Abstract
Background
Global research suggests that persons with disabilities face barriers when accessing health care services. Yet, information regarding the nature of these barriers, especially in low-income and middle-income countries is sparse. Rural contexts in these countries may present greater barriers than urban contexts, but little is known about access issues in such contexts. There is a paucity of research in South Africa looking at “triple vulnerability” – poverty, disability and rurality. This study explored issues of access to health care for persons with disabilities in an impoverished rural area in South Africa.
Methods
The study includes a quantitative survey with interviews with 773 participants in 527 households. Comparisons in terms of access to health care between persons with disabilities and persons with no disabilities were explored. The approach to data analysis included quantitative data analysis using descriptive and inferential statistics. Frequency and cross tabulation, comparing and contrasting the frequency of different phenomena between persons with disabilities and persons with no disabilities, were used. Chi-square tests and Analysis of Variance tests were then incorporated into the analysis.
Results
Persons with disabilities have a higher rate of unmet health needs as compared to non-disabled. In rural Madwaleni in South Africa, persons with disabilities faced significantly more barriers to accessing health care compared to persons without disabilities. Barriers increased with disability severity and was reduced with increasing level of education, living in a household without disabled members and with age.
Conclusions
This study has shown that access to health care in a rural area in South Africa for persons with disabilities is more of an issue than for persons without disabilities in that they face more barriers. Implications are that we need to look beyond the medical issues of disability and address social and inclusion issues as well.
Keywords: Disability, Rural, Health, Access, South Africa
Background
The United Nation’s Convention on the Rights of Persons with Disabilities (UNCRPD) is a human rights instrument on an international level intended to protect persons with disabilities’ dignity and rights. Eight guiding principles underlie the Convention, of which accessibility is one [1]. While access to health care is a major health issue [2], compromised access affects the performance of health care systems globally [3]. Health care needs that are not met and that exacerbate health disparities are experienced disproportionately by persons with disabilities [4]. Inequity in accessing health care for persons with disabilities is a global issue – in general, persons with disabilities have poorer health care access [5]. Political marginalisation, discrimination and inequitable access to health services are experienced by persons with disabilities resulting in poorer health outcomes [6].
According to Tomlinson et al. [7] and confirmed by the World Report on Disability [8], there is international evidence that persons with disabilities across the globe face distinctive barriers when accessing health care services, and show poorer health outcomes than nondisabled persons. Contemporary evidence continues to support the view that persons with disabilities have less access to health care [9–11]. Despite their frequent additional health care needs and limited access, persons with disabilities constitute a marginalised group in health services research. Their experiences within the health care system are not well understood, and research-based health service improvement interventions commonly exclude persons with disabilities [12].
This paper attempts to add to the health services research in exploring access to health care for persons with disabilities in a rural low-income context in South Africa.
Disability and access to health care in low-income contexts
The majority of individuals with disability live in low-income contexts [8]. Recently, there has been an accumulation of evidence that barriers to health care access exist for persons with disabilities in less resourced countries. According to MacLachlan and Mannan [13], access to health care, even in wealthy countries, is often difficult for persons with disabilities, but in poorer countries the challenges are exacerbated, combining physical, financial, and attitudinal components. The EquitAble Project (see www.sintef.no/en/projects/equitable/) has documented a number of barriers to health care experienced by persons with disabilities in resource-poor settings in Africa [14–17].
Rural access to health services
Concern over the availability of health services in rural areas has existed for decades [18] and “rural communities have long struggled to maintain access to quality health care services” [19] (p. 1). However, it is not enough, by itself, that a system of primary care be available in rural areas – the services must also be accessible [20]. One would expect that rural populations have reduced access to health care services compared to their urban counterparts, but according to Sibley and Weiner [21], studies have been contradictory and inconclusive.
Bourke, Humphreys, Wakerman, and Taylor [22] show that persons living in rural and remote areas face multiple challenges in accessing appropriate health services. These barriers to health care for the rural population have been well documented [23–27]. Rural communities share certain characteristics that affect both health and health care [28] and “do without ready access to the dense net of services – including health services – that characterises the urban environments” (p. 3). According to Rowland & Lyons (1989, cited in Schur & Franco) [29] (p. 25), some key characteristics for rural areas are:
poorly developed and fragile health infrastructures;
high prevalence rates for chronic illness and disability;
socioeconomic hardships; and
physical barriers such as distance and availability of transportation, including a lack of public transportation.
