Abstract
Innovative tools are needed to alleviate the burden of mosquito-borne diseases, and strategies that target the pathogen are being considered. A possible tactic is the use of Wolbachia, a maternally inherited, endosymbiotic bacterium that can (but does not always) suppress diverse pathogens when introduced to naive mosquito species. We investigated effects of somatic Wolbachia (strain wAlbB) infection on Rift Valley fever virus (RVFV) in Culex tarsalis mosquitoes. When compared to Wolbachia-uninfected mosquitoes, there was no significant effect of Wolbachia infection on RVFV infection, dissemination, or transmission frequencies, nor on viral body or saliva titers. Within Wolbachia-infected mosquitoes, there was a modest negative correlation between RVFV body titers and Wolbachia density, suggesting that Wolbachia may slightly suppress RVFV in a density-dependent manner in this mosquito species. These results are contrary to previous work in the same mosquito species, showing Wolbachia-induced enhancement of West Nile virus infection rates. Taken together, these results highlight the importance of exploring the breadth of pathogen modulations induced by Wolbachia.
Author summary
An integrated vector management program utilizes several practices, including pesticide application and source reduction, to reduce mosquito populations. However, mosquitoes are developing resistance to some of these methods and new control approaches are needed. A novel technique involves the bacterium Wolbachia that lives naturally in many insects. Wolbachia can be transferred to uninfected mosquitoes and can block pathogen transmission to humans, although in some circumstances pathogen enhancement has been observed. Additionally, Wolbachia is maternally inherited, allowing it to spread quickly through uninfected field populations of mosquitoes. We studied the impacts of Wolbachia on Rift Valley fever virus (RVFV) in the naturally uninfected mosquito, Culex tarsalis. Wolbachia had no effect on the frequencies at which Culex tarsalis became infected with or transmitted RVFV. However, when we analyzed the relationship between Wolbachia densities and RVFV titers, we determined that high densities of Wolbachia were associated with no virus infection or low levels of virus, suggesting that Wolbachia might suppress RVFV at high densities. These results contrast with our previous study that showed Wolbachia enhances West Nile virus infection in Culex tarsalis. Together, these studies highlight the importance of studying Wolbachia effects on a variety of pathogens so that control methods that use Wolbachia are not impeded by unintended or off-target effects.
Introduction
Globally, mosquito-borne diseases are a major health burden. To decrease mosquito populations, control programs often use integrated vector management practices including adulticide and larvicide application, source reduction, and biological control [1]. However, these mosquito control methods are losing efficacy due to increasing insecticide resistance and changes in mosquito behavior [2–4]. With these concerns, novel and sustainable control methods are under investigation, including strategies that target the pathogen [5,6]. Wolbachia is a maternally-inherited endosymbiotic bacterium that infects a large number of insects and other invertebrates [7]. Infection by Wolbachia can cause broad effects on host physiology. For example, natural Wolbachia infections in fruit flies protect against pathogen-induced mortality [8,9]. When experimentally transferred to uninfected mosquitoes, Wolbachia can suppress infection or transmission of viruses, Plasmodium parasites, and filarial nematodes [10–13]. Wolbachia also manipulates host reproduction in ways that allow it to spread through and persist in insect populations [14].
Investigations using Wolbachia-infected mosquitoes as a control method for dengue virus are underway [15], and field trials in Australia have indicated that Wolbachia can spread to near-fixation in naturally uninfected populations of Aedes aegypti mosquitoes [16,17]. These Wolbachia-infected Ae. aegypti populations can persist years after release, and mosquitoes retain the dengue virus-blocking phenotype [18]. Similar field experiments are being conducted in several other countries, but not all have reported successful replacement of the uninfected population with Wolbachia-infected mosquitoes [19].
The effects of Wolbachia-induced pathogen interference may differ depending on mosquito species, Wolbachia strain, pathogen type, and environment conditions [20–22]. For example, in Anopheles gambiae, transient somatic infection of the Wolbachia strain wAlbB inhibits Plasmodium falciparum but enhances Plasmodium berghei parasites [22,23]. Enhancement phenotypes have been observed in Anopheles, Culex, and Aedes mosquitoes, and across several malaria species and virus families [20,22,24–27]. Thus, it is important to examine the range of Wolbachia-induced phenotypes so that efficacy of disease control efforts using Wolbachia-induced pathogen interference are not impeded.
Previous work has demonstrated that somatic Wolbachia (strain wAlbB) infections in Culex tarsalis (Yolo strain) enhanced West Nile virus (WNV) infection rates [24]. To better understand the range of Wolbachia-induced phenotypes, we investigated the effects of wAlbB on Rift Valley fever virus (RVFV) infection in Cx. tarsalis. RVFV is a member of the genus Phlebovirus in the family Bunyaviridae and predominately affects domestic ruminants, causing severe economic losses in the livestock industry and human morbidity in Africa and the Middle East [28–30]. Additionally, models and laboratory studies have suggested the United States may have environmental conditions and mosquito vectors that would permit RVFV introduction and invasion [31–34]. Cx. tarsalis are abundant in the western U.S. and are highly competent laboratory vectors for RVFV [33–35]. We assessed the ability of Wolbachia to affect RVFV infection, dissemination, and transmission within Cx. tarsalis at two time points and evaluated relationships between viral titer and Wolbachia density in mosquitoes.
