Abstract
It is well-established that neuroticism, extraversion, and conscientiousness are individually associated with internalizing disorders, but research suggests that these main effects may be qualified by a three-way interaction when predicting depression. The current study was the first to examine this three-way interaction in a psychiatric sample (N=463) with a range of internalizing symptoms as the outcomes. Using two omnibus personality inventories and a diagnostic interview, the expected three-way interaction emerged most consistently for symptoms of major depression, and there was also evidence of synergistic effects for post-traumatic stress disorder and generalized anxiety disorder. Findings indicate that, even in a clinically-distressed and currently-disordered sample, high levels of extraversion and conscientiousness protect against distress disorders for those with high levels of neuroticism.
Keywords: neuroticism, extraversion, conscientiousness, interaction, internalizing disorders, distress disorders, depression, trait affect, disinhibition
1. Introduction
A large body of research has established that personality traits are associated with internalizing psychopathology (i.e., mood and anxiety disorders/symptoms), both concurrently and longitudinally (e.g., Jeronimus, Kotov, Riese, & Ormel, in press; Klein, Kotov, & Bufferd, 2011; see Kotov, Gamez, Schmidt, & Watson, 2010 for a meta-analysis of concurrent associations; Naragon-Gainey, Gallagher, & Brown, 2013; Watson & Naragon-Gainey, 2014). Specifically, neuroticism—which may be defined as a tendency to experience negative emotions and high stress reactivity—is a particularly strong predictor of depression and anxiety, along with related traits such as negative affectivity and the behavioral inhibition system (e.g., Kotov et al., 2010; Watson & Naragon-Gainey, 2014). Extraversion, or the tendency towards sociability, assertiveness, venturesomeness, and the experience of positive emotions (related constructs include positive affectivity and the behavioral activation system), is more moderately and inversely associated with these disorders. Furthermore, associations with extraversion show greater disorder specificity, with some evidence of stronger links to depression and social anxiety in particular (Brown, Chorpita, & Barlow, 1998; Kotov et al., 2010; Watson, Gamez, & Simms, 2005; Watson & Naragon-Gainey, 2014). Finally, conscientiousness (i.e., a tendency to be planful, organized, goal-oriented, and non-impulsive; similar to effortful control) is moderately inversely associated with all internalizing disorders (Kotov et al., 2010).
Most existing research has focused on the main effects of these traits on internalizing psychopathology, whether singly or additively. But theory suggests that there may be synergistic relationships among them that are particularly relevant to depression, such that their interactions should be considered (e.g., Dinovo & Vasey, 2011; Klein et al., 2011). For example, generally someone with high levels of neuroticism is at increased risk for depression, but if s/he is also very sociable and often experiences positive emotions such as enthusiasm and excitement (that is, high levels of extraversion), these protective experiences would greatly reduce or eliminate the risk conferred by his/her high neuroticism. In contrast, levels of neuroticism would be much more predictive of depression symptoms for an individual who is isolated and has fewer sources of pleasure (that is, low levels of extraversion). Similarly, high conscientiousness is associated with planful action and successful realization of goals, which may be critical to help an individual with high neuroticism and/or low extraversion mobilize themselves to overcome tendencies towards sadness, withdrawal, and inactivity and to contact rewarding stimuli, thereby reducing or eliminating depression risk. However, for those with low conscientiousness, high neuroticism and/or low extraversion would remain predictive of greater depression.
A number of studies have examined interactions between each pair of these traits and related constructs, generally (though not always) yielding significant interaction terms when predicting depression (e.g., Gershuny & Sher, 1998; Joiner & Lonigan, 2000; Verstraeten, Vasey, Raes, & Bijttebier, 2009). However, recent empirical work by Vasey and colleagues indicates that there is a significant three-way interaction1 that qualifies the two-way interactions, which may account for some of the null findings regarding two-way interaction. Specifically, in five of six samples with a cross-sectional design and in one prospective, longitudinal study, the positive association between neuroticism-related traits and depression was weakened only in the presence of high levels of extraversion-related traits and high levels of conscientiousness-related traits (Dinovo & Vasey, 2011; Vasey et al., 2013, 2014). More generally, “low-risk” levels of any two traits (i.e., low neuroticism, high extraversion, high conscientiousness) reduced or eliminated the negative impact of “high-risk” levels of the third (i.e., high neuroticism, low extraversion, or low conscientiousness). There was also evidence for the reverse manifestation of the three-way interaction, though the magnitude of this effect was weaker and more limited in the range at which it was observed. In this pattern, individuals with high neuroticism-related traits and low extraversion-related traits showed a weakened protective effect of high conscientiousness-related traits (with similar results for other combinations of two high-risk trait levels and one low-risk trait level).
In their series of three studies, Vasey and colleagues replicated the significant three-way interaction across different ages (children through young adults) and different self-report measures. Furthermore, they found evidence that the effect may be specific to depression, as the three-way interaction was not a significant predictor of general anxiety (i.e., a combination of different anxiety disorder symptoms; Vasey et al., 2013) or symptoms common to depression and anxiety (i.e., general distress; Dinovo & Vasey, 2011; Vasey et al., 2014). These robust results suggest that it is important to consider all three traits in concert and synergistically for a complete understanding of how they are associated with depression.
Although these studies are promising, they are few in number and leave open several important questions that the current study seeks to address. First, a three-way interaction has not yet been tested in a psychiatric sample, which would have more extreme mean levels of high-risk traits and symptoms than unselected samples. As such, it is not clear whether interactive effects among the traits are applicable only at average trait levels and minimal/mild psychological symptoms, or if they generalize to those with significant psychopathology. It is plausible, for example, that in a sample with more extreme high-risk trait levels, the protective effects of high extraversion and high conscientiousness may be insufficient (or high levels on these traits may some evidence of significant two-way interactions occur too rarely) to reduce the strong risk associated with very high neuroticism. As there is in clinical samples (e.g., Joiner & Lonigan, 2000), we hypothesize that the three-way interaction predicting depression will be present in the current study’s clinical sample, though it may be weaker or require higher levels of extraversion and conscientiousness for the protective effect to emerge in comparison to non-clinical samples.
In addition, there has not yet been a thorough examination of the three-way interaction in the anxiety disorders or other related disorders, as prior studies used a single anxiety outcome that collapsed across heterogeneous symptoms, potentially obscuring effects that may vary across disorders (Dinovo & Vasey, 2011; Vasey et al., 2013, 2014). Thus, in the current study, we examine a range of anxiety disorders (i.e., social anxiety, panic, agoraphobia, generalized anxiety disorder [GAD]) as well as other disorders that are associated with anxiety and depression (i.e., posttraumatic stress disorder [PTSD], obsessive-compulsive disorder [OCD]).
There are several reasons to expect that the three-way interaction may predict at least some anxiety disorders, including the fact that depression is highly comorbid with many of these disorders (e.g., Watson & Naragon-Gainey, 2014; Watson et al., 2005). Conceptually, the general rationale for the protective effect of high conscientiousness against depression risk seems equally applicable to anxiety disorders. That is, greater effortful control may mitigate the harmful tendencies of expressions of high levels of negative affect that are linked to anxiety (i.e., avoidance, cognitive perseveration), suggestive of a neuroticism X conscientiousness interaction (see Lonigan & Phillips, 2001). However, the main effect of extraversion is more selectively related to anxiety disorders (that is, most strongly to social anxiety), so the protective effects of extraversion in combination with low conscientiousness may emerge for social anxiety disorder only. In addition, depression has a particularly large neuroticism or general distress component, characterized by high levels of and it may be that low-risk traits are also important in protecting against other disorders neuroticism and general distress (i.e., GAD, PDD, PTSD; Watson & Naragon-Gainey, 2014; Watson et al., 2005). Though the examination of this three-way interaction in the anxiety disorders is exploratory due to a lack of prior studies analyzing specific anxiety symptoms, we tentatively hypothesize that the three-way interaction will be observed or strongest when predicting social anxiety, PDD, GAD, and PTSD, but weaker or absent for panic, agoraphobia, and OCD.