Access to quality health services becomes the single biggest issue, if not the defining issue, in rural health [30].
Disability and access to health care among the poor rural populations has received little attention. There is scarce data on their health needs [31]. What little literature there is suggests that persons with disabilities in rural areas have more problems and issues regarding their health care than persons with no disabilities in rural areas – especially when it comes to health care access [31].
Disability in rural communities in South Africa
The right to access health care services in South Africa is guaranteed by Section 27 of the Constitution, but considerable inequities still remain, largely due to discrepancies in resource allocation [32, 33]. In their study on access to health care in South Africa, Harris et al. [34] concur with previous South Africa studies, confirming that poor, uninsured, Black Africans and rural groups have poorer access to health care than do other members of South African society [32, 33, 35, 36]. Only a few studies have looked at disability issues in rural South Africa [14, 37–40]. These studies focused specifically on disability and access to health care. More large scale quantitative research contributing to assessing and improving access to health care for persons with disabilities needs to be prioritised – especially in South African rural areas.
This study forms part of a larger Equitable study (www.sintef.no/en/projects/equitable/). The aim of this study was to compare persons with disabilities and persons with no disabilities in terms of access to health care in a rural impoverished area in South Africa. While international literature brings support to the existence of access barriers and inequitable health services, evidence is still limited when it comes to equal access for persons with disabilities. Based on the above literature on health disparities and access to health care, this article aims to reveal and compare specific access barriers in a rural context. The hypothesis is that persons with disabilities have poorer access to health care in a rural impoverished area in South Africa.
Methods
Context of study
Madwaleni is the third largest rural population in South Africa [41] with a 62% rural population. It is a deeply rural and impoverished area of the Eastern Cape Province, 220 km up the coast from East London, 100 km from Mthatha, 30 km from Elliotdale and 16 km from the Wild Coast. The Madwaleni area is situated in the rolling hills of the Amatole District within the Mbashe Municipality. This rural area is defined by poor infrastructure, lack of basic service provision, low levels of literacy, high levels of unemployment, limited access to health care and education, high incidence of communicable diseases and high mortality rates (Watermeyer & Barratt 2013, cited in Neille and Penn) [37].
Sample of study
The sample in this observational cross-sectional study comprised of 773 individuals – 322 persons with disability and 451 controls (without disability) – covering 527 households. Children under the age of five were excluded from the sample. The age range was from 5 to 97. We used purposive sampling to first select four health centres surrounding the hospital, then random sampling to select the villages surrounding the health centres, and finally systematic sampling to select the households within the villages. Household questionnaires were administered with the head of the household to ascertain if the household had a person with a disability or not. Disability was defined by using the Washington Group Questions (WGQ) on Disability, wherein if an individual has “some difficulty” with two or more of the six questions, or has “a lot of difficulty” or is “unable to do” for one or more questions, they may be categorised as a person with activity or functional limitations, and categorised as “disabled”. Further details of the sampling and categorisation of participants have been reported by Eide et al. [42].
The Household questionnaire is a questionnaire administered to the head of the household in each household (after consent forms were completed). The Household questionnaire ascertained the composition of the household, i.e., the members of the household, and whether or not they had a disability using the Washington Group (WG) Questions on disability. If a person with a disability was identified in the household, then that person completed consent forms (relevant to age of persons; for example, Adult Consent Forms, Children Consent with parents and guardians forms and Assent Forms for children 15–17) and was also interviewed using the questionnaire for persons with disabilities. This questionnaire focused particularly on health and access to health care. If there were more than one person with a disability in a particular household, the person with the most severe disability was interviewed. This was ascertained by the disability rating scale in the household questionnaire where a higher total disability score according to the Washington Group method depicted more severe disability. This questionnaire focused particularly on health and access to health care. A third interview (after completion of consent forms) was carried out in the same household with a person without disability (in-house controls) matched to the person with disability by age (5 year latitude either way) and gender using a Control questionnaire. This questionnaire is a shortened version of the one administered to individuals with disability. If no matched non-disabled control was found in the household, no control interview was carried out in that household. If the household did not have a person with disability living in the house then this household became a neighbourhood control household. The head of the household would complete the Household questionnaire and a randomly selected person (using random tables) in the control household would complete the control questionnaire (neighbourhood controls). The sample used in the study was not a representative sample of the population. Characteristics of the Head of Household in this sample is that 66% of households were headed by women with an average age of 56 years. The average age for men-headed households was 55 years. Of the 532 households, there were 112 only case households, 175 only control households and 245 case and control households.