Materials and methods
Ethics statement
Mosquitoes were maintained on commercially obtained anonymous human blood using a membrane feeder (Biological Specialty Corporation, Colmar, PA). RVFV experiments were performed under biosafety-level 3 (BSL-3) and arthropod-containment level 3 (ACL3) conditions.
Research at the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) was conducted under an Institutional Animal Care and Use Committee (IACUC) approved protocol in compliance with the Animal Welfare Act, PHS Policy, and other federal statutes and regulations relating to animals and experiments involving animals. The facility where this research was conducted is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care, International and adheres to the principles stated in the Guide for the Care and Use of Laboratory Animals, National Research Council, 2011. The USAMRIID IACUC specifically approved this study.
Mosquitoes and Wolbachia
The Culex tarsalis colony used for all experiments was derived from field mosquitoes collected in Yolo County, CA in 2009. Mosquitoes were reared and maintained at 27°C ± 1°C, 12:12 hr light:dark diurnal cycle at 80% relative humidity in 30×30×30 cm cages. The wAlbB Wolbachia strain was purified from An. gambiae Sua5B cells according to published protocols [36]. Wolbachia viability and density was assessed using the LIVE/DEAD BacLight Bacterial Viability Kit (Invitrogen, Carlsbad, CA) and a hemocytometer. The RVFV vector competence experiment was replicated three times with different hamsters, and wAlbB concentrations for those replicates as follows: replicate one, 2.5 × 109 bacteria/ml; replicate two, 2.5 × 109 bacteria/ml; replicate three, 5.0 × 109 bacteria/ml.
Two- to 4-day-old adult female Cx. tarsalis were anesthetized with CO2 and intrathoracically injected with approximately 0.1 μl of either suspended wAlbB or Schneider’s insect media (Sigma Aldrich, Saint Louis, MO) as a control. Mosquitoes were provided with 10% sucrose ad libitum and maintained at 27°C in a growth chamber.
Vector competence for RVFV
RVFV strain ZH501 was isolated from the blood of a fatal human case in Egypt in 1977 [37]. Adult female Syrian hamsters were inoculated intraperitoneally with 0.2 ml of a suspension containing RVFV in diluent (10% heat-inactivated fetal bovine serum in Medium 199 with Earle’s salts [Invitrogen], sodium bicarbonate, and antibiotics) containing approximately 105 plaque-forming units (PFU) per ml of RVFV. Approximately 28–30 hr post-inoculation, infected hamsters were anesthetized with a suspension of ketamine, acepromazine, and xylazine. A single viremic hamster was placed across two 3.8-liter cardboard cages containing either Wolbachia-infected Cx. tarsalis or control-injected Cx. tarsalis, treatments to which the experimenter was blinded. Mosquitoes were allowed to feed for one hour. After this period, hamsters were removed, a blood sample taken to determine viremia, and hamsters were euthanized.
After feeding, mosquitoes were anesthetized with CO2 and examined for feeding status; partially or non-blood fed females were discarded. For all replicates, one blood fed mosquito from each treatment was sampled to test for input viral titers. Mosquitoes were sampled at 7 and 14 days post-blood feeding. On day 7, mosquitoes were anesthetized with CO2 and had their legs removed; each set of legs was placed into one 2-ml microcentrifuge tube containing 1 ml of mosquito diluent (20% heat-inactivated fetal bovine serum [FBS] in Dulbecco’s phosphate-buffered saline, 50 μg/ml penicillin streptomycin, and 2.5 μg/ml fungizone). Bodies were placed separately into 2-ml microcentrifuge tubes (Eppendorf, Hauppauge, NY) containing 1 ml of mosquito diluent. On day 14, bodies and legs were collected in the same manner as day 7, except that prior to placing bodies into microcentrifuge tubes, saliva was collected from mosquitoes by positioning the proboscis of each mosquito into a capillary tube containing approximately 10 μl of a 1:1 solution of 50% sucrose and FBS. After 30 minutes, the contents were expelled in individual microcentrifuge tubes containing 0.3 ml of mosquito diluent. A 5 mm stainless steel bead (Qiagen, Valencia, CA) was placed into all microcentrifuge tubes that contained mosquito bodies and legs, homogenized in a mixer mill (Retsch, Haan, Germany) for 30 seconds at 24 cycles per second, and centrifuged for 1 minute at 8000 rpm. All mosquito bodies, legs, and saliva were stored at -80°C until assayed.
Samples were tested for RVFV infectious particles by plaque assay on Vero cells according to previous published protocols [38]. Serial dilutions were prepared for all mosquito body, leg, and saliva samples. One hundred microliters of each dilution was inoculated onto Vero cell culture monolayers. Inoculated plates were incubated at 37°C for 1 hr and an agar overlay was added (1X EBME, 0.75% agarose, 7% FBS, 1% penicillin streptomycin, and 1% nystatin). Plates were incubated at 37°C for 3 days and then a second overlay (1X EBME, 0.75% agarose, and 4% neutral red) was added. Plaques were counted 24 hr after application of the second overlay and titers calculated.
