Highlights
-
•
Elderly women with knee osteoarthritis are at risk of developing limitations physical.
-
•
Hidrotherapy improves pain, function, muscle power and strength in older women with knee osteoarthritis.
-
•
Hydrotherapy is likely to be an effective treatment option for these patients.
Keywords: Rehabilitation, Hydrotherapy, Osteoarthritis, Pain, Randomized controlled trial, Women
Abstract
Background
Currently, there is poor evidence of the effect of hydrotherapy alone on patients with hip or knee osteoarthritis.
Objectives
The study aimed to assess the impact of hydrotherapy on pain, function, and muscle function in older women with knee osteoarthritis.
Methods
A randomized controlled trial was conducted to evaluate the efficacy of hydrotherapy in women with knee osteoarthritis. Seventy-three women aged 65 and older were randomized to hydrotherapy (n = 36) or a control group (n = 37). The hydrotherapy group received the intervention program in a heated pool (twice per week for six weeks) and an educational protocol while the control group received an educational protocol only. Primary outcomes (before and post-treatment) were pain intensity (0–100) and function (0–100), assessed with the WOMAC questionnaire. Secondary outcomes (before and post-treatment) were knee extensor and knee flexor muscle performance (strength, power, and endurance), assessed by an isokinetic dynamometer. The magnitude of change between the groups for the outcomes was calculated using linear regression models adjusted by baseline outcome values.
Results
The hydrotherapy group had better outcomes for pain (adjusted mean difference = 11 points, 95% CI: 3–18) and function (adjusted mean difference = 12 points, 95% CI: 5–18). Patients receiving hydrotherapy had better performance for knee flexor and extensor strength, knee flexor power, and knee extensor endurance.
Conclusion
Older women with knee osteoarthritis are likely to have benefits from a course of hydrotherapy exercises.
Registry of clinical trials (Trial number RBR-8F57KR) – http://www.ensaiosclinicos.gov.br/rg/RBR-8f57kr/.
Introduction
Osteoarthritis (OA) is one of the most prevalent musculoskeletal diseases in the world.1 Approximately 10% of the population aged 65 years and over present with OA symptoms and more than half of the population have subclinical radiographic OA.2, 3, 4 OA prevalence increases with age, and women show higher prevalence estimates in the frequency and severity of symptoms than men.5 OA is a chronic degenerative joint disease and the knee is its most frequently affected weight-bearing joint.1, 2 OA is associated with loss of physical function and a decline in quality of life in the elderly.6, 7
International clinical practice guidelines highlight the importance of non-pharmacological interventions, such as educational and exercise programs, as first-line treatment options in the management of hip and knee OA.8, 9 Exercise can be offered as water-based (hydrotherapy) or land-based exercises for hip and knee OA.10, 11 Hydrotherapy is often recommended as a treatment option in the elderly population mostly because it is performed in a safer environment with a lower risk of falls than land-based exercises.12 Furthermore, patients with OA show higher levels of treatment adherence with hydrotherapy than other forms of conservative management.6, 12, 13, 14, 15
It is argued that hydrotherapy offers additional physiological and biomechanical benefits compared to land-based exercises for patients with knee OA and these could lead to better clinical outcomes. It is hypothesized that hydrotherapy speeds patients’ early dynamic muscular strengthening and active mobilization even in the presence of severe pain.8, 16, 17 Furthermore, aquatic buoyancy potentially reduces weight-bearing stresses on joints, bones, and muscles. Hydrotherapy also allows the performance of closed-chain exercises, which are potentially painful with greater weight bearing.13
Randomized controlled trials comparing the efficacy of hydrotherapy to land-based exercises for patients with knee and/or hip OA have been previously conducted, but the findings are conflicting. Results range from hydrotherapy being superior for pain,6, 18 equally effective for function6, 18 and pain,19 and inferior for pain.14 A recent systematic review on this topic reported small effects on pain, function, and quality of life compared to control group.15 Given that the majority of the selected studies investigated the effect of hydrotherapy in patients with knee and/or hip OA and only three trials included patients with knee OA alone,14, 19, 20 a specific conclusion for the effect of hydrotherapy on knee OA alone could not be made.15 However, these trials investigated the effects of hydrotherapy in a mixed adult population with knee OA14, 18, 19, 20 and none of them concerned older women with knee OA. Women with knee OA are at a higher risk of developing restriction in physical function compared to men3, 4 and the assessment of the efficacy of conservative interventions on this patient population is still limited.
