Abstract
Background
Lower urinary tract symptoms (LUTSs) due to benign prostatic hyperplasia (BPH) are common conditions in middle-age or older men. The International Prostate Symptom Score (IPSS) is a useful and validated questionnaire to evaluate LUTS secondary to BPH. Van der Walt et al have developed an alternative questionnaire named the Visual Prostate Symptom Score (VPSS) questionnaire. This study aimed to evaluate the relationship between the VPSS and IPSS in the evaluation of men with LUTSs due to BPH in an Indian population.
Materials and methods
This was a prospectively designed study conducted at Sri Sathya Sai Institute of Higher Medical Sciences, Prashanthigram (Anantapur, Andhra Pradesh, India). A total of 121 patients who presented to the urology outpatient department with LUTS due to BPH were enrolled in the study. Patients were followed up at 1-month and 3-month intervals. All patients were given both questionnaires. The correlation test was used to assess the correlation between two symptom scores and various parameters. Observations with a P value < 0.05 were considered statistically significant.
Results
There was a statistically significant difference in the number of patients requiring assistance to fill the questionnaires according to their education level. There was a positive correlation between IPSS total score and VPSS total score (r = 0.7235; P < 0.0001), VPSS total score and VPSS quality of life (Qol; r = 0.70753; p < 0.0001), IPSS total versus IPSS Qol (r = 0.65583; P < 0.0001), and IPSS Qol versus VPSS Qol (r = 0.84093; P < 0.0001). A negative correlation was observed between total VPSS with Qmax, total IPSS with Qmax, IPSS total versus Qavg (r = −0.479; P < 0.0001), and VPSS total versus Qavg (r = −0.5; P < 0.0001). All VPSS questions showed statistically significant correlation with the corresponding IPSS questions.
Conclusion
There is a statistically significant correlation between the VPSS and IPSS and it can be completed by a greater number of patients without assistance.
Keywords: Benign prostate hyperplasia, International Prostate Symptom Score, Lower urinary tract symptoms, Visual Prostate Symptom Score
1. Introduction