Measures
Disability was defined by using the six questions developed by the Washington Group Questions on Disability [43]. The questions cover six domains: difficulty in hearing, seeing, walking, remembering, self-care and communicating. Answer alternatives are: i) no difficulty (0), ii) some difficulty (1), iii) a lot of difficulty (2), and iv) cannot do at all (3). For the purpose of this study, the six questions were added together to form a disability scale ranging from 0 (no difficulty in any of the six domains) to 18 (cannot do in all six domains). The scale had a mean value of 1.66 and standard deviation 2.27.
An asset scale was utilised to construct a measure on socio-economic status (SES). The respondents answered “yes” (1) or “no” (0) to the presence of 28 common items in the household, and the items were added together to form the asset scale. Range of the scale was then 0–28, mean value 3.52 and standard deviation 3.02.
Instruments
Interviews using three questionnaires, depending on circumstances, were used in the study:
A Household questionnaire, comprising socio-demographic and socio-economic variables.
A Questionnaire for a person with a disability, with a range of disability relevant variables including questions on functional difficulties and access to services.
A Control questionnaire, which is a shortened version (in that there were no questions on assistive devices) of the questionnaire for persons with disability.
The survey questionnaires that were originally in English were translated into isiXhosa and back-translated to make them appropriate for the study site and its community members. The 17 data collectors/interviewers made use of cell phone technology and the translated questionnaires were programmed into the cell phone according to methods described by Tomlinson et al. [7]. The data capturing was recorded directly into the cell phone and these data were then sent to a central data base where it was collated and analysed. This method provided more accurate data, minimal missing data, was easier to monitor locally and remotely, and had built-in quality checks.
The approach to data analysis included quantitative data analysis using descriptive and inferential statistics. Frequency and cross tabulation, comparing and contrasting the frequency of different phenomena between persons with disabilities and persons with no disabilities, were used. Chi-square test, bi-variate and multivariate linear regressions were used to analyse the difference in barriers experienced by persons with and without disabilities.
Results
Table 1 illustrates the sample characteristics of the study.
Table 1.
Sample characteristics
| Variables | N | % |
|---|---|---|
| Age: | ||
| 5–17 | 49 | 6.3 |
| 18–60 | 548 | 70.9 |
| 61 and over | 176 | 22.8 |
| Total | 773 | 100.0 |
| Gender: | ||
| Male | 209 | 27.0 |
| Female | 512 | 66.2 |
| Missing data | 52 | 6.8 |
| Total | 773 | 100.0 |
| Education level (18+): | ||
| No formal education | 162 | 31.5% |
| Less than primary school | 244 | 47.5% |
| Primary school | 87 | 16.9% |
| Secondary school | 18 | 3.5% |
| Tertiary level education | 3 | 0.6% |
The mean age for persons with disabilities was 54 years and persons without disabilities 33 years.
A higher percentage of persons with disabilities encountered barriers to accessing health care on a weekly and monthly basis. Of persons with no disabilities, 79.6% never had barriers to health care access compared to 70.8% of persons with disabilities (Table 2) (χ2 = 32.17, p < 0.001).
Table 2.
How often has the availability of health care services and medical care been a problem for you? (N = 772)
| No disability | Disability | ||
|---|---|---|---|
| Barriers to Health Care | Never/not applicable | 79.6% (312) | 70.8% (267) |
| Less than monthly | 11.0 (43) | 12.1 (46) | |
| Monthly | 0.5% (2) | 4.5% (17) | |
| Weekly | 2.0% (8) | 8.4% (17) | |
| Daily | 6.9% (27) | 4.2% (16) |
Of persons with disabilities, 24.4% report that they did not get health services the last time they needed it, while the corresponding figure for non-disabled is 12.6% (χ2 = 17.77, p < .001).
Participants (n = 773) were given a list of 18 potential access barriers that they were asked to rate with response options of “No Problem” (score 1), “Small Problem” (score 2), “Moderate Problem” (score 3), “Serious Problem” (score 4) or “Insurmountable Problem” (score 5).
In Fig. 1, the combined figures for “serious problems” and “insurmountable problems” are shown for both persons with and without disabilities. For all 18 items, more persons with than without disabilities report that the respective items are reasons for serious or insurmountable problems in accessing health care services.
Fig. 1.