The current study is the first to examine these effects with a method other than self-report, and our use of interview-based assessment of disorders reduces the effects of shared method variance between the predictors and outcomes. In addition, the personality measures in the current study are different than those in prior studies, which extends the examination of the generalizability of effects over different measures and trait conceptualizations. We selected two common omnibus personality inventories (the NEO Personality Inventory- 3 First Half [NEO PI-3FH; McCrae, Costa, & Martin, 2005] and Personality Inventory for DSM-5 [PID-5; Krueger, Derringer, Markon, Watson, & Skodol, 2012], both of which include neuroticism-, extraversion-, and conscientiousness-related traits. Analysis of both measures allows us to examine the robustness and consistency of effects, beyond measure-specific properties.
2. Method
2.1 Participants and Procedure
We analyzed data collected as part of a larger study to develop a new measure of personality pathology traits (CAT-PD; see Simms et al., 2011, for further details). Participants were recruited from mental health treatment centers in Western New York; they were eligible to participate if they were 18 years of age or older and reported receiving psychiatric treatment within the past two years. The final sample consisted of 628 participants. For the current study, samples sizes varied across analyses, as 266 participants completed the NEO PI-3FH and 463 completed the PID-5 scales used here.2 For the largest subgroup analyzed here (n = 463), the mean age was 41.9 years (SD = 12.5), and the majority of the sample was female (65%). Most participants identified primarily as Caucasian (68%) or African American (30%). Sixty-four percent of the sample reported currently receiving psychiatric treatment, whereas the rest of the sample reported having done so within the past two years. There were no significant differences in the above variables between the sample analyzed in the current study and the full sample of 628 participants (all ps > .10).
Based on the MINI International Neuropsychiatric Interview (MINI; see below for details about the interview), participants in the subsample analyzed here met criteria for DSM-5 current diagnoses at the following rates: GAD = 195 individuals (43%), MDD = 150 (33%), bipolar disorder I or II = 133 (30%), antisocial personality disorder = 130 (29%), OCD = 110 (24%), alcohol use disorder = 99 (22%), PTSD = 94 (21%), substance use disorder = 81 (18%), social anxiety disorder = 77 (17%), panic disorder = 59 (13%), PDD = 48 (11%), agoraphobia = 44 (10%), and psychotic disorder = 43 (10%).
Participants came to the lab for a four-hour session that included the completion of self-report questionnaires and clinical interviews; they received $50 plus the cost of transportation as compensation. We describe below the measures that were analyzed for the current study.
2.2 Measures
2.2.1 Mini International Neuropsychiatric Interview (MINI; Sheehan et al., 1998)
The MINI is a structured diagnostic interview that includes a range of diagnoses; the current study focuses on depressive and anxiety disorders. We adapted the MINI (with permission) to assess DSM-5 criteria for the sample disorders. We analyzed symptom counts, rather than dichotomous diagnoses, because they yield greater information/variability and have been shown to provide more reliable and valid measurement of depression and anxiety disorders (see Markon, Chmielewski, & Miller, 2011). Specifically, symptoms from the disorder criteria were rated as present (1) or absent (0), and these scores were summed for each disorder (note that because disorders have different numbers of symptoms and criteria, the possible range of scores varies across disorders; see Table 1). In the present study, trained interviewers, typically clinical psychology doctoral students, conducted MINI interviews. Interviewers received extensive training and ongoing supervision by the second author (LJS), which included weekly case conferences and tape review throughout the course of the study. Independent raters recoded 120 interviews with excellent reliability: MINI disorder-level kappas were strong, Mdn Κ = .96, range = .66-1.00.
Table 1.
Descriptive Statistics and Zero-Order Correlations Among the Personality Traits and DSM-5 Symptom Counts
| N-Neur | N-Ext | N-Con | P-NA | P-Det | P-Dis | MDD | PDD | Panic | Agor | SA | OCD | PTSD | GAD | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NEO Neuroticism | ||||||||||||||
| NEO Extraversion | −.48 | |||||||||||||
| NEO Conscientiousness | −.58 | .32 | ||||||||||||
| PID-5 Neg. Affectivity | .81 | −.33 | −.42 | |||||||||||
| PID-5 Detachment | .50 | −.74 | −.36 | .53 | ||||||||||
| PID-5 Disinhibition | .62 | −.23 | −.73 | .68 | .53 | |||||||||
| MDD | .54 | −.40 | −.36 | .56 | .51 | .51 | ||||||||
| PDD | .44 | −.36 | −.27 | .49 | .49 | .43 | .59 | |||||||
| Panic Disorder | .33 | −.21 | −.07 | .37 | .26 | .25 | .38 | .38 | ||||||
| Agoraphobia | .15 | −.15 | −.05 | .23 | .18 | .14 | .25 | .21 | .38 | |||||
| Social Anxiety | .46 | −.34 | −.23 | .46 | .34 | .35 | .44 | .39 | .38 | .22 | ||||
| OCD | .30 | −.14 | −.14 | .31 | .18 | .29 | .34 | .34 | .33 | .19 | .37 | |||
| PTSD | .49 | −.31 | −.30 | .58 | .49 | .52 | .71 | .60 | .47 | .29 | .51 | .42 | ||
| GAD | .49 | −.22 | −.17 | .52 | .28 | .36 | .51 | .56 | .40 | .22 | .42 | .33 | .61 | |
|
| ||||||||||||||
| N | 266 | 266 | 266 | 463 | 463 | 463 | 618 | 610 | 611 | 610 | 609 | 608 | 595 | 604 |
| Mean | 3.15 | 3.16 | 3.39 | 3.97 | 3.16 | 2.89 | 3.94 | 4.04 | 6.78 | 0.71 | 1.27 | 0.57 | 7.13 | 4.70 |
| SD | 0.70 | 0.57 | 0.63 | 2.08 | 1.76 | 1.78 | 2.85 | 2.52 | 6.21 | 1.73 | 1.72 | 0.97 | 5.74 | 2.51 |
| Possible range | 1–5 | 1–5 | 1–5 | 0–9 | 0–9 | 0–9 | 0–9 | 0–7 | 0–17 | 0–5 | 0–4 | 0–3 | 0–20 | 0–8 |
Note. Correlations greater than or equal to |.50| are shown in boldface; all correlations > |.10| are significant at p < .05.
2.2.2 NEO Personality Inventory-3 First Half (McCrae et al., 2005)
The NEO PI-3FH was developed within the Five Factor Model tradition, wherein each domain is the sum of six lower-order facets. This measure includes only the first half of the full NEO PI-3 to reduce participant burden and required administration time, with 120 items total (four items assessing each of the 30 facets). A 5-point Likert-type response scale is used to answer each item; the total score for each domain was computed as the mean item-level score across the six corresponding facets. This shortened measure retains the domain-level structure of the full NEO PI-3 (McCrae & Costa, 2007). In the current study, internal consistencies were good for the Neuroticism, Extraversion, and Conscientiousness domain scales (alpha = .83 to .90).