Quantitative real-time PCR of Wolbachia density
To evaluate relationships between Wolbachia density and RVFV titer, we measured wAlbB levels in individual mosquitoes. DNA was extracted from 200 μl of mosquito body homogenate using the DNeasy blood and tissue kit (Qiagen) and used as template for qPCR on a Rotor-Gene Q (Qiagen) with the PerfeCta SYBR FastMix kit (Quanta Biosciences, Beverly, MA) or on ABI 7500 with Power SYBR green master mix (Applied Biosystems, Foster City, CA). The qPCR assays were performed in 10μl reactions and amplification was carried out using a standardized program at 95°C for 5 min, 40 cycles of 95°C for 10 sec, 60°C for 15 sec, and 72°C for 10 sec. Wolbachia DNA was amplified with primers Alb-GF and Alb-GR [39] and was normalized to the Cx. tarsalis actin gene by using qGene software [24,40]. qPCRs were performed in duplicate.
Statistical analyses
Infection, dissemination, and transmission rates were compared between Wolbachia-infected and control Cx. tarsalis, and between replicates with Fisher’s exact tests. Due to violations of assumptions needed for parametric tests, Mann-Whitney U was used to compare the following data sets: RVFV body titers between Wolbachia-infected and control mosquitoes, RVFV body titers between RVFV-positive saliva and RVFV-negative saliva, RVFV body titers over time, and Wolbachia density over time. Unpaired t-tests were used to analyze data that passed normality tests, including the comparison of RVFV saliva titers between Wolbachia-infected and control mosquitoes. To determine relationships between Wolbachia density and RVFV body titer, the Spearman rank correlation test was used, as assumptions for Pearson correlation were violated. All statistical analyses were performed in GraphPad Prism version 7 for Windows (GraphPad Software, San Diego, CA).
Results
Vector competence for RVFV
After all hamster feeds (i.e., replicates), one blood fed mosquito from each treatment was tested for input RVFV titers on the day of blood feeding. These day 0 RVFV titer results for Wolbachia-infected Cx. tarsalis were as follows: replicate 1, 2.50 × 102 PFU/ml; replicate 2, 7.00 × 106 PFU/ml; replicate 3, 1.00 × 102 PFU/ml. Day 0 results for control Cx. tarsalis were as follows: replicate 1, 5.00 × 102 PFU/ml; replicate 2, 1.05 × 107 PFU/ml; replicate 3, 1.00 ×102 PFU/ml. Viremias in the three hamsters were 104, 109, and 103 PFU/ml, respectively.
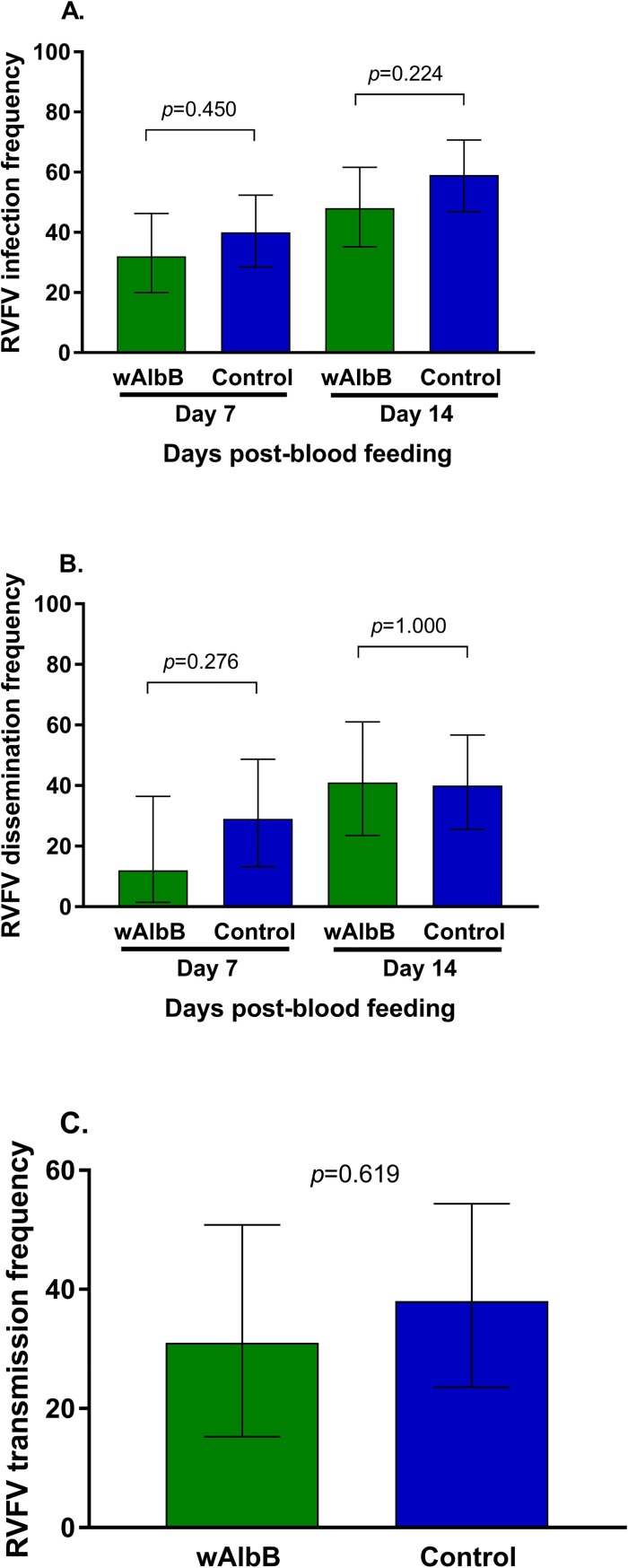
To determine RVFV vector competence of Wolbachia-infected and Wolbachia-uninfected Cx. tarsalis, we examined frequencies of RVFV-positive bodies (Fig 1A), legs (Fig 1B), and saliva (Fig 1C). Infection rate is the proportion of mosquito bodies that contained infectious RVFV. Dissemination and transmission rates are the proportion of infected mosquitoes with RVFV positive legs and saliva, respectively. Three replicate experiments were performed, and individual data from those experiments are available in S1 Table. Hamster viremia in replicate three was low and resulted in low mosquito infection rates. Replicate two infection frequencies were significantly higher than replicate one for both treatments and at both day 7 and day 14 (P < 0.0001) (S1 Table). However, Fig 1 and S1 Table show that across replicates and time points, Wolbachia-infected Cx. tarsalis infection, dissemination, and transmission rates did not differ significantly from Wolbachia-uninfected Cx. tarsalis. Thus, the data were pooled for further analysis.
