Highlights
-
•
Impaired movements and alignments may be associated with musculoskeletal conditions.
-
•
Signs of impaired alignments and movements may be seen before there are symptoms.
-
•
Treatment is based on using the findings of making the MSI diagnosis to correct the performance of daily activities.
Keywords: Classification, Movement system, Impairment, Rehabilitation, Musculoskeletal, Pain
Abstract
Background
Diagnoses and treatments based on movement system impairment syndromes were developed to guide physical therapy treatment.
Objectives
This masterclass aims to describe the concepts on that are the basis of the syndromes and treatment and to provide the current research on movement system impairment syndromes.
Results
The conceptual basis of the movement system impairment syndromes is that sustained alignment in a non-ideal position and repeated movements in a specific direction are thought to be associated with several musculoskeletal conditions. Classification into movement system impairment syndromes and treatment has been described for all body regions. The classification involves interpreting data from standardized tests of alignments and movements. Treatment is based on correcting the impaired alignment and movement patterns as well as correcting the tissue adaptations associated with the impaired alignment and movement patterns. The reliability and validity of movement system impairment syndromes have been partially tested. Although several case reports involving treatment using the movement system impairment syndromes concept have been published, efficacy of treatment based on movement system impairment syndromes has not been tested in randomized controlled trials, except in people with chronic low back pain.
Introduction
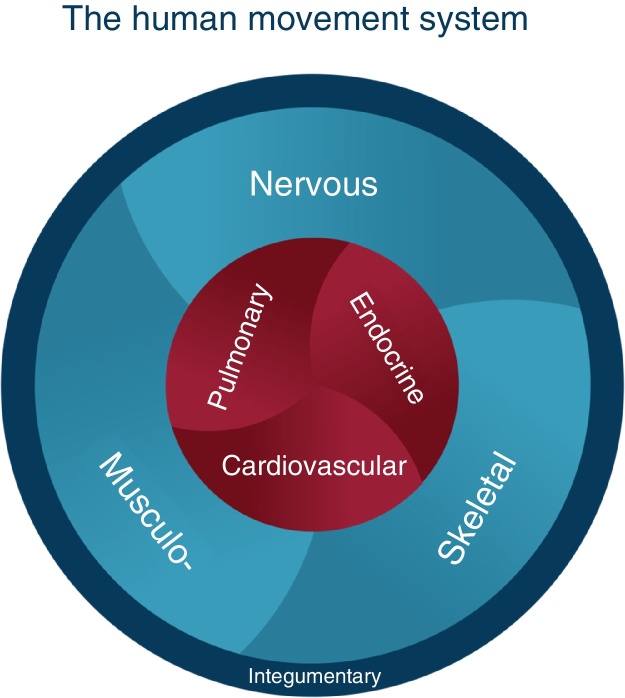
Since 1980, Sahrmann1, 2 and associates have been developing movement system impairment (MSI) syndromes to describe conditions that can be diagnosed by physical therapists and that guide treatment and inform prognosis.1, 2 The movement system was adopted as the identity of physical therapy by the American Physical Therapy Association in 2013. The definition of the movement system developed at Washington University is “a system of physiological organ systems that interact to produce movement of the body and its parts.” Fig. 1 depicts the key component systems. The conceptual framework that serves as the basis for the proposed MSI syndromes is the kinesiopathologic model (KPM) (Fig. 2). A basic premise of the KPM is that repetitive movement and sustained alignments can induce pathology. MSI syndromes are proposed to result from the repetitive use of alignments and movements that over time are proposed to become impaired and eventually induce pathoanatomical changes in tissues and joint structures. The model emphasizes the contribution of (1) the musculoskeletal system as the effector of movement, (2) the nervous system as the regulator of movement, and (3) the cardiovascular, pulmonary, and endocrine systems as providing support for the other systems, but that also are affected by movement.1, 2 For example, metabolic syndrome is known to be associated with insufficient physical activity.3 The prevailing theory, for which there is some evidence, is that the sustained alignments and repetitive movements during daily activities are the inducers of change in all the systems.4, 5, 6, 7 The modifiers of the changes are intrinsic factors such as the characteristics of the individual and extrinsic factors such as the degree and type of physical activity (work and fitness) in which a person participates. The key concept is that the body, at the joint level, follows the laws of physics and takes the path of least resistance for movement, typically in a specific direction such as flexion, extension or rotation. Determinants of the path are (1) both intra- and inter-joint relative flexibility, (2) relative stiffness of muscle and connective tissue, and (3) motor performance that becomes motor learning.1, 2 The result of a joint moving more readily in a specific direction is the development over time of hypermobility of accessory motion or micro-instability. The micro-instability causes tissue microtrauma that with repetition can become macrotrauma.
Figure 1.
Graphic of the human movement system. Developed by the faculty of the Program in Physical Therapy, Washington University School of Medicine in St. Louis.
Figure 2.
The kinesiopathologic model of the movement system.
The concepts incumbent in the KPM not only suggest that there are signs before there are symptoms, but that correction of the impaired alignments and movements and the contributing factors is also the most effective treatment of musculoskeletal pain conditions. The KPM places the emphasis on the cause of the tissue injury rather than on the pathoanatomy of the tissues. Deciding on a syndrome is based first on identifying the impaired alignments and movements across a series of clinical tests. The alignments and movements typically are associated with an elicitation or increase in symptoms. The therapist then guides the patient to correct the alignments and movements to determine if the symptoms are improved. When the examination is completed the information is used to (1) determine the syndrome, (2) identify the contributing factors, (3) determine the corrective exercises, (4) identify the alignments and movements to correct during daily activities, and (5) educate the patient about factors contributing to the musculoskeletal condition by practicing correction during activities.