Lower urinary tract symptoms (LUTSs) due to benign prostatic hyperplasia (BPH) are common conditions in middle-age or older men.1 The International Prostate Symptom Score (IPSS) is a useful and validated questionnaire to evaluate LUTS secondary to BPH.2 Thus, it has become a very useful tool for urologists in day-to-day practice for evaluation and follow-up of patients with LUTS. However, most patients with a low education level are not able to answer the IPSS questionnaire correctly.3 Furthermore, BPH incidence increases more after 50 years of age. In this age group, most men experience eyesight-related problems and/or cognitive impairment.4 Because of all these reasons, patients usually have to take assistance from the medical fraternity, however, this may lead to bias in patient's responses.5
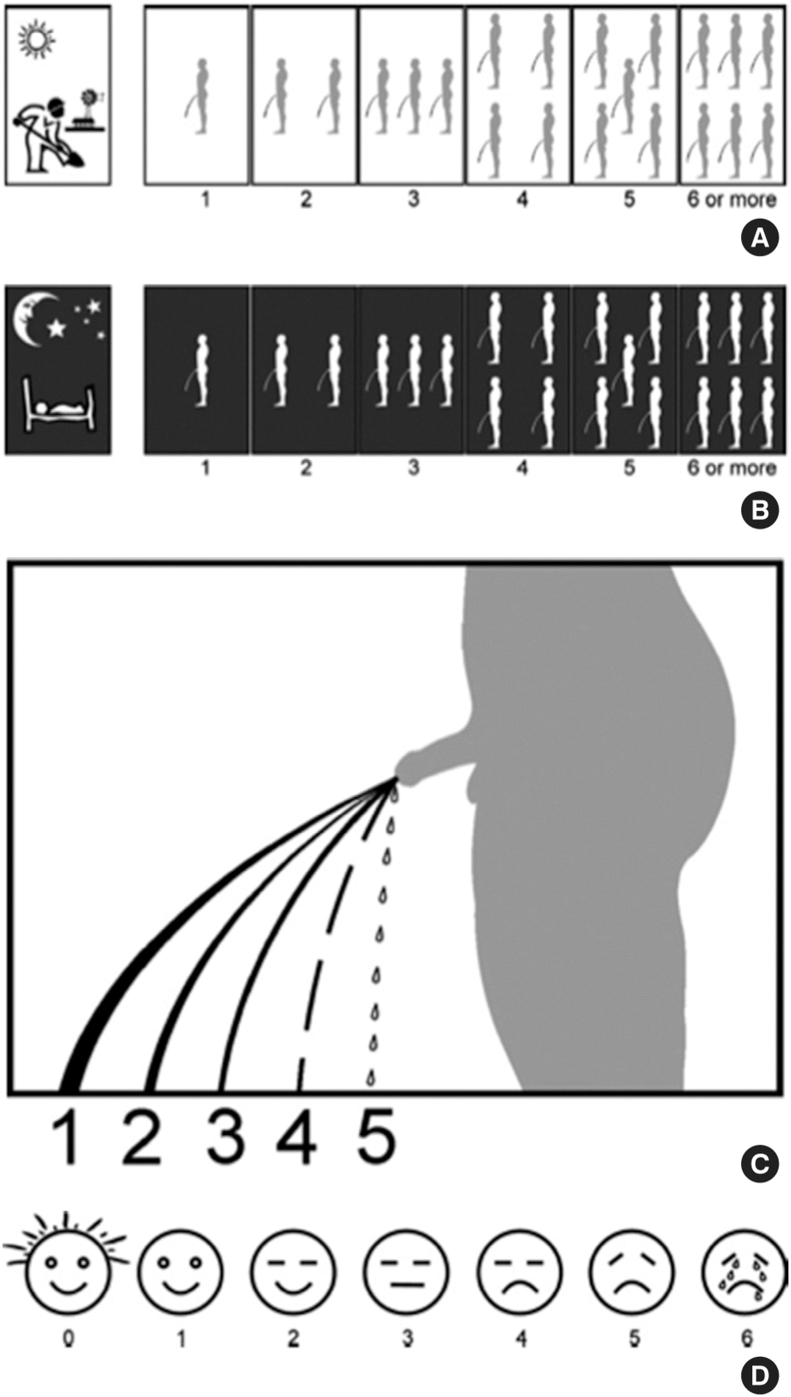
To avoid the aforementioned problems when using the IPSS, Van der Walt et al6 have developed an alternative questionnaire named “Visual Prostate Symptom Score (VPSS),” which assesses frequency, nocturia, and weak stream and quality of life (Qol) by means of pictograms.
There are many advantages in using the VPSS. It is easy to understand and simple to use even for elderly and less-educated persons.7 Various studies have been conducted in Turkish, Indonesian, South African, and Korean populations to assess its usefulness. However, limited data are available about its usefulness and applicability in Indian population.8, 9, 10, 11
2. Materials and methods
This was a prospectively designed study conducted at Sri Sathya Sai Institute of Higher Medical Sciences, Prashanthigram (Anantapur, Andhra Pradesh, India). Sri Sathya Sai Institute is a tertiary care center with daily outpatient visits of around 150–160 patients. Ethical committee approval was sought for the study according to our institute's protocol. The study was conducted from March 2016 to September 2016. A total number of 121 patients who presented to the urology outpatient department with LUTS due to BPH were enrolled in the study.
The study inclusion criteria were as follows: all patients who presented to the urology outpatient clinic with LUTSs and aged > 40 years. The exclusion criteria included the following cases: patients with uncontrolled diabetes (prostate-specific antigen > 4 ng/dL); patients with a history of transurethral resection of the prostate; patients that underwent surgery for urethral vesical calculus in the past; and patients, on evaluation, found to have LUTS due to a cause other than BPH.