Fig 1. Effects of Wolbachia infection on RVFV vector competence frequencies in Cx. tarsalis.
RVFV infection 7 and 14 days post-feeding (A), dissemination 7 and 14 days post-feeding (B), and transmission rates 14 days post-feeding (C) were compared between Wolbachia-infected and control Cx. tarsalis. Bars represent data pooled from three replicates. Error bars denote binomial confidence intervals. See S1 Table for replicate-specific analyses.
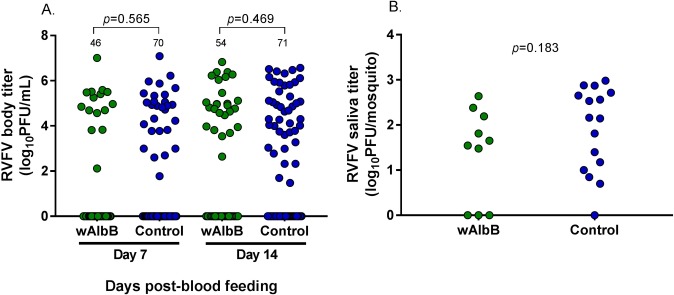
RVFV body (Fig 2A) and saliva titers (Fig 2B) were determined for Wolbachia-infected and control Cx. tarsalis. There were no significant differences in RVFV body titer or saliva titer between Wolbachia-infected and control Cx. tarsalis at either day 7 (Fig 2A) or day 14 (Fig 2B). Additionally, when replicate data were pooled, both Wolbachia-infected and uninfected Cx. tarsalis that had higher RVFV body titers were more likely to have RVFV-positive saliva (S1 Fig).
Fig 2. Comparison of RVFV body and saliva titers between Wolbachia-infected and control Cx. tarsalis.
At both 7 and 14 days post-blood meal, there were no significant differences in RVFV body titers (A) or saliva titers (B) of Wolbachia-infected Cx. tarsalis compared to control Cx. tarsalis. All replicates are combined in this figure; separate replicates are provided in supplementary materials (S2 Fig). Bars represent medians and bolded numbers above the data points denote sample sizes.
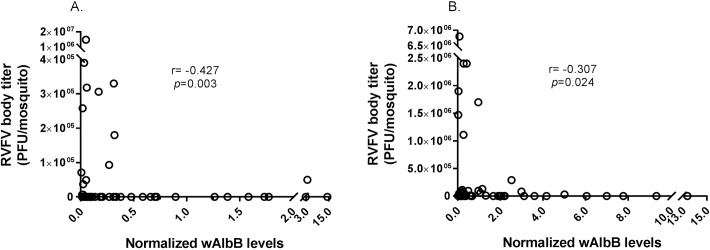
Quantitative real-time PCR of Wolbachia (wAlbB) density
We performed qPCR from the DNA of each mosquito and determined Wolbachia density as an expression normalized to a reference gene, actin [40]. We used all samples that were positive for Wolbachia to analyze relationships between Wolbachia density and RVFV body titer; we combined data from all replicate experiments (Fig 3). Overall, there was a moderate, negative correlation between Wolbachia density and RVFV body titer at both day 7 and 14 (Fig 3A and 3B). Replicate two, the replicate with the highest infection rates, did not have significant correlations between Wolbachia density and RVFV body titer at either day 7 (n = 14, r = 0.0516, p = 0.062) or day 14 (n = 27, r = 0.112, p = 0.577) (raw data available S2 Table). Wolbachia density was also compared across time; Wolbachia concentration at day 14 was significantly higher than at day 7, consistent with Wolbachia replication in mosquitoes (S3 Fig).
Fig 3. Correlation between RVFV body titer and Wolbachia levels in Cx. tarsalis.
Wolbachia levels were normalized to the host gene actin. Normalized Wolbachia levels and RVFV body titer for each mosquito were plotted and analyzed with the Spearman rank correlation test to determine relationships. There was a moderate, negative correlation between RVFV body titer and Wolbachia levels at both day 7 (n = 46) (A) and day 14 (n = 54) (B) post-blood feeding (Fig 3). Data for all replicates were combined; see S2 Table for replicate-specific raw data.
