Abstract
Background
This study explores medicinal plant knowledge and use among Muslim women in the city of Mecca, Saudi Arabia. Ethnobotanical research in the region has focused on rural populations and male herbal healers in cities, and based on these few studies, it is suggested that medicinal plant knowledge may be eroding. Here, we document lay, female knowledge of medicinal plants in an urban centre, interpreting findings in the light of the growing field of urban ethnobotany and gendered knowledge and in an Islamic context.
Methods
Free-listing, structured and semi-structured interviews were used to document the extent of medicinal plant knowledge among 32 Meccan women. Vernacular names, modes of preparation and application, intended therapeutic use and emic toxicological remarks were recorded. Women were asked where they learnt about medicinal plants and if and when they preferred using medicinal plants over biomedical resources. Prior informed consent was always obtained. We compared the list of medicinal plants used by these Meccan women with medicinal plants previously documented in published literature.
Results
One hundred eighteen vernacular names were collected, corresponding to approximately 110 plants, including one algae. Of these, 95 were identified at the species level and 39 (41%) had not been previously cited in Saudi Arabian medicinal plant literature. Almost one half of the plants cited are food and flavouring plants. Meccan women interviewed learn about medicinal plants from their social network, mass media and written sources, and combine biomedical and medicinal plant health care. However, younger women more often prefer biomedical resources and learn from written sources and mass media.
Conclusions
The fairly small number of interviews conducted in this study was sufficient to reveal the singular body of medicinal plant knowledge held by women in Mecca and applied to treat common ailments. Plant availability in local shops and markets and inclusion in religious texts seem to shape the botanical diversity used by the Meccan women interviewed, and the use of foods and spices medicinally could be a global feature of urban ethnobotany. Ethnobotanical knowledge among women in Islamic communities may be changing due to access to mass media and biomedicine. We recognise the lack of documentation of the diversity of medicinal plant knowledge in the Arabian Peninsula and an opportunity to better understand gendered urban and rural knowledge.
Keywords: Ethnobotany, Saudi Arabia, Islam, Transmission, Food-medicine continuum
Background
The use of medicinal plants in urban environments
Currently, more people live in cities than in rural areas, and urban populations continue to grow: by 2050, two thirds of the world’s population will live in cities [1]. Urbanisation brings new health challenges resulting from ease of contagion, maintenance of disease due to high population densities and stress-related ailments [2]. Although biomedicine is often easily available in urban settings, traditional medicines can still be the most convenient and affordable health care resource [2, 3]. Similar to people in rural areas, urban dwellers can hold rich medicinal plant knowledge. Recent studies evidence the dynamism and adaptive nature of urban medicinal plant knowledge (e.g. [3–7]), challenging views that such knowledge is lost in cities.
Since Balick et al. [4] noted a lack of ethnobotanical studies in urban areas, urban ethnobotany has flourished. Ethnobotanical surveys in cities have focused on issues such as the change of plant use by international immigrants [4, 6, 8–12] or the ethnobotanical diversity found in urban and peri-urban markets [13–15] and home gardens [16, 17]. With few exceptions [7, 14, 15], these studies are set in Northern and Western countries. Cities in other parts of the world are equally dynamic plant knowledge hubs, and some have played an important role in the trade of medicinal plant material and knowledge historically. This is the case of cities along the silk and incense trade routes in the Middle East [18–20].
Women’s medicinal plant knowledge
Several studies across the world have reported the pivotal role of women as holders of medicinal plant knowledge [21–28]. Medicinal plant knowledge is often women’s cultural domain because of the role women play in providing household care [21–23, 29, 30]. It also stems from gendered labour and spaces, which affect plant resource harvesting and management [21, 22, 26]. Women are often more knowledgeable about medicinal plant identification and use than are men [21, 23–25], and their knowledge can be epistemologically different [22].
Moreover, the documentation of traditional knowledge as part of plant biodiversity research has historically been gender-biased towards men, which can result in misleading and incomplete results [22, 31, 32]. Both Howard [22] and Pfeiffer and Butz [32] claim that focus on male specialists, such as shamans and herbalists, has ignored a wealth of lay, female plant knowledge in ethnobotanical research. Historically, ethnobotanists have been predominantly male, which hampered their access to women’s knowledge in societies where men are granted greater public access than women [32]. These considerations are particularly important in conducting ethnobotanical research in the Islamic world, where gendered spaces and networks are particularly strong. Women in urban Islamic contexts have so far gone unnoticed by ethnobotanical enquiry, although they are the main medicinal plant users in Saudi Arabian cities [33].
Islam and medicinal plants
In the Arabian Peninsula, where this study took place, the use of local plant diversity for medicines is part of the cultural heritage [34, 35] and is currently embedded in Islamic medicinal practices. Islamic medicine integrates ancient Greek medicine, which first arrived to the Islamic world through translations of the works of Hippocrates, Dioscorides and Galen [36], with the teachings of the Prophet Mohamed (Hadith) referring to health, disease and medical treatment that became known as ‘The Medicine of the Prophet’ [37, 38]. From ancient Greek medicine, understandings of the functioning of the body through the humoral system and the view of disease as a loss of balance became part of Islamic medicine [37, 39, 40]. Arabian physicians, such as Al Razi, Ibn Sina, Aby Al Kassin Al Zahrawi, Ibn Rushd and Ibn Naffs, further developed medicine as a scientific discipline in the Middle Ages [36].
Islamic religious practices generate specific cultural behaviours that aim to preserve health, and early Islamic medical tradition focused on preventive rather than therapeutic medicine [37–39]. Beliefs in jinni and Evil Eye as causes of illness are also common in the Arab world [29, 36, 40]. These magical features are possibly elements of the Bedouin world view that became legitimised by the Quran and the Hadith [40]. Stemming from religious teachings, Islamic medicine has a holistic view of health, where physical, spiritual, psychological, social and environmental factors are intertwined [38, 39]. The maintenance of health and recovery from illness are both a physical and spiritual process, underpinned by the belief in God [38, 39].
Study aims
Whilst medicinal plant uses are under-documented in the Middle East [41, 42] and a trend of loss of ethnobotanical and ethnomedicinal knowledge is observed in this area [36, 43], the extent of medicinal plant knowledge held by urban women remains unknown. The aim of this study was to document urban women’s medicinal plant knowledge in an Islamic context, identifying the plant species used. Additionally, modes of transmission of knowledge were evaluated, evidence for change noted. The extent to which women’s medicinal plant knowledge has been under-documented was inferred by comparing results from free-listing and semi-structured interviews conducted with women in Mecca to selected published literature on medicinal plants used in Saudi Arabia.
Methods
Research setting: Mecca as a study site
The city of Mecca (Kingdom of Saudi Arabia) is located in a narrow valley 80 km south of Jeddah on the Red Sea coast, west of the Arabian Peninsula (Fig. 1). The city is the capital of the Mecca region, neighbouring the regions of Medina in the north, Baha and Asir in the south and Al-Riyad in the east. The region of Mecca is situated in a subtropical dry environment [44]; its vegetation is dominated by xerophytic species and composed of floristic elements from the Saharo-Arabian, Irano-Turanian and Sudano-Zambian biogeographical regions [45].
Fig. 1.
