Abstract
Background
Neighborhood factors reported subjectively by residents and measured objectively at the census tract are both associated with adolescent alcohol, cigarette, electronic cigarette (e-cigarette), and marijuana (ATOD) use. Less clear is how these neighborhood factors are longitudinally associated with each substance. Equivocal findings may be due to lack of consideration of individual, peer, and family effect modifiers, which could help adolescents overcome exposure to stressful neighborhood environments.
Methods
We used multivariate logistic regressions with interaction terms to test whether parental monitoring, resistance self-efficacy (RSE) and being around peers who use ATOD modified the association between four subjective and objective neighborhood measures and odds of using each substance measured one year later among 2,539 high school students and college freshmen originally recruited from middle schools in Southern California.
Results
Census tract-level disadvantage was not longitudinally associated with ATOD use. However, perceptions of higher neighborhood disorganization, less social cohesion, and more neighborhood problems with alcohol and drug use were associated with higher odds of ATOD use. Higher RSE and weaker affiliations with peers who use ATOD consistently buffered negative effects of neighborhood disorganization and neighborhood problems with alcohol and drugs on past year ATOD use.
Conclusions
Community-level programs that increase social cohesion among neighbors, neighborhood monitoring of deviant behaviors, and better policing of open drug selling may prevent ATOD use. Programs should also target RSE and minimize affiliations with peers who use ATOD, which could reduce the magnitude of the association with ATOD, even for adolescents living in the most at-risk neighborhoods.
Keywords: Neighborhoods, youth, alcohol, cigarette, e-cigarette, marijuana, effect modification
1. Introduction
Alcohol, cigarettes, and marijuana are the most widely used substances in the U.S. with 38.3%, 17.5%, 29.0%, and 23.9% of 10th graders reporting past year alcohol, lifetime cigarette, lifetime electronic vaporizer such as electronic cigarette, and past year marijuana use, respectively (Johnston et al., 2016). Although a robust body of literature has identified individual, peer, and family risk and protective factors for alcohol, tobacco, and other drug (ATOD) use, the most effective prevention programs also include community-level influences (Griffin and Botvin, 2010). Thus, there has been increased attention on neighborhood factors that may influence adolescent ATOD use. Bronfenbrenner’s ecological systems theory (1979) purports that the entire ecological system, including neighborhood characteristics, interact with individual, peer, and family factors to influence adolescent behaviors such as ATOD use. Not including all of these levels of influence, and their potential interactive effects, may result in over or underestimating the effects of each of these factors. This is especially critical for the adolescent period when peers have an increasingly influential role in the risk of ATOD use (Connell et al., 2010; Creemers et al., 2010; D’Amico and McCarthy, 2006; Duan et al., 2009). In addition, adolescence is a time of rising independence and mobility (University of Minnesota, 2015), which affords greater exposure to their neighborhood environments. Social disorganization theory (Sampson, 1993) postulates that neighborhood environments matter when it comes to deviant behaviors such as ATOD use. For example, disorganized neighborhoods that are characterized by more crime, instability, and abandoned buildings tend to lack the resources to offer adolescents an alternative to deviancy. Examining how the magnitude of neighborhood effects vary by individual, peer, and family factors is critical to further clarifying the complex etiology of ATOD use and to inform the development of more efficient public health interventions and policies that can focus on multiple factors that represent the combination of greatest risk.
1.1. Associations Between Neighborhood Disadvantage (Objective Measures) and ATOD Use
To date, the majority of studies on neighborhoods and adolescent substance use focus on alcohol use only and census tract-level measures of family income, proportion of single-headed families, unemployment rates, education level, or residential stability. In a comprehensive review (Jackson et al., 2014), most studies did not find significant associations between disadvantage and alcohol use that may be partly attributable to lack of consideration of effect modifiers and the use of different definitions of neighborhood disadvantage. Many studies lack generalizability by focusing on samples with limited racial/ethnic diversity, or high-risk youth (Buu et al., 2009; Fite et al., 2009; Fuller et al., 2005; Jones-Webb and Karriker-Jaffe, 2013), and are older studies (Crum et al., 1996) that may not accurately reflect current neighborhood socioeconomic conditions or current ATOD use patterns.
Several studies have examined objectively measured neighborhood characteristics with cigarette and marijuana use. For example, three studies that examined neighborhood disorder measured by abandoned buildings (Furr-Holden et al., 2015; Furr-Holden et al., 2011; Tarter et al., 2009), found positive associations with marijuana use up to nine years later among a sample of approximately 200 19-year old predominantly White boys (Tarter et al., 2009), and approximately 400 predominantly Black youth followed 1–2 years after high school (Furr-Holden, 2011; 2015). Another study of 6th–9th grade Black adolescents found that neighborhood socioeconomic disadvantage was associated with an increased risk of transitioning from being offered marijuana to having marijuana use and problems (Reboussin et al., 2015). Diez-Roux and colleagues (2003) have shown that living in an area with higher neighborhood socioeconomic disadvantage is associated with higher odds of current cigarette use among adults aged 18–30 years. Other studies that have examined initiation of ATOD or injection drug use in relation to objective measures of neighborhood quality showing that neighborhood minority racial composition and education interacted with race to predict injection drug use initiation (Fuller et al., 2005) and that higher neighborhood disadvantage was associated with increased risk of ATOD initiation (Fite et al., 2009). However, these studies have limited generalizability because data came from small samples (approximately 100) of at-risk adolescents.
Overall, the existing literature on objective neighborhood measures that examine alcohol use as an outcome are mixed, and studies that examine cigarette or marijuana use have samples that are either relatively small or comprised of either predominantly Black or White adolescents. Some research suggests that neighborhood disadvantage has different effects depending on the substance (e.g., Crum et al., 1996), although more recent studies do not examine multiple substances. Moreover, no studies to date have examined neighborhood influences on e-cigarette use, a product which has increased rapidly in popularity in recently years (Singh et al., 2016) and has been associated with increased risk of subsequent cigarette use among adolescents (Leventhal et al., 2016; Wills et al., 2017). To address these limitations, we examine the longitudinal association with objective socioeconomic disadvantage on four different types of substances (alcohol, cigarettes, e-cigarettes, marijuana) in a diverse cohort of adolescents followed for one year using an index of neighborhood disadvantage.
1.2. Associations Between Self-Reported Neighborhood Factors (Subjective Measures) and ATOD Use
Examining perceived and objective neighborhood factors may provide different depictions of neighborhood environments in terms of risk for adolescent ATOD use (Hadley-Ives et al., 2000). Objective data can inform public health efforts by identifying populations living in high-risk areas using publically-available Census data. In contrast, self-reported perceptions of neighborhood quality may reflect more proximal effects on adolescents’ behaviors, thereby increasing the efficiency of prevention programs.
Similar to the literature on objective neighborhood measures, longitudinal studies on perceived neighborhood characteristics and ATOD use focus mainly on alcohol use and report equivocal findings on perceptions of neighborhood quality including social control, social capital, and collective efficacy. Some studies found no associations with alcohol use (Aslund and Nilsson, 2013; De Haan, 2010; Ennett et al., 2008; Fulkerson et al., 2008; Maimon and Browning, 2012), whereas others found greater perceived neighborhood disorganization was longitudinally associated with a composite measure of ATOD use among 521 African American youth (Lambert et al., 2004).