The following example illustrates how correcting the impaired alignments and movements address the cause of the pain, which is not achieved by identifying the pathoanatomical source of the symptoms. A patient is referred to physical therapy with the diagnosis of Supraspinatus Tendinopathy. Tendinopathy is the pathoanatomic source of pain. After assessing the patient's scapular and humeral alignments and movements and associated symptom behavior the physical therapist makes a diagnosis of insufficient scapular upward rotation with humeral anterior glide. The other components of the examination identify the contributing factors that include (1) relative stiffness, (2) muscle strength, and (3) neuromuscular activation patterns. The idea behind the KPM is that classifying the patient according to impaired alignments and movements (i.e., Scapular Insufficient Upward Rotation, Humeral Anterior glide) is more useful to guide physical therapy treatment than identifying a pathoanatomical problem because these are the impairments to be corrected. Table 1 summarizes the key concepts underlying the proposed MSI syndromes.1
Table 1.
Kinesiopathologic model: key concepts.
| Musculoskeletal pain syndromes are the result of cumulative micro-trauma from accumulation of tissue stress and irritation resulting from sustained alignments or repeated movements in a specific direction(s) associated with daily activities. |
| The joint(s) that is moving too readily in a specific direction is the site of pain generation. |
| The readiness of a joint to move in a specific direction, i.e., the micro-instability, combined with relative stiffness, the neuromuscular activation pattern and motor learning contribute to development and persistence of the path of least resistance. |
| Treatment is based on correcting the impaired alignments and movements contributing to tissue irritation as well as correcting the tissue adaptations, such as relative stiffness, muscle weakness, and neuromuscular activation patterns. |
| Training to correct impaired alignments and movements instead of training “isolated muscles” will induce appropriate neural and musculoskeletal adaptations. |
Relative intra- and inter-joint flexibility and relative stiffness
Important KPM concepts related to the proposed MSI syndromes are relative flexibility and relative stiffness.1, 2 Relative flexibility refers to a condition of the joint itself. Intra-joint relative flexibility is hypermobility of accessory motions, i.e., spin, roll, or glide. One or more of these motions occurs too readily resulting in excessive range of motion, as well as in how frequently the motion occurs. Inter-joint relative flexibility refers to motion of adjoining joints occurring more readily in one of the joints even if the motion should be occurring in the other joint. For example, during forward bending the lumbar spine flexes more readily than the hip flexes.8 Stiffness refers to the resistance present during passive elongation of muscle and connective tissue. Stiffness depends on the hypertrophy of muscle and the amount of collagen when considering whole muscle.9, 10, 11, 12, 13 Viscosity also contributes to stiffness and is affected by the rate of movement.14, 15 Movement follows the law of physics and takes the path of least resistance with (1) relative flexibility, (2) relative stiffness, and (3) motor learning as determinants of the path. When movement is performed across multiple joints, the body will tend to increase the amount of movement in the joint with lower resistance to motion or lower stiffness compared to the joint with higher resistance to motion or higher stiffness. For example, during hip extension, the lumbar spine will move more readily than the hip joint into extension. Relative flexibility impairments can also occur during single joint movements, such as knee extension in sitting. If the pelvis tilts posteriorly and the lumbar spine flexes early during the knee movement, this indicates an impairment in relative flexibility of the lumbar spine with the hamstring muscles being stiffer than the back extensor muscles.2
Movement system impairments: inducers and modifiers
Sustained alignments and repeated movements associated with daily activities are the inducers of the tissue adaptations, impaired alignments and movements associated with MSI syndromes.1, 2 For example, people who regularly participate in rotational demand activities have increased lumbopelvic rotation compared to people who do not participate in rotational demand activities.16, 17 Several studies have found that the repetition of movements associated with various sports leads to adaptations in different tissues including bone, joint and its surrounding tissues and muscles.4, 5, 6, 7
The effects of sustained alignments and repeated movements on tissue adaptations and the development of symptoms is modified by several factors, including age, gender, tissue mobility, anthropometrics, activity level and psychological factors.18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 Older individuals may respond differently to repeated movements than younger individuals because their joints and surrounding tissues usually have some degree of degeneration.35, 36 Older people also have different pain sensitivity compared to younger people.21, 25 Differences in alignment between men and women28 may also influence the effect of repeated movements or sustained alignments. Men and women with low back pain show different pain-inducing alignments and movements.32 Women have increased knee abduction during weight-bearing activities when compared to men22 resulting in increased risk of patellofemoral pain26 and anterior cruciate ligament tears.37 Tissue mobility may also influence movement precision. People with joint hypermobility have reduced joint proprioception33 and may be at greater risk of musculoskeletal conditions.20 Anthropometrics also should be considered as a potential modifier. For example, women with lower femoral neck shaft angle are at increased risk for greater trochanteric pain syndrome.24 Individuals with a long trunk usually have depressed shoulder alignment which has been associated with decreased pain threshold of the upper trapezius muscle region.19 While appropriate activity levels may protect from musculoskeletal conditions, inadequate or excessive activity levels may increase risk.18, 27, 29, 38 The development of imprecise motion is also considered to be a factor in the development of musculoskeletal pain. Psychological factors should also be considered since they can influence pain intensity34 and change the outcome of different musculoskeletal conditions like tendinopathy, low back pain and anterior cruciate ligament reconstruction.23, 30, 31
Impairments of alignment and movement in people with musculoskeletal pain and healthy people
The KPM is based on restoring ideal alignment and correcting movement impairments. Although some studies have not found differences in alignment and movement patterns between healthy people and people with musculoskeletal symptoms,39, 40 others have found significant differences.41, 42, 43, 44, 45, 46, 47, 48 Patellofemoral pain is related to increased peak hip adduction, internal rotation and contralateral pelvic drop.46 Studies assessing kinematics of the shoulder complex have identified differences between people with and people without shoulder pain.44, 45 Sitting alignment is related to upper quadrant musculoskeletal pain reported in sitting.42 People with femoroacetabular impingement have different pelvic movement during hip flexion movements compared to healthy subjects.41, 43, 48 People with low back pain move their lumbopelvic region to a greater extent and earlier during lower limb movements than people without low back pain.17, 47
Although most studies assess impairments of alignment and movement after the onset of musculoskeletal pain, there also are studies showing that some alignment and movement impairments seen in asymptomatic people may increase their risk for development of musculoskeletal pain. For example, lumbopelvic movement impairments during hip abduction49 as well as standing in more lumbar lordosis50 may be a risk factor for low back pain development in prolonged standing.