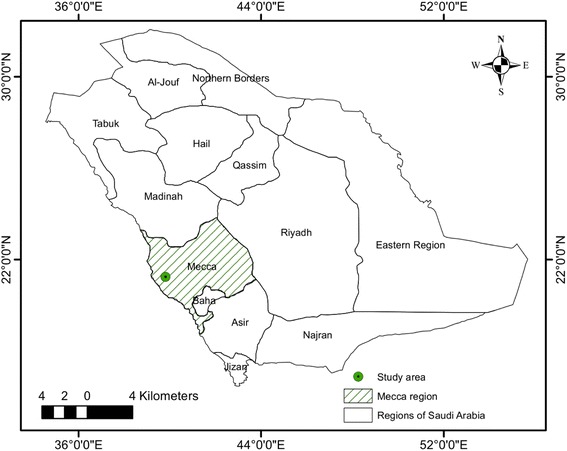
Map of Saudi Arabia with regional divisions. The city of Mecca is indicated by a dot
Mecca was the birthplace of the Prophet Muhammad and the site of the first Quranic revelation. It is regarded as the most holy city in Islam and the pilgrimage to Mecca, known as Hajj, is obligatory for all able Muslims. Due to the high numbers of pilgrims travelling to Mecca, the city is the most culturally diverse in the Islamic world. Saudi Arabians may use both traditional herbal and biomedical treatments [34, 36, 45], and a wide range of health care resources are available in Mecca: from traditional medicines and healers ([45], Al-Qethami, pers. obs), to modern biomedical care provided by the Saudi government for free to all Muslims.
Conducting interviews with Meccan women
The ethical guidelines of the Code of Ethics of the International Society of Ethnobiology [46], the Declaration of Helsinki [47] and University of Reading ethical protocols were followed in this research. Approval from the Ethics Committee of the School of Biological Sciences, University of Reading, was obtained (Research Ethics Project Submission SBS15-16 11).
Meccan women were interviewed by the first author from May to June 2016; individual free-listing and semi-structured interviews were conducted with 32 female adults. Targeted sampling was used for selecting informants who use medicinal plants [48] from the first author’s social network. Snowball sampling was later used to identify other local women who use medicinal plants [49]. All the informants were born in the Mecca region, with ages ranging between 28 and 69 years old (see Table 1 for the informants’ anonymous social data). Although older informants may hold further knowledge, interviews were conducted until a saturation of information was reached. Prior informed consent was obtained verbally from each woman before they were interviewed. Interviews were conducted in Arabic and recorded when the agreement from the informants was obtained (n = 9). Firstly, women were asked to list the medicinal plants they knew, documenting plant names. Then, semi-structured interviews were used to elucidate the parts used, therapeutic uses, preparation and administration processes (including use in mixtures) and perceptions of potential toxicity and side effects of plants used. Moreover, women were asked about how they had acquired this knowledge, if medicinal plants or biomedicine were preferred and when medicinal plants where preferred over biomedicine. The resulting ethnographic data were useful to understand women’s attitudes, beliefs and therapeutic goals underpinning medicinal plant use.
Table 1.
Informant’s details. Place of residence is at the time of the interview; three women were temporarily living in the UK, where they were interviewed. MP/BM refers to preference for medicinal plants or biomedicine
| Code | Age | Occupation | Literacy | N of children | Place of residence | N of household members | Place of origin | Number of plants listed | MP/BM | Source knowledge |
|---|---|---|---|---|---|---|---|---|---|---|
| inf1 | 30 | Lecturer | PhD (Arabic, English) | 1 | Reading, UK | 3 | Mecca | 15 | BM | Scientific lectures, grandparents and mother |
| inf2 | 47 | Lecturer | PhD (Arabic, English) | 6 | Reading, UK | 8 | Jeddah | 13 | MP | Grandmothers and mother |
| inf3 | 35 | Housewife | Secondary education (Arabic) | 5 | Mecca | 7 | Mecca | 9 | BM | Grandmothers and mother |
| inf4 | 31 | Student | PhD (Arabic, English) | 0 | Reading, UK | 9 | Mecca | 10 | BM | Mother, scientific lectures, Internet |
| inf5 | 49 | Housewife | Primary education (Arabic) | 6 | Mecca | 8 | Mecca | 23 | MP | Mother |
| inf6 | 51 | Housewife | Primary education (Arabic) | 3 | Mecca | 4 | Mecca | 18 | MP | Grandmothers |
| inf7 | 32 | Housewife | Secondary education (Arabic) | 5 | Mecca | 7 | Mecca | 21 | MP | Grandmothers, mother, neighbours, books, Internet, television |
| inf8 | 49 | Housewife | Primary education (Arabic) | 5 | Mecca | 6 | Mecca | 13 | MP | Grandmothers |
| inf9 | 50 | Housewife | Primary education (Arabic) | 4 | Mecca | 5 | Mecca | 24 | MP | Written sources, mother and aunt |
| inf10 | 60 | Housewife | Primary education (Arabic) | 10 | Mecca | 5 | Mecca | 18 | MP | Grandmothers |
| inf11 | 45 | Housewife | Primary education (Arabic) | 2 | Mecca | 3 | Mecca | 24 | MP | Grandmothers |
| inf12 | 56 | Housewife | Primary education (Arabic) | 2 | Mecca | 4 | Mecca | 24 | MP | Grandmothers |
| inf13 | 32 | Housewife | Bachelor (Arabic) | 4 | Mecca | 6 | Mecca | 9 | BM | Mother |
| inf14 | 65 | Housewife | Illiterate (Arabic) | 9 | Mecca | 10 | Mecca | 12 | MP | Grandmothers |
| inf15 | 34 | Housewife | Secondary education (Arabic) | 2 | Mecca | 4 | Mecca | 12 | BM | Wider community (social network beyond family members) |
| inf16 | 29 | Housewife | Bachelor (Arabic) | 3 | Mecca | 5 | Mecca | 15 | BM | Mother, Internet |
| inf17 | 69 | Housewife | Illiterate (Arabic) | 7 | Mecca | 9 | Mecca | 17 | MP | Grandmothers |
| inf18 | 60 | Housewife | Illiterate (Arabic) | 9 | Mecca | 6 | Mecca | 25 | MP | Mother, Internet, shops of medicinal plants |
| inf19 | 30 | Housewife | Bachelor (Arabic) | 3 | Mecca | 5 | Mecca | 8 | BM | Mother, Internet |
| inf20 | 59 | Housewife | Primary education (Arabic) | 3 | Mecca | 4 | Mecca | 18 | MP | Grandmothers |
| inf21 | 50 | Housewife | Illiterate (Arabic) | 6 | Mecca | 8 | Mecca | 17 | MP | Grandmothers |
| inf22 | 45 | Housewife | Bachelor (Arabic) | 6 | Mecca | 8 | Mecca | 16 | MP | Grandmothers |
| inf23 | 37 | Housewife | Secondary education (Arabic) | 5 | Mecca | 7 | Taif | 12 | MP | Grandmothers |
| inf24 | 39 | Housewife | Bachelor (Arabic) | 4 | Mecca | 6 | Mecca | 17 | MP | Grandmothers |
| inf25 | 34 | Housewife | Bachelor (Arabic) | 3 | Mecca | 5 | Mecca | 12 | BM | Mother |
| inf26 | 33 | Housewife | Bachelor (Arabic) | 3 | Mecca | 5 | Mecca | 12 | BM | Family |
| inf27 | 33 | Housewife | Bachelor (Arabic) | 4 | Mecca | 6 | Mecca | 24 | MP | Family, nutrition studies at the university |
| inf28 | 34 | Housewife | Bachelor (Arabic) | 6 | Mecca | 8 | Mecca | 17 | BM | Mother, family, friends, Internet |
| inf29 | 28 | Lecturer | Bachelor (Arabic) | 1 | Mecca | 3 | Mecca | 18 | BM | Mother, sisters, school |
| inf30 | 46 | Housewife | Bachelor (Arabic) | 4 | Mecca | 6 | Mecca | 17 | MP | Mother, family, books |
| inf31 | 60 | Housewife | Primary education (Arabic) | 9 | Mecca | 5 | Mecca | 12 | MP | Grandmothers |
| inf32 | 60 | Housewife | Illiterate (Arabic) | 10 | Mecca | 5 | Mecca | 10 | MP | Grandmothers |
Analysis of medicinal plant’s salience
Data collected during interviews were structured in ‘use reports’. A ‘use report’ is one citation of one plant use by one informant, and it includes vernacular name, part used, local use, preparation and administration. Alongside the emic use citations, therapeutic applications were classified by disease categories according to the International Classification of Primary Care, as recommended by Staub et al. [50]. The software anthropac [51] was used to analyse free-lists, obtaining the frequency of citation and Smith’s index for each plant [52]. Smith’s index is a measure of the cultural importance of each plant depending on the frequency of citation and its rank in the free-lists [52].
