/j.addbeh.2004.08.022. [DOI] [PubMed] [Google Scholar]
- 19.Maio RF, Shope JT, Blow FC, et al. A randomized controlled trial of an emergency department-based interactive computer program to prevent alcohol misuse among injured adolescents. Ann Emerg Med. 2005;45:420–9. doi: 10.1016/j.annemergmed.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 20.Neumann T, Neuner B, Weiss-Gerlach E, et al. The effect of computerized tailored brief advice on at-risk drinking in subcritically injured trauma patients. J Trauma. 2006;61:805–14. doi: 10.1097/01.ta.0000196399.29893.52. [DOI] [PubMed] [Google Scholar]
- 21.Trinks A, Festin K, Bendtsen P, Nilsen P. Reach and effectiveness of a computer-based alcohol intervention in a Swedish emergency room. Int Emerg Nurs. 2010;18:138–46. doi: 10.1016/j.ienj.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Vaca F, Winn D, Anderson C, Kim D, Arcila M. Feasibility of emergency department bilingual computerized alcohol screening, brief intervention, and referral to treatment. Subst Abus. 2010;31:264–9. doi: 10.1080/08897077.2010.514245. [DOI] [PubMed] [Google Scholar]
- 23.Houry D, Kaslow NJ, Kemball RS, et al. Does screening in the emergency department hurt or help victims of intimate partner violence? Ann Emerg Med. 2008;51:433–42. doi: 10.1016/j.annemergmed.2007.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.MacMillan HL, Wathen CN, Jamieson E, et al. Approaches to screening for intimate partner violence in health care settings: a randomized trial. JAMA. 2006;296:530–6. doi: 10.1001/jama.296.5.530. [DOI] [PubMed] [Google Scholar]
- 25.Rhodes KV, Lauderdale DS, He T, Howes DS, Levinson W. Between me and the computer: increased detection of intimate partner violence using a computer questionnaire. Ann Emerg Med. 2002;40:476–84. doi: 10.1067/mem.2002.127181. [DOI] [PubMed] [Google Scholar]
- 26.Rhodes KV, Drum M, Anliker E, Frankel RM, Howes DS, Levinson W. Lowering the threshold for discussions of domestic violence: a randomized controlled trial of computer screening. Arch Intern Med. 2006;166:1107–14. doi: 10.1001/archinte.166.10.1107. [DOI] [PubMed] [Google Scholar]
- 27.Trautman DE, McCarthy ML, Miller N, Campbell JC, Kelen GD. Intimate partner violence and emergency department screening: computerized screening versus usual care. Ann Emerg Med. 2007;49:526–34. doi: 10.1016/j.annemergmed.2006.11.022. [DOI] [PubMed] [Google Scholar]
- 28.Gielen AC, McKenzie LB, McDonald EM, et al. Using a computer kiosk to promote child safety: results of a randomized, controlled trial in an urban pediatric emergency department. Pediatrics. 2007;120:330–9. doi: 10.1542/peds.2006-2703. [DOI] [PubMed] [Google Scholar]
- 29.Claassen CA, Larkin GL. Occult suicidality in an emergency department population. Br J Psychiatry. 2005;186:352–3. doi: 10.1192/bjp.186.4.352. [DOI] [PubMed] [Google Scholar]
- 30.Fein JA, Pailler ME, Barg FK, et al. Feasibility and effects of a Web-based adolescent psychiatric assessment administered by clinical staff in the pediatric emergency department. Arch Pediatr Adolesc Med. 2010;164:1112–7. doi: 10.1001/archpediatrics.2010.213. [DOI] [PubMed] [Google Scholar]
- 31.Schriger DL, Gibbons PS, Langone CA, Lee S, Altshuler LL. Enabling the diagnosis of occult psychiatric illness in the emergency department: a randomized, controlled trial of the computerized, self-administered PRIME-MD diagnostic system. Ann Emerg Med. 2001;37:132–40. doi: 10.1067/mem.2001.112255. [DOI] [PubMed] [Google Scholar]
- 32.Schriger DL, Gibbons PS, Nezami WA, Langone CA. Failure of a patient-centered intervention to substantially increase the identification and referral for-treatment of ambulatory emergency department patients with occult psychiatric conditions: a randomized trial. BMC Emerg Med. 2005;5:e2. doi: 10.1186/1471-227X-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Merchant RC, Clark MA, Langan TJ, Seage GR, Mayer KH, DeGruttola VG. Effectiveness of increasing emergency department patients’ self-perceived risk for being human immunodeficiency virus (HIV) infected through audio computer self-interview-based feedback about reported HIV risk behaviors. Acad Emerg Med. 2009;16:1143–55. doi: 10.1111/j.1553-2712.2009.00537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rhodes KV, Lauderdale DS, Stocking CB, Howes DS, Roizen MF, Levinson W. Better health while you wait: a controlled trial of a computer-based intervention for screening and health promotion in the emergency department. Ann Emerg Med. 2001;37:284–91. doi: 10.1067/mem.2001.110818. [DOI] [PubMed] [Google Scholar]
- 35.Birnbaum A, Calderon Y, Gennis P, Rao R, Gallagher EJ. Domestic violence: diurnal mismatch between need and availability of services. Acad Emerg Med. 1996;3:246–51. doi: 10.1111/j.1553-2712.1996.tb03428.x. [DOI] [PubMed] [Google Scholar]
- 36.Rockett IR, Putnam SL, Jia H, Smith GS. Assessing substance abuse treatment need: a statewide hospital emergency department study. Ann Emerg Med. 2003;41:802–13. doi: 10.1067/mem.2003.189. [DOI] [PubMed] [Google Scholar]
- 37.Choo E, Newgard CD, Lowe RA, Hall MK, McConnell KJ. Rural-Urban disparities in intimate partner violence resources in the emergency department. West J Emerg Med. 2010;12:178–83. [PMC free article] [PubMed] [Google Scholar]
- 38.Miller JH, Hester RK. Computer-based tools for diagnosis and treatment of alcohol problems. Alcohol Res Health. 2006;29:36–40. [PMC free article] [PubMed] [Google Scholar]
- 39.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280:867–73. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.