Movement system impairment examination and classification
The MSI examination and process for classification51, 52, 53 involve interpreting data from a series of tests of alignments and movements. Judgments about the timing and the magnitude of movement and degree of end-range alignment in specific joints, and the effect on symptoms are made during each test. Tests that are symptom-provoking are immediately followed by systematic corrections of the impairment to determine the role on the patient's symptoms. Correction involves (1) minimizing movement that occurs in the early part of the range of motion or excessive movement, particularly accessory motion, in the affected joint, while increasing movement in other joints or (2) reducing positions of end-range alignment in specific direction(s). An improvement in the symptoms indicates that the alignment or movement impairment is associated with the patient's symptoms.53, 54, 55
MSI syndromes have been developed for all body regions, including the cervical, thoracic and lumbar spine, shoulder, elbow and hand, hip, knee, ankle and foot1, 2 (Table 2).
Table 2.
MSI syndromes for different body regions.
| Body region | Syndrome |
|---|---|
| Cervical | Cervical extension |
| Cervical extension-rotation | |
| Cervical flexion | |
| Cervical flexion-rotation | |
| Cervical rotation | |
| Thoracic | Thoracic rotation-flexion |
| Thoracic flexion | |
| Thoracic rotation-extension | |
| Thoracic rotation | |
| Thoracic extension | |
| Shoulder | Scapular insufficient upward rotation |
| Scapular internal rotation | |
| Scapular depression | |
| Scapular abduction | |
| Scapular adduction | |
| Scapular winging and tilting | |
| Humeral anterior glide | |
| Humeral superior glide | |
| Shoulder medial rotation glenohumeral hypomobility | |
| Elbow | Wrist extension with forearm pronation |
| Elbow hypomobility | |
| Elbow flexion | |
| Elbow valgus | |
| Elbow extension | |
| Wrist flexion with forearm pronation elbow impairment | |
| Wrist and hand | Insufficient finger and/or thumb flexion |
| Insufficient finger and/or thumb extension | |
| Insufficient thumb palmar abduction and/or opposition | |
| Thumb carpometacarpal accessory hypermobility | |
| Finger or thumb flexion with or without finger rotation | |
| Source or regional impairment of the hand | |
| Lumbar spine | Lumbar flexion |
| Lumbar extension | |
| Lumbar rotation | |
| Lumbar rotation with flexion | |
| Lumbar rotation with extension | |
| Hip | Femoral anterior glide |
| Femoral anterior glide with medial rotation | |
| Femoral anterior glide with lateral rotation | |
| Femoral posterior glide | |
| Femoral multidirectional accessory hypermobility | |
| Femoral hypomobility with superior glide | |
| Hip adduction | |
| Hip adduction with medial rotation | |
| Femoral lateral glide | |
| Hip extension with knee extension | |
| Hip extension with medial rotation | |
| Hip lateral rotation | |
| Knee | Tibiofemoral rotation |
| Tibiofemoral hypomobility | |
| Knee extension | |
| Knee extension with patellar superior glide | |
| Knee hyperextension | |
| Patellar lateral glide knee impairment | |
| Foot and ankle | Pronation |
| Supination | |
| Insufficient dorsiflexion | |
| Hypomobility | |
| Foot and ankle impairment | |
| Proximal tibiofibular glide | |
MSI syndromes: validity and reliability testing
Several studies have been performed to examine the validity of the MSI syndromes all of them examining either the lumbar region8, 52, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70 or the knee joint.71 Partial construct validity has been reported for MSI-syndromes proposed for the lumbar and knee regions.59, 71 Other studies have compared movement impairments and associated signs and symptoms between different MSI syndromes. Gombatto et al.56 showed that people with Lumbar Rotation with Extension Syndrome displayed an asymmetric pattern of lumbar movement during a trunk lateral flexion test compared to people with Lumbar Rotation Syndrome. People with Lumbar Rotation Syndrome and people with Lumbar Rotation with Extension Syndrome displayed systematic differences in hip and lumbopelvic region movement during the test of active hip lateral rotation.52, 57 Kim et al.8 showed that people with Lumbar Rotation with Flexion Syndrome have a greater amount of lumbar flexion during a trunk flexion test compared to people with Lumbar Rotation with Extension Syndrome. People with Lumbar Rotation Syndrome demonstrated greater end-range lumbar flexion during slumped sitting compared to people with Lumbar Rotation with Extension Syndrome.58
The reliability of examiners to classify also has been assessed for the lumbar spine and the knee. Clinicians are able to reliably classify people into MSI syndromes for the lumbar spine,60, 62, 72, 73, 74, 75 even if they have limited clinical experience.75, 76, 77 Kaibafvala et al.78 assessed reliability for the MSI syndromes for the knee region. Kappa values of intra- and inter-rater reliability for judgments of classifications ranged from 0.66 to 0.71, and 0.48 to 0.58, respectively.
MSI syndromes: treatment
Treatment includes patient education, analysis and correction of daily activities and prescription of specific exercises.1, 2, 79, 80, 81 Patient education refers to educating the patient about how the repetition of impaired movements and sustained alignments in a specific direction may be related to his musculoskeletal condition and how to correct the impairments during all of his daily activities, particularly those that cause symptoms. For example, patients with Scapular Depression Syndrome may be taught to keep their scapula elevated by supporting their arms while working at a computer. The goal of the support is to reduce the sustained load on the cervical spine and the muscles that elevate the scapulae.19, 82, 83
The most important part of the program is teaching the patient to perform daily activities correctly and without symptoms. Because the sustained alignments and repeated movements are the cause of the problem they must be corrected.1, 2 The correction also helps the patient know what contributes to the symptoms and how to decrease or limit the symptoms. Patients are advised to correct their daily activities throughout the day. Recent work has shown that in people with LBP higher adherence to performing corrected daily activities compared to adherence to exercise is associated with greater improvement in function and pain as well as a number of other LBP-related outcomes.84
The prescription of specific exercises is based on the patient's syndrome and contributing factors identified during the initial examination. The exercises require practicing correction of impaired alignments and movements identified during the clinical tests in the examination. For example, a patient with Hip Adduction Syndrome may present with excessive hip adduction associated with hip pain while performing a partial squat movement test. The partial squat movement test then would be used as a specific exercise having the patient modify the amount and timing of hip adduction that occurs during the squat.