Plant collection and identification
Most voucher specimens were obtained directly from informants. When this was not possible, they were obtained from local shops and supermarkets (Atar AlKuwait, Atar Alamana and Matager Alsudia; Fig. 2). Voucher specimens were not obtained for two plants; specimens from the Umm Al-Qura University herbarium were used to identify these according to vernacular names. Voucher specimens (including market samples) were deposited in the Umm Al-Qura University herbarium. Since no plants were collected from the wild directly, collection permits were not necessary. Plant identification was carried out by the first author in the herbarium of Umm Al-Qura University using the Flora of Saudi Arabia [53], and identifications were validated by a plant taxonomist in Umm Al-Qura University. Nomenclature and family adscriptions follow The Plant List [54], and the list was contrasted with the online checklist of the Flora of Saudi Arabia [55].
Fig. 2.

Herbalist store in Mecca. Atar AlKuwait, one of the most famous establishments selling medicinal plant products in Mecca
Literature review
In order to assess the documented Saudi Arabian medicinal plant knowledge, a systematic literature review was conducted. Google Scholar, the Saudi Digital Library, Research Gate and King Abdullah bin Abdulaziz Library were searched for books and scientific articles using the search terms ‘Saudi Arabia’, ‘Mecca’, ‘Medicinal Plant’, ‘Herbal’, ‘Traditional Medicine’ or ‘Ethnobotany’ in English and Arabic, with no restriction on date of publication. Literature were excluded if they only reported pharmacological activities without mention of local knowledge sources, or if they focused on veterinary plant uses. Eleven sources were identified, obtained and reviewed, including seven journal articles and four books. For these, the methods were reviewed, examining how local names and plant uses were recorded and how plant identification was achieved. Explicit knowledge documentation methods, collection of herbarium specimens, the literature used to identify them and deposition in herbaria were quality criteria used to identify rigorous literature sources [5, 56]. One book and three scientific articles were considered rigorous and selected to compare the medicinal plants listed with those used by the women in Mecca interviewed during this study. The names from selected literature were cross-checked with The Plant List [54] to identify accepted plant names and family assignments. Botanical species, vernacular names and uses mentioned by women in Mecca during the field study were then compared to those in the selected literature to identify the extent of the overlap between lists.
Results
Medicinal plants used by women in Mecca
In total, 753 use reports were collected during interviews and 118 medicinal plant vernacular names were documented, belonging to approximately 110 botanical taxa (43 families; Table 2), including one algae (Fucus vesiculosus). Ninety-five medicinal plants were identified at the species level, 12 were identified at the genus level, one at the family level and two could not be identified. The most common medicinal families are Apiaceae (10%; 11 taxa), Fabaceae (9%; 10 taxa) and Lamiaceae (7%; eight taxa). Asteraceae, Brassicaceae and Poaceae were represented by five taxa each; Myrtaceae, Rosaceae and Zingiberaceae by four taxa each; and Amaranthaceae, Apocynaceae, Burseraceae and Rutaceae by three taxa each. Seven families were represented by two taxa and 24 families were represented only by one taxon. The most cited salient medicinal plants during the interviews are helba (Trigonella foenum-graecum), kamun (Cuminum cyminum), yansun (Pimpinella anisum), qurfa (Cinnamomum verum) and zanajabil (Zingiber officinale) (Table 2). Interestingly, we observed that one third (32%) of the plants mentioned in the interviews are common vegetable and fruit crops, and almost one fifth (17%) are spices. More than half of the taxa were not native to Saudi Arabia (54%; Table 2).
Table 2.
Comprehensive inventory of the plants listed by women in Mecca including the scientific name and family, whether the plant is found in the Flora of Saudi Arabia and whether it is used as a food or spice, vernacular name(s), part(s) used, therapeutic use categories, preparation, administration, toxicity and side effects, frequency of citation and Smith’s S. For presence or absence in the Flora of Saudi Arabia, Y = yes, N = no, and for food and/or spice use, F = food and S = spice. Plants not documented in the selected literature are marked with ‘*’
| Scientific name (family, voucher) | Flora of Saudi Arabia | Food (F) or spice (S) | Vernacular name(s) (Arabic) | Part(s) used | Therapeutic use categories | Preparation | Administration | Toxicological remarks and reported side effects | Frequency of citation | Smith’s S |
|---|---|---|---|---|---|---|---|---|---|---|
| Acacia nilotica (L.) Delile. (Fabaceae, EWM_62) | N | – | Qard (ضرق) | Fruit, root | Neurological, digestive | Infusion, decoction | Wash, bath | N | 2 | 0.041 |
|
Acacia senegal (L.) Willd. (Fabaceae, EWM_77) |
N | – | Samg arabi (يبرع غمص) | Resin | Urological, endocrine and nutritional | Infusion | Oral ingestion (drink) | N | 2 | 0.042 |
| Aerva javanica (Burm.f.) Juss. ex Schult. (Amaranthaceae, EWM_90) | Y | – | Tarf (فرط) | All plant | Neurological, digestive | Infusion, ground | Oral ingestion (drink), put directly on the teeth | N | 1 | 0.009 |
| * Alchemilla sp. (Rosaceae, EWM_68) | Y | – | Rajel alasad (دسلآا لجر) | Root | Digestive | Infusion | Oral ingestion (drink) | Not to be used by pregnant women | 1 | 0.01 |
| *Alchemilla xanthochlora Rothm. (Rosaceae, EWM_01) | N | – | Abat alseda (ةأبع ةديسلا) | Leaf | Gynaecological | Infusion | Oral ingestion (drink) | N | 1 | 0.021 |
| Allium cepa L. (Amaryllidaceae, EWM_14) | N | F | Bsal (لصب) | Bulb, tunic | General and unspecified, gynaecological | Juice with lemon, added to food | Oral ingestion (drink or eat), fumigation, placing onions on the bottom of the feet and wear socks | N | 4 | 0.034 |
| Allium sativum L. (Amaryllidaceae, NA) | N | F | Thoom (موث) | Bulb | General and unspecified, cardiovascular, digestive, ear | Put with food, in water, mash, no preparation | Oral ingestion (eat or drink), put directly on the teeth | N | 7 | 0.069 |
| Aloe sp. (Xanthorrhoeaceae, EWM_74) | Y | – | Sabr (ربص) | Leaf flesh | Digestive, gynaecological, skin | Put in water | Oral ingestion (drink), topic on wounds | Causes diarrhoea | 1 | 0.007 |
| Aloe vera (L.) Burm.f. (Xanthorrhoeaceae, EWM_73) | N | – | Sabbar (رابص) | Leaf flesh | Skin | No preparation | Topic on wounds or hair | Overdose may cause colon cancer | 2 | 0.041 |