2.2.3 Personality Inventory for DSM-5 (Krueger et al., 2012)
The PID-5 was designed to assess 25 lower-order traits relevant to personality pathology as conceptualized for Section III of DSM-5. These lower-order scales can be grouped into one of five domains (i.e., Negative Affectivity, Detachment, Disinhibition, Antagonism, Psychoticism) that are consistent with the Five Factor Model (corresponding to (high) neuroticism, (low) extraversion, (low) conscientiousness, (low) agreeableness, and (low) openness, respectively). The PID-5 uses a 4-point Likert-type response scale and contains a total of 220 items, and the domain scores were computed as the sum of the three corresponding facets, with each facet scored as the mean item-level response. The scales analyzed here— Negative Affectivity, Detachment, and Disinhibition— demonstrated good internal consistency in our sample (alpha = .93 to .94).
2.3 Data Analysis
As noted previously, sample sizes varied across measures, which led to different sample sizes across analyses. Data were analyzed using SAS© software, version 9.4. Moderation was examined with Hayes’ (2013) PROCESS macro, version 2.13. Given that neuroticism is most closely and broadly associated with the internalizing disorders, we specified the models such that neuroticism/negative affectivity was the independent variable, with extraversion/detachment and conscientiousness/disinhibition as the moderators. Significant interactions were probed using two approaches: (1) simple slopes of neuroticism/negative affectivity predicting the disorder at one standard deviation above and below the mean of each moderator, and (2) Johnson-Neyman regions of significance (Bauer & Curran, 2005), a technique that identifies the range of values of the moderator (if any) for which the association between the two-way interaction (neuroticism/negative affectivity X extraversion/detachment) and outcome is significantly positive and significantly negative. Region of significance values were expressed in standard deviation units (mean = 0) to enhance interpretability. We also reported both the model R and R2— given evidence that R may more accurately estimate the magnitude of the associations between model predictors and the outcome (e.g., Ozer, 1985) but R2 is straight-forwardly interpretable as the proportion of variance accounted for— as well as the incremental variance explained by the three-way interactions.
3. Results
Descriptive statistics and zero-order correlations among study variables are shown in Table 1. As expected, corresponding pairs of scales across measures (e.g., NEO PI-3FH Neuroticism and PID-5 Negative Affectivity) showed strong convergent validity. In addition, traits were moderately to strongly associated with one another in the expected directions within and across each inventory. Internalizing disorder symptom counts were generally moderately associated with Neuroticism/Negative Affectivity, and more weakly but significantly associated with Extraversion/Detachment and Conscientiousness/Disinhibition. Last, the symptom count variables were mostly moderately associated, indicating overlap between the symptoms, with the strongest correlations among MDD, PDD, GAD, and PTSD (rs = .51 to .71).
Results of the moderation analyses are shown in Table 2.3 The three personality traits and their interactions ranged from accounting for very little variance in the disorder outcomes (R2 = .037 for agoraphobia) to accounting for substantial variance (R2 = .420 for PTSD). The three-way interaction term was a significant predictor of MDD for both personality inventories (ΔR2s = .012 and .015 for the NEO PI-3FH and PID-5, respectively), whereas no other symptoms yielded a significant three-way interaction that was replicated across measures. See Figures 1a and 1b for a depiction of the simple slopes, showing all four combinations of high and low values on each moderator. The graphs depict a similar overall pattern, taking into account that the moderators are keyed in opposite directions in the two measures.
Table 2.
Hierarchical Regressions of Internalizing Symptoms on Neuroticism/Negative Affectivity, Extraversion/Detachment, Conscientiousness/Disinhibition, and their Interactions
| NEO PI-3FH | PID-5 | |||||
|---|---|---|---|---|---|---|
| Model R2 (R) | ΔR23-way | B (SE) | Model R2 (R) | ΔR23-way | B (SE) | |
| MDD | .336*** (.580) | .012* | .409*** (.640) | .015*** | ||
| Neuroticism/Negative Affectivity | 1.80*** (.28) | .49*** (.07) | ||||
| Extraversion/Detachment | −1.14*** (.33) | .55*** (.08) | ||||
| Conscientiousness/Disinhibition | −.42 (.29) | .29** (.09) | ||||
| N/NA × E/Det | .04 (.44) | .03 (.04) | ||||
| N/NA × C/Dis | −.16 (.38) | .05 (.04) | ||||
| C/Dis × E/Det | .16 (.53) | .01 (.05) | ||||
| N/NA × E/Det × C/Dis | −1.24* (.58) | −.05*** (.01) | ||||
| PDD | .231*** (.481) | .001 | .322*** (.576) | .001 | ||
| Neuroticism/Negative Affectivity | 1.23*** (.28) | .35*** (.07) | ||||
| Extraversion/Detachment | −1.03** (.33) | .46*** (.08) | ||||
| Conscientiousness/Disinhibition | −.15 (.30) | .16 (.09) | ||||
| N/NA × E/Det | .42 (.45) | .03 (.04) | ||||
| N/NA X C/Dis | .25 (.39) | −.03 (.04) | ||||
| C/Dis × E/Det | .34 (.55) | −.00 (.06) | ||||
| N/NA × E/Det ×X C/Dis | −.29 (.64) | −.01 (.02) | ||||
| Panic | .141*** (.375) | .003 | .150*** (.387) | .002 | ||
| Neuroticism/Negative Affectivity | 3.36*** (.69) | 1.09*** (.19) | ||||
| Extraversion/Detachment | −1.30 (.81) | .45* (.21) | ||||
| Conscientiousness/Disinhibition | 1.39 (.73) | −.15 (.23) | ||||
| N/NA × E/Det | .56 (1.10) | −.11 (.12) | ||||
| N/NA × C/Dis | .88 (.95) | −.01 (.10) | ||||
| C/Dis × E/Det | 1.09 (1.33) | .21 (.14) | ||||
| N/NA × E/Det × C/Dis | −1.41 (1.56) | −.04 (.04) | ||||
| Agoraphobia | .037 (.192) | .001 | .069*** (.263) | .002 | ||
| Neuroticism/Negative Affectivity | .29 (.18) | .19*** (.05) | ||||
| Extraversion/Detachment | −.36 (.21) | .11 (.06) | ||||
| Conscientiousness/Disinhibition | .08 (.19) | −.04 (.06) | ||||
| N/NA × E/Det | .05 (.29) | .04 (.03) | ||||
| N/NA × C/Dis | .17 (.25) | −.03 (.03) | ||||
| C/Dis × E/Det | .28 (.35) | .02 (.04) | ||||
| N/NA × E/Det × C/Dis | −.25 (.41) | −.01 (.01) | ||||
| Social Anxiety | .246*** (.496) | .000 | .236*** (.486) | .000 | ||
| Neuroticism/Negative Affectivity | 1.02*** (.18) | .30*** (.05) | ||||
| Extraversion/Detachment | −.49* (.22) | .11* (.05) | ||||
| Conscientiousness/Disinhibition | .13 (.19) | .04 (.06) | ||||
| N/NA × E/Det | −.48 (.29) | .05 (.03) | ||||
| N/NA × C/Dis | .12 (.25) | −.01 (.03) | ||||
| C/Dis × E/Det | −.16 (.35) | −.02 (.04) | ||||
| N/NA × E/Det × C/Dis | −.11 (.41) | −.00 (.01) | ||||
| OCD | .097*** (.311) | .000 | .133*** (.365) | .002 | ||
| Neuroticism/Negative Affectivity | .41*** (.11) | .09** (.03) | ||||
| Extraversion/Detachment | −.02 (.13) | −.02 (.03) | ||||
| Conscientiousness/Disinhibition | .07 (.12) | .07 (.03) | ||||
| N/NA × E/Det | −.07 (.18) | .03 (.02) | ||||
| N/NA × C/Dis | .11 (.15) | .02 (.02) | ||||
| C/Dis × E/Det | .17 (.21) | −.03 (.02) | ||||
| N/NA × E/Det × C/Dis | .08 (.25) | .01 (.01) | ||||
| PTSD | .269*** (.519) | .008 | .420*** (.648) | .012*** | ||
| Neuroticism/Negative Affectivity | 3.31*** (.60) | 1.07*** (.15) | ||||
| Extraversion/Detachment | −1.88** (.70) | .96*** (.16) | ||||
| Conscientiousness/Disinhibition | −.63 (.63) | .64*** (.17) | ||||
| N/NA × E/Det | 1.46 (.94) | .01 (.09) | ||||
| N/NA × C/Dis | 1.07 (.81) | −.10 (.07) | ||||
| C/Dis × E/Det | 2.56* (1.13) | .26* (.10) | ||||
| N/NA × E/Det × C/Dis | −2.16 (1.34) | −.09** (.03) | ||||
| GAD | .280*** (.529) | .016* | .294*** (.542) | .003 | ||
| Neuroticism/Negative Affectivity | 2.15*** (.26) | .63*** (.07) | ||||
| Extraversion/Detachment | −.40 (.31) | .07 (.08) | ||||
| Conscientiousness/Disinhibition | .41 (.28) | .05 (.08) | ||||
| N/NA × E/Det | .65 (.42) | −.03 (.04) | ||||
| N/NA × C/Dis | .26 (.36) | −.09* (.04) | ||||
| C/Dis × E/Det | .74 (.51) | .14** (.05) | ||||
| N/NA × E/Det × C/Dis | −1.41* (.60) | −.02 (.01) | ||||
Note. N = 255–260 for the NEO PI-3FH analyses and 445–454 for PID-5 analyses. Unstandardized regression weights from the final step of each model are shown.