The specific exercises and activities are performed during the treatment sessions and also are part of the home program. Each patient receives pictures or figures of the specific exercises and daily activities with written instructions. Videos also can be used to teach the patient how to perform the exercises and activities. The patient's ability to perform his program is assessed during clinic visits and used to progress the program. Judgments about the patient's knowledge of the key concept of each exercise or activity and independence in performance of each exercise or activity is important information used to make decisions about when and what to progress.85
Clinical trials of treatment of MSI syndromes
Several case reports involving treatment of MSI syndromes have been published.79, 80, 81, 86, 87, 88, 89, 90 The studies describe in detail the examination and treatment of people with shoulder pain,86 low back pain,79, 80, 81, 88 abdominal pain,90 cervicogenic headache89 and knee pain.87 Treatment also was described in a feasibility randomized clinical trial in people with chronic hip pain.91 In a randomized controlled trial assessing the effect of treatment of people with chronic low back pain,84, 92 Van Dillen et al.84 found no difference when comparing the efficacy of a Classification-Specific (CS) treatment to a non-Classification-Specific (NCS) treatment in people with chronic non-specific low back pain. Both CS and NCS treatments included some form of exercise and correction of performance of daily activities. The CS treatment involved education, exercise and daily activity correction as described for the MSI syndromes above. The NCS treatment involved education and daily activity correction emphasizing maintenance of a neutral spine. Exercise was directed at strengthening the trunk and increasing the flexibility of the trunk and lower limbs. The authors proposed that the similar improvements found in both groups was because both were prescribed correction of daily activities that emphasized maintaining a neutral spine while increasing movement of other joints when performing daily activities. The proposal also was based on the fact that people in the CS and NCS group adhered more and longer to correcting daily activities than they did to exercise.
Conclusion
The MSI based classification and treatment allows physical therapists to diagnosis and treat musculoskeletal conditions based on principles of the KPM where impaired alignments and movements are proposed to induce pain and pathology. MSI syndromes and treatment have been described for all body regions. The reliability and validity of the system for some anatomical regions have been partially described.8, 52, 56, 57, 58, 59, 60, 62, 71, 72, 73, 75, 76, 77, 78 Several case reports describing MSI examination and treatment of different musculoskeletal conditions have been published79, 80, 81, 86, 87, 88, 89, 90 although efficacy of treatment has not been tested in randomized controlled trials, except in people with chronic low back pain.84 More randomized controlled trials are needed to assess the efficacy of treatment of MSI syndromes.
Conflicts of interest
Daniel Azevedo works as an instructor in continuing education courses that include MSI content.
Shirley Sahrmann teaches continuing education courses on MSI. She has published two books. She receives royalties on Diagnosis and Treatment of Impairment Syndromes from Elsevier Publishing Company. She does not receive any royalties from the book Movement System Impairment syndromes of the Cervical and Thoracic Spine and the Extremities also published by Elsevier.
Linda Van Dillen does not have any conflict of interests.
Acknowledgements
This work was supported in part by the NIH/NICHD/NCMRR Grant number HD 047709 (PI: Van Dillen).
References
- 1.Sahrmann S. Elsevier Health Sciences; 2010. Movement System Impairment Syndromes of the Extremities, Cervical and Thoracic Spines. [Google Scholar]
- 2.Sahrmann S.A. 1st ed. Mosby; St Louis: 2001. Diagnosis and Treatment of Movement Impairment Syndromes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Oliveira R.G., Guedes D.P. Physical activity, sedentary behavior, cardiorespiratory fitness and metabolic syndrome in adolescents: systematic review and meta-analysis of observational evidence. PLoS ONE. 2016;11(12):e0168503. doi: 10.1371/journal.pone.0168503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Medrano D., Jr., Smith D. Soccer: a comparison of knee joint laxity among male and female collegiate soccer players and non-athletes. Sports Biomech. 2003;2(2):203–212. doi: 10.1080/14763140308522818. [DOI] [PubMed] [Google Scholar]
- 5.Mascarenhas V.V., Rego P., Dantas P. Imaging prevalence of femoroacetabular impingement in symptomatic patients, athletes, and asymptomatic individuals: a systematic review. Eur J Radiol. 2016;85(January (1)):73–95. doi: 10.1016/j.ejrad.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 6.Kibler W.B., Sciascia A., Thomas S.J. Glenohumeral internal rotation deficit: pathogenesis and response to acute throwing. Sports Med Arthrosc. 2012;20(March (1)):34–38. doi: 10.1097/JSA.0b013e318244853e. [DOI] [PubMed] [Google Scholar]
- 7.Arnout N., Verhaar J., Bellemans J. How does lower leg alignment differ between soccer players, other athletes and non-athletic controls? Osteoarthr Cartil. 2016;24:S108–S109. doi: 10.1007/s00167-016-4348-y. [DOI] [PubMed] [Google Scholar]
- 8.Kim M.-H., Yi C.-H., Kwon O.-Y. Comparison of lumbopelvic rhythm and flexion-relaxation response between 2 different low back pain subtypes. Spine (Phila Pa 1976) 2013;38(15):1260–1267. doi: 10.1097/BRS.0b013e318291b502. [DOI] [PubMed] [Google Scholar]
- 9.Chleboun G.S., Howell J.N., Conatser R.R., Giesey J.J. The relationship between elbow flexor volume and angular stiffness at the elbow. Clin Biomech (Bristol, Avon) 1997;12(6):383–392. doi: 10.1016/s0268-0033(97)00027-2. [DOI] [PubMed] [Google Scholar]