| *Alpinia officinarum Hance (Zingiberaceae, EWM_43) | N | S | Kholanjan (ناجنلوخ) | Rhizome | Digestive, cardiovascular, skin | Infusion | Oral ingestion (drink) | N | 1 | 0.013 |
| *Ammi visnaga (L.) Lam. (Apiaceae, EWM_44) | Y | S | Khull (ةلخ) | Seed, leaf, fruit | Cardiovascular, urological | Infusion | Oral ingestion (drink) | Overdose may cause dryness and hypotension, not to be used by pregnant women | 4 | 0.053 |
| Anastatica hierochuntica L. (Brassicaceae, EWM_34) | Y | – | Kaff maryam (فك ميرم) | Fruit | Family planning, gynaecological | Infusion | Oral ingestion (drink), topic | Can cause stomach disorders and nausea | 4 | 0.04 |
| Anethum graveolens L. (Apiaceae, EWM_81) | Y | S | Shabath (ثبش) | Leaf | Digestive | Infusion | Oral ingestion (drink) | Not to be used by those who suffer from kidney disease | 1 | 0.004 |
| *Apium graveolens L. (Apiaceae, EWM_46) | Y | F | Korfos (سفرك) | Leaf | Gynaecological, digestive, neurological | Infusion, juice, no preparation | Oral ingestion (eat or drink) | Not to be used by pregnant women | 2 | 0.02 |
| *Artemisia judaica L. (Asteraceae, EWM_87) | Y | – | Shayh (حيش) | All plant | Digestive | Infusion | Oral ingestion (drink) | Not to be used by pregnant women | 1 | 0.007 |
| *Avena sativa L. (Poaceae, EWM_88) | Y | F | Shuran (نافوش) | Seed | Endocrine and nutritional | Ground | Oral ingestion (eat) | N | 1 | 0.002 |
| Azadirachta indica A. Juss. (Meliaceae, EWM_60) | N | – | Nim (مين) | Leaf | Digestive, general and unspecified | Decoction | Oral ingestion (drink), bath | N | 2 | 0.035 |
| *Beta vulgaris L. (Amaranthaceae, EWM_09) | Y | F | Banjr (رجنب) | Fruit | Blood and immune mechanisms | Decoction, juice, no preparation | Oral ingestion (drink ore at) | N | 7 | 0.054 |
| Boswellia sacra Flueck. (Burseraceae, EWM_50) | N | – | Laban aldakar, laban shahari (نابل ،ركذلا يرحش نابل) | Resin | General and unspecified, respiratory, neurological | Infusion, chewing, fumigation | Oral ingestion (drink) | N | 8 | 0.113 |
| *Brassica oleracea L. (Brassicaceae, NA) | N | F | Kronb (بنرك) | Leaf | Digestive | Juice (with apples and milk), in food, decoction | Oral ingestion (drink or eat) | N | 7 | 0.018 |
| Brassica rapa L. (Brassicaceae, EWM_40) | N | F | Khardal (لدرخ) | Seed | Musculoskeletal, cardiovascular | Ground, infusion | In hot water (to put feet in) | N | 2 | 0.028 |
| Calotropis procera (Ait.) Ait. fil., (Apocynaceae, NA) | Y | – | Eshr (راشع) | Flower | Respiratory | In water, ground | Oral ingestion (drink or eat) | Can cause diarrhoea | 1 | 0.005 |
| *Camellia sinensis (L.) Kuntze (Theaceae, EWM_85) | N | F | Shay, shay akhdar (ياش, رضخأ ياش) | Leaf | Digestive, metabolic and nutritional, gynaecological, general and unspecified, family planning | Decoction, infusion | Topic, oral ingestion (drink), fumigation | When ingested, overdose may cause diarrhoea | 7 | 0.09 |
| Carthamus tinctorius L. (Asteraceae, EWM_61) | Y | – | Osforr (رفصع) | Flower | Endocrine and nutritional, cardiovascular | Infusion | Oral ingestion (drink) | Overdose may cause diarrhoea | 1 | 0.03 |
| *Carum carvi L. (Apiaceae, EWM_37) | N | S | Karawia (ةيوارك) | Seed | Digestive, gynaecological, general and unspecified, respiratory, family planning | Decoction | Oral ingestion (drink) | Overdose may affect the kidneys | 6 | 0.111 |
| Ceratonia siliqua L. (Fabaceae, EWM_41) | N | F | Kharnub (بونرخ) | Fruit | Digestive | Infusion | Oral ingestion (drink) | N | 1 | 0.025 |
| *Cinnamomum verum J. S. Presl (Lauraceae, EWM_67) | N | S | Qurfa (هفرق) | Bark | Gynaecological, digestive, blood and immune system, endocrine and nutritional, respiratory, family planning | Decoction, ground | Oral ingestion (eat or drink) | Overdose may cause fainting, hypotension, dizziness and sweating, bleeding if used for more than 3 days, not to be used with ginger, not to be used by pregnant women (may cause abortion) | 20 | 0.349 |
| Citrullus colocynthis (L.) Schrad. (Cucurbitaceae, EWM_28) | Y | – | Hanzal (لظنح) | Leaf, fruit | Digestive, skin | Infusion, no preparation | Oral ingestion (drink), topic | N | 2 | 0.041 |
| *Citrus sinensis (L.) Osbeck (Rutaceae, EWM_51) | N | F | Portokal (لاقترب) | Fruit | Digestive, general and unspecified | Juice, no preparation | Oral ingestion (eat or drink) | N | 2 | 0.04 |
| Citrus sp. (Rutaceae, EWM_51) | N | F | Limon (نوميل) | Fruit | General and unspecified, digestive, endocrine and nutritional, respiratory | Juice, dry until black and ground in water, decoction | Oral ingestion (drink), topic | N | 10 | 0.201 |
| Coffea arabica L. (Rubiaceae, EWM_64) | N | F | Qashr album (رشق نبللا) | Pericarp | Blood and immune system, gynaecological, endocrine and nutritional | Decoction, infusion | Oral ingestion (drink) | Not to be used by pregnant women | 6 | 0.117 |
| Commiphora gileadensis (L.) C. Christ. (Burseraceae, EWM_12 | Y | – | Basham (ماشب) | Root | Gynaecological, general and unspecified, respiratory, neurological | Decoction, infusion | Oral ingestion (drink), topic | N | 3 | 0.051 |
| Commiphora myrrha (Nees) Engl. (Burseraceae, EWM_53) | Y | – | Marr (رم) | Resin | Skin, digestive, respiratory, gynaecological, general and unspecified | In water, infusion | Poultice, mouthwash, oral ingestion (drink) | Overdose may upset the stomach and cause general discomfort | 17 | 0.323 |
| Coriandrum sativum L. (Apiaceae, EWM_47) | Y | F | Kozbra (ةربزك) | Leaf | Digestive, cardiovascular, neurological | Ground, infusion, with food | Oral ingestion (eat or drink) | Overdose may cause infertility | 5 | 0.079 |
| *Costus sp. (Costaceae, EWM_63) | N | – | Qasd hindi (يدنه دصق) | Root | Endocrine and nutritional, general and unspecified, gynaecological, blood and immune system, urological, family planning | Ground, decoction | Oral ingestion (eat or drink) | N | 4 | 0.05 |
| *Crocus sativus L. (Iridaceae, EWM_99) | N | S | Zafran (نارفعز) | Stigma | General and unspecified, digestive, respiratory | With food, in water | Oral ingestion (eat or drink) | Not to be used by pregnant women | 3 | 0.025 |
| Cucumis sativus L. (Cucurbitaceae, NA) | N | F | Khiar (رايخ) | Fruit | Urological, digestive, neurological | No preparation | Oral ingestion (eat) | N | 2 | 0.033 |
| Cuminum cyminum L. (Apiaceae, EWM_36) | Y | S | Kamun (نومك) | Seed | Digestive, gynaecological, endocrine and nutritional, general and unspecified, respiratory | Infusion, decoction, ground | Oral ingestion (eat or drink) | Overdose may upset the stomach and produce constipation) | 22 | 0.486 |
| Curcuma longa L. (Zingiberaceae, EWM_38) | N | S | Karrakum (مكرك) | Rhizome | Musculoskeletal, skin, blood and immune system, general and unspecified, digestive, respiratory, endocrine and nutritional | Ground, infusion, with honey | Oral ingestion (eat or drink), poultice | Overdose may upset the stomach | 8 | 0.09 |