Two studies have examined both objective and perceived neighborhood characteristics. Reboussin and colleagues (2015) found that self-reported perceptions of neighborhood disorder and drug activity and objectively measured socioeconomic disadvantage were associated with the transition from marijuana offers to subsequent marijuana use and problems. Tucker and colleagues (2013) found that living in an area with higher unemployment rates was longitudinally associated with marijuana initiation, whereas unexpectedly, higher perceived neighborhood safety was associated with initiation of heavy drinking. Yet, this study used 1990 Census data in the National Longitudinal Study of Adolescent Health, which is a mostly-white sample. Although many studies have reported significant associations with self-reported neighborhood quality and substance use, those studies typically report a composite measure of substance use, or combine delinquency outcomes with substance use (Byrnes et al., 2011; Burlew et al., 2009; Choi et al., 2006; Hadley-Ives et al., 2000; Lambert et al., 2004; Joon Jang and Johnson, 2001). It is important to examine substances separately instead of a composite measure because of potentially different mechanisms by which neighborhood quality may influence ATOD use. For example, Tucker et al. (2013) hypothesized that lack of employment opportunities in the neighborhood was related to drug selling whereas the measure of perceived neighborhood safety may have reflected low parental supervision in the neighborhood increasing the likelihood of heavy drinking. We build on this study and others to also examine cigarette and e-cigarette use, and multiple subjective and objective neighborhood characteristics to test which aspects of neighborhoods are longitudinally associated with ATOD use in a racially/ethnically diverse sample.
1.3. Interactions of Neighborhood Effects By Individual, Peer, and Family Factors
Whereas some studies have examined effect modification by race/ethnicity (Browning, 2012; Choi et al., 2006; Fuller et al., 2005), we focus on modifiable factors that may serve an important role in helping adolescents overcome exposure to stressful environments. To our knowledge, only three longitudinal studies have examined interactions with modifiable factors. These studies have been limited by small samples, select populations with limited generalizability, or an inability to determine whether modifiable factors interacted with neighborhood factors for certain substances because of the use of a composite measure of substance use (Burlew et al., 2009; Xue et al., 2007; Tucker et al., 2013). Together, these studies suggest it may be important to distinguish between individual, peer, and family risk factors because they may modify neighborhood effects differently, depending on substance. Thus, we build on this previous work by longitudinally examining both subjective and objective measures of neighborhoods on risk of using four different types of substances (alcohol, cigarettes, e-cigarettes, and marijuana) in a diverse adolescent sample, and identifying individual (resistance self-efficacy), peer (associating with peers who use), and family (parental monitoring) factors shown in prior research to be important contributors to ATOD that may mitigate negative effects of poor neighborhood quality.
2. Material and Methods
2.1 Study Sample
Sixteen middle schools within three districts in southern California participated in an evaluation of a school-based substance use prevention program (D’Amico et al., 2012b). Schools were initially selected to participate across three districts to obtain a diverse sample and to have similar substance use rates at baseline. A total of 14,979 students across all 16 schools received parental consent forms; 92% (n = 13,785) of parents returned this form. Approximately 71% (n = 9,828) of parents gave consent for their child to participate and 94% (n = 8,932) of students who gave assent and completed the survey (D’Amico et al., 2012a; D’Amico et al., 2016; Tucker et al., 2015). The recruited sample was comparable to the racial/ethnic composition of the relevant school populations based on published demographic information for the schools. The intervention was a voluntary after-school program that sought to reduce alcohol and other drug use and ended in 2009. We then continued to follow two cohorts of youth (the original 6th and 7th graders) as they transitioned into high school. Loss to follow-up was not associated with demographics or risk behaviors, such as alcohol and marijuana use (D’Amico et al., 2016). The “baseline” data for analyses reported herein come from the web-based Wave 6 survey (completed May 2013–April 2014) when most participants were in 10th–12th grades and web-based Wave 7 survey (completed one year later May 2014–May 2015) when most participants were either in 11th or 12th grade, were no longer in school, or were in college. Almost 70% (4,366) of the 6,396 youth who were in 6th–7th grade at Wave 1 were located, contacted, and re-consented for the Wave 6 survey. Sixty-one percent (2,653) completed the web-based survey. Of the 2,653 students that completed Wave 6, 2,127 (80%) also completed Wave 7. From the 2,653 Wave 6 respondents, we excluded 114 respondents with potentially unreliable data determined by a quality-check question. The remaining 2,539 respondents constituted our analytic sample for all analyses in this paper. Survey responses are protected by a Certificate of Confidentiality from NIH. All materials and procedures were approved by the school districts, individual schools, and the institution’s IRB.
2.2 Sociodemographic Measures
Each survey asked students about their sex, age, grade, mother’s education, and race/ethnicity. Respondents initially classified themselves by ethnicity (Hispanic or not Hispanic) and then asked about race (DHHS, 2001). We then classified them as either Hispanic, non-Hispanic White (hereafter referred to as White), or Asian/Other/Multiracial (which included non-Hispanic Blacks). Response options for the highest level of education that their mother achieved were: did not finish high school, graduated from high school, some college, graduated from college, and don’t know. Information about grade level and current school were used to define an indicator identifying students that were in college at follow-up.
2.3 Neighborhood Measures
We used census tracts as a proxy for neighborhoods. Although neighborhoods may span more than a single tract, most U.S. epidemiological studies use census tracts as the unit of analysis (Krieger et al., 2003; Pickett et al., 2001) because census tract characteristics are shown to be robust predictors of health (Cockings et al., 2004; Krieger et al., 2001). Objective neighborhood disadvantage was an index created using an exploratory factor analysis to identify five census tract-level indicator variables which fit a single factor structure using the 2008–2012 American Community Survey data, described previously (Miles et al., 2015). The five indicator variables were median household income, level of education for the population 25 years and older (categories were less than a high school diploma or general education development (GED) equivalent; a high school diploma or GED equivalent, but not a bachelor’s degree; and a bachelor’s degree or higher), percent of the population age 16 and older that is unemployed, percent of households with children 18 years and younger that are female headed, and percent of households below the federal poverty level. The index was calculated using coefficients estimated from a confirmatory factor analysis (RMSEA=0.063 and CFI=0.958) using Mplus 7.11 (Muthén and Muthén, 2013). Neighborhood disadvantage values were mean standardized and ranged from −1.65 to 1.77. The value of this census tract-level variable was linked to each student using Wave 6 address data that was geocoded to the census tract using 2010-based Census definitions of census tracts. Geocoding was successful for 2,080 (82%) respondents (no P.O. Box, missing, or incomplete addresses). Missingness of census tract information was handled using multiple imputation methods noted below in Section 2.5.
The three subjective measures were identified using factor analysis of 19 survey items from validated scales that measured social control, social cohesion, disorder, problems with alcohol and drug use (Duncan et al., 2002; Sampson et al., 1997; Winstanley et al., 2008), and social capital from the Los Angeles Family and Neighborhoods Study (Carpiano, 2008). A scree plot suggested extracting three factors and an exploratory factor analysis with promax rotation revealed six items loading on neighborhood disorganization (a lot of crime, drug selling, street fights, empty or abandoned buildings, graffiti, and people often moving in and out of the neighborhood). Nine items loaded on a neighborhood cohesion factor (e.g., people willing to help neighbors, sharing the same values, how many adults in the neighborhood do you know, and likelihood that neighbors would do something about children skipping school or spray-painting graffiti). The remaining four items loaded on a factor we labeled neighborhood problems with alcohol and drugs (e.g., alcohol use/drug use/cigarette use among kids and teens is a problem) which we refer to hereafter as “problems with alcohol/drugs”. The score for each factor was the mean of the items that loaded most highly on each factor (Cronbach alphas: disorganization = 0.86; cohesion=0.74; problems with alcohol/drugs = 0.86). Each neighborhood factor ranged 1–5 and higher scores indicated higher values on the factor.
2.4 Potential Effect Modifiers
2.4.1 Resistance self-efficacy (RSE)
For RSE, respondents were asked three questions for each of the three substances assessed: “Suppose you are offered alcohol [cigarettes]/[marijuana] and you do not want to use it. What would you do in these situations: (A) your best friend is drinking alcohol [smoking cigarettes]/[using marijuana]; (B) you are bored at a party; and (C) all your friends at a party are drinking alcohol [smoking cigarettes]/[using marijuana]?” These three items were rated on a 4-point scale ranging from “I would definitely drink [use cigarettes]/[use marijuana]” to “I would definitely not drink [smoke cigarettes]/[use marijuana]” and scores were averaged (Ellickson et al., 2003) to develop a single RSE measure for each substance (range 1–4, Cronbach’s alpha = 0.95 (alcohol), 0.97 (cigarettes), 0.97 (marijuana)).