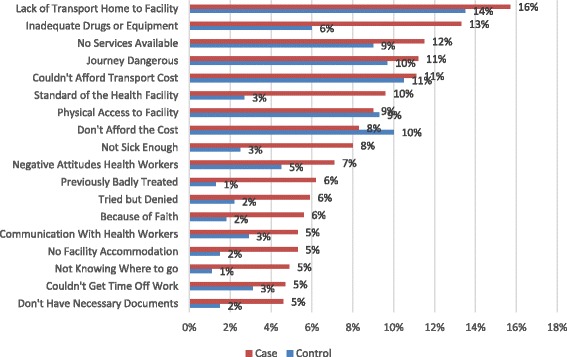
Access to Health Care-Madwaleni
The 18 items were subject to scale analyses (Alpha = 0.90). A principal component analyses gave support to a one-factor solution. The 18 items were then added together to form a “Barrier to health services” scale (range 18–62, mean value: 21.88, st.dev. 7.25). Mean value on the scale was 23.37 for persons with disabilities and 20.49 for non-disabled (F = 31.19, p < .001), indicating more experienced barriers among persons with disabilities.
Socio-economic status (SES) was measured by means of an Asset scale comprising 28 household items (1 = possess, 0 = do not possess) that were added together. In the Madwaleni sub-sample, minimum and maximum values on the scale ranged from 0 and 16, mean value 3.52 and standard deviation 3.02. Mean value among households with disabled persons was 3.70 and 3.33 among non-disabled households (F = 3.03, p = .08).
Mean number of household members was 4.4, and 4.6 and 4.3 in households with and without disabled members respectively (F = 3.21, p = .07).
A variable on household type (1 = have a disabled member, 2 = have no disabled member was included to control for household effect of disability.
The Washington Group 6 questions were used as an indicator of disability severity. All six items were added together, ranging from 6 to 24, mean value 7.7, standard deviation 2.27.
Time to get to health facility was registered by hours and minutes and ranged from 1 min to 20 h.
The bi-variate regressions (see Table 3) show that barriers to accessing health care services increase with age and severity of disability (score on WG 6), and reduce with increasing level of education and (near significant) with increasing number of members in the household. Further, being in a household without disabled members (household type) is associated with reduced barriers. No difference between males and females was revealed. The strongest association is the positive association between disability (WG 6) and barriers, closely followed by household type. Out of the six different items included in the Washington group questions used to determine disability, difficulties with seeing, hearing. Walking and remembering were all positively associated with increased barriers, while no association was found for difficulties with self-care and communication.
Table 3.
Bivariate regressions on Barriers to health services (N = 762)
| Variable | Beta | t | p |
|---|---|---|---|
| Age | 0.08 | 2.13 | <. 05 |
| Sex | 0.06 | 1.67 | n.s. |
| Level of education | - 0.12 | - 3.11 | < .001 |
| SES | - 0.42 | - 1.15 | n.s. |
| Disability (WG6 scale) | 0.17 | 4.60 | < .001 |
| Type of household (1 = with disabled members, 2 = without disabled members) | - 0.16 | - 4.32 | < .001 |
| Number of members in the household | - .07 | - 1.82 | .07 |
| Difficulty (1–4) | |||
| Seeing | 0.13 | 3.62 | < .001 |
| Hearing | 0.14 | 3.93 | < .001 |
| Walking | 0.12 | 3.26 | < .001 |
| Remembering | 0.13 | 3.62 | < .001 |
| Self-care | 0.04 | 1.18 | n.s. |
| Communicating | 0.03 | 0.88 | n.s. |
In the multivariate model (see Table 4), the strongest predictors for reduced barriers to health services are type of household (with and without disabled members) and level of education. Belonging to a household without disabled member (s) and higher level of education reduce barriers. Increased disability severity and being female are associated with higher levels of barriers. Socio-economic status and number of household members remains non-significant . R2 for the entire model in 0.045.
Table 4.
Multivariate regression of disability status, age, sex and level of education on barriers for accessing health services (N = 709)a
| Variable | Beta | t | P |
|---|---|---|---|
| Age | - 0.08 | - 1.79 | .07 |
| Sex | 0.08 | 2.02 | < .05n.s. |
| Level of education | - 0.09 | - 2.24 | < .05 |
| Type of household (1 = with disabled members, 2 = without) | - .11 | - 2.35 | < .05 |
| Disability () (WG6) | 0.09 | 2.7 | < .05 |
| Total number in household | - .05 | - 1.43 | n.s. |
| SES | - .00 | - .02 | n.s. |
aR 2 = 0.045
Comparing the specific difficulties, we found the highest figure for not getting health care the last time it was needed among persons with difficulties hearing (31.3%), followed by seeing difficulties (28.1%), walking difficulties (28.0%), difficulties with remembering (21.7%) and with self care (21.7%). For these difficulties significant differences were found between persons with and without the specific difficulties, and with the difference in percentage point ranging from 18 (hearing) to 4 (self-care).