Patients were followed up at 1-month and 3-month intervals. All patients were evaluated and after routine investigations, they were given both the IPSS and VPSS questionnaires. Uroflowmetry, serum prostate-specific antigen, renal function tests, and ultrasonography for prostate were done. Various parameters including the total scores, uroflowmetry parameters, age, education level, and assistance required to fill the questionnaires were noted and compared using chi-square test. The correlation test was used to assess correlation between two symptom scores and various parameters. Observations with a P value < 0.05 were considered statistically significant.
3. Results
The characteristics of the patients included in this study are presented in Table 1. The patients' mean age was 66 years (range, 44–79 years). All patients were divided into two groups based on their education level. Patients with education level < 9th standard were included in Group A and those with education level > 9th standard in Group B. Around 55% of patients had education level < 9th standard.
Table 1.
Patients characteristics.
| Characteristics | Value |
|---|---|
| Age (yr) | 66 (44–79) |
| Education level | |
| Grade < 9th (Group A) | 60/110 (54.5) |
| Grade > 9th (Group B) | 50/110 (45.5) |
A greater proportion of patients could complete the VPSS questionnaire without assistance compared with the IPSS questionnaire. In Group A (education level < 9th), the VPSS questionnaire was completed without assistance by 44 of 60 patients, whereas only 12 of 60 patients could complete the IPSS questionnaire without assistance (Table 2).
Table 2.
Relationship between education level and requirement of assistance to complete the questionnaires.
| Group | VPSS assistance | IPSS assistance | P |
|---|---|---|---|
| Group A < 9th | 16/60 | 48/60 | <0.0001 |
| Group B > 9th | 5/50 | 14/50 | <0.0001 |
IPSS, International Prostate Symptom Score; VPSS, Visual Prostate Symptom Score.
In Group B (education level > 9th), the VPSS questionnaire was completed without assistance by 45 of 50 patients, whereas only 36 of 50 patients could complete the IPSS questionnaire without assistance. This difference was found to be statistically significant (P < 0.0001).
There was a significant difference in time taken by the patients to fill the VPSS versus the IPSS questionnaire and this was found to be statistically significant (P < 0.0001) as shown in Table 3.
Table 3.
Average time taken to fill the questionnaires.
| Questionnaires | Time taken (sec) | P |
|---|---|---|
| VPSS | 166 (30–480) | <0.0001 |
| IPSS | 283 (90–600) |
IPSS, International Prostate Symptom Score; VPSS, Visual Prostate Symptom Score.
Both the questionnaires were evaluated for correlation. All the results are summarized in Table 4.
Table 4.
Correlation between various VPSS and IPSS parameters recorded in the study.
| Group | Correlation coefficient (r) | P |
|---|---|---|
| IPSS total vs. VPSS total | 0.7235 | <0.0001 |
| IPSS total vs. Qmax | −0.6287 | <0.0001 |
| VPSS total vs. Qmax | −0.5782 | <0.0001 |
| IPSS total vs. Qavg | −0.479 | <0.0001 |
| VPSS total vs. Qavg | −0.5 | <0.0001 |
| VPSS total vs. VPSS Qol | 0.70753 | <0.0001 |
| IPSS total vs. IPSS Qol | 0.65583 | <0.0001 |
| IPSS Qol vs. VPSS Qol | 0.84093 | <0.0001 |
| Frequency: VPSS Q1 vs. IPSS Q2 | 0.5083 | <0.0001 |
| Nocturia: VPSS Q2 vs. IPSS Q7 | 0.88558 | <0.0001 |
| Poor stream: VPSS Q3 vs. IPSS Q5 | 0.76122 | <0.0001 |
| Poor stream: IPSS Q5 vs. Qmax | −0.7134 | <0.0001 |
| Poor stream: VPSS Q3 vs. Qmax | −0.7533 | <0.0001 |
IPSS, International Prostate Symptom Score; VPSS, Visual Prostate Symptom Score.