| *Cydonia oblonga Mill. (Rosaceae, NA) | N | F | Safarjil (لجرفس) | Fruit | Digestive | No preparation | Oral ingestion (eat) | N | 1 | 0.02 |
| *Cymbopogon schoenanthus (L.) Spreng. (Poaceae, EWM_02) | Y | – | Adhkhur (رخذا) | Leaf | Neurological, digestive, urological, general and unspecified | Decoction | Oral ingestion (drink), decoction (steam inhalation) | N | 3 | 0.069 |
| *Dialium sp. (Fabaceae, EWM_26) | N | – | Hamayd (ضيمح) | Fruit | Digestive, urological | Infusion | Oral ingestion (drink) | N | 1 | 0.008 |
| *Dipterygium glaucum Decne. (Cleomaceae, EWM_06) | Y | – | Arfaj (جفرع) | Leaf | Digestive, respiratory | Infusion | Oral ingestion (drink), decoction (steam inhalation) | N | 1 | 0.003 |
| *Dracaena cinnabari Balf.f. (Asparagaceae, EWM_16) | N | – | Dam alakhwan (مد نيوخلأا) | Resin | General and unspecified, digestive | Ground | Poultice | N | 1 | 0.006 |
| *Elettaria cardamomum (L.) Maton (Zingiberaceae, EWM_24) | N | S | Hal (لاه) | Fruit, seed | Respiratory | Infusion | Oral ingestion (drink) | N | 1 | 0.004 |
| Eruca sp. (Brassicaceae, EWM_33) | Y | – | Jarjir (ريجرج) | Leaf | Blood and immune system, respiratory | With food, no preparation | Oral ingestion (eat or drink) | N | 9 | 0.133 |
| Eucalyptus camaldulensis Dehnh. (Myrtaceae, EWM_35) | N | – | Kafor (روفاك) | Leaf | Neurological, digestive, general and unspecified | Infusion, decoction | Oral ingestion (drink) | N | 3 | 0.035 |
| Ferula assa-foetida L. (Apiaceae, EWM_25) | N | – | Halatayta (ةتيتلح) | Resin | Digestive, respiratory | Maceration | Oral ingestion (drink) | Not to be used by breastfeeding women, children should not take more than 5 ml | 4 | 0.068 |
| Ficus palmata Forssk. (Moraceae, NA) | Y | F | Hamat (طامح) | Fruit | Digestive | No preparation | Oral ingestion (eat) | N | 1 | 0.007 |
| Foeniculum vulgare Mill. (Apiaceae, EWM_83) | Y | S | Shamr (رمش) | Seed | Digestive, urological, gynaecological, general and unspecified, neurological, blood and immune system | Infusion, decoction, ground | Oral ingestion (drink or eat) | Overdose may cause inflammation of the intestines | 14 | 0.248 |
| *Fucus vesiculosus L. (Fucaceae, EWM_21) | N | – | Foqus (سقوف) | Leaf | Endocrine and nutritional, cardiovascular | Infusion | Oral ingestion (drink) | N | 1 | 0.004 |
| *Glebionis coronaria (L.) N.N. Tzvel. (Asteraceae, EWM_04) | N | – | Aqhwan (ناوحقا) | Leaf, flower | Digestive | Infusion | Oral ingestion (drink) | Not recommended for babies | 1 | 0.004 |
| Glycyrrhiza glabra L. (Fabaceae, EWM_18) | Y | – | Eirqsos (سوسقرع) | Root | Digestive, musculoskeletal | Infusion | Oral ingestion (drink) | N | 1 | 0.023 |
| *Hibiscus sabdariffa L. (Malvaceae, EWM_49) | N | – | Kwajara karakadi (،يتارجوك ةيدكرك) | Calyx, sepal | Cardiovascular, blood and immune system, digestive, urological, neurological | Infusion, decoction | Oral ingestion (drink) | N | 15 | 0.209 |
| *Hordeum vulgare L. (Poaceae, EWM_82) | Y | F | Shaeir (ريعش) | Seeds | Urological, digestive | Decoction | Oral ingestion (drink) | Not to be used by pregnant women | 5 | 0.041 |
| *Hyphaene sp. (Arecaceae, EWM_17) | Y | – | Dom (مود) | Fruit | Cardiovascular | Ground, infusion with honey | Oral ingestion (drink) | N | 1 | 0.026 |
| Juniperus procera Hochst. ex Endl. (Cupressaceae, EWM_05) | Y | – | Arar (رعرع) | Fruit | Urological | Infusion, decoction | Oral ingestion (drink) | Not to be used by pregnant women | 1 | 0.006 |
| *Lactuca sativa L. (Asteraceae, NA) | N | F | Khas (سخ) | Leaf | Blood and immune system, urological, digestive | With food | Oral ingestion (eat) | N | 2 | 0.02 |
| *Laurus nobilis L. (Lauraceae, EWM_93) | N | S | Waraq alghar (قرو راغلا) | Leaf | Urological, general and unspecified | Infusion | Oral ingestion (drink) | N | 1 | 0.007 |
| Lawsonia inermis L. (Lythraceae, EWM_27) | Y | – | Hana (انح) | Leaf | Neurological, musculoskeletal, skin | Ground, with honey in water | Topic, poultice | N | 3 | 0.03 |
| Lepidium sativum L. (Brassicacea, EWM_70) | Y | S | Rashad, thafa (،داشر ءافث) | Seed | Gynaecological, musculoskeletal, skin, digestive, endocrine and nutritional, neurological, general and unspecified, cardiovascular | Ground, infusion, no preparation | Oral ingestion (eat or drink), poultice | Not to be used for over a month, nor by pregnant women, overdose may cause diarrhoea and upset stomach | 13 | 0.228 |
| Linum usitatissimum L. (Linaceae, EWM_13) | Y | – | Bidharrat alkitan (ةرذب ناتكلا) | Seed | Digestive, endocrine and nutritional, general and unspecified, gynaecological | Ground, infusion | Oral ingestion (eat or drink) | Can cause stomach and abdominal pain, and gases | 4 | 0.079 |
| *Lupinus albus L. (Fabaceae, EWM_91) | N | F | Tarmas (سمرت) | Seed | Neurological, endocrine and nutritional, blood and immune system | With food, infusion, decoction | Oral ingestion (eat or drink) | Overdose may cause phlegm and skin yellowing | 4 | 0.035 |
| Lycopersicon esculentum Mill. (Solanaceae, NA) | N | F | Tamatum (مطامط) | Fruit | Blood and immune system | No preparation | Oral ingestion (eat) | Overdose may cause diarrhoea | 1 | 0.023 |
| Malva parviflora L. (Malvaceae, EWM_39) | Y | – | Khabiza (ةزيبخ) | Leaf, flower | Family planning, general and unspecified, respiratory | Infusion, no preparation | Chewing, oral ingestion (drink) | N | 1 | 0.002 |
| Matricaria aurea (L.) Sch. Bip. (Asteraceae, EWM_07) | Y | – | Babunj (جنوباب) | Flower | General and unspecified, neurological, cardiovascular, digestive, respiratory | Infusion | Inhale, oral ingestion (drink) | Overdose may cause dizziness or headache | 9 | 0.134 |
| *Melissa officinalis L. (Lamiaceae, EWM_52) | N | – | Malisaa (اسيلم) | Leaf | Digestive | Infusion | Oral ingestion (drink) | Not to be used by pregnant women or children | 1 | 0.019 |
| Mentha sp. (Lamiaceae, EWM_59) | Y | – | Nena (عانعن) | Leaf | Digestive, cardiovascular, general and unspecified, neurological, respiratory, gynaecological | Decoction, infusion | Oral ingestion (drink) | N | 16 | 0.289 |
| Morus nigra L. (Moraceae, EWM_95) | N | F | Waraq tawt (توت قرو) | Leaf | Family planning | Decoction | Oral ingestion (drink) | N | 1 | 0.013 |
| *Musa acuminata Colla (Musaceae, NA) | N | F | Moz (زوم) | Fruit | Digestive | No preparation | Oral ingestion (eat) | N | 1 | 0.029 |
| Myrtus communis L. (Myrtaceae, EWM_92) | Y | – | Waraq alas (سلاا قرو) | Leaf | General and unspecified, respiratory, blood and immune system, cardiovascular | Decoction, infusion | Oral ingestion (drink) | N | 2 | 0.022 |