Discussion
Persons with disabilities in rural Madwaleni in South Africa faced significantly more barriers to accessing health care compared to persons without disabilities. The study’s hypothesis was thus confirmed by the findings. This is in accordance with, for instance, McDoom et al. [42] and Van Rooy et al. [16].
Transport-related issues were especially prominent – four of the top five barriers mentioned had to do with transport. In Madwaleni, transport is a particularly important issue because of the rugged terrain and great distances which need to be covered. Transport has been identified as a major issue in many other studies of this kind [31, 44–46].
The current study also showed that barriers to health care access increased with age, though this ceased to be significant in the multivariate analysis. Henning-Smith et al. [47] mention that older adults face barriers to care due to high health costs and lack of accessible transportation. This may be particularly true for older persons with disabilities who may face additional barriers to health care. Their study concluded that older adults with disabilities were more likely to experience barriers.
Education was shown to reduce barriers in Madwaleni. This may be because of the probable association between educational disadvantage and poverty.
Socio-economic status and total number of members in the households were not associated with barriers to health care. However, as the sample was drawn from a rather homogeneous and predominantly poor population, such household level characteristics vary less and will thus contribute less to explaining variation in the dependent variable.
Many persons with disabilities reported that they did not receive health care when they needed it and significantly fewer non-disabled reported the same. Persons with disabilities thus had higher rates of unmet health care needs. This is supported by the World Disability Report [8] as well as other sources [48, 49].
Increased understanding of the day-to-day challenges of persons with disabilities and their needs can educate those involved in health planning and care, especially “on how to incorporate various equities in order to create conditions that would enable the individuals with disabilities to achieve optimum health care” [50] (p. 258). It is clear from our study that the issue of access stretches far beyond questions about the health care system as narrowly understood – the questions of transport, poverty, and attitudinal barriers all need attention. In qualitative work as part of the same broad project, we have shown how attitudes towards disability may be intertwined with a lack of understanding of transport needs (see Vergunst et al.) [51].
There are limitations with this study. Being a quantitative study made it difficult to explore in depth the complexities and nuances of disability in terms of access to health care. The study is also descriptive and cross-sectional and does not develop or test interventions or causal pathways. Finally, the multivariate model, while demonstrating relevant associations, is limited in its explanation of barriers.
Conclusion
This paper has highlighted that being a person with disability living in rural Madwaleni is not only about the “medical” issues, but more importantly about social and inclusion issues. As Swartz and Watermeyer [52] state, the story of disability in South Africa, as well as in other countries, is about social oppression. It is with this in mind that we need to shift and open our minds and ideas about disability (particularly with rural impoverished areas in South Africa), and that is a more complex situation. There is still much to do before persons with disabilities in general, and those living in rural impoverished areas in particular, can be included in all parts of society, including access to health care.
Acknowledgements
Not Applicable.
Funding
This research was funded by the European Commission Framework Programme 7: “Enabling Universal and Equitable Access to Healthcare for Vulnerable People in Resource poor Settings in Africa” (Grant Agreement No. 223501).
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- UNCRPD
United Nation’s Convention on the Rights of Persons with Disabilities
Authors contributions
RV, GM, KGH and SHB did the data collection, KGH, AHE the data analysis, RV drafted the article, LS, AHE, GM, MM, HM, SHB and MS made conceptual contributions to the article. All authors have read and approved the final version of this manuscript.
Ethics approval and consent to participate
Ethics Reference Number N10/10/349 from Stellenbosch University.