There was a positive correlation between IPSS total score and VPSS total score (r = 0.7235; P < 0.0001). Similarly, a positive correlation was observed between VPSS total score and VPSS Qol (r = 0.70753; P < 0.0001), IPSS total versus IPSS Qol (r = 0.65583; P < 0.0001), and IPSS Qol versus VPSS Qol (r = 0.84093; P < 0.0001). Both total VPSS and total IPSS showed a negative correlation with Qmax: IPSS total versus Qmax (r = −0.6287; P < 0.0001) and VPSS total versus Qmax (r = −0.5782; P < 0.0001). Similarly, a negative correlation was observed between IPSS total versus Qavg (r = −0.479; P < 0.0001) and VPSS total versus Qavg (r = −0.5; P < 0.0001). All VPSS questions showed statistically significant correlation with the corresponding IPSS questions: poor stream, VPSS Q3 versus IPSS Q5 (r = 0.76122; P < 0.0001); nocturia, VPSS Q2 versus IPSS Q7 (r = 0.88558; P < 0.0001); and frequency, VPSS Q1 versus IPSS Q2 (r = 0.5083; P < 0.0001).
4. Discussion
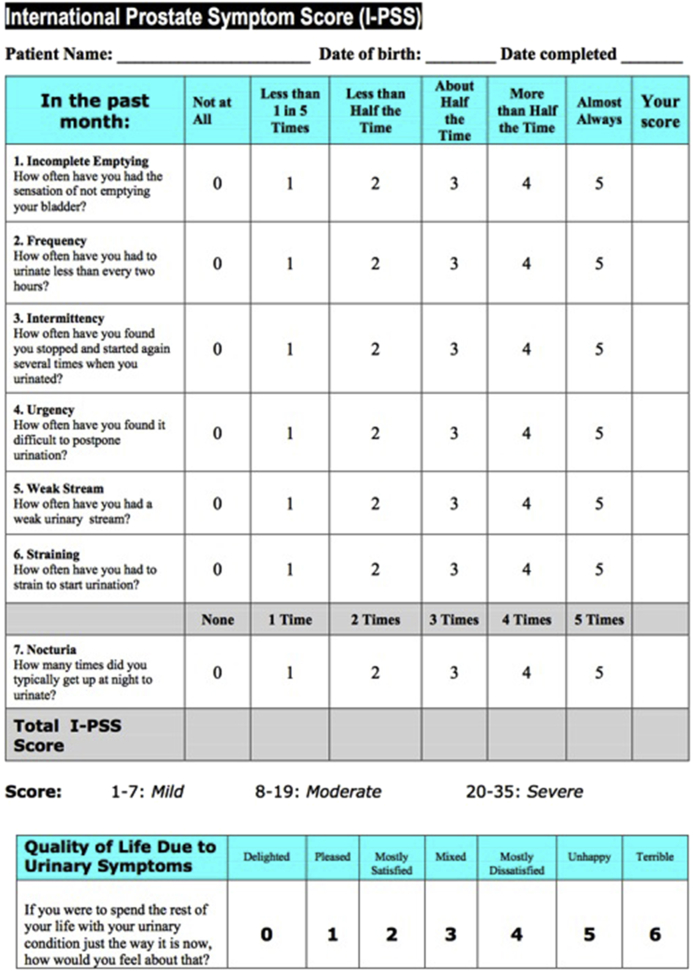
In this study, we attempted to evaluate the relationship between the VPSS (Fig. 1) and IPSS (Fig. 2) in Indian population.
Fig. 1.
Visual Prostate Symptom Score questionnaire.
Fig. 2.
International Prostate Symptom Score questionnaire.