- 10.Gajdosik R.L. Passive extensibility of skeletal muscle: review of the literature with clinical implications. Clin Biomech (Bristol, Avon) 2001;16(February (2)):87–101. doi: 10.1016/s0268-0033(00)00061-9. [DOI] [PubMed] [Google Scholar]
- 11.Herbert R. The passive mechanical properties of muscle and their adaptations to altered patterns of use. Aust J Physiother. 1988;34(3):141–149. doi: 10.1016/S0004-9514(14)60606-1. [DOI] [PubMed] [Google Scholar]
- 12.Rakos D.M., Shaw K.A., Fedor R.L., Lamanna M., Yocum C.C., Lawrence K.J. Interrater reliability of the active-knee-extension test for hamstring length in school-aged children. Pediatr Phys Ther. 2001;13(Spring (1)):37–41. [PubMed] [Google Scholar]
- 13.Ryan E.D., Herda T.J., Costa P.B. Passive properties of the muscle-tendon unit: the influence of muscle cross-sectional area. Muscle Nerve. 2009;39(February (2)):227–229. doi: 10.1002/mus.21218. [DOI] [PubMed] [Google Scholar]
- 14.Valle M.S., Casabona A., Sgarlata R., Garozzo R., Vinci M., Cioni M. The pendulum test as a tool to evaluate passive knee stiffness and viscosity of patients with rheumatoid arthritis. BMC Musculoskelet Disord. 2006;7(1):89. doi: 10.1186/1471-2474-7-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Magnusson S.P., Simonsen E.B., Aagaard P., Boesen J., Johannsen F., Kjaer M. Determinants of musculoskeletal flexibility: viscoelastic properties, cross-sectional area, EMG and stretch tolerance. Scand J Med Sci Sports. 1997;7(August (4)):195–202. doi: 10.1111/j.1600-0838.1997.tb00139.x. [DOI] [PubMed] [Google Scholar]
- 16.Sadeghisani M., Sobhani V., Kouchaki E., Bayati A., Ashari A.A., Mousavi M. Comparison of lumbopelvic and hip movement patterns during passive hip external rotation in two groups of low back pain patients with and without rotational demand activities. Ortop Traumatol Rehabil. 2015;17(6):611–618. doi: 10.5604/15093492.1193032. [DOI] [PubMed] [Google Scholar]
- 17.Weyrauch S.A., Bohall S.C., Sorensen C.J., Van Dillen L.R. Association between rotation-related impairments and activity type in people with and without low back pain. Arch Phys Med Rehabil. 2015;96(8):1506–1517. doi: 10.1016/j.apmr.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aartun E., Boyle E., Hartvigsen J. The most physically active Danish adolescents are at increased risk for developing spinal pain: a two-year prospective cohort study. BMJ Open Sport Exerc Med. 2016;2(1):e000097. doi: 10.1136/bmjsem-2015-000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Azevedo D.C., Pires T.L., Andrade F.S., McDonnell M.K. Influence of scapular position on the pressure pain threshold of the upper trapezius muscle region. Eur J Pain. 2008;12(2):226–232. doi: 10.1016/j.ejpain.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 20.Cattalini M., Khubchandani R., Cimaz R. When flexibility is not necessarily a virtue: a review of hypermobility syndromes and chronic or recurrent musculoskeletal pain in children. Pediatr Rheumatol Online J. 2015;13(1):1. doi: 10.1186/s12969-015-0039-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cole L.J., Farrell M.J., Gibson S.J., Egan G.F. Age-related differences in pain sensitivity and regional brain activity evoked by noxious pressure. Neurobiol Aging. 2010;31(March (3)):494–503. doi: 10.1016/j.neurobiolaging.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 22.Cronstrom A., Creaby M.W., Nae J., Ageberg E. Gender differences in knee abduction during weight-bearing activities: A systematic review and meta-analysis. Gait Posture. 2016;49(September):315–328. doi: 10.1016/j.gaitpost.2016.07.107. [DOI] [PubMed] [Google Scholar]
- 23.Everhart J.S., Best T.M., Flanigan D.C. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(March (3)):752–762. doi: 10.1007/s00167-013-2699-1. [DOI] [PubMed] [Google Scholar]
- 24.Fearon A., Stephens S., Cook J. The relationship of femoral neck shaft angle and adiposity to greater trochanteric pain syndrome in women. A case control morphology and anthropometric study. Br J Sports Med. 2012;46(September (12)):888–892. doi: 10.1136/bjsports-2011-090744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gibson S.J., Farrell M. A review of age differences in the neurophysiology of nociception and the perceptual experience of pain. Clin J Pain. 2004;20(July–August (4)):227–239. doi: 10.1097/00002508-200407000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Glaviano N.R., Kew M., Hart J.M., Saliba S. Demographic and epidemiological trends in patellofemoral pain. Int J Sports Phys Ther. 2015;10(June (3)):281–290. [PMC free article] [PubMed] [Google Scholar]
- 27.Heneweer H., Vanhees L., Picavet H.S. Physical activity and low back pain: a U-shaped relation? Pain. 2009;143(May (1–2)):21–25. doi: 10.1016/j.pain.2008.12.033. [DOI] [PubMed] [Google Scholar]
- 28.Janssen M.M., Drevelle X., Humbert L., Skalli W., Castelein R.M. Differences in male and female spino-pelvic alignment in asymptomatic young adults: a three-dimensional analysis using upright low-dose digital biplanar X-rays. Spine (Phila Pa 1976) 2009;34(23):E826–E832. doi: 10.1097/BRS.0b013e3181a9fd85. [DOI] [PubMed] [Google Scholar]
- 29.Kayihan G. Relationship between daily physical activity level and low back pain in young, female desk-job workers. Int J Occup Med Environ Health. 2014;27(5):863–870. doi: 10.2478/s13382-014-0315-3. [DOI] [PubMed] [Google Scholar]
- 30.Mallows A., Debenham J., Walker T., Littlewood C. Association of psychological variables and outcome in tendinopathy: a systematic review. Br J Sports Med. 2017;51(May (9)):743–748. doi: 10.1136/bjsports-2016-096154. [DOI] [PubMed] [Google Scholar]
- 31.Pinheiro M.B., Ferreira M.L., Refshauge K. Symptoms of depression as a prognostic factor for low back pain: a systematic review. Spine J. 2016;16(1):105–116. doi: 10.1016/j.spinee.2015.10.037. [DOI] [PubMed] [Google Scholar]