Discussion
Wolbachia infection can have varied effects on viruses and parasites transmitted by mosquitoes. These effects can include moderate to complete pathogen inhibition, as well as pathogen enhancement [17,22,24,41,42]. In a previous study, we found that Wolbachia strain wAlbB enhanced WNV infection frequency in Cx. tarsalis [24], although in that study, viral infection titers were not measured. To understand how widespread the Wolbachia-induced enhancement phenotype is in Cx. tarsalis, we studied wAlbB effects on RVFV, an important arthropod-borne virus with potential to invade the United States [43,44]. In contrast to our previous results, we found that wAlbB did not affect RVFV body or saliva titers, nor RVFV infection, dissemination, or transmission frequencies in Cx. tarsalis.
Wolbachia-mediated effects on pathogens may depend on Wolbachia density. Several studies have reported that high densities of Wolbachia are more likely than low densities to block viruses in Drosophila spp. and mosquitoes [45–48]. Similarly, we found a moderate, negative correlation between RVFV body titer and Wolbachia density. High Wolbachia levels were associated with RVFV negative mosquitoes or those with low RVFV body titers. The low numbers of mosquitoes at the high Wolbachia densities may explain why we did not see a Wolbachia effect on population level vector competence measures. However, our correlation data suggests that in this system, Wolbachia may suppress RVFV in a density-dependent manner.
In this Cx. tarsalis-wAlbB system, we have reported different effects of Wolbachia on vector competence for WNV and RVFV [24]. Other studies have found similar differences in Wolbachia phenotypes and suggested they may depend on various factors including environmental conditions, and pathogen type [20,49]. RVFV and WNV belong to different virus families and could interact with the mosquito host environment and Wolbachia in different ways. For example, a recent study suggested that the mosquito JAK/STAT pathway may not have the same antiviral effects on closely related viruses [50]. Although the mosquitoes in our two studies have the same genetic background, they were reared in separate facilities and may have different microbiomes that may explain differences in vector competence [51].
While artificial feeding methods such as membrane feeders or pledgets allow one to easily standardize viral titers, previous studies on mosquito RVFV and other virus infections demonstrated significantly reduced mosquito infectivity using an artificial feeding system compared to a live infected animal [52, 53]. We therefore decided to use live hamsters infected with a highly virulent and epidemiologically relevant viral strain in our experiments. However, this more biologically relevant choice comes with a trade-off; it is impossible to standardize the viral titer in a live animal infection model. While all hamsters were infected with approximately the same amount of virus, they varied in their response to the infection, resulting in significant variation in final viral blood titers across experimental replicates that reduced statistical power.
Our study was performed with an adult microinjection model that generates mosquitoes transiently infected with Wolbachia. It remains to be seen whether this model reflects relationships between Wolbachia and viruses in Cx. tarsalis in a stable infection system. However, a recent study showed that both stable and transient wAlbB infections in Ae. aegypti produced similar results [45]. This suggests that our transient infection model may correlate with a stable infection in Cx. tarsalis.
Despite relatively modest measurable effects in these experiments, our results underscore the necessity of studying diverse Wolbachia-host-pathogen systems. It is becoming increasingly clear that one cannot extrapolate results of one system of interactions across all systems; every Wolbachia-host-pathogen system must be individually examined. Future studies should seek to understand the mechanisms underlying variation of Wolbachia protective effects across diverse mosquito species, viral/pathogen species, and Wolbachia strains.
Supporting information
RVFV infection, dissemination, and transmission frequencies were compared between Wolbachia-infected and control mosquitoes. Replicates are displayed individually.
(XLSX)
(XLSX)
RVFV body titers were compared between mosquitoes that tested positive or negative for RVFV in their saliva. For both Wolbachia-infected and control Cx. tarsalis, mosquitoes positive for RVFV in the saliva had significantly higher RVFV body titers compared to mosquitoes negative for virus in the saliva There was no significant difference in RVFV body titer of transmitters between Wolbachia-infected and control mosquitoes (p = 0.7692). Data from three replicates were pooled and analyzed with Mann-Whitney U, and the bars represent medians.
(TIF)
RVFV body titers were compared between Wolbachia-infected and control mosquitoes for replicates 1 (A), 2 (B), and 3 (C). In all replicates, there were no significant differences in RVFV body titer between Wolbachia-infected and control mosquitoes. Data did not pass assumptions for normality and were analyzed with Mann-Whitney U, and sample sizes are denoted above data points.
(TIF)
Wolbachia levels for each mosquito, determined by qPCR, were combined across all three replicates. Wolbachia levels were significantly higher at day 14 compared to day 7. Due to violations of normality, Mann-Whitney U was used for comparisons, bars are medians, and numbers above data points are sample sizes.