p < .05,
p < .01,
p < .001.
Figure 1.
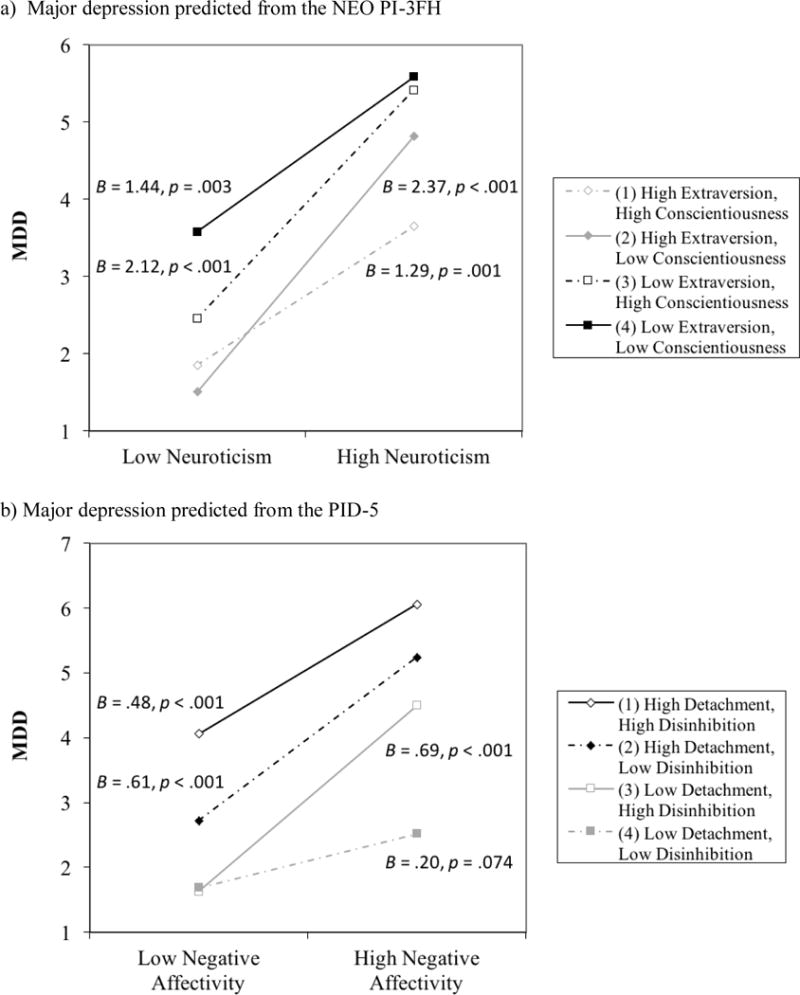
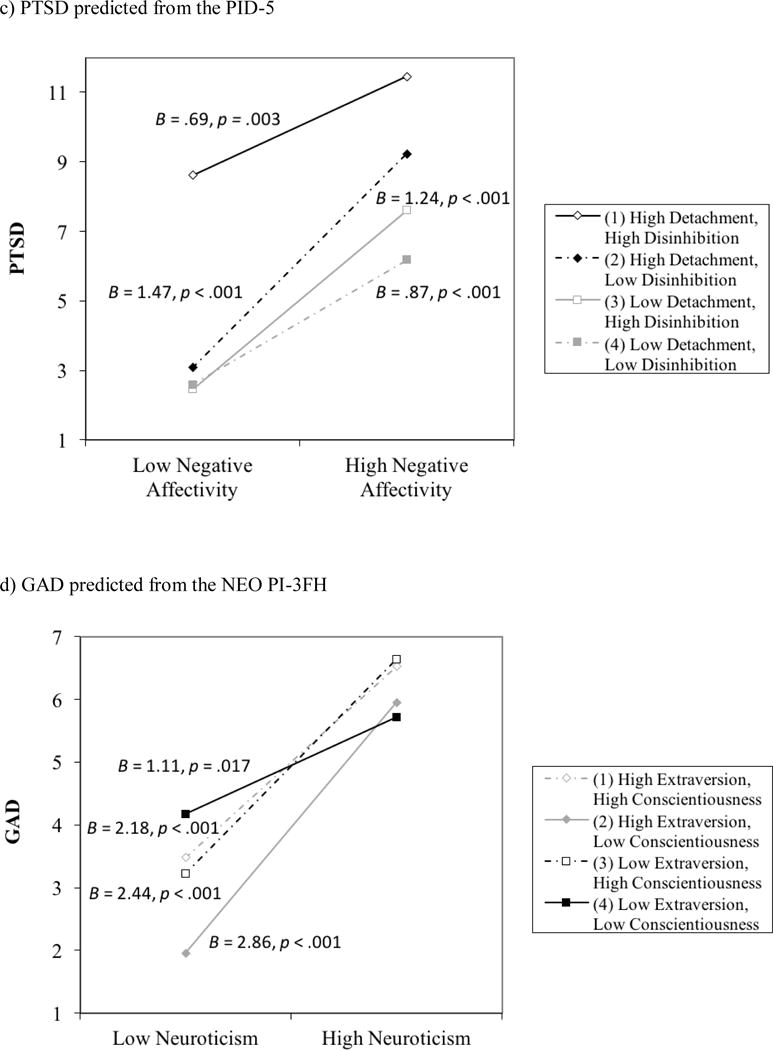
Unstandardized simple slopes for significant three-way interactions, showing Neuroticism/Negative Affectivity predicting the disorder at one standard deviation above (high) and below (low) the mean of each moderator.
For the NEO PI-3FH model, the simple slopes of Neuroticism predicting MDD were positive and significant regardless of the moderator values. These slopes did not differ significantly from one another, although the slope when Extraversion and Conscientiousness were both high trended towards being weaker than those of the other three moderator groupings (ps = .10 to .19). Johnson-Neyman regions of significance indicated that the interaction between Neuroticism and Extraversion was non-significant at nearly all observed values of Conscientiousness (i.e., the positive effect of Neuroticism did not depend on levels of Extraversion, and the negative effect of Extraversion did not depend on levels of Neuroticism). However, the Neuroticism X Extraversion interaction became significantly negative (that is, high levels of Extraversion attenuated the association between Neuroticism and MDD) when Conscientiousness was very high (lower boundary for the region of significance was 2.00 SDs above the mean; 99.61%ile).