- 32.Scholtes S.A., Van Dillen L.R. Gender-related differences in prevalence of lumbopelvic region movement impairments in people with low back pain. J Orthop Sports Phys Ther. 2007;37(December (12)):744–753. doi: 10.2519/jospt.2007.2610. [DOI] [PubMed] [Google Scholar]
- 33.Smith T.O., Jerman E., Easton V. Do people with benign joint hypermobility syndrome (BJHS) have reduced joint proprioception? A systematic review and meta-analysis. Rheumatol Int. 2013;33(11):2709–2716. doi: 10.1007/s00296-013-2790-4. [DOI] [PubMed] [Google Scholar]
- 34.Sorensen C.J., George S.Z., Callaghan J.P., Van Dillen L.R. Psychological factors are related to pain intensity in back-healthy people who develop clinically relevant pain during prolonged standing: a preliminary study. PM R. 2016;8(November (11)):1031–1038. doi: 10.1016/j.pmrj.2016.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Teraguchi M., Yoshimura N., Hashizume H. Progression, incidence, and risk factors for intervertebral disc degeneration in a longitudinal population-based cohort: the Wakayama Spine Study. Osteoarthr Cartil. 2017;25(July (7)):1122–1131. doi: 10.1016/j.joca.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 36.Toh W.S., Brittberg M., Farr J. Cellular senescence in aging and osteoarthritis: implications for cartilage repair. Acta Orthop. 2016:1–9. doi: 10.1080/17453674.2016.1235087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Walden M., Hagglund M., Werner J., Ekstrand J. The epidemiology of anterior cruciate ligament injury in football (soccer): a review of the literature from a gender-related perspective. Knee Surg Sports Traumatol Arthrosc. 2011;19(January (1)):3–10. doi: 10.1007/s00167-010-1172-7. [DOI] [PubMed] [Google Scholar]
- 38.Briani R.V., Pazzinatto M.F., De Oliveira Silva D., Azevedo F.M. Different pain responses to distinct levels of physical activity in women with patellofemoral pain. Braz J Phys Ther. 2017;21(March–April (2)):138–143. doi: 10.1016/j.bjpt.2017.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barrett E., O’Keeffe M., O'Sullivan K., Lewis J., McCreesh K. Is thoracic spine posture associated with shoulder pain, range of motion and function? A systematic review. Man Ther. 2016;26:38–46. doi: 10.1016/j.math.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 40.Ratcliffe E., Pickering S., McLean S., Lewis J. Is there a relationship between subacromial impingement syndrome and scapular orientation? A systematic review. Br J Sports Med. 2014;48(16):1251–1256. doi: 10.1136/bjsports-2013-092389. [DOI] [PubMed] [Google Scholar]
- 41.Azevedo D.C., Paiva E.B., Lopes A.M.A. Pelvic rotation in femoroacetabular impingement is decreased compared to other symptomatic hip conditions. J Orthop Sports Phys Ther. 2016;46(11):957–964. doi: 10.2519/jospt.2016.6713. [DOI] [PubMed] [Google Scholar]
- 42.Brink Y., Louw Q., Grimmer K., Jordaan E. The relationship between sitting posture and seated-related upper quadrant musculoskeletal pain in computing South African adolescents: a prospective study. Man Ther. 2015;20(6):820–826. doi: 10.1016/j.math.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 43.Lamontagne M., Kennedy M.J., Beaule P.E. The effect of cam FAI on hip and pelvic motion during maximum squat. Clin Orthop Relat Res. 2009;467(March (3)):645–650. doi: 10.1007/s11999-008-0620-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lawrence R.L., Braman J.P., Laprade R.F., Ludewig P.M. Comparison of 3-dimensional shoulder complex kinematics in individuals with and without shoulder pain, part 1: sternoclavicular, acromioclavicular, and scapulothoracic joints. J Orthop Sports Phys Ther. 2014;44(9):636–638. doi: 10.2519/jospt.2014.5339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lawrence R.L., Braman J.P., Staker J.L., LaPrade R.F., Ludewig P.M. Comparison of 3-dimensional shoulder complex kinematics in individuals with and without shoulder pain, part 2: glenohumeral joint. J Orthop Sports Phys Ther. 2014;44(9):646–655. doi: 10.2519/jospt.2014.5556. B1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Neal B.S., Barton C.J., Gallie R., O’Halloran P., Morrissey D. Runners with patellofemoral pain have altered biomechanics which targeted interventions can modify: a systematic review and meta-analysis. Gait Posture. 2016;45:69–82. doi: 10.1016/j.gaitpost.2015.11.018. [DOI] [PubMed] [Google Scholar]
- 47.Scholtes S.A., Gombatto S.P., Van Dillen L.R. Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests. Clin Biomech (Bristol, Avon) 2009;24(January (1)):7–12. doi: 10.1016/j.clinbiomech.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Van Houcke J., Pattyn C., Vanden Bossche L., Redant C., Maes J.W., Audenaert E.A. The pelvifemoral rhythm in cam-type femoroacetabular impingement. Clin Biomech (Bristol, Avon) 2014;29(January (1)):63–67. doi: 10.1016/j.clinbiomech.2013.10.019. [DOI] [PubMed] [Google Scholar]
- 49.Sorensen C.J., Johnson M.B., Norton B.J., Callaghan J.P., Van Dillen L.R. Asymmetry of lumbopelvic movement patterns during active hip abduction is a risk factor for low back pain development during standing. Hum Mov Sci. 2016;50:38–46. doi: 10.1016/j.humov.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sorensen C.J., Norton B.J., Callaghan J.P., Hwang C.-T., Van Dillen L.R. Is lumbar lordosis related to low back pain development during prolonged standing? Man Ther. 2015;20(4):553–557. doi: 10.1016/j.math.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Van Dillen L.R., Bloom N.J., Gombatto S.P., Susco T.M. Hip rotation range of motion in people with and without low back pain who participate in rotation-related sports. Phys Ther Sport. 2008;9(May (2)):72–81. doi: 10.1016/j.ptsp.2008.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Van Dillen L.R., Gombatto S.P., Collins D.R., Engsberg J.R., Sahrmann S.A. Symmetry of timing of hip and lumbopelvic rotation motion in 2 different subgroups of people with low back pain. Arch Phys Med Rehabil. 2007;88(March (3)):351–360. doi: 10.1016/j.apmr.2006.12.021. [DOI] [PubMed] [Google Scholar]