| Nigella sativa L. (Ranunculaceae, EWM_22) | N | S | Haba sawda (ةبح ءادوس) | Seed | Blood and immune system, general and unspecified, respiratory, gynaecological, musculoskeletal, neurological | Ground, 7 seeds with honey or dates, no preparation | Oral ingestion (eat or drink) | Not to be used by pregnant women, children, or babies, if more than 7 seeds are taken in a day, it can cause abortion, overdose may affect the kidneys | 13 | 0.201 |
| Ocimum basilicum L. (Lamiaceae, EWM_71) | N | – | Rihan (ناحير) | Leaf, flower | General and unspecified, respiratory | Infusion | Oral ingestion (drink) | N | 1 | 0.006 |
| Ocimum sp. (Lamiaceae, EWM_23) | Y | – | Habaq (قبح) | Leaf | General and unspecified, digestive | Decoction, infusion | Oral ingestion (drink) | Not to be used by pregnant women or children | 3 | 0.04 |
| Olea europaea L. (Oleaceae, EWM_101) | Y | F | Zeetoun (نوتيز) | Oil, leaf | General and unspecified, endocrine and nutritional, respiratory | Syrup, liniment, infusion, decoction | Oral ingestion (eat or drink), liniment | If boiled (leaves) may become toxic, overdose may cause diarrhoea | 5 | 0.086 |
| *Origanum majorana L. (Lamiaceae, EWM_11) | N | – | Bardaqush (شوقدرب) | Leaf | Endocrine and nutritional, urological, digestive, musculoskeletal, cardiovascular | Infusion, decoction | Oral ingestion (drink) | N | 5 | 0.078 |
| *Pennisetum glaucum (L.) R.Br. (Poaceae, EWM_15) | Y | F | Dakhun (نخد) | Seed | Digestive | Ground | Oral ingestion (eat) | N | 1 | 0.015 |
| Petroselinum crispum (Mill.) Fuss (Apiaceae, EWM_10) | N | F | Baqdunas (سنودقب) | Leaf | Cardiovascular, urological, female, gynaecological, blood and immune system, musculoskeletal, skin | Infusion, ground, decoction, juice, no preparation | Oral ingestion (eat or drink), wash | Overuse may cause skin irritation | 10 | 0.163 |
| Phoenix dactylifera L. (Arecaceae, NA) | Y | F | Nakhel, tamr (،ليخن رمت) | Fruit, seed | Family planning, digestive | Ground, in hot milk or honey | Oral ingestion (drink) | N | 1 | 0.012 |
| Pimpinella anisum L. (Apiaceae, EWM_96) | N | S | Yansun (نوسناي) | Seed | Digestive, gynaecological, respiratory, general and unspecified, urological, neurological | Decoction, infusion | Oral ingestion (drink) | Overdose may cause abdominal distension | 21 | 0.559 |
| Piper nigrum L. (Piperaceae, EWM_20) | N | S | Flfl aswad, flfl abyad (،دوسا لفلف, ضيبا لفلف) | Fruit | Respiratory, gynaecological, digestive, urological | Ground | Oral ingestion (eat or drink) | Overdose may cause heartburn | 6 | 0.084 |
| Pistacia lentiscus L. (Anacardiaceae, EWM_57) | N | – | Mustaka (اكتسم) | Resin | General and unspecified, musculoskeletal | In small pieces on a gauze with lemon | Poultice | N | 1 | 0.008 |
| *Prunus mahaleb L. (Rosaceae, EWM_55) | N | F | Mhallab (بلحم) | Seed | Digestive, general and unspecified | Ground, infusion | Rubbed on gums, topic, oral ingestion (drink), poultice | N | 4 | 0.069 |
| *Psidium guajava L. (Myrtaceae, EWM_94) | N | F | Waraq jawwafa (قرو ةفاوج) | Leaf | General and unspecified, respiratory, neurological | Decoction, infusion | Oral ingestion (drink) | N | 7 | 0.106 |
| Punica granatum L. (Lythraceae, EWM_72) | N | F | Roman (نامر) | Peel | Digestive, skin, gynaecological | Ground, decoction | Oral ingestion (eat), poultice, topic | N | 7 | 0.103 |
| Rhazya stricta Decne. (Apocynaceae, EWM_30) | Y | – | Harmal (لمرح) | Leaf, root | General and unspecified, digestive | Decoction, ground, infusion | Oral ingestion (drink) | Can cause dizziness and sleeping problems, overdose can be toxic | 4 | 0.08 |
| *Rheum sp. (Polygonaceae, EWM_69) | Y | – | Raoud (دنوار) | Leaf, root | Digestive | Infusion | Oral ingestion (drink) | Not to be used by pregnant or breastfeeding women, or people with kidney problems | 1 | 0.017 |
| Ricinus communis L. (Euphorbiaceae, EWM_45) | Y | – | Khurue (عورخ) | Seeds, oil | Digestive, musculoskeletal, skin | Liniment, in juice | Oral ingestion (drink) | Not to be used by pregnant women | 2 | 0.033 |
| *Rosmarinus officinalis L. (Lamiaceae, EWM_03) | N | – | Aklel aljabal (ليلكا لبجلا) | Leaf | Respiratory, general and unspecified, digestive, neurological, cardiovascular | Ground, infusion | Oral ingestion (eat or drink), decoction (steam inhalation) | Not to be used by pregnant women or patients with blood pressure problems | 6 | 0.1 |
| Ruta chalepensis L. (Rutaceae, EWM_84) | Y | – | Shathab (باذش) | Leaf | Neurological, ear, respiratory | Decoction | Oral ingestion (drink) | Overdose may cause sleepiness, cirrhosis, abortion | 1 | 0.024 |
| *Salix mucronata Thunb. (Salicaceae, EWM_76) | Y | – | Safsaf (فاصفص) | Leaf | Musculoskeletal | Infusion | Oral ingestion (drink) | N | 1 | 0.003 |
| *Salvia officinalis L. (lamiaceae, EWM_56) | N | – | Miramia (ةيماريم) | Leaf | General and unspecified, digestive, gynaecological, neurological | Decoction, infusion | Oral ingestion (drink), mouthwash | Not to be used during menstruation, increases production of milk | 5 | 0.106 |
| Senna alexandrina Mill. (Fabaceae, EWM_78) | Y | – | Sana maki (يكم انس) | Leaf | Digestive, gynaecological | Decoction | Oral ingestion (drink) | Dry, not to be used by pregnant and breastfeeding women | 8 | 0.195 |
| Sesamum indicum L. (Pedaliaceae, EWM_89) | Y | F | Smsm (مسمس) | Seed | Neurological, endocrine and nutritional | In food, ground, no preparation | Oral ingestion (eat) | N | 2 | 0.039 |
| *Solenostemma argel (Delile) Hayne (Apocynaceae, EWM_29) | N | – | Hargal (لجرح) | Leaf | Musculoskeletal, digestive, blood and immune system, endocrine and nutritional | Ground, in water | Topic, oral ingestion (drink) | Not to be used by pregnant or breastfeeding women | 2 | 0.042 |
| *Spinacia oleracea L. (Amaranthaceae, EWM_80) | N | F | Sbanekh (خنابس) | Leaf | Blood and immune system, digestive, general and unspecified | With food | Oral ingestion (eat) | N | 4 | 0.052 |
| Syzygium aromaticum (L.) Merr. & Perry (Myrtaceae, EWM_66) | N | S | Qrnfol (لفنورق) | Flower bud | Digestive, general and unspecified, endocrine and nutritional, neurological, blood and immune system | Ground, infusion | Oral ingestion (drink), put directly on teeth | Overdose may upset the stomach, not to be used by people with liver problems | 14 | 0.22 |
| Tamarindus indica L. (Fabaceae, NA) | Y | F | Tamrr hindi, homar (رمت رمح ،يدنه) | Fruit | General and unspecified, digestive, skin | In water, decoction | Oral ingestion (drink), poultice | N | 2 | 0.034 |
| Thymus vulgaris L. (Lamiaceae, EWM_98) | N | – | Zaetir (رتعز) | Leaf | General and unspecified, respiratory, digestive, gynaecological, cardiovascular, neurological | In water or tea, decoction, infusion, in food | Oral ingestion (eat or drink) | Overdose may cause digestion | 7 | 0.114 |
| Trachyspermum ammi (L.) Sprague (Apiaceae, EWM_58) | Y | S | Nankha (ةخنان) | Seed | Digestive, musculoskeletal, gynaecological | Ground | Oral ingestion (eat or drink) | Overdose may cause constipation | 7 | 0.062 |