Therefore, the aim of this study was to evaluate whether a structured hydrotherapy exercise program, supplemented by an educational program, improves pain, function, and muscle performance in older women with knee OA compared to an educational program.
Methods
Design
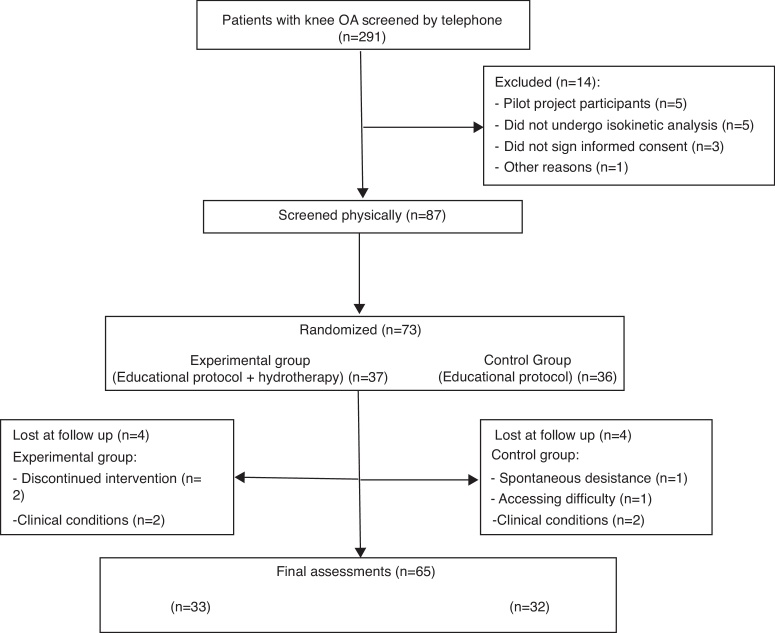
This study was a randomized controlled trial designed to evaluate the efficacy of hydrotherapy in individuals with knee OA. The study design was approved by the Ethics Committee of Universidade Federal de Minas Gerais (COEP/UFMG, Belo Horizonte, MG, Brazil; ETIC number 426/05) and was registered at the Brazilian registry of clinical trials (trial number RBR-8F57KR). The recruitment period started on March 30, 2011, and two hundred and ninety-one older women from community centers in the city of Belo Horizonte, MG, Brazil, were contacted over the telephone. A total of 87 potential participants fulfilled the eligibility criteria and were invited to participate in the study (Fig. 1). Seventy-three women agreed to participate. Baseline measures were taken for the two primary outcomes and the secondary outcomes prior to randomization. All volunteers received a detailed explanation about the objectives of the study before signing the written informed consent. The last day of assessments was September 30, 2011.
Figure 1.
Flow diagram of the study.
Randomization
Each participant was randomized either to an educational group only (n = 36) or an educational group supplemented by a hydrotherapy exercise program (n = 37). Randomization was by a computer randomization program. The randomization schedule was known only to one investigator who was not involved in recruiting participants, and it was concealed from patients and the other investigators using consecutively numbered, sealed, opaque envelopes.
Participants
Seventy-three community-dwelling elderly women with clinical and radiological diagnosis of knee OA participated in the study. To be eligible to participate in the trial, participants needed to be aged 65 years or older; have been diagnosed with OA in at least one knee based on the clinical and radiographic criteria of the American College of Rheumatology2; have not undergone lower-limb joint replacement surgery; to report no history of recent trauma in lower-limbs; not to be using any walking support (such as a walking stick or crutches); not have received physiotherapy or any other rehabilitation treatment in the past 3 months; demonstrate no cognitive limitations to do aquatic activities assessed by the Mini-Mental State Test (MMST)21; present with no open wounds or skin disease and urinary or fecal incontinence. Furthermore, the volunteers who were unable to safely enter and exit the pool or who had severe radiological diagnosis of knee OA (level IV), following the criteria of Kelgreen and Lawrence,22 were not included in the study.