For the PID-5 predicting MDD, the simple slopes were significantly positive, except for when Detachment and Disinhibition were both low (B = .201, p = .074). Furthermore, the slope at low Detachment and low Disinhibition was significantly weaker or approached significance as compared to the slopes of the other three moderator groupings (ps = .005 to .092), whereas the slopes of the other three groups did not significantly differ from one another (ps > .27). The Negative Affectivity X Detachment interaction was significantly positive at moderately low levels of Disinhibition (at or below −1.32SDs; 29.1%ile), such that low levels of Detachment attenuated the association between Negative Affectivity and MDD. This interaction was non-significant at average levels of Disinhibition, yielding only positive main effects of Negative Affectivity and Detachment. However, the interaction was reversed at very high levels of Disinhibition (at or above 2.01SDs; 97.36%ile), where low Detachment failed to mitigate the effect of Negative Affectivity on Depression. In summary, a protective effect against the harmful outcome high levels of Neuroticism/Negative Affectivity (i.e., major depression) was observed in the presence of low-risk levels of both Extraversion/Detachment and Conscientiousness/ Disinhibition for both the NEO PI-3FH and PID-5, although the observed effect was stronger for the PID-5 trait scales.
Most of the other disorders (PDD, panic, agoraphobia, social anxiety, OCD) did not yield any significant two- or three-way interactions in either personality inventory. However, PTSD was significantly predicted by the Extraversion × Conscientiousness interaction in the NEO PI-3FH analyses, and by the three-way interaction in the PID-5 analyses (as well as a significant Detachment X Disinhibition two-way interaction); the three-way interaction in the NEO analyses only approached significance (p = .108). For the PID-5 three-way interaction (shown in Figure 1c; ΔR2 = .012), all Negative Affectivity simple slopes were positive. However, contrary to findings for MDD, the slope for the group with high levels of Detachment and of Disinhibition was significantly weaker or approached significance compared to the other three moderator groups (ps = .01 to .16), which did not differ significantly from one another (ps > .28). Similar to the models predicting MDD, the two-way interaction between Negative Affectivity and Detachment was significantly positive at low levels of Disinhibition (−1.13SDs; 14.8%ile), levels of Disinhibition, and significantly negative at very high levels of Disinhibition (1.73SDs; indicating the presence of a protective effect. This interaction was non-significant at average 95.1%ile). Last, the significant two-way interaction between Extraversion/Detachment and Conscientiousness/Disinhibition was consistent in pattern across measures: high Conscientiousness/low Disinhibition was protective against the negative effects of low Extraversion/High Detachment.
GAD was significantly predicted by the three-way interaction in the NEO PI-3FH analyses (see Figure 1d; ΔR2 = .016) and by two two-way interactions (Negative Affectivity X Disinhibition; Detachment X Disinhibition) in the PID-5 analyses. In the NEO PI-3FH analyses, all simple slopes were positive, but the group with low levels of both Extraversion and Conscientiousness had a slope that was significantly weaker or approached significance compared to the other three moderator groups (ps = .015 to .067), whereas the other three groups did not differ in slope from one another (ps > .30). This pattern was similar to that observed in the PTSD three-way interaction and opposite of the simple slopes observed for MDD. The Neuroticism X Extraversion interaction was significantly positive at moderately low levels of Conscientiousness (−.28SDs; 38.4%ile), indicating that there was a weaker association between Neuroticism and GAD at low levels of Extraversion, whereas the interaction was non-significant at all other values of Conscientiousness. Finally, turning to the PID-5 model for GAD, the Negative Affectivity X Detachment interaction was negative and yielded a pattern consistent with the association described above for the NEO, whereas the positive Detachment X Disinhibition interaction indicated that low Disinhibition was protective against the harmful effects of high Detachment.
Given that three disorders (i.e., MDD, PTSD, GAD) showed evidence of a three-way interaction with at least one of the personality measures and were all strongly correlated (rs = .51 to .71), we also conducted follow-up analyses to examine the specificity of these interactions by including the other two disorders as covariates (e.g., the main effects of PTSD and GAD were added for the models predicting MDD). In all four models with significant three-way interactions, the magnitude of the interaction term was reduced after adding the other disorders as covariates. When predicting MDD with covariates in the model, the three-way interaction term was at a trend level for the NEO PI-3FH model (B = −.85, SE = .49, p = .076; 31% reduction in B magnitude relative to the model without covariates) and was just above conventional levels of significance for the PID-5 model (B = −.03, SE = .01, p = .052; 40% reduction). Similarly, the model with the NEO traits predicting GAD had a three-way interaction that approached significance (B = −1.02, SE = .55, p = .064; 28% reduction). In contrast, when predicting PTSD from the PID-5, the three-way interaction was more substantially weakened (B = −.04, SE = .02, p = .126; 56% reduction) and both MDD and GAD had significant main effects (ps < .001). Thus, the shared variance among these three disorders contributed to some degree to the significant three-way interactions, but it does not appear to be fully responsible for the interactions.
4. Discussion
The current study was the first to examine a three-way interaction among neuroticism-, extraversion-, and conscientiousness-related traits in a psychiatric sample and across a broad range of internalizing disorders. Our primary hypothesis was that the three-way interaction would significantly predict depression, whereas the examination of anxiety disorders was more exploratory. We found strong evidence for the three-way interaction in predicting symptoms of major depressive disorder, with a consistent three-way interaction pattern across two measures of personality that was highly similar to those reported in previous studies with non-clinical samples (Dinovo & Vasey, 2011; Vasey et al., 2013, 2014). Thus, these findings further bolster confidence in the robustness of the interaction, across samples varying in clinical status, age, personality measures, and assessment method for depression (self-report vs. clinical interview). With regard to the three-way interaction predicting anxiety disorders, we tentatively hypothesized that this interaction may be present or strongest for social anxiety, PTSD, GAD, and PDD given their similarities in personality profiles with MDD. We found some evidence for this interaction for PTSD and GAD, but not for social anxiety and PDD (see some possible post hoc explanations below). Though the three-way interaction term was significant in only one of the personality measures for both of these disorders (i.e., PID-5 for PTSD and NEO PI-3FH for GAD), one or more significant two-way interactions were present in the other personality measures, providing consistent evidence of synergistic relationships across personality inventories. Additionally, comorbidity with depression appears to contribute to the interactions for PTSD and GAD, but does not seem to account entirely for them (particularly in the case of GAD).
The nature of the three-way interaction in MDD was generally such that high levels of conscientiousness-related traits and extraversion-related traits in combination were protective against the deleterious effects of high levels of neuroticism-related traits; in fact, the association between neuroticism and MDD was not significant at high levels of both traits in the PID-5 and the small intercept indicated low levels of predicted MDD. The PID-5 also showed evidence of the reverse three-way interaction, wherein at very high levels of disinhibition, low detachment was weakened in its protection against the maladaptive effects of high negative affectivity. levels of depression even at high-risk levels of detachment and disinhibition. Furthermore, similar to prior work Nonetheless, simple slopes indicated that low negative affectivity remained associated with low by Vasey and colleagues, this reverse interaction was less consistent (i.e., only present in one measure) and less strong (i.e., limited in the range at which it was observed) than the protective pattern of high extraversion- and conscientiousness-related traits described previously.