(TIF)
Acknowledgments
We thank the Cell Culture and Diagnostics Systems Divisions at the United States Army Medical Research Institute of Infectious Diseases (USAMRIID) for providing experimental materials and equipment. We also thank J. Hinson (USAMRIID) for providing technical assistance. The views of the authors ESA and MJT do not necessarily reflect the position of the Department of Defense or the Department of the Army.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was funded by NIH grants R01AI116636 and R21AI128918 to JLR. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Best Management Practices for Integrated Mosquito Management. In: American Mosquito Control Association [Internet]. 2009. Available: http://www.mosquito.org/assets/Resources/PRTools/Resources/bmpsformosquitomanagement.pdf
- 2.Moiroux N, Gomez MB, Pennetier C, Elanga E, Djènontin A, Chandre F, et al. Changes in Anopheles funestus biting behavior following universal coverage of long-lasting insecticidal nets in Benin. J Infect Dis. 2012;206: 1622–1629. doi: 10.1093/infdis/jis565 [DOI] [PubMed] [Google Scholar]
- 3.Syed Z, Leal WS. Mosquitoes smell and avoid the insect repellent DEET. Proc Natl Acad Sci. 2008;105: 13598–13603. doi: 10.1073/pnas.0805312105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ranson H, Lissenden N. Insecticide resistance in African Anopheles mosquitoes: A worsening situation that needs urgent action to maintain malaria control. Trends Parasitol. Elsevier Ltd; 2016;32: 187–196. doi: 10.1016/j.pt.2015.11.010 [DOI] [PubMed] [Google Scholar]
- 5.Read AF, Lynch PA, Thomas MB. How to make evolution-proof insecticides for malaria control. PLoS Biol. 2009;7: e1000058 doi: 10.1371/journal.pbio.1000058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ricci I, Damiani C, Rossi P, Capone A, Scuppa P, Cappelli A, et al. Mosquito symbioses: from basic research to the paratransgenic control of mosquito-borne diseases. J Appl Entomol. 2011;135: 487–493. doi: 10.1111/j.1439-0418.2011.01613.x [Google Scholar]
- 7.Hilgenboecker K, Hammerstein P, Schlattmann P, Telschow A, Werren JH. How many species are infected with Wolbachia?-A statistical analysis of current data. FEMS Microbiol Lett. 2008;281: 215–220. doi: 10.1111/j.1574-6968.2008.01110.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teixeira L, Ferreira A, Ashburner M. The bacterial symbiont Wolbachia induces resistance to RNA viral infections in Drosophila melanogaster. PLoS Biol. 2008;6: e1000002 doi: 10.1371/journal.pbio.1000002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hedges LM, Brownlie JC, O’Neill SL, Johnson KN. Wolbachia and virus protection in insects. Science. 2008;322: 702 doi: 10.1126/science.1162418 [DOI] [PubMed] [Google Scholar]
- 10.Kambris Z, Cook PE, Phuc HK, Sinkins SP. Immune activation by life-shortening Wolbachia and reduced filarial competence in mosquitoes. Science. 2009;326: 134–136. doi: 10.1126/science.1177531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moreira LA, Iturbe-Ormaetxe I, Jeffery JA, Lu G, Pyke AT, Hedges LM, et al. A Wolbachia symbiont in Aedes aegypti limits infection with dengue, Chikungunya, and Plasmodium. Cell. 2009;139: 1268–1278. doi: 10.1016/j.cell.2009.11.042 [DOI] [PubMed] [Google Scholar]
- 12.Kambris Z, Blagborough AM, Pinto SB, Blagrove MSC, Godfray HCJ, Sinden RE, et al. Wolbachia stimulates immune gene expression and inhibits Plasmodium development in Anopheles gambiae. PLoS Pathog. 2010;6: e1001143 doi: 10.1371/journal.ppat.1001143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andrews ES, Crain PR, Fu Y, Howe DK, Dobson SL. Reactive oxygen species production and Brugia pahangi survivorship in Aedes polynesiensis with artificial Wolbachia infection types. PLoS Pathog. 2012;8 doi: 10.1371/journal.ppat.1003075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Werren JH, Baldo L, Clark ME. Wolbachia: master manipulators of invertebrate biology. Nat Rev Microbiol. 2008;6: 741–751. doi: 10.1038/nrmicro1969 [DOI] [PubMed] [Google Scholar]
- 15.Bourtzis K, Dobson SL, Xi Z, Rasgon JL, Calvitti M, Moreira L a, et al. Harnessing mosquito-Wolbachia symbiosis for vector and disease control. Acta Trop. Elsevier B.V.; 2014;132S: S150–S163. doi: 10.1016/j.actatropica.2013.11.004 [DOI] [PubMed] [Google Scholar]
- 16.Hoffmann AA, Montgomery BL, Popovici J, Iturbe-Ormaetxe I, Johnson PH, Muzzi F, et al. Successful establishment of Wolbachia in Aedes populations to suppress dengue transmission. Nature. Nature Publishing Group; 2011;476: 454–457. doi: 10.1038/nature10356 [DOI] [PubMed] [Google Scholar]
- 17.Walker T, Johnson PH, Moreira LA, Iturbe-Ormaetxe I, Frentiu FD, McMeniman CJ, et al. The wMel Wolbachia strain blocks dengue and invades caged Aedes aegypti populations. Nature. Nature Publishing Group; 2011;476: 450–453. doi: 10.1038/nature10355 [DOI] [PubMed] [Google Scholar]