Intervention
Educational protocol
The educational protocol was designed to provide educational information about the diagnosis, symptoms, prognosis, and basic care of knee OA during daily activities. The protocol consisted of a lecture given by the principal investigator for all participants, followed by a discussion. This session was provided in groups of six participants, face to face, in a classroom. The group that received the educational protocol only also received weekly advice via telephone about controlling knee loading during daily activities during six consecutive weeks.23, 24 The intervention was designed and no changes were made during the course of the study.
Hydrotherapy
A standardized hydrotherapy protocol was designed to improve pain, function, and muscle performance. The principal investigator conducted the protocol for the groups of participants. It consisted of progressive exercises, which were implemented twice a week for six weeks (Table 1). The program included three stages: warm-up (5 min), strengthening exercises (30 min), and a cool-down session (5 min). Warm-up exercises consisted of walking in the water in increasing velocity followed by stretching exercises of the anterior and posterior muscles of the lower limbs. After the warm-up session, participants performed lower limb strengthening exercises that included closed kinetic chain exercises using floats as well as multidirectional walking tasks. Participants were instructed to perform the exercises on the maximal possible intensity. The intensity of the exercise program was moderate and was controlled with the Borg scale. The cool-down session consisted of light walking followed by breathing exercises.
Table 1.
Hydrotherapy exercise protocol.
| Week | Session | Lower limb exercises | Sets and repetitions |
|---|---|---|---|
| 1 | 1st | Adaptation | – |
| 2nd | Anterior muscle exercises | 2 × 20 | |
| Posterior muscle exercises | |||
| 2 | 3rd | 2nd exercise session plus: | 2 × 20 |
| Abduction and adduction exercises | |||
| 4th | 3rd exercise session plus: | 3 × 20 | |
| Plantarflexion exercises | |||
| 3 | 5th | 4th exercise session plus: | 3 × 20 |
| Closed kinetic chain exercises (floats) | |||
| 6th | 5th exercise session plus: | 3 × 20 | |
| Multidirectional walk | |||
| 4 | 7th | 6th exercise session | 4 × 20 |
| 8th | 6th exercise session | 4 × 20 | |
| 5 | 9th | 6th exercise session | 4 × 20 |
| 10th | 6th exercise session | 4 × 25 | |
| 6 | 11th | 6th exercise session | 4 × 25 |
| 12th | 6th exercise session | 4 × 25 |
Before leaving the pool, the participants also performed a relaxation exercise session using circular floats. Pool temperature was maintained around 32 °C and the water depth was maintained constant above the umbilical height. The intervention was delivered at the Outpatient Physiotherapy Clinic at UFMG/Brazil.
Outcome measures
Primary outcomes
Primary outcomes included pain and function assessed with the Western Ontario & McMaster Universities Osteoarthritis Index (WOMAC), which were assessed before randomization and after the conclusion of the intervention protocol by a blinded assessor. The WOMAC questionnaire is a valid and reliable knee-specific measurement that has been translated and adapted to Portuguese.25 Pain and function scores were converted to a 0–100 scale using the WOMAC items that assess pain (five items) and function (17 items). Higher scores on the WOMAC indicate worse pain and functional status.
Secondary outcomes
The secondary outcomes were muscular performance assessed by an isokinetic device (Biodex System 3 Pro®, Biodex Medical Systems Inc., Shirley, NY, USA). The volunteers were submitted to a familiarization session before the baseline assessment. The volunteers were positioned as the manufacturer's recommendations for evaluation of knee flexion-extension movements. A 10-minute warm-up walk followed by 20 concentric knee flexion-extension repetitions at 180° s−1 were performed before each evaluation. The assessment protocol included concentric muscle strength performance normalized by body weight (five repetitions at 60°/s), average power (15 repetitions at 180°/s), and fatigue index (15 repetitions at 180°/s), reflecting muscle strength, power, and resistance, respectively. Power and endurance were evaluated with the same performance in the isokinetic test. Patients were assessed before randomization and after the conclusion of the intervention protocol by an investigator blinded to group allocation. The participants were previously instructed to perform maximal force and verbal encouragement was given by the researchers during the tests.