| Trigonella foenum-graecum L. (Fabaceae, EWM_31) | Y | S | Helba (ةبلح) | Seed | Family planning, digestive, gynaecological, musculoskeletal, blood and immune system, endocrine and nutritional, urological, respiratory, general and unspecified | Ground in milk, decoction, infusion | Oral ingestion (drink) | Use is not recommended for children under 2, overdose may cause nausea or overweight | 24 | 0.56 |
| *Triticum aestivum L. (Poaceae, EWM_32) | N | F | Janen alqmah (نينج حمقلا) | Seed | Neurological, cardiovascular | Ground | Oral ingestion (eat) | Overdose may cause overweight | 1 | 0.022 |
| *Vigna radiata (L.) R. Wilczek (Fabaceae, EWM_54) | N | F | Mash (شام) | Seed | Neurological, general and unspecified, blood and immune system, musculoskeletal, endocrine and nutritional | With food, ground, decoction | Oral ingestion (eat or drink) | Can cause overweight | 8 | 0.1 |
| *Viola sp. (Violaceae, EWM_08) | Y | – | Banafsj (جسفنب) | Leaf, flower | Respiratory | No preparation | Sublingual, chewing | N | 1 | 0.031 |
| Vitis sp. (Vitaceae, EWM_97) | N | F | Zabib (بيبز) | Fruit | Blood and immune system, neurological, endocrine and nutritional | In food, with juice | Oral ingestion (eat or drink) | N | 5 | 0.086 |
| Zingiber officinale Roscoe (Zingiberaceae, EWM_100) | N | S | Zanajabil (ليبجنز) | Root | General and unspecified, musculoskeletal, digestive, endocrine and nutritional, cardiovascular, respiratory, neurological, blood and immune system | Decoction, infusion, ground | Oral ingestion (drink) | Overdose may cause heartburn or skin reactions | 18 | 0.294 |
| Ziziphus spina-christi (L.) Desf. (Rhamnaceae, EWM_75) | Y | – | Sader (ردس) | Leaf | Skin | Infusion, ground | Wash | N | 2 | 0.015 |
| Not identified (Cupressaceae, EWM_65) | – | – | Qatiran (نارطق) | Oil | Skin | Liniment | Topic | N | 1 | 0.005 |
| Not identified (EWM_79) | – | – | Saq alhamam, khawa jawa (قاس ،مامحلا اوجاوخ) | Root | Skin | Ground | Poultice | N | 2 | 0.049 |
| Not identified (EWM_48) | – | – | Krela (لايرك) | Fruit | Endocrine and nutritional | Ground | Oral ingestion (eat) | N | 1 | 0.031 |
The modes of preparation and administration for each plant can be found in Table 2. The most used plant parts are leaves (35%), fruits (21%) and seeds (18%). Underground parts (9%), flowers (8%), resin (5%), oil (2%), the whole plant (2%) and bark (1%) are also used. Infusion is the most used mode of preparation (26%), followed by decoction (22%), grinding (22%), mixing with food (7%) and maceration (6%). Plants are sometimes used as they were sourced without any (further) preparation process (5%), juiced (4%) or mixed with dates (2%), milk (1%), honey (1%) or fruits (1%). The most popular modes of administration are oral ingestion as a drink (63%) and eaten (21%). Plants are also administered as poultices (7%) or applied directly on the teeth (2%). They are rarely (1%) used in mouthwash, fumigation and lotions, inhaled, chewed, rubbed or used as washes.
A total of 67 mixtures were documented including combinations of two to four plant ingredients (Table 3). Forty-four medicinal plants (40%) were sometimes used in the mixtures. The medicinal plants most commonly used in mixtures are Ziziphus spina-christi (zanajabil) cited in 17 mixtures and Pimpinella anisum (yansun), Mentha sp. (nena) and Citrus sp. (limon) each cited in 10 mixtures. The most common mixtures are the combination of Pimpinella anisum, Carum carvi and Foeniculum vulgare used as a digestive, for gynaecological and urological problems; Pimpinella anisum, Cuminum cyminum and Foeniculum vulgare for digestive problems; and Trigonella foenum-graecum, Foeniculum vulgare and Pimpinella anisum for digestive, respiratory and neurological problems. Modes of administration for mixtures are limited to decoctions and infusions and dried and ground plants added to food.
Table 3.
Mixtures and combinations used by women in Mecca
| Mixture | Medicinal plants included (vernacular and scientific names) |
|---|---|
| Mix1 | Qashr albun (Coffea arabica), nakhel, tamr (Phoenix dactylifera), kamun (Cuminum cyminum) |
| Mix2 | Zeetoun (Olea europaea), limon (Citrus sp.) |
| Mix3 | Zeetoun (Olea europaea), dakhun (Pennisetum glaucum) |
| Mix4 | Yansun (Pimpinella anisum), karawia (Carum carvi), shamr (Foeniculum vulgare) |
| Mix5 | Marr (Commiphora myrrha), rashad, thafa (Lepidium sativum), haba sawda (Nigella sativa) |
| Mix6 | Shay, shay akhdar (Camellia sinensis), kamun (Cuminum cyminum) |
| Mix7 | Yansun (Pimpinella anisum), kamun (Cuminum cyminum), shamr (Foeniculum vulgare) |
| Mix8 | Nena (Mentha sp.), shay, shay akhdar (Camellia sinensis), zanajabil (Zingiber officinale) |
| Mix9 | Karawia (Carum carvi), helba (Trigonella foenum-graecum), kamun (Cuminum cyminum) |
| Mix10 | Nena (Mentha sp.), shay, shay akhdar (Camellia sinensis) |
| Mix11 | Qrnfol (Syzygium aromaticum), hal (Elettaria cardamomum), qashr albun (Coffea arabica) |
| Mix12 | Yansun (Pimpinella anisum), shamr (Foeniculum vulgare) |
| Mix13 | Helba (Trigonella foenum-graecum), shamr (Foeniculum vulgare), yansun (Pimpinella anisum) |
| Mix14 | Qashr albun (Coffea arabica), shamr (Foeniculum vulgare), yansun (Pimpinella anisum), haba sawda (Nigella sativa) |
| Mix15 | Nena (Mentha sp.), limon (Citrus sp.), zanajabil (Zingiber officinale) |
| Mix16 | Limon (Citrus sp.), kamun (Cuminum cyminum) |
| Mix17 | Yansun (Pimpinella anisum), bardaqush (Origanum majorana) |
| Mix18 | Marr (Commiphora myrrha), karrakum (Curcuma longa) |
| Mix19 | Marr (Commiphora myrrha), haba sawda (Nigella sativa), shamr (Foeniculum vulgare), nankha (Trachyspermum ammi) |
| Mix20 | Zanajabil (Zingiber officinale), shay, shay akhdar (Camellia sinensis) |
| Mix21 | Zanajabil (Zingiber officinale), qashr albun (Coffea arabica) |
| Mix22 | Nankha (Trachyspermum ammi), kozbra (Coriandrum sativum) |
| Mix23 | Nena (Mentha sp.), bardaqush (Origanum majorana), habaq (Ocimum sp.) |
| Mix24 | Marr (Commiphora myrrha), shay, shay akhdar (Camellia sinensis) |
| Mix25 | Zanajabil (Zingiber officinale), karrakum (Curcuma longa) |
| Mix26 | Kaff maryam (Anastatica hierochuntica), halatayta (Ferula assa-foetida), marr (Commiphora myrrha) |
| Mix27 | Basham (Commiphora gileadensis), roman (Punica grantum), qrnfol (Syzygium aromaticum) |
| Mix28 | Nena (Mentha sp.), zanajabil (Zingiber officinale) |
| Mix29 | Aklel aljabal (Rosmarinus officinalis), zanajabil (Zingiber officinale) |
| Mix30 | Limon (Citrus sp.), zanajabil (Zingiber officinale) |
| Mix31 | Limon (Citrus sp.), nena (Mentha sp.) |
| Mix32 | Qrnfol (Syzygium aromaticum), haba sawda (Nigella sativa), zanajabil (Zingiber officinale) |