It is important to acknowledge that the effect sizes of the three-way interaction in predicting depression (and any other disorders) were small (change in R2 for significant interaction terms = .012 to .016). To examine whether the combined protective effect of high extraversion and high conscientiousness may be substantively meaningful (i.e., applicable to a non-negligible proportion of the sample), we identified individuals that scored at least moderately high (in the adaptive direction) on both of these scales. Specifically, we tallied those with scores of 4 or greater on NEO PI-3FH Extraversion and Conscientiousness (80% of the maximum possible score), or scores of 2 or less on PID-5 Detachment and Disinhibition (22% of the maximum possible score). Few individuals met this criteria for the NEO (2.7% of the sample, 7 people), whereas a sizable portion of the sample met these criteria for the PID-5 (19.9% of the sample; 92 people). These different rates likely at least partially reflect differences in “difficulty” between the two measures. That is, given that abnormal measures of personality such as the PID-5 are most precise at high-risk, extreme levels of traits (e.g., Suzuki, Samuel, Pahlen, & Krueger, 2015), they should better assess the typical trait levels found in clinical samples and therefore more readily detect interactions.
Overall, it is notable and encouraging that even in a treatment-seeking sample with high rates of internalizing disorders (a) there was reasonable variability in the “low-risk” ends of personality traits, (b) such protective traits were sufficient to either override or decrease the risk conferred by high neuroticism for depression, and (c) although the combination of two “high-risk” traits may weaken the protective ability of a third “low-risk” trait, this effect is relatively small and does not appear more marked than in prior work with non-clinical samples. Taken together, these results suggest that it is relevant and important to consider interactive effects when examining personality in relation to depression, not only in general unselected samples but also in currently-distressed clinical samples.
The analyses for GAD and PTSD showed both of the above patterns for the three-way interactions. But in contrast to the predominance of the protective interaction pattern in MDD, for GAD and PTSD the detrimental amplifying effects of the combination of low extraversion and low conscientiousness appeared to be the stronger and more consistent interaction pattern. The simple slopes between neuroticism and symptoms were significantly weakened (though the slopes were still positive) at low levels of both traits and the regression line had a relatively high intercept. In other words, there was a tendency for the combination of low extraversion and low conscientiousness to increase risk for PTSD and GAD, even at low levels of neuroticism, whereas high levels of these traits did not significantly impact neuroticism’s association with these symptoms. While this reverse interaction pattern was observed only at very high levels of Disinhibition for the PID-5 in PTSD, it was evident at moderately low levels of Conscientiousness (found in almost 40% of the sample) for the NEO in GAD. Thus, it appears that for PTSD and GAD, the combination of high-risk levels of extraversion and conscientiousness may be particularly detrimental, although low-risk levels of traits also conferred some protection against high neuroticism.
It was striking that we did not find any interactions (two- or three-way) for any of the other anxiety disorders or for OCD, despite some theory that high conscientiousness/effortful control should protect against risk conferred by high neuroticism for the mood and anxiety disorders generally (e.g., Lonigan & Phillips, 2001). As described previously, one commonality shared by MDD, PTSD, and GAD is they are characterized by particularly high levels of neuroticism (Watson & Naragon-Gainey, 2014; Watson et al., 2005), and empirical analyses of comorbidity data have consistently found that these three disorders form a latent factor, labeled “anxious-misery disorders” or “distress disorders” (e.g., Kendler, Prescott, Myers, & Neale, 2003; Krueger, 1999; Sellbom, Ben-Porath, & Bagby, 2008; Slade & Watson, 2006; Watson, 2005). Relative to the more situationally-specific “fear disorders” (e.g., panic, social anxiety, OCD, agoraphobia, specific phobia) derived from these comorbidity analyses, the distress disorders have a broad, generalized focus of distress. Thus, the wide-ranging effects of extraversion and conscientiousness in daily life (e.g., greater approach of enjoyable activities, higher goal-striving, more social contact) may directly and generally bear on the broad implications of very high neuroticism (e.g., general withdrawal, perseverative thinking, self-criticism) that are manifest in the distress disorders. In contrast, specific learning experiences (e.g., bullying, modeling of health anxiety, being bitten by a dog) and specific lower-order traits (e.g., anxiety sensitivity, fear of negative evaluation, disgust sensitivity) may be most relevant to the fear disorders, which are more situationally-specific and less impacted by broad personality functioning. Our finding of disorder-specificity also may be due in part to a statistical phenomenon: the detection of these interactions requires adequate variance at extreme trait levels (McClelland & Judd, 1993), and so the more moderate levels of neuroticism associated with the fear disorders may require larger samples for small interaction effects to emerge.
We thought it particularly plausible that the three-way interaction would occur in other disorders closely related to depression, such as PDD (which differs from depression primarily with regard to chronicity) and social anxiety (which also tends to have low levels of positive affectivity). In addition, dysthymic disorder (the DSM-IV predecessor to PDD) consistently loads with the distress disorders (Krueger, 1999; Slade & Watson, 2006; Watson, 2005), and social anxiety has been linked to the distress disorders in some structural studies (Naragon-Gainey, Prenoveau, Brown, & Zinbarg, 2016). But neither of these disorders showed any interactive effects among traits in our data. With regard to social anxiety, there is evidence that generalized or interaction social anxiety (that is, social anxiety in most or all social interactions) is distinct in terms of personality and functioning from performance social anxiety (that is, social anxiety in specific situations in which one is observed), and that interaction social anxiety is more closely related to depression and to the distress disorders (Carter & Wu, 2010; Hughes et al., 2006; Naragon-Gainey et al., 2016). Thus, it is plausible that the three-way interaction may have emerged for interaction social anxiety, but combining these symptoms in the current study may have inhibited the detection of this effect.
Consistent with its more chronic course relative to MDD, PDD/dysthymic disorder generally exhibits more extreme levels of neuroticism, extraversion, and conscientiousness than does MDD or other anxiety disorders (Klein et al., 2011; Kotov et al., 2010). Thus, low-risk levels of these traits may be quite rare in the context of high PDD symptoms, or the observed trait levels may be so intense that any one extreme trait is sufficient to increase risk for PDD and its effects are too strong to be modulated by the presence of other low-risk traits. One possible reason for these more extreme trait levels is that the chronic nature of PDD may increase the likelihood of “scar” effects, wherein personality traits are changed by the experience of the disorder (Klein et al., 2011). To test this post-hoc explanation, we compared mean trait levels of participants with and without PDD in this sample, using Cohen’s d to quantify the magnitude of differences. Consistent with this hypothesis, individuals with PDD had higher levels of Neuroticism/Negative Affect (d = .29 and .45, respectively), lower Extraversion/higher Detachment (d = −.30 and .45), and lower Conscientiousness/higher Disinhibition (d = −.25 and .29) than the rest of the sample. Note, however, that these effects sizes are only small to medium in magnitude and do not indicate extreme trait differences between psychiatric outpatients with and without PDD.
Strengths of the current study include a relatively large treatment-seeking sample, dimensional assessment of symptoms via clinical interview, and an examination of results across two personality measures. However, there are a number of study limitations that are important to consider when interpreting our results. The study design was cross-sectional, and as such we cannot draw any conclusions regarding causal directions of the observed associations. Nonetheless, it is encouraging that a prior study found evidence that this interaction prospectively predicts depression (Vasey et al., 2014). Relatedly, since most study participants already had a disorder at the time of assessment, the results cannot speak to the development of psychopathology or disorder onset. In addition, findings may have differed if we had used other personality inventories that assessed variations of these traits (for example, measures of positive affectivity instead of extraversion), though we note that findings have been mostly consistent across measures in prior studies. It is also important to note that the disorders were generally moderately to strongly correlated with one another, aligned with expected levels of comorbidity among these conditions, so the symptom-specific regression analyses should not be interpreted as independent of one another. However, we attempted to examine the impact of this dependence by including all disorders that were significantly predicted by the three-way interaction as covariates in a second set of regression analyses. Finally, as described previously, the incremental variance contributed by the three-way interaction term was small, though this magnitude is fairly typical for significant three-way interactions. McClelland and Judd (1993) describe several reasons why it is difficult to detect and quantify the magnitude of interaction effects in observational studies, leading them to suggest that the presence of a significant effect is more important than its effect size. Nevertheless, in some contexts, it may be reasonable and more efficient to focus on the main effects of these traits.