Data analysis
Data were analyzed by a statistician who was given grouped data, with data coded to allow blinding of the participants’ group allocation. Separate analyses were conducted to determine the effects of treatment for each outcome at treatment discharge (six weeks). We attempted to conduct the analysis by intention-to-treat when data from patients who dropped out of the study was available, and no attempt was made to impute values for missing data. Analysis was conducted with emphasis on estimation of the effects of intervention rather than hypothesis testing. We used analysis of covariance to maximize precision. For each analysis, the only covariate, chosen a priori, was the baseline value of the outcome. The sample size of 73 provided an 80% chance of detecting differences between groups of 20 points on a 100-point scale of function. These calculations assumed a worst-case loss to follow-up of 20%. An α-level of 0.05 was used to test statistical significance, and analyses were conducted with SPSS 12.0 for Windows (Chicago Illinois Software).
Results
Four volunteers from each group, representing 10.8% of the treatment group and 11.1% of the control group, dropped out during treatment and were not available for follow up. At treatment, discharge data were available from 33 participants in the treatment group and 32 in the control group and were used in the analysis. In the control group, the reasons for dropping out of the study included difficulties with transport to treatment facility (n = 1), presence of co-morbidities (deep venous thrombosis in the lower limb [n = 1] and high blood pressure [n = 1]), and being uncontactable (n = 1). In the hydrotherapy group, the reasons for dropping out of the study included presence of co-morbidities (food poisoning [n = 1]), surgery (n = 1), and being uncontactable (n = 2). Because we were unable to follow up participants who dropped out of the study, their data was not used in the analyses. Participants reported no significant harm or unintended effects related to treatment. The attendance rate was 83.3% (n = 2), 95.6% (n = 1), and 100% (n = 30) for the intervention group. The attendance rate was 100% (n = 32) for the control group.
Participants had a mean age of 70.8 (SD 5.1) years, mean body weight of 71.7 (SD 10.9) kg, mean height of 1.54 (SD 0.06) m, and mean body mass index (BMI) of 30.3 (SD 4.7) kg/m2. OA in both knees was present in most participants (84.6%). Thirty-six volunteers (55.4%) presented with higher pain levels in the left knee and 27 (41.5%) in the right knee, while only two participants (3.1%) reported the same pain level in both knees.
Baseline values of demographic and clinical measures were similar between groups (Table 2).
Table 2.
Baseline characteristics of participants.
| Characteristic | Experimental (n = 33) | Control (n = 32) |
|---|---|---|
| Age (yr) mean (SD) | 70.8 (5.00) | 71.0 (5.20) |
| BMI (kg/m2) mean (SD) | 30.5 (4.30) | 30.0 (5.20) |
| Dominant side, number (%) | ||
| Right | 32 (96.96%) | 30 (93.75%) |
| Left | 1 (3.03%) | 2 (6.25%) |
| Involvement, number (%) | ||
| Bilateral | 26 (78.78%) | 29 (90.62%) |
| Unilateral | 7 (21.21%) | 3 (9.37%) |
| Knee > complaint, number (%) | ||
| Both | – | 2 (6.25%) |
| Right | 18 (54.54%) | 18 (56.25%) |
| Left | 15 (45.45%) | 12 (37.50%) |
| WOMAC, mean (SD) | ||
| Pain (0–100) | 51.06 (20.45) | 50.94 (19.49) |
| Stiffness (0–100) | 36.18 (31.51) | 46.25 (32.65) |
| Physical Function (0–100) | 52.76 (20.58) | 55.34 (21.41) |
| MS, mean (SD) | ||
| Extension | 104.10 (27.59) | 106.90 (29.13) |
| Flexion | 51.34 (15.91) | 52.79 (19.61) |
| MP (W), mean (SD) | ||
| Extension | 59.92 (14.58) | 59.95 (15.87) |
| Flexion | 25.89 (10.11) | 30.34 (29.63) |
| MR, mean (SD) | ||
| Extension | 22.20 (16.21) | 24.08 (11.57) |
| Flexion | 21.49 (20.00) | 24.38 (20.22) |
BMI, body mass index; WOMAC, Western Ontario & McMaster Universities Osteoarthritis Index; MS, muscle strength; MP, muscle power; MR, muscle resistance.