Written Consent.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
R. Vergunst, Email: rvergunst@sun.ac.za
L. Swartz, Email: lswartz@sun.ac.za
K.-G. Hem, Email: karl-gerhard.hem@sintef.no
A. H. Eide, Email: arne.h.eide@sintef.no
H. Mannan, Email: hasheem.mannan@ucd.ie
M. MacLachlan, Email: mlachlanmac@gmail.com
G. Mji, Email: gumji@sun.ac.za
S. H. Braathen, Email: stine.h.braathen@sintef.no
M. Schneider, Email: marguerite.schneider@uct.ac.za
References
- 1.United Nations . Convention on the rights of persons with disabilities. 2008. [Google Scholar]
- 2.Obrist B, Iteba N, Lengeler C, Makemba A, Mshana C, Nathan R, et al. Access to health care in contexts of livelihood insecurity: a framework for analysis and action. PLoS Med. 2007;4(10):e308. doi: 10.1371/journal.pmed.0040308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualizing access at the interface of health systems and populations. Int J Equity Health. 2013;12:18. doi: 10.1186/1475-9276-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pharr JR. Accommodations for patients with disabilities in primary care: a mixed methods study of practice administrators. Glob J Health Sci. 2014;6(1):23–32. doi: 10.5539/gjhs.v6n1p23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ali A, Scior K, Ratti V, Strydom A, King M, Hassiotis A. Discrimination and other barriers to accessing health care: perspectives with mild and moderate intellectual disability and their carers. PLoS One. 2013;8(8):e70855. doi: 10.1371/journal.pone.0070855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mulumba M, Nantaba J, Brolan CE, Ruano AL, Brooker K, Hammonds R. Perceptions and experiences of access to public healthcare by people with disabilities and older people in Uganda. Int J Equity Health. 2014;13:76. doi: 10.1186/s12939-014-0076-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tomlinson M, Swartz L, Officer A, Chan KY, Rudan I, Saxena S. Research priorities for health of people with disabilities: an expert opinion exercise. Lancet. 2009;374(9704):1857–1862. doi: 10.1016/S0140-6736(09)61910-3. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization . WHO library cataloguing-in-publication data. 2011. World report on disability. [Google Scholar]
- 9.Danquah L, Polack S, Brus A, Mactaggart I, Houdon CP, Senia P, et al. Disability in post-earthquake Haiti: prevalence and inequality in access to services. Disabil Rehabil. 2015;37(12):1082–1089. doi: 10.3109/09638288.2014.956186. [DOI] [PubMed] [Google Scholar]
- 10.Jeon B, Kwon S, Kim H. Health care utilisation by people with disabilities: a longitudinal analysis of the Korea welfare panel study. Disabil Health J. 2015;8:353–362. doi: 10.1016/j.dhjo.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 11.Mahmoudi E, Meade MA. Disparities in access to health care among adults with physical disabilities: analysis of a representative national sample for a ten-year period. Disabil Health J. 2015;8:182–190. doi: 10.1016/j.dhjo.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 12.Scheer J, Kroll T, Neri MT, Beatty P. Access barriers for persons with disabilities – the consumer’s perspective. J Disabil Policy Stud. 2003;13(4):221–230. doi: 10.1177/104420730301300404. [DOI] [Google Scholar]
- 13.MacLachlan M, Mannan H. The world report on disability and its implications for rehabilitation psychology. Rehabil Psychol. 2014;59(2):117–124. doi: 10.1037/a0036715. [DOI] [PubMed] [Google Scholar]
- 14.Braathen SH, Vergunst R, Mji G, Mannan H, Swartz L. Understanding the local context for the application of global mental health: a rural south African experience. Int Health. 2013;5:38–42. doi: 10.1093/inthealth/ihs016. [DOI] [PubMed] [Google Scholar]
- 15.Kritzinger J, Schneider M, Swartz L, Braathen SH. I just answer ‘yes’ to everything they say: access to health care for deaf people in Worcester, South Africa and the politics of exclusion. Patient Educ Couns. 2014;94(3):379–383. doi: 10.1016/j.pec.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 16.Van Rooy G, Amadhila EM, Mufune P, Swartz L, Mannan H, MacLachlan M. Perceived barriers to accessing health services among people with disabilities in rural northern Namibia. Disabil Soc. 2012;27(6):761–775. doi: 10.1080/09687599.2012.686877. [DOI] [Google Scholar]