- 18.Frentiu FD, Zakir T, Walker T, Popovici J, Pyke AT, van den Hurk A, et al. Limited dengue virus replication in field-collected Aedes aegypti mosquitoes infected with Wolbachia. PLoS Negl Trop Dis. 2014;8: e2688 doi: 10.1371/journal.pntd.0002688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen TH, Nguyen H Le, Nguyen TY, Vu SN, Tran ND, Le TN, et al. Field evaluation of the establishment potential of wmelpop Wolbachia in Australia and Vietnam for dengue control. Parasit Vectors. 2015;8: 563 doi: 10.1186/s13071-015-1174-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murdock CC, Blanford S, Hughes GL, Rasgon JL, Thomas MB. Temperature alters Plasmodium blocking by Wolbachia. Sci Rep. 2014;4: 3932 doi: 10.1038/srep03932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van den Hurk AF, Hall-Mendelin S, Pyke AT, Frentiu FD, McElroy K, Day A, et al. Impact of Wolbachia on infection with chikungunya and yellow fever viruses in the mosquito vector Aedes aegypti. PLoS Negl Trop Dis. 2012;6: e1892 doi: 10.1371/journal.pntd.0001892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hughes GL, Vega-Rodriguez J, Xue P, Rasgon JL. Wolbachia strain wAlbB enhances infection by the rodent malaria parasite Plasmodium berghei in Anopheles gambiae mosquitoes. Appl Environ Microbiol. 2012;78: 1491–1495. doi: 10.1128/AEM.06751-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hughes GL, Koga R, Xue P, Fukatsu T, Rasgon JL. Wolbachia infections are virulent and inhibit the human malaria parasite Plasmodium falciparum in Anopheles gambiae. PLoS Pathog. 2011;7: e1002043 doi: 10.1371/journal.ppat.1002043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dodson BL, Hughes GL, Paul O, Matacchiero AC, Kramer LD, Rasgon JL. Wolbachia enhances West Nile virus (WNV) infection in the mosquito Culex tarsalis. Kittayapong P, editor. PLoS Negl Trop Dis. 2014;8: e2965 doi: 10.1371/journal.pntd.0002965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baton LA, Pacidônio EC, Gonçalves DDS, Moreira LA. wFlu: Characterization and evaluation of a native Wolbachia from the mosquito Aedes fluviatilis as a potential vector control agent. PLoS One. 2013;8: e59619 doi: 10.1371/journal.pone.0059619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zélé F, Nicot A, Berthomieu A, Weill M, Duron O, Rivero A, et al. Wolbachia increases susceptibility to Plasmodium infection in a natural system. Proc R Soc. 2014;281 doi: 10.1098/rspb.2013.2837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Graham RI, Grzywacz D, Mushobozi WL, Wilson K. Wolbachia in a major African crop pest increases susceptibility to viral disease rather than protects. Ecol Lett. 2012;15: 993–1000. doi: 10.1111/j.1461-0248.2012.01820.x [DOI] [PubMed] [Google Scholar]
- 28.Bird BH, Ksiazek TG, Nichol ST, MacLachlan J. Zoonosis Update Rift Valley fever virus. Vet Med Today. 2009; 883–893. [DOI] [PubMed] [Google Scholar]
- 29.Wilson M. Rift Valley fever virus ecology and the epidemiology of disease emergence. Ann New York Acad Sci. 1994;15: 169–180. [DOI] [PubMed] [Google Scholar]
- 30.Jupp PG, Kemp A, Grobbelaar A, Lema P, Burt FJ, Alahmed AM, et al. The 2000 epidemic of Rift Valley fever in Saudi Arabia: mosquito vector studies. Med Vet Entomol. 2002;16: 245–252. [DOI] [PubMed] [Google Scholar]
- 31.Konrad SK, Miller SN. A temperature-limited assessment of the risk of Rift Valley fever transmission and establishment in the continental United States of America. Geospat Health. 2012;6: 161–170. doi: 10.4081/gh.2012.134 [DOI] [PubMed] [Google Scholar]
- 32.Pfeffer M, Dobler G. Emergence of zoonotic arboviruses by animal trade and migration. Parasit Vectors. 2010;3: 35 doi: 10.1186/1756-3305-3-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Turell MJ, Wilson WC, Bennett KE. Potential for North American mosquitoes (Diptera: Culicidae) to transmit Rift Valley fever virus. J Med Entomol. 2010;47: 884–889. doi: 10.1603/ME10007 [DOI] [PubMed] [Google Scholar]
- 34.Gargan TP, Clark GG, Dohm DJ, Turell MJ, Bailey CL. Vector potential of selected North American mosquito species for Rift Valley fever virus. Am J Trop Med Hyg. 1988;38: 440–446. Available: http://www.ncbi.nlm.nih.gov/pubmed/2895591 [DOI] [PubMed] [Google Scholar]
- 35.Bohart RM and Washino R. Mosquitoes of California. 3rd ed. Berkeley: University of California Division of Agricultural Sciences; 1978. [Google Scholar]
- 36.Rasgon JL, Gamston CE, Ren X. Survival of Wolbachia pipientis in cell-free medium. Appl Environ Microbiol. 2006;72: 6934–6937. doi: 10.1128/AEM.01673-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meegan JM. The Rift Valley fever epizootic in Egypt 1977–78. Trans R Soc Trop Med Hyg. 1979;73: 618–623. [DOI] [PubMed] [Google Scholar]
- 38.Blow JA, Dohm DJ, Negley DL, Mores CN. Virus inactivation by nucleic acid extraction reagents. J Virol Methods. 2004;119: 195–198. doi: 10.1016/j.jviromet.2004.03.015 [DOI] [PubMed] [Google Scholar]
- 39.Ruang-areerate T, Kittayapong P. Wolbachia transinfection in Aedes aegypti: A potential gene driver of dengue vectors. Proc Natl Acad Sci. 2006;103: 6–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simon P. Q-Gene: processing quantitative real-time RT-PCR data. Bioinformatics. 2003;19: 1439–1440. doi: 10.1093/bioinformatics/btg157 [DOI] [PubMed] [Google Scholar]