Primary outcomes of pain and function
The analysis of covariance showed that participants from the treatment group had significantly less knee pain (adjusted mean difference = 11 points, 95% CI: 3–18) and higher levels of function (adjusted mean difference = 12 points, 95% CI: 5–18), after adjusting for baseline values, when compared to participants in the control group (Table 3).
Table 3.
Mean (SD) of each group, mean (SD) difference within each group, and mean (95% CI) difference between groups.
| Experimental (n = 33) |
Control (n = 32) |
Within-group differences |
Between-group differences | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| Initial | 6 weeks | Initial | 6 weeks | Exp | Control | |||
| Pain (0–100) | 51.1 (20.4) | 37.7 (16.5) | 50.9 (19.5) | 48.6 (22.1) | 13.33 (16.23) | 2.3 (15.1) | 10.9 (18 to 3) | 0.003 |
| Physical function (0–100) | 52.7 (20.6) | 36.3 (19.0) | 55.3 (21.4) | 50.2 (22.7) | 16.4 (17.5) | 5.1 (9.6) | 11.9 (18 to 5) | 0.001 |
Secondary outcomes of muscular performance
The analysis of covariance for the secondary outcomes of muscle strength, power, and resistance for knee muscle flexors and extensors showed that the improvements in all muscle parameters were greater for the hydrotherapy group. Statistical significance was reached for muscle strength of the knee flexors and extensors, for muscle power for the knee flexors, and for resistance for the knee extensors (Table 4).
Table 4.
Mean (SD) of each group, mean (SD) difference within group, and mean (95% CI) difference between groups.
| Experimental (n = 33) |
Control (n = 32) |
Within-group differences |
Between-group differences | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| Initial | 6 weeks | Initial | 6 weeks | Exp | Control | |||
| Strength (%), mean (SD) | ||||||||
| Extension | 104.1 (27.6) | 111.6 (23.1) | 106.9 (29.1) | 106.7 (34.3) | −7.47 (15.8) | 0.2 (14.1) | 7.3 (0.006–14) | 0.050 |
| Flexion | 51.3 (15.6) | 57.8 (15.2) | 54.2 (20.6) | 52.8 (19.6) | −6.5 (7.5) | −1.4 (11.4) | 4.9 (0.2–9) | 0.040 |
| Power (W), mean (SD) | ||||||||
| Extension | 59.9 (14.6) | 64.5 (14.4) | 59.9 (15.9) | 61.7 (15.4) | −4.5 (8.2) | −1.8 (6.2) | 2.7 (0.7–6) | 0.120 |
| Flexion | 25.6 (10.1) | 25.9 (9.6) | 30.3 (29.6) | 26.1 (11.3) | −4.4 (5.7) | 4.2 (27.3) | 5.0 (0.3–9) | 0.035 |
| Resistance (%), mean (SD) | ||||||||
| Extension | 22.2 (16.2) | 27.6 (9.1) | 24.1 (15.6) | 23.7 (13.4) | −5.4 (12.9) | 0.4 (9.7) | 4.8 (0.3–9) | 0.035 |
| Flexion | 21.5 (20.0) | 27.8 (14.8) | 24.4 (20.2) | 26.0 (28.5) | −6.3 (20.9) | −1.7 (24.0) | 3.2 (6–13) | 0.523 |
Discussion
The results of the present study demonstrated that a structured six-week hydrotherapy program in conjunction with an educational program led to greater improvements in pain and function in the short term when compared to an educational program alone in women suffering from knee OA. Furthermore, women with knee OA who received hydrotherapy showed greater improvements in knee muscle performance such as knee flexor and extensor strength, knee flexor power, and knee extensor resistance.