- 17.Eide AH, Mannan H, Khogali M, van Rooy G, Swartz L, Munthali A, et al. Perceived barriers for accessing health services among individuals with disability in four African countries. PLoS One. 2015;10(5):e0125915. doi: 10.1371/journal.pone.0125915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cordes S, Doeksen GA, Shaffer R. Rural economic development and health services. In: Beaulieu JE, Berry DE, editors. Rural health services – a management perspective. Michigan: Health Administration Press; 1998. pp. 27–56. [Google Scholar]
- 19.Weisgrau S. Issues in rural health: access, hospitals and reform. Health Care Financ Rev. 1995;17(1):1–14. [PMC free article] [PubMed] [Google Scholar]
- 20.Davis R, McAdams R, Tilden N. Primary care access. In: Beaulieu JE, Berry DE, editors. Rural health services: a management perspective. Ann Arbor, MI: AUPHA/Health Administration Press; 1998. pp. 203–227. [Google Scholar]
- 21.Sibley LM, Weiner JP. An evaluation of access to health care services along the rural-urban continuum in Canada. BMC Health Serv Res. 2011;11:20. doi: 10.1186/1472-6963-11-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bourke L, Humphreys JS, Wakerman J, Taylor J. Understanding rural and remote health: a framework for analysis in Australia. Health Place. 2012;18(3):496–503. doi: 10.1016/j.healthplace.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 23.Brems C, Johnson ME, Warner TD, Weiss RL. Barriers to healthcare as reported by rural and urban interprofessional providers. J Interprof Care. 2006;20(2):105–118. doi: 10.1080/13561820600622208. [DOI] [PubMed] [Google Scholar]
- 24.Chipp C, Dewane S, Brems C, Johnson ME, Warner TD, Weiss RL. “If only someone had told me ...”: lessons from rural providers. J Rural Health. 2011;27(1):122–130. doi: 10.1111/j.1748-0361.2010.00314.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goins RT, Williams KA, Carter MW, Spencer SM, Solovieva T. Perceived barriers to health care access among rural older adults: a qualitative study. J Rural Health. 2005;21(3):206–213. doi: 10.1111/j.1748-0361.2005.tb00084.x. [DOI] [PubMed] [Google Scholar]
- 26.Iezzoni LI, Killeen MB, O’Day BL. Rural residents with disabilities confront substantial barriers to obtaining primary care. Health Serv Res. 2006;41(4):1258–1275. doi: 10.1111/j.1475-6773.2006.00534.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ricketts TC, Savitz L. Access to health services. In: Ricketts TC, Gesler LWM, Savitz L, Osborne D, editors. Geographic methods for health services research. Lanham: University Press of America; 1994. pp. 91–119. [Google Scholar]
- 28.Rosenblatt RA. The health of rural people and the communities and environments in which they live. In: Geyman JP, Norris TE, Hart LG, editors. Rural medicine. New York: McGraw-Hill; 2002. pp. 3–15. [Google Scholar]
- 29.Schur CL, Franco SJ. Access to health care. In: Ricketts TC, editor. Rural health in the United States. New York: Oxford University Press; 1999. pp. 25–37. [Google Scholar]
- 30.Reid SJ. Rural health and transformation in South Africa. S Afr Med J. 2006;96(8):676–677. [PubMed] [Google Scholar]
- 31.Lishner DM, Richardson M, Levine P, Patrick D. Access to primary health care among persons with disabilities in rural areas: a summary of the literature. J Rural Health. 1996;12(1):45–53. doi: 10.1111/j.1748-0361.1996.tb00772.x. [DOI] [PubMed] [Google Scholar]
- 32.Coovadia H, Jewkes R, Barron P, Sanders D, McIntyre D. The health and health system of South Africa: historical roots of current public health challenges. Lancet. 2009;374(9692):817. doi: 10.1016/S0140-6736(09)60951-X. [DOI] [PubMed] [Google Scholar]
- 33.Gilson L, McIntyre D. Post-apartheid challenges: household access and use of health care in South Africa. Int J Health Serv. 2007;37(4):673–691. doi: 10.2190/HS.37.4.f. [DOI] [PubMed] [Google Scholar]
- 34.Harris B, Goudge J, Ataguba JE, McIntyre D, Nxumalo N, Jikwana S, et al. Inequities in access to health care in South Africa. J Public Health Policy. 2011;32(S1):S102–S123. doi: 10.1057/jphp.2011.35. [DOI] [PubMed] [Google Scholar]
- 35.Goudge J, Russell S, Gilson L, Gumede T, Tollman S, Mills A. Illness-related impoverishment in rural South Africa: why does social protection work for some households but not others? J Int Dev. 2009;21:231–251. doi: 10.1002/jid.1550. [DOI] [Google Scholar]