- 41.Glaser RL, Meola MA. The native Wolbachia endosymbionts of Drosophila melanogaster and Culex quinquefasciatus increase host resistance to West Nile virus infection. PLoS One. 2010;5: e11977 doi: 10.1371/journal.pone.0011977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Aliota MT, Peinado SA, Velez ID, Osorio JE. The wMel strain of Wolbachia reduces transmission of Zika Virus by Aedes aegypti. Sci Rep. Nature Publishing Group; 2016;6: 28792 doi: 10.1038/srep28792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barker CM, Niu T, Reisen WK, Hartley DM. Data-driven modeling to assess receptivity for Rift Valley fever virus. PLoS Negl Trop Dis. 2013;7: e2515 doi: 10.1371/journal.pntd.0002515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Konrad SK, Miller SN. Application of a degree-day model of West Nile virus transmission risk to the East Coast of the United States of America. Geospat Health. 2012;7: 15–20. Available: http://www.ncbi.nlm.nih.gov/pubmed/23242676 doi: 10.4081/gh.2012.100 [DOI] [PubMed] [Google Scholar]
- 45.Joubert DA, O’Neill SL. Comparison of stable and transient Wolbachia infection models in Aedes aegypti to block dengue and West Nile viruses. PLoS Negl Trop Dis. 2017;11: e0005275 doi: 10.1371/journal.pntd.0005275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Joubert DA, Walker T, Carrington LB, De Bruyne JT, Kien DHT, Hoang NLT, et al. Establishment of a Wolbachia superinfection in Aedes aegypti mosquitoes as a potential approach for future resistance management. PLoS Pathog. 2016;12: 1–19. doi: 10.1371/journal.ppat.1005434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Osborne SE, Iturbe-Ormaetxe I, Brownlie JC, O’Neill SL, Johnson KN. Antiviral protection and the importance of Wolbachia density and tissue tropism in Drosophila simulans. Appl Environ Microbiol. 2012;78: 6922–6929. doi: 10.1128/AEM.01727-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martinez J, Longdon B, Bauer S, Chan Y-S, Miller WJ, Bourtzis K, et al. Symbionts commonly provide broad spectrum resistance to viruses in insects: A comparative analysis of Wolbachia strains. PLoS Pathog. 2014;10: e1004369 doi: 10.1371/journal.ppat.1004369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hughes GL, Rivero A, Rasgon JL. Wolbachia can enhance Plasmodium infection in mosquitoes: Implications for malaria control? PLoS Pathog. 2014;10: e1004182 doi: 10.1371/journal.ppat.1004182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jupatanakul N, Sim S, Angleró-Rodríguez YI, Souza-Neto J, Das S, Poti KE, et al. Engineered Aedes aegypti JAK/STAT pathway-mediated immunity to dengue virus. PLoS Negl Trop Dis. 2017;11: e0005187 doi: 10.1371/journal.pntd.0005187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hegde S, Rasgon JL, Hughes GL. The microbiome modulates arbovirus transmission in mosquitoes. Curr Opin Virol. 2015;15: 97–102. doi: 10.1016/j.coviro.2015.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Turell MJ. Reduced Rift Valley fever virus infection rates in mosquitoes associated with feedings. Am J Trop Med Hyg. 1988;39: 597–602. [DOI] [PubMed] [Google Scholar]
- 53.Weaver SC, Lorenz LH, Scott TW. Distribution of western equine encephalomyelitis virus in the alimentary tract of Culex tarsalis (Diptera: Culicidae) following natural and artificial blood meals. J Med Entomol. 1993;30: 391–397. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
RVFV infection, dissemination, and transmission frequencies were compared between Wolbachia-infected and control mosquitoes. Replicates are displayed individually.
(XLSX)
(XLSX)
RVFV body titers were compared between mosquitoes that tested positive or negative for RVFV in their saliva. For both Wolbachia-infected and control Cx. tarsalis, mosquitoes positive for RVFV in the saliva had significantly higher RVFV body titers compared to mosquitoes negative for virus in the saliva There was no significant difference in RVFV body titer of transmitters between Wolbachia-infected and control mosquitoes (p = 0.7692). Data from three replicates were pooled and analyzed with Mann-Whitney U, and the bars represent medians.
(TIF)
RVFV body titers were compared between Wolbachia-infected and control mosquitoes for replicates 1 (A), 2 (B), and 3 (C). In all replicates, there were no significant differences in RVFV body titer between Wolbachia-infected and control mosquitoes. Data did not pass assumptions for normality and were analyzed with Mann-Whitney U, and sample sizes are denoted above data points.
(TIF)
Wolbachia levels for each mosquito, determined by qPCR, were combined across all three replicates. Wolbachia levels were significantly higher at day 14 compared to day 7. Due to violations of normality, Mann-Whitney U was used for comparisons, bars are medians, and numbers above data points are sample sizes.
(TIF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.