2.4.2 Affiliation with Peers Who Use ATOD
Adolescents were asked how often they were around other teens who are drinking alcohol [smoking cigarettes]/[using marijuana]. Higher values for each substance indicate higher affiliation with peers who use, which we refer to as “peer affiliation” (range = 1–4).
2.4.3 Parental monitoring
Parental monitoring was calculated using level of agreement (ranging 1–4) with five statements such as “When I am not at home, one of my parent(s) or guardian(s) knows where I am and whom I am with”; and “My family has clear rules about alcohol.” Responses were averaged such that higher values indicate more monitoring (Cronbach’s alpha = 0.79).
2.5 ATOD Use Outcomes
Past year ATOD use was assessed using well-established measures (Miech et al., 2016) that asked: “During the past year, how many times have you used or tried [one full drink of alcohol]/[cigarettes]/[electronic cigarettes or e-cigarettes]/[marijuana]? One full drink was defined in the survey as one regular size can/bottle of beer or wine cooler, one glass of wine, one mixed drink, or one shot glass of liquor. Respondents were specifically told not to include drinking a few sips or drinking for religious purposes. Responses ranged from “none”, “1 time” “2 times”, “3–10 times”, “11–20 times”, and “more than 20 times” and were dichotomized (1=“any past year use” versus 0=“no past year use”) due to infrequent responses at high levels of use.
2.6 Statistical Analysis
Our analytic sample included 2,539 Wave 6 respondents. Our previous work has shown that from waves 1 to 7, loss to follow-up was not associated with demographics or risk behaviors, such as alcohol and marijuana use (D’Amico et al., 2016). We used multiple imputation to account for missing data resulting from loss to follow-up from Wave 6 to Wave 7, item-missingness, and lack of geocoded address which was used for the neighborhood disadvantage analyses (Allison, 2002; Rubin, 1987). Specifically, 40 imputed datasets were generated using multivariate imputation by chained equations (MICE) using the mi and mice packages in R Version 3.2.4 (Azur et al., 2011; Buuren and Groothuis-Oudshoorn, 2011; White et al., 2011). MICE is a particular multiple imputation technique that imputes missing values conditional on all other variables in an iterative process; this approach does not require the specification of a subjective subset of non-missing variables to be used for imputation. Analyses were performed within each imputed dataset and results were pooled across datasets (Schafer and Graham, 2002). Logistic regression analyses examined the association between each of the four neighborhood measures and each ATOD use outcome. All analyses adjusted for age, sex, race/ethnicity, mother’s education, an indicator for college at follow-up, and whether the participant was in the intervention group in the original study. To examine effect modification for each potential individual-level effect modifier (parental monitoring, peer affiliation, and resistance self-efficacy), we added a main effect for the individual-level effect modifier as a continuous score, and an interaction effect term between the effect modifier and the neighborhood measure. Models were not adjusted for clustering at the census tract because more than half of the census tracts contained just one student (Bell et al., 2010).
A subset of respondents (n=272, 11%) were known to have moved between the initial and follow-up survey for this study. We conducted sensitivity analyses in which, for these respondents only, we assigned the neighborhood disadvantage value based on the respondent’s address at the follow-up survey instead of the initial survey. In addition, for these sensitivity analyses, we used the three subjective neighborhood measures based on responses to the follow-up survey instead of the initial survey.
3. Results
3.1 Descriptive Statistics
At the initial wave for these analyses, the sample was 16.2 years old, on average, 53.7% female, 43.9% Hispanic, 21.0% Asian, 21.0% non-Hispanic White, and 11.8% Other/Multiracial (Table 1). The percentage of participants reporting past year alcohol, cigarette, e-cigarette, and marijuana use at follow-up was 41.1%, 11.4%, 21.3%, and 27.5%, respectively.
Table 1.
Sample characteristics (n=2,539).
| Mean (SD) or N (%) | |
|---|---|
| Demographics at Baseline | |
| Age | 16.23 (0.74) |
| Sex | |
| Female | 1359 (53.7%) |
| Mother’s Education | |
| Did not finish high school | 326 (12.9%) |
| Graduated from high school | 389 (15.3%) |
| Some college | 429 (16.9%) |
| Graduated from college | 1105 (43.6%) |
| Don’t know | 287 (11.3%) |
| Race/ethnicity | |
| Non-Hispanic White | 533(21.0%) |
| Hispanic | 1115 (43.9%) |
| Asian | 532 (21.0%) |
| Other/Multiracial | 300 (11.8%) |
| In college at follow-up | 386 (15.2%) |
| Neighborhood Measures at Baseline | |
| Problems with Alcohol and Drugs | 2.34 (0.96) |
| Disorganization | 1.35 (0.50) |
| Cohesion | 3.20 (0.58) |
| Neighborhood disadvantage | −0.33 (0.65) |
| Potential Effect Modifiers at Baseline | |
| Parental Monitoring | 3.45 (0.62) |
| Resistance self-efficacy | |
| Alcohol | 3.21 (0.91) |
| Cigarette | 3.81 (0.55) |
| Marijuana | 3.48 (0.87) |
| Peer Affiliation | |
| Alcohol | 2.18 (1.06) |
| Cigarette | 1.62 (0.88) |
| Marijuana | 2.16 (1.11) |
| Past Year Use at Follow-up | |
| Alcohol | 839 (41.1%) |
| Cigarette | 233 (11.4%) |
| Marijuana | 563 (27.5%) |
| E-cigarette | 436 (21.3%) |
Notes: All means, standard deviations (SD) and percentages calculated among non-missing values
3.2 Main Effects of Neighborhood Characteristics
Table 2 presents adjusted associations between the four neighborhood measures and each outcome. Each one unit increase (scale of 1–5) in neighborhood problems with alcohol/drugs was significantly associated (p <.05) with a 11%, 16%, and 25% higher odds of alcohol, marijuana and e-cigarette use, respectively, in the past year. Each one unit increase in neighborhood disorganization was significantly associated (p <.05) with higher odds of past year alcohol (29%), cigarette (38%), e-cigarette (59%), and marijuana (46%) use. Higher neighborhood cohesion was statistically significantly associated (p <.05) with lower odds of cigarette use (by 25%), e-cigarette use (by 17%), and marijuana use (by 16%) in the past year. Objectively measured neighborhood disadvantage was not statistically significantly associated with any outcomes.
Table 2.
Main Effects of Neighborhood Measures on Past Year Use
| Alcohol Odds Ratio (95% CI) |
Cigarette Odds Ratio (95% CI) |
Marijuana Odds Ratio (95% CI) |
E-cigarettes Odds Ratio (95% CI) |
|
|---|---|---|---|---|
|
| ||||
| Neighborhood problems with alcohol and drugs | 1.11 | 1.08 | 1.16 | 1.25 |
| (1.01, 1.21)* | (0.93, 1.26) | (1.04, 1.30)** | (1.13, 1.38)*** | |
|
| ||||
| Neighborhood disorganization | 1.29 | 1.38 | 1.46 | 1.59 |
| (1.07, 1.54)** | (1.05, 1.80)* | (1.19, 1.78)*** | (1.29, 1.96)*** | |
|
| ||||
| Neighborhood cohesion | 0.97 | 0.75 | 0.84 | 0.83 |
| (0.84, 1.13) | (0.58, 0.95)* | (0.7, 1.00)* | (0.7, 0.97)* | |
|
| ||||
| Neighborhood disadvantage | 0.94 | 0.94 | 0.93 | 1.01 |
| (0.81, 1.10) | (0.74, 1.19) | (0.77, 1.12) | (0.85, 1.19) | |
Notes: Estimates are from models adjusted for age, sex, race/ethnicity, mother’s education, whether or not the participant was in the intervention group in Wave 1, and an indicator for whether in college at follow-up; CI = confidence interval
p-value < 0.05
p-value <0.01
p-value < 0.001.