- 36.Schneider H, le Marcis F, Grard J, Penn-Kekena L, Blaauw D, Fassin D. Negotiating care: patient tactics at an urban south African hospital. J Health Serv Res Policy. 2010;15(3):137–142. doi: 10.1258/jhsrp.2010.008174. [DOI] [PubMed] [Google Scholar]
- 37.Neille J, Penn C. Beyond physical access: a qualitative analysis into the barriers to policy implementation and service provision experienced by persons with disabilities living in a rural context. Rural Remote Health. 2015;15:3332. [PubMed] [Google Scholar]
- 38.Grut L, Mji G, Braathen SH, Ingstad B. Accessing community health services: challenges faced by poor people with disabilities in a rural community in South Africa. AJOD. 2012;1(1) Art. #19. doi:10.4102/ajod.v1i1.19 [DOI] [PMC free article] [PubMed]
- 39.Maart S, Eide AH, Jelsma J, Loeb ME, Ka TM. Environmental barriers experienced by urban and rural disabled people in South Africa. Disabil Soc. 2007;22(4):357–369. doi: 10.1080/09687590701337678. [DOI] [Google Scholar]
- 40.Jelsma J, Maart S, Eide A, Ka’Toni M, Loeb M. The determinants of health-related quality of life in urban and rural isi-Xhosa-speaking people with disabilities. Int J Rehabil Res. 2007;30(2):119–126. doi: 10.1097/MRR.0b013e32813a2e88. [DOI] [PubMed] [Google Scholar]
- 41.Kok P, Collinson M. Migration and urbanisation in South Africa. Report 03–04-02. Pretoria: Statistics South Africa; 2006. [Google Scholar]
- 42.McDoom MM, Koppleman E, Drainoni M. Barriers to accessible health care for medicaid eligible people with disabilities: a comparative analysis. J Disabil Policy Stud. 2014;25(3):154–163. doi: 10.1177/1044207312469829. [DOI] [Google Scholar]
- 43.Madans JH, Loeb ME, Altman BM. Measuring disability and monitoring the UN convention on the rights of persons with disabilities: the work of the group on disability statistics. BMC Public Health. 2011;11(Suppl 4):S4. doi: 10.1186/1471-2458-11-S4-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goodridge D, Rogers M, Klassen L, Jeffery B, Knox K, Rohatinsky N, et al. Access to health and support services: perspectives of people living with a long-term traumatic spinal cord injury in rural and urban areas. Disabil Rehabil. 2015;37(16):1401–1410. doi: 10.3109/09638288.2014.972593. [DOI] [PubMed] [Google Scholar]
- 45.Syed ST, Gerber BS, Sharp LK. Travelling towards disease: transportation barriers to health care access. J Community Health. 2013;38:976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paez A, Mercado RG, Farber S, Morency C, Roorda M. Accessibility to health care facilities in Montreal Island: an application of relative accessibility indicators from the perspective of senior and non-senior residents. Int J Health Geogr. 2010;9(52) doi:10.1186/1476-072x-9-52. [DOI] [PMC free article] [PubMed]
- 47.Henning-Smith CE, Gonzales G, Shippee TE. Barriers to timely medical care for older adults by disability status and household composition. J Disabil Policy Stud. 2016;27(2):116–127. doi: 10.1177/1044207316637547. [DOI] [Google Scholar]
- 48.Gudlavalleti MVS, John N, Allagh K, Sagar J, Kamalakannan S, Ramachandra SS, et al. Access to health care and employment status of people with disabilities in South India, the SIDE study. BMC Public Health. 2014;14:1125–1132. doi: 10.1186/1471-2458-14-1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Casey R. Disability and unmet health care needs in Canada: a longitudinal analysis. Disabil Health J. 2015;8:173–181. doi: 10.1016/j.dhjo.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 50.Mahtab A. Health care access and barriers for the physically disabled in rural Punjab. Pakistan. Int J Sociol Soc Policy. 2013;33(3/4):246–260. doi: 10.1108/01443331311308276. [DOI] [Google Scholar]
- 51.Vergunst R, Swartz L, Mji G, MacLachlan M, Mannan H. “You must carry your wheelchair” – barriers to accessing health care in a south African rural area. Glob Health Action. 2015;8 [DOI] [PMC free article] [PubMed]
- 52.Swartz L, Watermeyer B. Introduction and overview. In: Watermeyer B, Swartz L, Lorenzo T, Schneider M, Priestley M, editors. Disability and social change – a south African agenda. Cape Town: HSRC; 2006. pp. 1–6. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.