The IPSS questionnaire has seven questions, which are used to evaluate storage and voiding symptoms in patients with BPH. The patient is given five options for the first seven questions and each option indicates severity of that symptom. The total score ranges from 0 to 35 and LUTSs are classified as mild to severe depending on the total score. Patients having a total score ≤7 are classified as having mild symptoms, scores from 8 to 19 are classified as moderate symptoms, and symptom scores ≥20 are classified as severe symptoms.12 The last question of the IPSS is about Qol. Studies have shown that this question is the single best predictor of outcome related to treatment prescribed.13
One of the major problems associated with the IPSS questionnaire is its complex nature. Rodrigues et al14 showed that almost 50% of the patients were unable to complete the IPSS questionnaire when they were given the freedom to not answer any question that they are not clear about. Another study by Luján Galán et al15 confirmed these findings. They found that around 33% of patients could not complete the IPSS questionnaire.
Cam et al16 in their study found that 34% of patients with a low (elementary school) educational level did not even fill the IPSS questionnaire and returned them totally unmarked. Van der Walt et al6 observed that 87% of patients with an education level ≤ 7th grade required assistance to complete the IPSS questionnaire compared with 24% of patients with an education level ≥ 10th grade. In this study, it was clear that patients with education level ≤ 9th require more assistance for completing the IPSS questionnaire.
There have been previous studies from Namibia, Turkish society, Korean populations, and Indonesian populations that have evaluated the correlation between the IPSS and VPSS.8, 9, 10, 11
They all found a positive correlation between IPSS total score and VPSS total score. Similarly, a positive correlation was observed between VPSS total score and VPSS Qol, IPSS total versus IPSS Qol, and IPSS Qol versus VPSS Qol. Both total VPSS and total IPSS showed a negative correlation with Qmax. Similarly, a negative correlation was observed between IPSS total versus Qavg and VPSS total versus Qavg. All VPSS questions showed a statistically significant correlation with the corresponding IPSS questions: poor stream, VPSS Q3 versus IPSS Q5; nocturia, VPSS Q2 versus IPSS Q7; and frequency, VPSS Q1 versus IPSS Q2. Our results were found to be consistent with all these studies.
4.1. Study limitations and importance
Because this study included data from a single institution, a potential selection bias may have occurred. Nevertheless, our study results are valuable because limited data are available from rural Indian populations to elucidate an association between the VPSS and IPSS.
4.2. Conclusion and take home message
There is a statistically significant correlation between VPSS and IPSS, and it can be completed by a greater number of patients without assistance. The VPSS can be a useful tool to evaluate the severity of symptoms in patients presenting with LUTS due to BPH even with low education level.
Conflicts of interest
None.
References
- 1.Cornu J.N., Cussenot O., Haab F., Lukacs B. A widespread population study of actual medical management of lower urinary tract symptoms related to benign prostatic hyperplasia across Europe and beyond official clinical guidelines. Eur Urol. 2010;58:450–456. doi: 10.1016/j.eururo.2010.05.045. [DOI] [PubMed] [Google Scholar]
- 2.Barry M.J., Fowler F.J., Jr., O'Leary M.P., Bruskewitz R.C., Holtgrewe H.L., Mebust W.K. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148:1549–1557. doi: 10.1016/s0022-5347(17)36966-5. [DOI] [PubMed] [Google Scholar]
- 3.Netto N.R., Jr., de Lima M.L. The influence of patient education level on the International Prostatic Symptom Score. J Urol. 1995;154:97–99. doi: 10.1097/00005392-199507000-00034. [DOI] [PubMed] [Google Scholar]