3.3 Effect Modification by Individual, Peer, and Family Factors
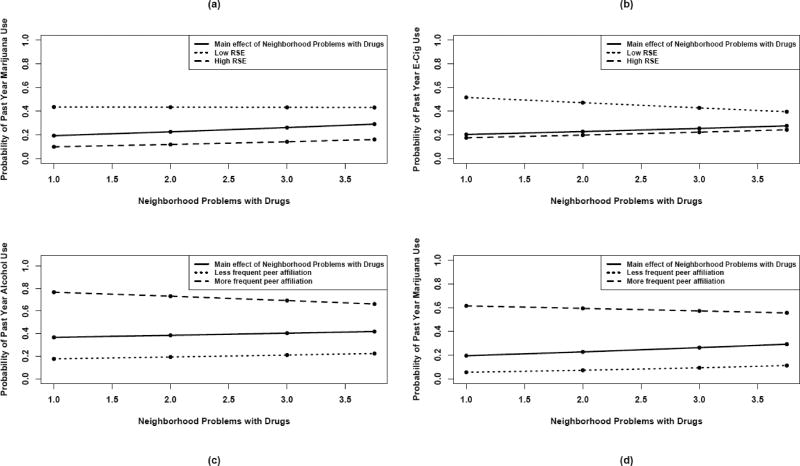
Tables 3–5 provide interactions effects with each of the three perceived neighborhood variables. Perceiving more neighborhood problems with alcohol, cigarettes, and drugs among kids and teens was significantly associated with higher odds of e-cigarettes and marijuana, and higher RSE mitigated the negative effects of neighborhood problems with alcohol/drugs (Table 3). To illustrate the interaction effect for marijuana use (Figure 1a), when neighborhood problems with alcohol/drugs is perceived to be low, adolescents who have higher alcohol RSE (dashed line) have a lower probability of alcohol use than the whole sample (solid line) while adolescents with lower RSE (dotted line) have a higher probability of alcohol use. The dashed and solid lines are parallel suggesting that higher alcohol RSE can buffer some of the negative effects of neighborhood problems with alcohol/drugs, reducing the probability of past year marijuana use by almost half, at any level of neighborhood problems with alcohol/drugs. Although adolescents who have lower RSE have a higher probability of past year use than the whole group, these differences attenuate slightly at the highest levels of neighborhood problems with alcohol/drugs, with RSE making less of a difference in terms of alcohol use, over the range of neighborhood problems with alcohol/drugs. For alcohol, cigarettes, and marijuana, the negative effect of neighborhood problems with alcohol/drugs was also exacerbated by higher affiliation with peers who use (see Figures 1c and 1d). There were no significant interactions found for parental monitoring.
Table 3.
Effect Modifiers of Neighborhood Problems with Alcohol and Drugs on Past Year Use
| Alcohol Odds Ratio (95% CI) |
Cigarettes Odds Ratio (95% CI) |
E-cigarettes Odds Ratio (95% CI) |
Marijuana Odds Ratio (95% CI) |
|
|---|---|---|---|---|
| Resistance self-efficacy | ||||
| Main neighborhood effect | 0.87 (0.6, 1.27) | 0.57 (0.29, 1.11) | 0.46 (0.24, 0.88)* | 0.71 (0.45, 1.13) |
| Main modifier effect | 0.31 (0.23, 0.42)*** | 0.22 (0.13, 0.38)*** | 0.25 (0.16, 0.42)*** | 0.21 (0.15, 0.3)*** |
| Interaction effect | 1.05 (0.94, 1.17) | 1.16 (0.97, 1.39) | 1.26 (1.07, 1.49)** | 1.15 (1.01, 1.31)* |
| LRT (p-value) | 0.423 | 0.102 | 0.007 | 0.030 |
| Peer Affiliation | ||||
| Main neighborhood effect | 1.29 (1.02, 1.64)* | 1.29 (0.94, 1.75) | 1.14 (0.89, 1.44) | 1.55 (1.16, 2.06)** |
| Main modifier effect | 2.87 (2.25, 3.67)*** | 2.86 (2.02, 4.04)*** | 2.09 (1.55, 2.83)*** | 3.45 (2.63, 4.54)*** |
| Interaction effect | 0.9 (0.82, 0.99)* | 0.88 (0.77, 1.00)* | 0.96 (0.86, 1.08) | 0.88 (0.80, 0.98)* |
| LRT (p-value) | 0.026 | 0.046 | 0.488 | 0.017 |
| Parental Monitoring | ||||
| Main neighborhood effect | 0.73 (0.44, 1.19) | 0.79 (0.41, 1.54) | 0.72 (0.42, 1.24) | 0.99 (0.59, 1.67) |
| Main modifier effect | 0.42 (0.28, 0.63)*** | 0.57 (0.33, 0.97)* | 0.49 (0.31, 0.76)** | 0.48 (0.32, 0.73)*** |
| Interaction effect | 1.12 (0.97, 1.29) | 1.1 (0.9, 1.33) | 1.14 (0.97, 1.33) | 1.06 (0.91, 1.23) |
| LRT (p-value) | 0.123 | 0.347 | 0.100 | 0.473 |
Notes: Estimates are from models adjusted for age, sex, race/ethnicity, mother’s education, whether or not the participant was in the intervention group at Wave 1, and a separate indicator for whether in college at follow-up;. CI = confidence interval, LRT = likelihood ratio test comparing model with versus without interaction
p-value < 0.05
p-value <0.01
p-value < 0.001.
Table 5.
Effect Modifiers of Neighborhood Social Cohesion on Past Year Use
| Alcohol Odds Ratio (95% CI) |
Cigarettes Odds Ratio (95% CI) |
E-cigarettes Odds Ratio (95% CI) |
Marijuana Odds Ratio (95% CI) |
|
|---|---|---|---|---|
| Resistance self-efficacy | ||||
| Main neighborhood effect | 2.01 (1.03, 3.95)* | 0.87 (0.23, 3.25) | 2.13 (0.62, 7.37) | 2.5 (1.05, 5.93)* |
| Main modifier effect | 0.56 (0.29, 1.05) | 0.34 (0.11, 1.04) | 0.96 (0.35, 2.6) | 0.66 (0.31, 1.4) |
| Interaction effect | 0.86 (0.70, 1.05) | 0.98 (0.69, 1.39) | 0.80 (0.58, 1.1) | 0.77 (0.61, 0.99)* |
| LRT (p-value) | 0.130 | 0.890 | 0.170 | 0.037 |
| Peer Affiliation | ||||
| Main neighborhood effect | 0.94 (0.64, 1.38) | 0.57 (0.34, 0.96)* | 1.00 (0.67, 1.47) | 0.91 (0.57, 1.46) |
| Main modifier effect | 1.71 (1.02, 2.86)* | 1.14 (0.57, 2.30) | 2.03 (1.09, 3.78)* | 2.28 (1.34, 3.88)** |
| Interaction effect | 1.09 (0.93, 1.27) | 1.21 (0.97, 1.50) | 0.98 (0.81, 1.19) | 1.04 (0.88, 1.22) |
| LRT (p-value) | 0.293 | 0.087 | 0.843 | 0.652 |
| Parental Monitoring | ||||
| Main neighborhood effect | 1.21 (0.50, 2.92) | 0.59 (0.2, 1.80) | 1.13 (0.43, 2.96) | 1.25 (0.51, 3.04) |
| Main modifier effect | 0.56 (0.26, 1.21) | 0.49 (0.18, 1.30) | 0.79 (0.34, 1.86) | 0.67 (0.30, 1.50) |
| Interaction effect | 0.99 (0.77, 1.27) | 1.1 (0.80, 1.51) | 0.95 (0.72, 1.25) | 0.93 (0.72, 1.20) |
| LRT (p-value) | 0.925 | 0.489 | 0.716 | 0.580 |
Notes: Estimates are from models adjusted for age, sex, race/ethnicity, mother’s education, whether or not the participant was in the intervention group at Wave 1, and a separate indicator for whether in college at follow-up;. CI = confidence interval, LRT = likelihood ratio test comparing model with versus without interaction
p-value < 0.05
p-value <0.01
p-value < 0.001.
Figure 1.