Hydrotherapy exercises are usually advocated in the treatment of knee OA because of the water properties, particularly those associated with buoyancy, which potentially reduces joint loading.26 Water pressure and temperature could also lead to an increased sensory input and further help in joint pain relief. The improvements in pain and function observed in our study with the implementation of hydrotherapy exercises are similar and consistent with the findings of previous clinical trials of hydrotherapy for patients with knee OA.13, 18, 27 However, our results are greater than those reported on a recent systematic review in comparison to a control group,15 even though previous randomized controlled trials have shown that hydrotherapy exercises are not superior to land-based exercises for pain relief in OA.14, 16, 28 Furthermore, our results showed slightly better improvements in terms of pain and function than those reported in a recent systematic review, which compared land-based exercise to control group for patients with knee OA.29 The control groups of the studies included in the review consisted mostly of no treatment groups, which is different from ours. Our control group received an educational protocol, which can be related to the slight improvements in pain and function in this group. This gives more support to our results and allows the conclusion that hydrotherapy can be as effective as other types of exercises. To our knowledge, no previous trial has investigated the effects of water-based exercises on pain, function, and muscle function in women suffering from knee OA alone. It is likely that women represent a special group of patients with OA because of higher incidence rates and disability reports in women compared to men.3, 4 Considering that water-based exercises usually result in greater levels of patient adherence6, 27 and fewer joint-related adverse effects, it is likely that they play a positive role in OA improving symptoms in women. Our study is the first step in trying to identify the efficacy of water-based exercises in this subgroup of patients.
It could be argued that the effect sizes observed in our study are small and perhaps not clinically worthwhile, particularly when the costs associated with the treatment setup of hydrotherapy are considered. However, the minimal clinically important rehabilitation effect for patients with lower limb OA for WOMAC function on a 0–10 scale ranges from 0.51 to 1.3330, 31 and reductions of 8.4–9.0 mm on a 0–100 visual analog scale for pain are considered clinically important,32, 33 which highlights the improvements in pain and function observed in the intervention group. Moreover, there are clinical advantages associated with hydrotherapy and factors that are likely to mediate its effectiveness. It is known that hydrotherapy does not worsen joint condition14 and leads to higher levels of treatment adherence6, 12, 13, 14, 15 compared to other forms of treatments, which could represent an important initial treatment option for rehabilitation programs for patients with severe symptoms of OA even if the effect sizes are not considered substantial.8 In addition to that, our results are slightly better than those reported in other types of exercise for knee OA and they are comparable to estimates on the effect of non-steroidal anti-inflammatory drugs.29
One of the innovative aspects of our study was the assessment of muscular performance with the implementation of hydrotherapy in women with OA. Similar to previous studies,34 we found significant increases in knee flexor (mean difference 4.9; 95% CI: 0.2–9) and extensor (mean difference = 7.3; 95% CI: 0.006–14) muscle strength in women receiving hydrotherapy compared to the education only group. The evidence is conflicting for quadriceps femoris strength in response to hydrotherapy, with some studies28, 34 reporting improvements in quadriceps femoris strength with aquatic exercises, while others13, 14, 20, 27, 35 do not. Moreover, we did observe differences between treatment groups for knee extensor muscle resistance (mean difference = 4.8; 95% CI: 0.3–9) and for knee flexor muscle power (mean difference = 5.0; 95% CI: 0.3–9) associated with hydrotherapy compared to the control group. These results are clinically important as stronger muscles act as shock absorbers and joint stabilizers, assisting in the preservation of the diseased joint.36