- 53.Van Dillen L.R., Sahrmann S.A., Norton B.J. Effect of active limb movements on symptoms in patients with low back pain. J Orthop Sports Phys Ther. 2001;31(August (8)):402–413. doi: 10.2519/jospt.2001.31.8.402. (discussion 414–408) [DOI] [PubMed] [Google Scholar]
- 54.Van Dillen L.R., Sahrmann S.A., Norton B.J., Caldwell C.A., McDonnell M.K., Bloom N. The effect of modifying patient-preferred spinal movement and alignment during symptom testing in patients with low back pain: a preliminary report. Arch Phys Med Rehabil. 2003;84(March (3)):313–322. doi: 10.1053/apmr.2003.50010. [DOI] [PubMed] [Google Scholar]
- 55.Salsich G.B., Graci V., Maxam D.E. The effects of movement pattern modification on lower extremity kinematics and pain in women with patellofemoral pain. J Orthop Sports Phys Ther. 2012;42(December (12)):1017–1024. doi: 10.2519/jospt.2012.4231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gombatto S.P., Collins D.R., Sahrmann S.A., Engsberg J.R., Van Dillen L.R. Patterns of lumbar region movement during trunk lateral bending in 2 subgroups of people with low back pain. Phys Ther. 2007;87(April (4)):441–454. doi: 10.2522/ptj.20050370. [DOI] [PubMed] [Google Scholar]
- 57.Harris-Hayes M., Sahrmann S.A., Van Dillen L.R. Relationship between the hip and low back pain in athletes who participate in rotation-related sports. J Sport Rehabil. 2009;18(February (1)):60–75. doi: 10.1123/jsr.18.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hoffman S.L., Johnson M.B., Zou D., Van Dillen L.R. Differences in end-range lumbar flexion during slumped sitting and forward bending between low back pain subgroups and genders. Man Ther. 2012;17(April (2)):157–163. doi: 10.1016/j.math.2011.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Van Dillen L.R., Sahrmann S.A., Norton B.J., Caldwell C.A., McDonnell M.K., Bloom N.J. Movement system impairment-based categories for low back pain: stage 1 validation. J Orthop Sports Phys Ther. 2003;33(March (3)):126–142. doi: 10.2519/jospt.2003.33.3.126. [DOI] [PubMed] [Google Scholar]
- 60.Kim M.-H., Yoo W.-G., Choi B.-R. Differences between two subgroups of low back pain patients in lumbopelvic rotation and symmetry in the erector spinae and hamstring muscles during trunk flexion when standing. J Electromyogr Kinesiol. 2013;23(2):387–393. doi: 10.1016/j.jelekin.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 61.Marich A.V., Hwang C.T., Salsich G.B., Lang C.E., Van Dillen L.R. Consistency of a lumbar movement pattern across functional activities in people with low back pain. Clin Biomech (Bristol, Avon) 2017;44(May):45–51. doi: 10.1016/j.clinbiomech.2017.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Norton B.J., Sahrmann S.A., Van Dillen L.R. Differences in measurements of lumbar curvature related to gender and low back pain. J Orthop Sports Phys Ther. 2004;34(September (9)):524–534. doi: 10.2519/jospt.2004.34.9.524. [DOI] [PubMed] [Google Scholar]
- 63.Roussel N.A., Nijs J., Mottram S., Van Moorsel A., Truijen S., Stassijns G. Altered lumbopelvic movement control but not generalized joint hypermobility is associated with increased injury in dancers. A prospective study. Man Ther. 2009;14(6):630–635. doi: 10.1016/j.math.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 64.Luomajoki H., Kool J., de Bruin E.D., Airaksinen O. Movement control tests of the low back; evaluation of the difference between patients with low back pain and healthy controls. BMC Musculoskelet Disord. 2008;9(December (1)):170. doi: 10.1186/1471-2474-9-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hoffman S.L., Johnson M.B., Zou D., Van Dillen L.R. Sex differences in lumbopelvic movement patterns during hip medial rotation in people with chronic low back pain. Arch Phys Med Rehabil. 2011;92(7):1053–1059. doi: 10.1016/j.apmr.2011.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sadeghisani M., Namnik N., Karimi M. Evaluation of differences between two groups of low back pain patients with and without rotational demand activities based on hip and lumbopelvic movement patterns. Ortop Traumatol Rehabil. 2015;17(1):51–57. doi: 10.5604/15093492.1143536. [DOI] [PubMed] [Google Scholar]
- 67.Hoffman S.L., Johnson M.B., Zou D., Van Dillen L.R. Gender differences in modifying lumbopelvic motion during hip medial rotation in people with low back pain. Rehabil Res Pract. 2012;2012 doi: 10.1155/2012/635312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gombatto S.P., D’Arpa N., Landerholm S. Differences in kinematics of the lumbar spine and lower extremities between people with and without low back pain during the down phase of a pick up task, an observational study. Musculoskelet Sci Pract. 2017;28:25–31. doi: 10.1016/j.msksp.2016.12.017. [DOI] [PubMed] [Google Scholar]
- 69.Mazzone B., Wood R., Gombatto S. Spine kinematics during prone extension in people with and without low back pain and among classification-specific low back pain subgroups. J Orthop Sports Phys Ther. 2016;46(7):571–579. doi: 10.2519/jospt.2016.6159. [DOI] [PubMed] [Google Scholar]
- 70.Gombatto S.P., Collins D.R., Sahrmann S.A., Engsberg J.R., Van Dillen L.R. Gender differences in pattern of hip and lumbopelvic rotation in people with low back pain. Clin Biomech (Bristol, Avon) 2006;21(3):263–271. doi: 10.1016/j.clinbiomech.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 71.Kajbafvala M., Ebrahimi-Takamjani I., Salavati M. Validation of the movement system impairment-based classification in patients with knee pain. Man Ther. 2016;25(September):19–26. doi: 10.1016/j.math.2016.05.333. [DOI] [PubMed] [Google Scholar]