High resistance self-efficacy and lower affiliation with peers who use mitigate negative effects of neighborhood problems with alcohol and drugs on probability of past year alcohol, marijuana, and e-cigarette use.
Notes: Neighborhood problems with alcohol and drugs ranges 1–5 but is plotted 1–3.75 to reflect the 5th–95th percentiles of the observed distribution; low peer affiliation = 1 and high peer affiliation = 4, and low RSE = 2.6 and high RSE = 4. RSE= resistance self-efficacy for [cigarettes]/[marijuana]; Peer affiliation is measured as the frequency of being around other teens who drink alcohol [smoke cigarettes]/[use marijuana]. These substance-specific measures were the same as the substance-specific outcome.
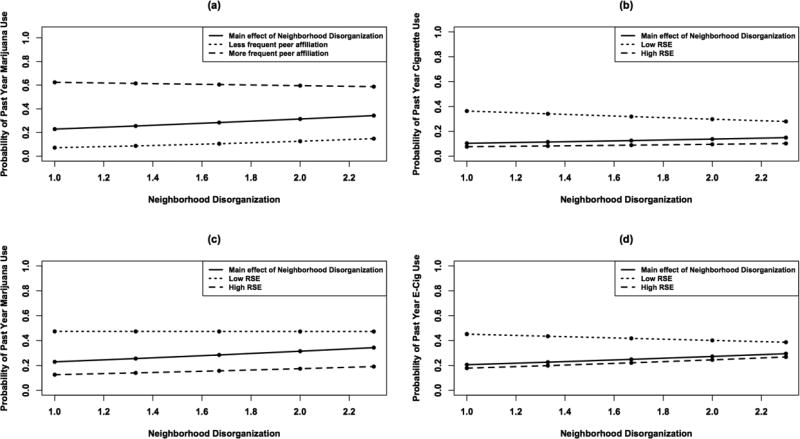
Table 4 and Figure 2 shows that interaction effects between both RSE and peer affiliation with neighborhood disorganization were significant for cigarette, e-cigarette, and marijuana use. As neighborhood disorganization increases, youth with higher RSE or lower peer affiliation have a lower probability of cigarette, e-cigarette, and marijuana use than the whole sample. In contrast, youth with low RSE or higher peer affiliation have as much as a 2-fold higher probability of cigarette, e-cigarette, and marijuana use at the lowest levels of neighborhood disorganization. This association is tempered slightly as neighborhood disorganization increases.
Table 4.
Effect Modifiers of Neighborhood Disorganization on Past Year Use
| Alcohol Odds Ratio (95% CI) |
Cigarettes Odds Ratio (95% CI) |
E-cigarettes Odds Ratio (95% CI) |
Marijuana Odds Ratio (95% CI) |
|
|---|---|---|---|---|
| Resistance self-efficacy | ||||
| Main neighborhood effect | 0.81 (0.43, 1.54) | 0.27 (0.09, 0.77)* | 0.3 (0.11, 0.81)* | 0.53 (0.25, 1.11) |
| Main modifier effect | 0.31 (0.23, 0.43)*** | 0.17 (0.10, 0.28)*** | 0.26 (0.16, 0.4)*** | 0.2 (0.14, 0.29)*** |
| Interaction effect | 1.08 (0.88, 1.33) | 1.48 (1.11, 1.97)** | 1.49 (1.15, 1.93)** | 1.3 (1.04, 1.63)* |
| LRT (p-value) | 0.434 | 0.006 | 0.002 | 0.017 |
| Peer Affiliation | ||||
| Main neighborhood effect | 1.33 (0.82, 2.17) | 2.06 (1.14, 3.72)* | 1.72 (1.07, 2.76)* | 2.7 (1.53, 4.75)*** |
| Main modifier effect | 2.46 (1.9, 3.19)*** | 3.01 (2.10, 4.32)*** | 2.34 (1.71, 3.21)*** | 3.72 (2.8, 4.93)*** |
| Interaction effect | 0.92 (0.77, 1.1) | 0.76 (0.60, 0.97)* | 0.86 (0.69, 1.06) | 0.76 (0.63, 0.91)** |
| LRT (p-value) | 0.387 | 0.022 | 0.147 | 0.004 |
| Parental Monitoring | ||||
| Main neighborhood effect | 1.74 (0.7, 4.33) | 1.93 (0.73, 5.12) | 1.38 (0.56, 3.41) | 1.8 (0.72, 4.49) |
| Main modifier effect | 0.64 (0.43, 0.96)* | 0.77 (0.48, 1.23) | 0.68 (0.44, 1.04) | 0.59 (0.39, 0.89)* |
| Interaction effect | 0.91 (0.7, 1.18) | 0.89 (0.66, 1.19) | 1.01 (0.77, 1.31) | 0.95 (0.73, 1.24) |
| LRT (p-value) | 0.462 | 0.796 | 0.962 | 0.722 |
Notes: Estimates are from models adjusted for age, sex, race/ethnicity, mother’s education, whether or not the participant was in the intervention group at Wave 1, and a separate indicator for whether in college at follow-up,;. CI = confidence interval, LRT = likelihood ratio test comparing model with versus without interaction
p-value < 0.05
p-value <0.01
p-value < 0.001.
Figure 2.
High resistance self-efficacy and less frequent affiliation with peers who use mitigates negative effects of neighborhood disorganization on past year cigarette, marijuana, and e-cigarette usea.
Notes: Neighborhood disorganization ranges 1–5 but is plotted 1–2.3 to reflect the 5th–95th percentiles of the observed distribution; low peer affiliation = 1 and high peer affiliation = 4, and low RSE = 2.6 and high RSE = 4. RSE= resistance self-efficacy for [cigarettes]/[marijuana]; Peer affiliation is measured as the frequency of being around other teens who [smoke cigarettes]/[use marijuana]. These substance-specific measures were the same as the substance-specific outcome.
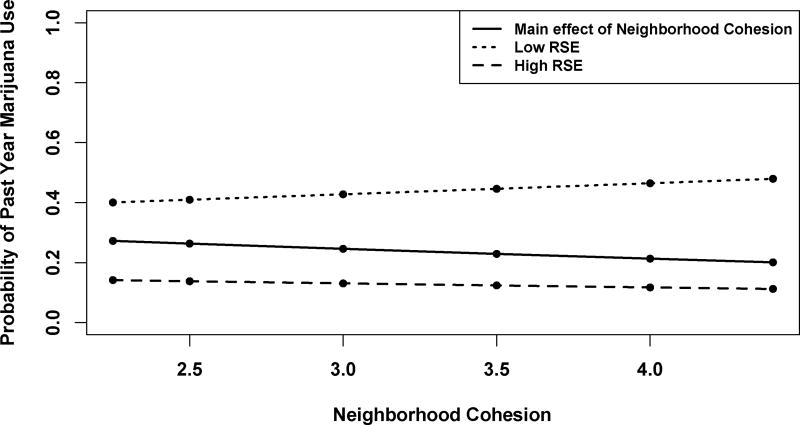
Table 5 and Figure 3 show that as neighborhood social cohesion increases, the probability of past year marijuana use declines. However, youth with higher RSE (dashed line in Figure 3) have the lowest probability of marijuana use and youth with low RSE (dotted line) have the highest probability of marijuana use.
Figure 3.
High resistance self-efficacy bolsters positive effects of neighborhood cohesion on past year marijuana usea.
Notes: Neighborhood cohesion ranges 1–5 but is plotted from 2.25–4/5 to reflect the 5th–95th percentiles of the observed distribution; low RSE = 2.6 and high RSE = 4. RSE= resistance self-efficacy for marijuana.
Sensitivity analyses showed that significant results in the main effects analyses were mostly robust to accommodation of movers. However, three interaction terms were no longer significant: the neighborhood social cohesion interaction term with RSE and neighborhood problems with alcohol/drugs with RSE for marijuana use, and neighborhood problems with alcohol/drugs with peer affiliation for cigarette use. This may be due to either (i) differences in social cohesion and neighborhood problems with alcohol/drugs before and after a move (see Appendix Table A1)1; (ii) analyses involving a less common outcome are more sensitive to small changes in neighborhood values; or (iii) neighborhood social cohesion and problems with alcohol/drugs differed in magnitude and were statistically significant (p<0.01) between movers and non-movers (Appendix Table A2)1.