- 4.Huh J.S., Kim Y.J., Kim S.D. Prevalence of benign prostatic hyperplasia on Jeju Island: analysis from a cross-sectional community-based survey. World J Mens Health. 2012;30:131–137. doi: 10.5534/wjmh.2012.30.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cam K. BPH: how useful is a Visual Prostate Symptom Score for patients? Nat Rev Urol. 2011;8:536–537. doi: 10.1038/nrurol.2011.137. [DOI] [PubMed] [Google Scholar]
- 6.Van der Walt C.L., Heyns C.F., Groeneveld A.E., Edlin R.S., van Vuuren S.P. Prospective comparison of a new Visual Prostate Symptom Score versus the International Prostatic Symptom Score in men with lower urinary tract symptoms. Urology. 2011;78:17–20. doi: 10.1016/j.urology.2011.01.065. [DOI] [PubMed] [Google Scholar]
- 7.Heyns C.F., van der Walt C.L., Groeneveld A.E. Correlation between a new Visual Prostate Symptom Score (VPSS) and uroflowmetry parameters in men with lower urinary tract symptoms. S Afr Med J. 2012;102:237–240. [PubMed] [Google Scholar]
- 8.Ceylan Y., Gunlusoy B., Degirmenci T., Kozacioglu Z., Bolat D., Minareci S. Is new Visual Prostate Symptom Score useful as International Prostate Symptom Score in the evaluation of men with lower urinary tract symptoms? a prospective comparison of 2 symptom scores in Turkish society. Urology. 2015;85:653–657. doi: 10.1016/j.urology.2014.10.057. [DOI] [PubMed] [Google Scholar]
- 9.Afriansyah A., Gani Y.I., Nusali H. Comparison between Visual Prostate Symptom Score and International Prostate Symptom Score in males older than 40 years in rural Indonesia. Prostate Int. 2014;2:176–181. doi: 10.12954/PI.14059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heyns C.F., Steenkamp B.A., Chiswo J., Stellmacher G.A., Fortsch H.E., Van der Merwe A. Evaluation of the Visual Prostate Symptom Score in a male population with great language diversity and limited education: a study from Namibia. S Afr Med J. 2014;104:353–357. doi: 10.7196/samj.7917. [DOI] [PubMed] [Google Scholar]
- 11.Park Y.W., Lee J.H. Correlation between the Visual Prostate Symptom Score and International Prostate Symptom Score in patients with lower urinary tract symptoms. Int Neurourol J. 2014;18:37–41. doi: 10.5213/inj.2014.18.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reohrborn G.C. Benign prostatic hyperplasia: etiology, pathophysiology, epidemiology, and natural history. In: Wein A.J., Kavaoussi L.R., Novick A.C., Partin A.W., Peters C.A., editors. Campbell-Wash urology. 10th ed. Saunders Elsevier; Philadelphia: 2012. pp. 2576–2581. [Google Scholar]
- 13.Barry M.J., Girman C.J., O'Leary M.P., Walker-Corkery E.S., Binkowitz B.S., Cockett A.T. Using repeated measures of symptom score, uroflowmetry and prostate-specific antigen in the clinical management of prostate disease. Benign Prostatic Hyperplasia Treatment Outcomes Study Group. J Urol. 1995;153:99–103. doi: 10.1097/00005392-199501000-00036. [DOI] [PubMed] [Google Scholar]
- 14.Rodrigues N.N., Jr., de Lima M.L., de Andrade E.F., Apuzzo F., da Silva M.B., Davidzon I.M. Latin American study on patient acceptance of the International Prostate Symptom Score (IPSS) in the evaluation of symptomatic benign prostatic hyperplasia. Urology. 1997;49:46–49. doi: 10.1016/s0090-4295(96)00372-x. [DOI] [PubMed] [Google Scholar]
- 15.Luján Galán M., Páez Borda A., Martín Osés E., Llanes González L., Berenguer Sánchez A. The validity of the IPSS questionnaire in a sample of 262 patients with benign prostatic hyperplasia. Arch Esp Urol. 1997;50:847–853. [Article in Spanish] [PubMed] [Google Scholar]
- 16.Cam K., Senel F., Akman Y., Erol A. The efficacy of an abbreviated model of the International Prostate Symptom Score in evaluating benign prostatic hyperplasia. BJU Int. 2003;91:186–189. doi: 10.1046/j.1464-410x.2003.04055.x. [DOI] [PubMed] [Google Scholar]