Future studies should examine whether the disorder-specific associations we found generalize to other samples with other properties, including non-clinical samples. It will also be important to begin to specify the mechanisms (e.g., rumination, decreased avoidance) by which the three-way interaction protects from symptoms of distress disorders and the extent to which levels of these traits may be impacted by preventative measures or interventions.
Highlights.
Personality traits interacted when predicting some disorders in a psychiatric sample.
High extraversion, conscientiousness reduced the risk conferred by high neuroticism.
The most consistent effects were for symptoms of major depression.
There was also evidence of trait interactions for PTSD and GAD symptoms.
Acknowledgments
This work was supported by a grant from the National Institute of Mental Health (R01 MH080086, Simms). The opinions expressed are solely those of the authors and not necessarily those of the funding source.
APPENDIX
Hierarchical Regressions of Internalizing Symptoms on Neuroticism/Negative Affectivity, Extraversion/Detachment, Conscientiousness/Disinhibition, and their Interactions, with Gender as a Covariate
| NEO PI-3FH | PID-5 | |||||
|---|---|---|---|---|---|---|
| Model R2 (R) | ΔR23-way | B (SE) | Model R2 (R) | ΔR23-way | B (SE) | |
| MDD | .338*** (.581) | .012* | .412*** (.642) | .014*** | ||
| Gender | −.27 (.30) | .39 (.22) | ||||
| Neuroticism/Negative Affectivity | 1.85*** (.28) | .47*** (.07) | ||||
| Extraversion/Detachment | −1.13*** (.33) | .55*** (.08) | ||||
| Conscientiousness/Disinhibition | −.41 (.29) | .30*** (.09) | ||||
| N/NA X E/Det | .06 (.44) | .03 (.04) | ||||
| N/NA X C/Dis | −.17 (.38) | .05 (.04) | ||||
| C/Dis X E/Det | .16 (.53) | .00 (.05) | ||||
| N/NA X E/Det X C/Dis | −1.24* (.58) | −.05*** (.01) | ||||
| PDD | .241*** (.491) | .001 | .344*** (.587) | .001 | ||
| Gender | .56 (.31) | .85*** (.21) | ||||
| Neuroticism/Negative Affectivity | 1.13*** (.29) | .31*** (.07) | ||||
| Extraversion/Detachment | −1.06** (.33) | .47*** (.08) | ||||
| Conscientiousness/Disinhibition | −.17 (.30) | .19* (.09) | ||||
| N/NA X E/Det | .37 (.45) | .03 (.04) | ||||
| N/NA X C/Dis | .28 (.39) | −.02 (.04) | ||||
| C/Dis X E/Det | .36 (.54) | −.02 (.05) | ||||
| N/NA X E/Det X C/Dis | −.26 (.64) | −.01 (.01) | ||||
| Panic | .152*** (.390) | .003 | .156*** (.394) | .002 | ||
| Gender | 1.35 (.75) | .92 (.57) | ||||
| Neuroticism/Negative Affectivity | 3.12*** (.70) | 1.05*** (.19) | ||||
| Extraversion/Detachment | −1.37 (.81) | .46* (.21) | ||||
| Conscientiousness/Disinhibition | 1.34 (.73) | −.12 (.23) | ||||
| N/NA X E/Det | .45 (1.10) | −.10 (.12) | ||||
| N/NA X C/Dis | .93 (.95) | −.01 (.10) | ||||
| C/Dis X E/Det | 1.11 (1.33) | .19 (.14) | ||||
| N/NA X E/Det X C/Dis | −1.33 (1.56) | −.04 (.04) | ||||
| Agoraphobia | .037 (.193) | .001 | .069*** (.262) | .002 | ||
| Gender | −.00 (.20) | −.04 (.16) | ||||
| Neuroticism/Negative Affectivity | .29 (.19) | .19*** (.05) | ||||
| Extraversion/Detachment | −.36 (.21) | .11 (.06) | ||||
| Conscientiousness/Disinhibition | .08 (.19) | −.04 (.06) | ||||
| N/NA X E/Det | .05 (.29) | .04 (.03) | ||||
| N/NA X C/Dis | .17 (.25) | −.03 (.03) | ||||
| C/Dis X E/Det | .28 (.35) | .02 (.04) | ||||
| N/NA X E/Det X C/Dis | −.25 (.41) | −.01 (.01) | ||||
| Social Anxiety | .248*** (.498) | .000 | .237*** (.487) | .000 | ||
| Gender | −.18 (.20) | −.18 (.15) | ||||
| Neuroticism/Negative Affectivity | 1.05*** (.19) | .31*** (.05) | ||||
| Extraversion/Detachment | −.48* (.22) | .11* (.05) | ||||
| Conscientiousness/Disinhibition | .14 (.20) | .04 (.06) | ||||
| N/NA X E/Det | −.47 (.29) | .05 (.03) | ||||
| N/NA X C/Dis | .11 (.25) | −.01 (.03) | ||||
| C/Dis X E/Det | −.17 (.35) | −.02 (.04) | ||||
| N/NA X E/Det X C/Dis | −.12 (.41) | −.00 (.01) | ||||
| OCD | .001*** (.318) | .000 | .133*** (.365) | .002 | ||
| Gender | −.13 (.12) | −.06 (.09) | ||||
| Neuroticism/Negative Affectivity | .43*** (.11) | .09** (.03) | ||||
| Extraversion/Detachment | −.01 (.13) | −.02 (.03) | ||||
| Conscientiousness/Disinhibition | .07 (.12) | .06 (.03) | ||||
| N/NA X E/Det | −.06 (.18) | .03 (.02) | ||||
| N/NA X C/Dis | .10 (.15) | .02 (.02) | ||||
| C/Dis X E/Det | .16 (.21) | −.02 (.02) | ||||
| N/NA X E/Det X C/Dis | .07 (.25) | .01 (.01) | ||||
| PTSD | .269*** (.519) | .008 | .424*** (.651) | .012*** | ||
| Gender | −.12 (.65) | .87* (.44) | ||||
| Neuroticism/Negative Affectivity | 3.33*** (.61) | 1.02*** (.15) | ||||
| Extraversion/Detachment | −1.88** (.70) | .97*** (.16) | ||||
| Conscientiousness/Disinhibition | −.63 (.63) | .66*** (.17) | ||||
| N/NA X E/Det | 1.47 (.95) | .01 (.09) | ||||
| N/NA X C/Dis | 1.07 (.81) | −.10 (.08) | ||||
| C/Dis X E/Det | 2.55* (1.14) | .24* (.10) | ||||
| N/NA X E/Det X C/Dis | −2.17 (1.34) | −.09** (.03) | ||||
| GAD | .298*** (.546) | .015* | .310*** (.557) | .002 | ||
| Gender | .73* (.29) | .71*** (.21) | ||||
| Neuroticism/Negative Affectivity | 2.02*** (.27) | .59*** (.07) | ||||
| Extraversion/Detachment | −.44 (.31) | .07 (.08) | ||||
| Conscientiousness/Disinhibition | .38 (.28) | .07 (.08) | ||||
| N/NA X E/Det | .59 (.42) | −.02 (.04) | ||||
| N/NA X C/Dis | .29 (.36) | −.09* (.04) | ||||
| C/Dis X E/Det | .75 (.51) | .13* (.05) | ||||
| N/NA X E/Det X C/Dis | −1.37* (.59) | −.02 (.01) | ||||
Note. N = 255–260 for the NEO PI-3FH analyses and 445–454 for PID-5 analyses. Unstandardized regression weights from the final step of each model are shown. Gender was coded as 1 = male, 2 = female.
p < .05,
p < .01,
p < .001.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
These studies did not use the Five Factor traits, but rather the related constructs described previously (i.e., negative affectivity and positive affectivity, behavioral inhibition system and behavioral activation system, effortful control).