4. Discussion
The current study is the first to report that perceptions of one’s neighborhood were longitudinally associated with using four different types of substances in a diverse sample of adolescents, whereas objectively measured neighborhood disadvantage was not significantly associated with ATOD use. The most consistent predictor of all four types of substances was neighborhood disorganization. This suggests that reducing neighborhood crime, drug selling, and the social plights that precede housing turnover could help prevent adolescent ATOD use.
To our knowledge, no other study that examined subjective neighborhood characteristics has tested associations with cigarette use separately from other substances, nor has any prior study examined neighborhood associations with e-cigarettes. Our findings suggest that supporting more social connections between neighbors and monitoring of adolescent deviant behaviors by neighbors may be effective in reducing cigarette, e-cigarette, and marijuana use. One prior study of adults 18–30 years of age found that objectively measured neighborhood disadvantage was cross-sectionally associated with current cigarette smoking (Diez Roux et al., 2003). In contrast, we did not find any association between neighborhood disadvantage and past year cigarette use. This difference in findings could be attributable to differences between the two studies in terms of design (cross-sectional vs. longitudinal), sample characteristics (e.g., 18–30 year olds vs. mostly adolescents under age 18), and the measure of smoking (currently smoking at least five cigarettes a week almost every week vs. any past year cigarette smoking). In general, objective neighborhood disadvantage was not associated with any other substance suggesting that perceived neighborhood characteristics may be more proximal to ATOD use, and that the constructs of problems with alcohol/drugs, disorganization, and cohesion and adolescent’s perceptions of those neighborhood qualities are important to intervene on.
Our study significantly extends previous research by examining whether associations of neighborhood factors with ATOD use differ according to potentially modifiable individual, peer, and family factors. Had we not examined effect modifiers, we would have missed significant interaction effects, potentially overlooking critical opportunities for multi-level interventions. Unlike findings by Burlew and colleagues (2009), our study did not find that parental monitoring modified effects of living in a lower quality neighborhood. This may be because our measure of parental monitoring was more general and not specific to use of each substance, and also due to the relatively low variability in the measure. However, we found that RSE and affiliation with peers who use ATOD showed consistent modification of neighborhood quality. These interactions suggest that at lower levels of neighborhood disorganization, less affiliation with peers who use and greater ability to resist ATOD have strong protective effects, whereas for adolescents living in a more disorganized neighborhood, these two factors had a smaller (but still statistically significant) protective effects on cigarette, e-cigarette, and marijuana use. Similar interaction effects were seen with neighborhood problems with alcohol/drugs. Thus, interventions that focus on reducing affiliations with peers who use ATOD, and increasing ability to resist ATOD will be the most consistent way to reduce negative influences of neighborhood disorganization and problems with alcohol/drugs. Interventions that focus on these individual- and peer-level factors will be most efficient for adolescents living in better quality neighborhoods. Evaluations of out of-school interventions have shown that reducing time spent with peers who use ATOD, and increasing RSE (Aseltine et al., 2000) by encouraging structured, organized activities and mentoring relationships with adults show reduced substance use rates and other risky behaviors (Aseltine et al., 2000; Cohen et al., 2007). Xue and colleagues (2007) have also reported that objective neighborhood disadvantage effects on cigarette use were buffered by participation in school and church activities.
The significant interaction effects we found also suggest that community interventions that address adolescents’ perceptions of problems with alcohol/drugs and disorganization in their neighborhoods could very well buffer the negative effects of low resistance self-efficacy or spending more time with peers who use ATOD. For instance, community-level interventions to encourage adult neighbors to monitor and intervene when they observe adolescents engaging in deviant behaviors, to curb open drug selling and street fights, and to increase social cohesion among neighbors may buffer against individual and peer risk factors. These interventions should also seek to ensure that communities have adequate law enforcement and training on evidence-based programs that help communities reduce problem behaviors and promote healthy youth development (Baum et al., 2013; Griffin and Botvin, 2010; Haggerty 2016; Sabal and Listenbee, 2014).
Findings should be considered in the context of several limitations. First, as with most research of this nature, we relied on self-report from adolescents, the limitations of which are well-known, although possibly exaggerated (Chan, 2008). In fact, recent work with young adults age 18–21 has shown that self-reported alcohol use is corroborated by a biochemical measure, transdermal alcohol assessment (Simons et al., 2015). Second, an individual’s use of alcohol or other drugs may be correlated with the perception of one’s neighborhood. However, our study’s longitudinal nature attempts to minimize the potential for same-source bias since the independent and dependent variables are measured at two different time points. Also, our study did not examine changes in ATOD use, or changes in neighborhood characteristics over time among non-movers or changes in the type of neighborhood one moves into. This complex depiction of changing neighborhoods and changing ATOD use are future directions that we can pursue with more variability in shorter-term measures of substance use that comes with young adulthood. Third, our sample is relatively under-represented by non-Hispanic Blacks, limiting generalizability of our findings to that group. Nevertheless, the inclusion of Hispanics and Asians in our sample offers a more racially/ethnically diverse sample than prior studies, which focused on more homogeneous (either majority White or Black) samples (Brenner et al., 2011; Burlew et al., 2009; Fite et al., 2009; Fuller et al., 2005; Furr-Holden et al., 2011; Lloyd and Anthony, 2003). Although our study provides unique findings on the longitudinal association with multiple substances, including e-cigarettes, future studies should also examine other substances such as opioids, cocaine, and other tobacco use.
In sum, our findings suggest that community-level programs that increase social cohesion among neighbors, effective monitoring of adolescent deviant behaviors by adult neighbors, and better policing of open drug selling and street fights may prevent individual-level ATOD use. Community prevention programs often require significant economic resources (Griffin and Botvin, 2011), thus, public health impacts of those programs can be more efficient by partnering with individual-level programs that target resistance self-efficacy and minimize affiliations with peers who use ATOD. Although our findings are based on just two waves of data and cannot infer causality, targeting resistance self-efficacy and peer influence in particular may reduce ATOD use, even for adolescents living in the most at-risk neighborhoods.
Supplementary Material
Highlights.
Neighborhood alcohol/drug problems are associated with alcohol and marijuana use
Higher neighborhood disorganization is associated with lower odds of substance use
Parental monitoring did not modify effects of neighborhood quality
More affiliation with peers who use exacerbated poor quality neighborhood effects
Resistance self-efficacy may curb substance use for youth in unsafe neighborhood
Acknowledgments
The authors wish to thank the districts and schools who participated in and supported this project. We would also like to thank Kirsten Becker and Megan Zander-Cotugno for overseeing survey administrations.