The current study has some limitations that should be considered, mainly the absence of a long-term follow up assessment and the inclusion of a sample of older women only. Arguably, it is likely that the intervention time of only six weeks might not have been sufficiently long to cause more significant changes. However, when we look at the results reported in studies with equal duration, we also find improvements in pain,6, 13, 16, 18 function,6, 13, 16, 28 and muscle strength.28 Furthermore, in a medium-term follow-up assessment, the improvements obtained within the six-week intervention were maintained,16 suggesting that the intervention can generate improvements which are maintained in the follow-up. When we consider the trials that included volunteers with knee OA only, patients reported slightly milder14, 20 or slightly harsher19 symptoms. The severity of the symptoms should be considered as a factor that might interfere in the results, which could be observed by the absence of improvements in the trial that included participants with the milder complaints.14
Future research should evaluate whether the effects of hydrotherapy observed in this trial remain over a longer period of time. The potential benefits of hydrotherapy over other forms of exercise should be considered in view of the treatment effects so that clinicians can consider a comprehensive patient-centered approach during the treatment decision-making process.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgements
We acknowledge the financial support of the Brazilian funding agencies Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
References
- 1.Felson D. Osteoarthritis of knee. N Engl J Med. 2006;354:841–848. doi: 10.1056/NEJMcp051726. [DOI] [PubMed] [Google Scholar]
- 2.Arden N., Nevitt M. Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol. 2006;20(1):3–25. doi: 10.1016/j.berh.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 3.O’Connor M. Sex differences in osteoarthritis of the hip and knee. J Am Acad Orthop Surg. 2007;15:522–525. [PubMed] [Google Scholar]
- 4.Sarikanth V., Fryer J., Zhai G., Winzenberg T., Hosmer D., Jones G. A metaanalysis of the sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage. 2005;13:769–781. doi: 10.1016/j.joca.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 5.Vannucci A. Osteoartrose. Rev Bras Med. 2002;20(1):36–43. [Google Scholar]
- 6.Silva L., Valim V., Pessanha A. Hydrotherapy versus conventional land-based exercise for the management of patients with osteoarthritis of the knee: a randomized clinical trial. Phys Ther. 2008;88:12–21. doi: 10.2522/ptj.20060040. [DOI] [PubMed] [Google Scholar]
- 7.O’Brien K.M., Williams A., Wiggers J. Effectiveness of a healthy lifestyle intervention for low back pain and osteoarthritis of the knee: protocol and statistical analysis plan for two randomised controlled trials. Braz J Phys Ther. 2016;20(September (5)):477–489. doi: 10.1590/bjpt-rbf.2014.0189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peter W., Jansen M., Hurkmans E. Physiotherapy in hip and knee osteoarthritis: development of a practice guideline concerning initial assessment, treatment and evaluation. Acta Reumatol Port. 2011;36:268–281. [PubMed] [Google Scholar]
- 9.Zhang W., Doherty M., Arden N. EULAR evidence based recommendations for the management of hip osteoarthritis: report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics. Ann Rheum Dis. 2005;64:669–681. doi: 10.1136/ard.2004.028886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Batterham S., Heywood S., Keating J. Systematic review and meta-analysis comparing land and aquatic exercise for people with hip or knee arthritis on function, mobility and other health outcomes. BMC Musculoskelet Dis. 2011;12:123–136. doi: 10.1186/1471-2474-12-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hochberg M., Altman R., April K. American college of rheumatology recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012;64:465–474. doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
- 12.Geytenbeek J. Evidence for effective hydrotherapy. Physiotherapy. 2002;88:514–529. [Google Scholar]
- 13.Hinman R., Heywood S., Day A. Aquatic physical therapy for hip and knee osteoarthritis: results of a single-blind randomized controlled trial. Phys Ther. 2007;87:32–43. doi: 10.2522/ptj.20060006. [DOI] [PubMed] [Google Scholar]
- 14.Lund H., Weile U., Christensen R. A randomized controlled trial of aquatic and land-based Exercise in patients with knee osteoarthritis. J Rehabil Med. 2008;40:137–144. doi: 10.2340/16501977-0134. [DOI] [PubMed] [Google Scholar]
- 15.Bartels E.M., Juhl C.B., Christensen R. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev. 2016;3:CD005523. doi: 10.1002/14651858.CD005523.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gill S., McBurney H., Schulz D. Land-based versus pool-based exercise for people awaiting joint replacement surgery of the hip or knee: results of a randomized controlled trial. Arch Phys Med Rehabil. 2009;90:388–394. doi: 10.1016/j.apmr.2008.09.561. [DOI] [PubMed] [Google Scholar]