Note that sample sizes were determined based on the primary aims of the larger study. However, a power analysis using effect sizes from prior studies of three-way personality interactions predicting depression in adults (Dinovo & Vasey, 2011; Vasey et al., 2014) indicated that the current study has adequate power (.83) to detect a significant three-way interaction for analyses with the NEO PI-3FH and excellent power (.97) for analyses with the PID-5.
Since prior studies have statistically accounted for gender (Dinovo & Vasey, 2011; Vasey et al., 2013, 2014), we also ran all analyses with gender as a covariate. This did not appreciably affect the results (e.g., all two-way and three-way interactions yielded identical conclusions), so analyses without gender are presented in the main text. Complete results from the analyses that include gender as a covariate may be found in the Appendix.
References
- Bauer DJ, Curran PJ. Probing interactions in fixed and multilevel regression: Inferential and graphical techniques. Multivariate Behavioral Research. 2005;40:373–400. doi: 10.1207/s15327906mbr4003_5. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Carter SA, Wu KD. Symptoms of specific and generalized social phobia: An examination of discriminant validity and structural relations with mood and anxiety symptoms. Behavior Therapy. 2010;41:254–265. doi: 10.1016/j.beth.2009.04.002. [DOI] [PubMed] [Google Scholar]
- Dinovo SA, Vasey MW. Reactive and self-regulatory dimensions of temperament: Interactive relations with symptoms of general distress and anhedonia. Journal of Research in Personality. 2011;45:430–440. doi: 10.1016/j.jrp.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershuny BS, Sher KJ. The relation between personality and anxiety: Findings from a 3-year prospective study. Journal of Abnormal Psychology. 1998;107:252–262. doi: 10.1037//0021-843x.107.2.252. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press; 2013. [Google Scholar]
- Hughes AA, Heimberg RG, Coles ME, Gibb BE, Liebowitz MR, Schneier FR. Relations of the factors of the tripartite model of anxiety and depression to social anxiety. Behaviour Research and Therapy. 2006;44:1629–1641. doi: 10.1016/j.brat.2005.10.015. [DOI] [PubMed] [Google Scholar]
- Jeronimus BF, Kotov R, Riese H, Ormel J. Neuroticism’s prospective association with mental disorders halves after adjustment for baseline symptoms and psychiatric history, but the adjusted association hardly decays with time: A meta-analysis on 59 longitudinal/prospective studies with 443313 participants. Psychological Medicine. doi: 10.1017/S0033291716001653. (in press) [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr, Lonigan CJ. Tripartite model of depression and anxiety in youth psychiatric inpatients: Relations with diagnostic status and future symptoms. Journal of Clinical Child Psychology. 2000;29:372–382. doi: 10.1207/S15374424JCCP2903_8. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Klein DN, Kotov R, Bufferd SJ. Personality and depression: Explanatory models and review of the evidence. Annual Review of Clinical Psychology. 2011;7:269–295. doi: 10.1146/annurev-clinpsy-032210-104540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Derringer J, Markon KE, Watson D, Skodol AE. Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychological Medicine. 2012;42:1879–1890. doi: 10.1017/S0033291711002674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychological Bulletin. 2010;136:768–821. doi: 10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, Phillips BM. Temperamental influences on the development of anxiety disorders. In: Vasey MW, Dadds MR, editors. The developmental psychopathology of anxiety. New York: Oxford University Press; 2001. pp. 60–91. [Google Scholar]
- Markon KE, Chmielewski M, Miller CJ. The reliability and validity of discrete and continuous measures of psychopathology: A quantitative review. Psychological Bulletin. 2011;137:856–879. doi: 10.1037/a0023678. [DOI] [PubMed] [Google Scholar]
- McClelland GH, Judd CM. Statistical difficulties of detecting interactions and moderator effects. Psychological Bulletin. 1993;114:376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Costa PT. Brief versions of the NEO PI-3. Journal of Individual Differences. 2007;28:116–128. [Google Scholar]
- McCrae RR, Costa PT, Martin TA. The NEO PI-3: A more readable Revised NEO Personality Inventory. Journal of Personality Assessment. 2005;84:261–270. doi: 10.1207/s15327752jpa8403_05. [DOI] [PubMed] [Google Scholar]
- Naragon-Gainey K, Gallagher MW, Brown TA. Stable “trait” variance of temperament as a predictor of the temporal course of depression and social phobia. Journal of Abnormal Psychology. 2013;122:611–623. doi: 10.1037/a0032997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naragon-Gainey K, Prenoveau JM, Brown TA, Zinbarg RE. A comparison and integration of structural models of depression and anxiety in a clinical sample: Support for and validation of the tri-level model. Journal of Abnormal Psychology. 2016;125:853–867. doi: 10.1037/abn0000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozer DJ. Correlation and the coefficient of determination. Psychological Bulletin. 1985;97(2):307–315. [Google Scholar]
- Sheehan DV, Lecubrier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Supp. 20):22–33. [PubMed] [Google Scholar]
- Sellbom M, Ben-Porath YS, Bagby RM. On the hierarchical structure of mood and anxiety disorders: Confirmatory evidence and elaboration of a model of temperament markers. Journal of Abnormal Psychology. 2008;117:576–590. doi: 10.1037/a0012536. [DOI] [PubMed] [Google Scholar]
- Simms LJ, Goldberg LR, Roberts JE, Watson D, Welte J, Rotterman JH. Computerized adaptive assessment of personality disorder: Introducing the CAT-PD project. Journal of Personality Assessment. 2011;93:380–389. doi: 10.1080/00223891.2011.577475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- Suzuki T, Samuel DB, Pahlen S, Krueger RF. DSM-5 alternative personality disorder model traits as maladaptive extreme variants of the five-factor model: An item-response theory analysis. Journal of Abnormal Psychology. 2015;124:343–354. doi: 10.1037/abn0000035. [DOI] [PubMed] [Google Scholar]
- Vasey MW, Harbaugh CN, Fisher LB, Heath JH, Hayes AF, Bijttebier P. Temperament synergies in risk for and protection against depressive symptoms: A prospective replication of a three-way interaction. Journal of Research in Personality. 2014;53:134–147. [Google Scholar]
- Vasey MW, Harbaugh CN, Lonigan CJ, Phillips BM, Hankin BL, Willem L, Bijttebier P. Dimensions of temperament and depressive symptoms: Replicating a three-way interaction. Journal of Research in Personality. 2013;47:908–921. doi: 10.1016/j.jrp.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verstraeten K, Vasey MW, Raes F, Bijttebier P. Temperament and risk for depressive symptoms in adolescence: Mediation by rumination and moderation by effortful control. Journal of Abnormal Child Psychology. 2009;37:349–361. doi: 10.1007/s10802-008-9293-x. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: A qualitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Watson D, Gamez W, Simms LJ. Basic dimensions of temperament and their r relation to anxiety and depression: A symptom-based perspective. Journal of Research in Personality. 2005;39:46–66. [Google Scholar]
- Watson D, Naragon-Gainey K. Personality, emotions, and the emotional disorders. Clinical Psychological Science. 2014;2:422–442. doi: 10.1177/2167702614536162. [DOI] [PMC free article] [PubMed] [Google Scholar]