Role of Funding Source
This work was funded by grants from the National Institute on Alcohol Abuse and Alcoholism (R01AA016577 and R01AA021786, PI Elizabeth J. D’Amico) and National Institute on Aging (AG043960, PI Regina Shih).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Author Disclosures
Contributors
Regina Shih: Drafted the manuscript, directed all statistical analyses, assisted with survey development and data collection
Layla Parast: Assisted with the drafting of the manuscript, conducted statistical analyses
Eric Pedersen: Assisted with the literature review and assisted with survey development and data collection, reviewed the manuscript
Wendy Troxel: Assisted with the study design, and reviewed the manuscript
Joan Tucker: Assisted survey development and data collection, reviewed the manuscript
Jeremy Miles: Contributed to the statistical analyses, and reviewed the manuscript
Lisa Miyashiro: Lead the geocoding of address data and assisted with merging of neighborhood and survey data
Elizabeth D’Amico: Oversaw all survey development and data collection, contributed to study design, reviewed the manuscript
Conflict of Interest
The authors have no conflicts to declare
References
- Allison P. Missing data. Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- Aseltine R, Dupre M, Lamlein P. Mentoring as a drug prevention strategy: An evaluation of Across Ages. Adolesc. Family Health. 2000;1:11–20. [Google Scholar]
- Aslund C, Nilsson KW. Social capital in relation to alcohol consumption, smoking, and illicit drug use among adolescents: A cross-sectional study in Sweden. Int. J. Equity Health. 2013;12:33. doi: 10.1186/1475-9276-12-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: What is it and how does it work? Int. J. Methods Psychiatr. Res. 2011;20:40–49. doi: 10.1002/mpr.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum K, Blakeslee KM, Lloyd J, Petrosino A. Violence Prevention: Moving from Evidence to Implementation. Institute of Medicine, National Academy of Sciences 2013 [Google Scholar]
- Bell BAGBM, Kromrey JD, Ferron JM. The Impact of Small Cluster Size on Multilevel Models: A Monte Carlo Examination of Two-Level Models with Binary and Continuous Predictors. Joint Statistical Meeting. 2010:4057–4067. [Google Scholar]
- Brenner AB, Bauermeister JA, Zimmerman MA. Neighborhood variation in adolescent alcohol use: Examination of socioecological and social disorganization theories. J. Stud. Alcohol Drugs. 2011;72:651–659. doi: 10.15288/jsad.2011.72.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. The Ecology of Human Development: Experiments byNature and Design. Harvard University Press; Cambridge, MA: 1979. [Google Scholar]
- Browning SE. Neighborhood, school, and family effects on the frequency of alcohol use among Toronto youth. Subst. Use Misuse. 2012;47:31–43. doi: 10.3109/10826084.2011.625070. [DOI] [PubMed] [Google Scholar]
- Burlew AK, Johnson CS, Flowers AM, Peteet BJ, Griffith-Henry KD, Buchanan ND. Risk, parental supervision and the onset of substance use among African American adolescents. J. Child Fam. Stud. 2009;18:680–689. [Google Scholar]
- Buu A, Dipiazza C, Wang J, Puttler LI, Fitzgerald HE, Zucker RA. Parent, family, and neighborhood effects on the development of child substance use and other psychopathology from preschool to the start of adulthood. J. Stud. Alcohol Drugs. 2009;70:489–498. doi: 10.15288/jsad.2009.70.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buuren S, Groothuis-Oudshoorn K. Mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 2011:45. [Google Scholar]
- Byrnes HF, Miller BA, Chen MJ, Grube JW. The roles of mothers’ neighborhood perceptions and specific monitoring strategies in youths’ problem behavior. J. Youth Adolesc. 2011;40:347–360. doi: 10.1007/s10964-010-9538-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpiano RM. Actual or potential neighborhood resources and access to them: Testing hypotheses of social capital for the health of female caregivers. Soc. Sci. Med. 2008;67:568–582. doi: 10.1016/j.socscimed.2008.04.017. [DOI] [PubMed] [Google Scholar]
- Chan D. So why ask me? Are self-report data really that bad? In. In: Lance CE, Vandenberg RJ, editors. Statistical and methodological myths and urban legends: Received doctrine, verity, and fable in the organizational and social sciences. Erlbaum; Hillsdale, NJ: 2008. pp. 309–336. [Google Scholar]
- Choi Y, Harachi TW, Catalano RF. Neighborhoods, family, and substance use: Comparisons of the relations across racial and ethnic groups. Soc. Serv. Rev. 2006;80:675–704. doi: 10.1086/508380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen DA, Taylor SL, Zonta M, Vestal KD, Schuster MA. Availability of high school extracurricular sports programs and high-risk behaviors. J. Sch. Health. 2007;77:80–86. doi: 10.1111/j.1746-1561.2007.00171.x. [DOI] [PubMed] [Google Scholar]
- Connell CM, Gilreath TD, Aklin WM, Brex RA. Social-ecological influences on patterns of substance use among non-metropolitan high school students. Am. J. Comm. Psychol. 2010;45:36–48. doi: 10.1007/s10464-009-9289-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creemers HE, Dijkstra JK, Vollebergh WA, Ormel J, Verhulst FC, Huizink AC. Predicting life-time and regular cannabis use during adolescence; the roles of temperament and peer substance use: The TRAILS study. Addiction. 2010;105:699–708. doi: 10.1111/j.1360-0443.2009.02819.x. [DOI] [PubMed] [Google Scholar]
- Crum RM, Lillie-Blanton M, Anthony JC. Neighborhood environment and opportunity to use cocaine and other drugs in late childhood and early adolescence. Drug Alcohol Depend. 1996;43:155–161. doi: 10.1016/s0376-8716(96)01298-7. [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Green HD, Jr, Miles JN, Zhou AJ, Tucker JS, Shih RA. Voluntary after-school alcohol and drug programs for middle school youth: If you build it right, they will come. J. Res. Adolesc. 2012a;22:571–582. doi: 10.1111/j.1532-7795.2012.00782.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, McCarthy DM. Escalation and initiation of younger adolescents’ substance use: The impact of perceived peer use. J. Adolesc. Health. 2006;39:481–487. doi: 10.1016/j.jadohealth.2006.02.010. [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JN, Ewing BA, Shih RA, Pedersen ER. Alcohol and marijuana use trajectories in a diverse longitudinal sample of adolescents: examining use patterns from age 11 to 17 years. Addiction. 2016;111:1825–1835. doi: 10.1111/add.13442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JN, Zhou AJ, Shih RA, Green HD., Jr Preventing alcohol use with a voluntary after-school program for middle school students: Results from a cluster randomized controlled trial of CHOICE. Prev. Sci. 2012b;13:415–425. doi: 10.1007/s11121-011-0269-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Haan L, Boljevac T. Alcohol prevalence and attitudes among adults and adolescents: Their relation to early adolescent alcohol use in rural communities. J. Child Adolesc. Subst. Abuse. 2010;19:223–243. doi: 10.1080/1067828X.2010.488960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DHHS. [accessed on October 28 2016];NIH Policy and Guidelines on The Inclusion of Women and Minorities as Subjects in Clinical Research. 2001 http://grants.nih.gov/grants/funding/women_min/guidelines_amended_10_2001.htm.