- 17.Biscarini A., Cerulli G. Modeling of the knee joint load in rehabilitative knee extension exercises under water. J Biomech. 2006;17:1–11. doi: 10.1016/j.jbiomech.2005.12.018. [DOI] [PubMed] [Google Scholar]
- 18.Wyatt F., Milam S., Manske R., Deere R. The effects of aquatic and traditional exercise programs on persons with knee osteoarthritis. J Strength Cond Res. 2001;15:337–340. [PubMed] [Google Scholar]
- 19.Wang T., Lee S., Liang S., Tung H., Wu S., Lin Y. Comparing the efficacy of aquatic exercises and land-based exercises for patients with knee osteoarthritis. J Clin Nurs. 2011;20(17–18):2609–2622. doi: 10.1111/j.1365-2702.2010.03675.x. [DOI] [PubMed] [Google Scholar]
- 20.Lim J.Y., Tchai E., Jang S.N. Effectiveness of aquatic exercise for obese patients with knee osteoarthritis: a randomized controlled trial. PM R. 2010;2(August (8)):723–731. doi: 10.1016/j.pmrj.2010.04.004. quiz 793. [DOI] [PubMed] [Google Scholar]
- 21.Bertolucci P.H., Brucki S.M., Campacci S.R., Juliano Y. The Mini-Mental State Examination in a general population: impact of educational status. Arq Neuropsiquiatr. 1994;52(Mar (1)):1–7. [PubMed] [Google Scholar]
- 22.Kellgren J.H., Lawrence J.S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(December (4)):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cochrane T., Davey R., Matthes Edwards S.M. Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis. Health Technol Assess. 2005;9(31):1–114. doi: 10.3310/hta9310. iii–xi, ix–xi. [DOI] [PubMed] [Google Scholar]
- 24.Patrick D., Ramsey S., Spencer A., Kinne S., Belza B., Topolski T. Economic evaluation of aquatic exercise for persons with osteoarthritis. Med Care. 2001;39:413–424. doi: 10.1097/00005650-200105000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Fernandes M.I. Universidade Federal de São Paulo; São Paulo: 2003. Tradução e validação do questionário de qualidade de vida específico para osteoartrose WOMAC (Western Ontario McMaster Universities) para a língua portuguesa. 103p. [Google Scholar]
- 26.Kidd B. Osteoarthritis and joint pain. Pain. 2006;123:6–9. doi: 10.1016/j.pain.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 27.Lin S., Davey R., Cochrane T. Community rehabilitation for older adults with osteoarthritis of the lower limb: a controlled clinical trial. Clin Rehabil. 2004;18:92–101. doi: 10.1191/0269215504cr706oa. [DOI] [PubMed] [Google Scholar]
- 28.Foley A., Halbert J., Hewitt T., Crotty M. Does hydrotherapy improve strength and physical function in patients with osteoarthritis – a randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Ann Rheum Dis. 2003;62:1162–1167. doi: 10.1136/ard.2002.005272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fransen M., McConnell S., Harmer A.R., Van der Esch M., Simic M., Bennell K.L. Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med. 2015;49(December (24)):1554–1557. doi: 10.1136/bjsports-2015-095424. [DOI] [PubMed] [Google Scholar]
- 30.Angst F., Aeschlimann A., Michel B.A., Stucki G. Minimal clinically important rehabilitation effects in patients with osteoarthritis of the lower extremities. J Rheumatol. 2002;29(1):131–138. [PubMed] [Google Scholar]
- 31.Angst F., Aeschlimann A., Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45(August (4)):384–391. doi: 10.1002/1529-0131(200108)45:4<384::AID-ART352>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 32.Eberle E., Ottillinger B. Clinically relevant change and clinically relevant difference in knee osteoarthritis. Osteoarthritis Cartilage. 1999;7(September (5)):502–503. doi: 10.1053/joca.1999.0246. [DOI] [PubMed] [Google Scholar]
- 33.Wandel S., Juni P., Tendal B. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ. 2010;341(September):c4675. doi: 10.1136/bmj.c4675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang T., Belza B., Elaine Thompson F., Whitney J., Bennett K. Effects of aquatic exercise on flexibility, strength and aerobic fitness in adults with osteoarthritis of the hip or knee. J Adv Nurs. 2006;57:141–152. doi: 10.1111/j.1365-2648.2006.04102.x. [DOI] [PubMed] [Google Scholar]
- 35.Fisher N., Dolan D., Brenner C., Pendergast D. Quantitative effects of water exercise program on the functional and physiological capacity in subjects with knee osteoarthritis: a pilot study. Sport Sci Health. 2004;1:17–24. [Google Scholar]
- 36.Hurley M.V. The role of muscle weakness in the pathogenesis of osteoarthritis. Rheum Dis Clin North Am. 1999;25(May (2)):283–298. doi: 10.1016/s0889-857x(05)70068-5. vi. [DOI] [PubMed] [Google Scholar]