- 72.Harris-Hayes M., Van Dillen L.R. The inter-tester reliability of physical therapists classifying low back pain problems based on the movement system impairment classification system. PM R. 2009;1(February (2)):117–126. doi: 10.1016/j.pmrj.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Henry S.M., Van Dillen L.R., Trombley A.L., Dee J.M., JYB Reliability of the movement system impairment classification schema for subgrouping people with low back pain. J Orthop Sports Phys Ther. 2009;39:A97. [Google Scholar]
- 74.Luomajoki H., Kool J., de Bruin E.D., Airaksinen O. Reliability of movement control tests in the lumbar spine. BMC Musculoskelet Disord. 2007;8(September):90. doi: 10.1186/1471-2474-8-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Trudelle-Jackson E., Sarvaiya-Shah S.A., Wang S.S. Interrater reliability of a movement impairment-based classification system for lumbar spine syndromes in patients with chronic low back pain. J Orthop Sports Phys Ther. 2008;38(June (6)):371–376. doi: 10.2519/jospt.2008.2760. [DOI] [PubMed] [Google Scholar]
- 76.Henry S.M., Van Dillen L.R., Trombley A.R., Dee J.M., Bunn J.Y. Reliability of novice raters in using the movement system impairment approach to classify people with low back pain. Man Ther. 2013;18(February (1)):35–40. doi: 10.1016/j.math.2012.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Azevedo D.C., Lauria A.C., Pereira A.R. Intraexaminer and interexaminer reliability of pressure biofeedback unit for assessing lumbopelvic stability during 6 lower limb movement tests. J Manipulative Physiol Ther. 2013;36(January (1)):33–43. doi: 10.1016/j.jmpt.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 78.Kajbafvala M., Ebrahimi-Takamjani I., Salavati M. Intratester and intertester reliability of the movement system impairment-based classification for patients with knee pain. Man Ther. 2016;26(December):117–124. doi: 10.1016/j.math.2016.07.014. [DOI] [PubMed] [Google Scholar]
- 79.Harris-Hayes M., Van Dillen L.R., Sahrmann S.A. Classification, treatment and outcomes of a patient with lumbar extension syndrome. Physiother Theory Pract. 2005;21(July–September (3)):181–196. doi: 10.1080/09593980500212987. [DOI] [PubMed] [Google Scholar]
- 80.Maluf K.S., Sahrmann S.A., Van Dillen L.R. Use of a classification system to guide nonsurgical management of a patient with chronic low back pain. Phys Ther. 2000;80(November (11)):1097–1111. [PubMed] [Google Scholar]
- 81.Van Dillen L.R., Sahrmann S.A., Wagner J.M. Classification, intervention, and outcomes for a person with lumbar rotation with flexion syndrome. Phys Ther. 2005;85(April (4)):336–351. [PubMed] [Google Scholar]
- 82.Van Dillen L.R., McDonnell M.K., Susco T.M., Sahrmann S.A. The immediate effect of passive scapular elevation on symptoms with active neck rotation in patients with neck pain. Clin J Pain. 2007;23(October (8)):641–647. doi: 10.1097/AJP.0b013e318125c5b6. [DOI] [PubMed] [Google Scholar]
- 83.Andrade G.T., Azevedo D.C., De Assis Lorentz I. Influence of scapular position on cervical rotation range of motion. J Orthop Sports Phys Ther. 2008;38(November (11)):668–673. doi: 10.2519/jospt.2008.2820. [DOI] [PubMed] [Google Scholar]
- 84.Van Dillen L.R., Norton B.J., Sahrmann S.A. Efficacy of classification-specific treatment and adherence on outcomes in people with chronic low back pain. A one-year follow-up, prospective, randomized, controlled clinical trial. Man Ther. 2016;24(August):52–64. doi: 10.1016/j.math.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Harris-Hayes M., Holtzman G.W., Earley J.A., Van Dillen L.R. Development and preliminary reliability testing of an assessment of patient independence in performing a treatment program: standardized scenarios. J Rehabil Med. 2010;42(March (3)):221–227. doi: 10.2340/16501977-0505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Caldwell C., Sahrmann S., Van Dillen L. Use of a movement system impairment diagnosis for physical therapy in the management of a patient with shoulder pain. J Orthop Sports Phys Ther. 2007;37(9):551–563. doi: 10.2519/jospt.2007.2283. [DOI] [PubMed] [Google Scholar]
- 87.Harris-Hayes M., Sahrmann S.A., Norton B.J., Salsich G.B. Diagnosis and management of a patient with knee pain using the movement system impairment classification system. J Orthop Sports Phys Ther. 2008;38(4):203–213. doi: 10.2519/jospt.2008.2584. [DOI] [PubMed] [Google Scholar]
- 88.Hoffman S.L., Johnson M.B., Zou D., Harris-Hayes M., Van Dillen L.R. Effect of classification-specific treatment on lumbopelvic motion during hip rotation in people with low back pain. Man Ther. 2011;16(August (4)):344–350. doi: 10.1016/j.math.2010.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McDonnell M.K., Sahrmann S.A., Van Dillen L. A specific exercise program and modification of postural alignment for treatment of cervicogenic headache: a case report. J Orthop Sports Phys Ther. 2005;35(January (1)):3–15. doi: 10.2519/jospt.2005.35.1.3. [DOI] [PubMed] [Google Scholar]
- 90.Spitznagle T.M., Sahrmann S. Diagnosis and treatment of 2 adolescent female athletes with transient abdominal pain during running. J Sport Rehabil. 2011;20(May (2)):228–249. doi: 10.1123/jsr.20.2.228. [DOI] [PubMed] [Google Scholar]
- 91.Harris-Hayes M., Czuppon S., Van Dillen L.R. Movement-pattern training to improve function in people with chronic hip joint pain: a feasibility randomized clinical trial. J Orthop Sports Phys Ther. 2016;46(June (6)):452–461. doi: 10.2519/jospt.2016.6279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Azevedo D.C., Van Dillen L.R., Santos Hde O., Oliveira D.R., Ferreira P.H., Costa L.O. Movement system impairment-based classification versus general exercise for chronic low back pain: protocol of a randomized controlled trial. Phys Ther. 2015;95(September (9)):1287–1294. doi: 10.2522/ptj.20140555. [DOI] [PubMed] [Google Scholar]