- Diez Roux AV, Merkin SS, Hannan P, Jacobs DR, Kiefe CI. Area characteristics, individual-level socioeconomic indicators, and smoking in young adults: The coronary artery disease risk development in young adults study. Am. J. Epidemiol. 2003;157:315–326. doi: 10.1093/aje/kwf207. [DOI] [PubMed] [Google Scholar]
- Duan L, Chou CP, Andreeva VA, Pentz MA. Trajectories of peer social influences as long-term predictors of drug use from early through late adolescence. J Youth Adolesc. 2009;38:454–465. doi: 10.1007/s10964-008-9310-y. [DOI] [PubMed] [Google Scholar]
- Duncan SC, Duncan TE, Strycker LA. A multilevel analysis of neighborhood context and youth alcohol and drug problems. Prev. Sci. 2002;3:125–133. doi: 10.1023/a:1015483317310. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, McCaffrey DF, Ghosh-Dastidar B, Longshore DL. New inroads in preventing adolescent drug use: Results from a large-scale trial of project ALERT in middle schools. Am. J. Public Health. 2003;93:1830–1836. doi: 10.2105/ajph.93.11.1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ennett ST, Foshee VA, Bauman KE, Hussong A, Cai L, Reyes HL, Faris R, Hipp J, Durant R. The social ecology of adolescent alcohol misuse. Child Dev. 2008;79:1777–1791. doi: 10.1111/j.1467-8624.2008.01225.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fite PJ, Wynn P, Lochman JE, Wells KC. The influence of neighborhood disadvantage and perceived disapproval on early substance use initiation. Addict. Behav. 2009;34:769–771. doi: 10.1016/j.addbeh.2009.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulkerson JA, Pasch KE, Perry CL, Komro K. Relationships between alcohol-related informal social control, parental monitoring and adolescent problem behaviors among racially diverse urban youth. J. Comm. Health. 2008;33:425–433. doi: 10.1007/s10900-008-9117-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller CM, Borrell LN, Latkin CA, Galea S, Ompad DC, Strathdee SA, Vlahov D. Effects of race, neighborhood, and social network on age at initiation of injection drug use. Am. J. Public Health. 2005;95:689–695. doi: 10.2105/AJPH.2003.02178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furr-Holden CD, Lee MH, Johnson R, Milam AJ, Duncan A, Reboussin BA, Leaf PJ, Ialongo NS. Neighborhood environment and marijuana use in urban young adults. Prev. Sci. 2015;16:268–278. doi: 10.1007/s11121-014-0497-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furr-Holden CD, Lee MH, Milam AJ, Johnson RM, Lee KS, Ialongo NS. The growth of neighborhood disorder and marijuana use among urban adolescents: A case for policy and environmental interventions. J. Stud. Alcohol Drugs. 2011;72:371–379. doi: 10.15288/jsad.2011.72.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin KW, Botvin GJ. Evidence-based interventions for preventing substance use disorders in adolescents. Child Adolesc. Psychiatr. Clin. N. Am. 2010;19:505–526. doi: 10.1016/j.chc.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadley-Ives E, Stiffman AR, Elze D, Johnson SD, Dore P. Measuring neighborhood and school environments: Perceptual and aggregate approaches. J. Hum. Behav. Soc. Environ. 2000;3:1–28. [Google Scholar]
- Haggerty K. [Accessed on October 28, 2016];Communities That Care. 2016 http://www.communitiesthatcare.net/how-ctc-works/
- Jackson N, Denny S, Ameratunga S. Social and socio-demographic neighborhood effects on adolescent alcohol use: A systematic review of multi-level studies. Soc. Sci. Med. 2014;115:10–20. doi: 10.1016/j.socscimed.2014.06.004. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Volume I: Secondary school students. National Institute on Drug Abuse; Bethesda, MD: 2009. Monitoring the Future national survey results on drug use, 1975–2008. 09-7402, N.P.N. (Ed.) [Google Scholar]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. In: Monitoring the Future National Survey Results on Drug Use, 1975–2016: Overview, Key Findings on Adolescent Drug Use. Research, I.f.S., editor. University of Michigan; Ann Arbor: 2016. [Google Scholar]
- Jones-Webb R, Karriker-Jaffe KJ. Neighborhood disadvantage, high alcohol content beverage consumption, drinking norms, and drinking consequences: A mediation analysis. J. Urban Health. 2013;90:667–684. doi: 10.1007/s11524-013-9786-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joon Jang S, Johnson BR. Neighborhood disorder, individual religiosity, and adolescent use of illicit drugs: A test of multilevel hypotheses. Criminology. 2001;39:109–144. [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: A comparison of area-based socioeconomic measures—The Public Health Disparities Geocoding Project. Am. J. Public Health. 2003;93:1655–1671. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Waterman P, Lemieux K, Zierler S, Hogan JW. On the wrong side of the tracts? Evaluating the accuracy of geocoding in public health research. Am. J. Public Health. 2001;91:1114–1116. doi: 10.2105/ajph.91.7.1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert SF, Brown TL, Phillips CM, Ialongo NS. The relationship between perceptions of neighborhood characteristics and substance use among urban African American adolescents. Am. J. Comm. Psychol. 2004;34:205–218. doi: 10.1007/s10464-004-7415-3. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Strong DR, Sussman S, Kirkpatrick MG, Unger JB, Barrington-Trimis JL, Audrain-McGovern J. Psychiatric comorbidity in adolescent electronic and conventional cigarette use. J. Psychiatr. Res. 2016;73:71–78. doi: 10.1016/j.jpsychires.2015.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd JJ, Anthony JC. Hanging out with the wrong crowd: How much difference can parents make in an urban environment? J. Urban Health. 2003;80:383–399. doi: 10.1093/jurban/jtg043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maimon D, Browning CR. Underage drinking, alcohol sales and collective efficacy: Informal control and opportunity in the study of alcohol use. Soc. Sci. Res. 2012;41:977–990. doi: 10.1016/j.ssresearch.2012.01.009. [DOI] [PubMed] [Google Scholar]
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2015: Volume I, Secondary school students. Institute for Social Research, The University of Michigan; Ann Arbor: 2016. [Google Scholar]
- Miles JNVMMW, Lavery D, Escarce JJ, Cagney KA, Shih RA. Constructing a time-invariant measure of the socio-economic status of U.S. census tracts. J. Urban Health. 2015;93:213–232. doi: 10.1007/s11524-015-9959-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén BO, Muthén L. Mplus Version 7.11. Muthen and Muthen; Los Angeles, CA: 2013. [Google Scholar]
- Primack BA, Soneji S, Stoolmiller M, Fine MJ, Sargent JD. Progression to traditional cigarette smoking after electronic cigarette use among US adolescents and young adults. JAMA Pediatr. 2015;169:1018–1023. doi: 10.1001/jamapediatrics.2015.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett K, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: A critical review. J. Epidemiol. Community Health. 2001;55:111–122. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reboussin BA, Green KM, Milam AJ, Furr-Holden DM, Johnson RM, Ialongo NS. The role of neighborhood in urban black adolescent marijuana use. Drug Alcohol Depend. 2015;154:69–75. doi: 10.1016/j.drugalcdep.2015.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. John Wiley and Sons; New York: 1987. [Google Scholar]
- Sabal WJ, Listenbee RL. Changing Lives: Prevention and Intervention to Reduce Serious Offending. Justice Research. Office of Juvenile Justice and Delinquency Prevention 2014 [Google Scholar]
- Sampson RJ. The Community Context of Violent Crime. In: Wilson WJ, editor. Sociology and the Public Agenda. Sage Publications; Newbury Park, CA: 1993. pp. 267–274. [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science (New York, NY) 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychol. Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Simons JS, Wills TA, Emery NN, Marks RM. Quantifying alcohol consumption: Self-report, transdermal assessment, and prediction of dependence symptoms. Addict. Behav. 2015;50:205–212. doi: 10.1016/j.addbeh.2015.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh T, Arrazola RA, Corey CG, Husten CG, Neff LJ, Homa DM, King BA. Tobacco use among middle and high school students--United States, 2011–2015. MMWR Morb. Mortal. Wkly. Rep. 2016;65:361–367. doi: 10.15585/mmwr.mm6514a1. [DOI] [PubMed] [Google Scholar]
- Tarter RE, Kirisci L, Gavaler JS, Reynolds M, Kirillova G, Clark DB, Wu J, Moss HB, Vanyukov M. Prospective study of the association between abandoned dwellings and testosterone level on the development of behaviors leading to cannabis use disorder in boys. Biol. Psychiatry. 2009;65:116–121. doi: 10.1016/j.biopsych.2008.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JS, Ewing BA, Miles JN, Shih RA, Pedersen ER, D’Amico EJ. Predictors and consequences of prescription drug misuse during middle school. Drug Alcohol Depend. 2015;156:254–260. doi: 10.1016/j.drugalcdep.2015.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JS, Pollard MS, de la Haye K, Kennedy DP, Green HD., Jr Neighborhood characteristics and the initiation of marijuana use and binge drinking. Drug Alcohol Depend. 2013;128:83–89. doi: 10.1016/j.drugalcdep.2012.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- University of Minnesota. Adolescence: Developing Independence and Identity. Introduction to Psychology. University of Minnesota Libraries Publishing; Minneapolis, MN: 2015. [Google Scholar]
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat. Med. 2011;30:377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, Williams RJ. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tob. Control. 2017;26:34–39. doi: 10.1136/tobaccocontrol-2015-052705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winstanley EL, Steinwachs DM, Ensminger ME, Latkin CA, Stitzer ML, Olsen Y. The association of self-reported neighborhood disorganization and social capital with adolescent alcohol and drug use, dependence, and access to treatment. Drug Alcohol Depend. 2008;92:173–182. doi: 10.1016/j.drugalcdep.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue Y, Zimmerman MA, Caldwell CH. Neighborhood residence and cigarette smoking among urban youths: the protective role of prosocial activities. Am. J. Public Health. 2007;97:1865–1872. doi: 10.2105/AJPH.2005.081307. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.