| Mix33 | Haba sawda (Nigella sativa), qurfa (Cinnamomum verum) |
| Mix34 | Qrnfol (Syzygium aromaticum), hal (Elettaria cardamomum) |
| Mix35 | Qrnfol (Syzygium aromaticum), hana (Lawsonia inermis) |
| Mix36 | Basham (Commiphora gileadensis), adhkhur (Cymbopogon schoenanthus) |
| Mix37 | Zanajabil (Zingiber officinale), qurfa (Cinnamomum verum) |
| Mix38 | Nena (Mentha sp.), limon (Citrus sp.), zanajabil (Zingiber officinale) |
| Mix39 | Yansun (Pimpinella anisum), shay, shay akhdar (Camellia sinensis), nena (Mentha sp.) |
| Mix40 | Zanajabil (Zingiber officinale), flfl abyad, flfl aswad (Piper nigrum) |
| Mix41 | Zanajabil (Zingiber officinale), limon (Citrus sp.), qashr albun (Coffea arabica) |
| Mix42 | Sana maki (Cassia senna), tamrr hindi, homar (Tamarindus indica) |
| Mix43 | Nankha (Trachyspermum ammi), kamun (Cuminum cyminum), shamr (Foeniculum vulgare) |
| Mix44 | Kamun (Cuminum cyminum), karrakum (Curcuma longa) |
| Mix45 | Nankha (Trachyspermum ammi), kamun (Cuminum cyminum), shamr (Foeniculum vulgare), haba sawda (Nigella sativa) |
| Mix46 | Bsal (Allium cepa), limon (Citrus sp.) |
| Mix47 | Helba (Trigonella foenum-graecum), yansun (Pimpinella anisum), shamr (Foeniculum vulgare) |
| Mix48 | Haba sawda (Nigella sativa), yansun (Pimpinella anisum), qrnfol (Syzygium aromaticum) |
| Mix49 | Qashr albun (Coffea arabica), zanajabil (Zingiber officinale) |
| Mix50 | Hargal (Solenostemma argel), raond (Rheum sp.) |
| Mix51 | Zanajabil (Zingiber officinale), qurfa (Cinnamomum verum) |
| Mix52 | Zanajabil (Zingiber officinale), nena (Mentha sp.), kamun (Cuminum cyminum) |
| Mix53 | Nena (Mentha sp.), helba (Trigonella foenum-graecum) |
| Mix54 | Qrnfol (Syzygium aromaticum), qurfa (Cinnamomum verum), zanajabil (Zingiber officinale), hal (Elettaria cardamomum) |
| Mix55 | Helba (Trigonella foenum-graecum), mash (Vigna radiata) |
| Mix56 | Yansun (Pimpinella anisum), habaq (Ocimum sp.) |
| Mix57 | Qashr albun (Coffea arabica), qurfa (Cinnamomum verum) |
| Mix58 | Portokal (Citrus sinensis), limon (Citrus sp.) |
| Mix59 | Mhallab (Prunus mahaleb), hana (Lawsonia inermis), qrnfol (Syzygium aromaticum) |
| Mix60 | Qashr albun (Coffea arabica), qurfa (Cinnamomum verum), qrnfol (Syzygium aromaticum) |
| Mix61 | Nim (Azadirachta indica), harmal (Rhazya stricta), sader (Ziziphus spina-christi) |
| Mix62 | Nankha (Trachyspermum ammi), limon (Citrus sp.) |
| Mix63 | Nankha (Trachyspermum ammi), qashr albun (Coffea arabica) |
| Mix64 | Nankha (Trachyspermum ammi), haba sawda (Nigella sativa), rashad, thafa (Lepidium sativum) |
| Mix65 | Rashad, Thafa (Lepidium sativum), nakhel, tamr (Phoenix dactylifera) |
| Mix66 | Haba sawda (Nigella sativa), nakhel, tamr (Phoenix dactylifera) |
| Mix67 | Hargal (Solenostemma argel), raond (Rheum sp.), hndba (chicory), aomloj (Phyllanthus cf.) |
Ailments treated with medicinal plants by women in Mecca and remarks on side effects
Medicinal plant uses were documented for 13 etic therapeutic use categories (Table 4). Almost half of the use reports referred to digestive, general and unspecified and respiratory issues, which are common children’s, as well as adult’s, complaints, but do not reflect the most important diseases afflicting the Saudi Arabian population (cardiovascular diseases, diabetes, neuro-psychiatric conditions and injuries [57]). Gynaecological problems, which encompass menstrual cramps and other menstrual disorders, polycystic ovaries, pregnancy and postpartum issues, are fourth in importance both in number of use reports and number of plant taxa used.
Table 4.
Use reports and number of taxa used for each therapeutic use category
| Emic therapeutic use category | Number of use reports | Number of plant taxa |
|---|---|---|
| Digestive | 215 | 67 |
| General and unspecified | 96 | 43 |
| Respiratory | 70 | 32 |
| Gynaecological | 60 | 29 |
| Endocrine and nutritional | 53 | 24 |
| Blood and immune system | 50 | 21 |
| Neurological | 48 | 29 |
| Musculoskeletal | 38 | 16 |
| Cardiovascular | 36 | 19 |
| Urological | 36 | 17 |
| Skin | 34 | 16 |
| Family planning | 15 | 9 |
| Ear | 2 | 2 |
Informants indicated potentially toxic or side effects for almost half of the medicinal plants (n = 52, 47%), often associated with inappropriate use (especially overdosing; Table 2). Many observations on plants’ side effects or toxicology made by informants referred to the negative effects of plants on pregnant or breastfeeding women (53% of the plants with noted side effects), or children (11%), and as causing digestive issues (37%) amongst other problems (30%).
Acquiring medicinal plant knowledge and choosing health care
Social and family networks, as well as mass media, were the two sources of medicinal plant knowledge mentioned by the Meccan women interviewed, who were all responsible for the household health. The same sources have been documented for herbal knowledge among the population of Riyadh [33]. Most elderly women interviewed mentioned that they had learned about medicinal plants from their mothers, grandmothers and neighbours (Table 1). Mecca’s everyday social interactions among women provide plenty of opportunities for the younger generation to learn from older women’s experience about medicinal plant use. Informant 18 (age 60, housewife) mentioned: ‘We always encourage our daughters to help us in the preparation of medicinal plants from early age’. Although some younger women interviewed acknowledged learning about medicinal plant knowledge from their elders, written sources, such as popular books on medicinal plants, were also mentioned as sources of medicinal plant knowledge (Table 1). Women of all ages also mentioned television programs as a source of knowledge about medicinal plants; mass media is put forward by biomedical practitioners as a tool for educational programs to modernise health concepts and make aware of available treatments among the poorly educated [34].
Overall, most of the women interviewed (n = 21, 66%) preferred to use medicinal plants rather than biomedicine, but others (n = 11, 34%) preferred biomedicine. Medicinal plants were more often preferred by older than younger women (Table 1). However, preference for medicinal plants also varied depending on the ailment that needed treating. Plants were often preferred to treat general malaise, digestive, respiratory, nutritional, neurological, musculoskeletal, cardiovascular, urological, skin and pregnancy-related ailments, some gynaecological problems and anaemia. The women interviewed preferred to use biomedicine in cases of psychological illnesses, eye problems, cancer, unusual gynaecological bleeding, wounds and infectious diseases. Often, they would prefer biomedicine when they suffer an illness for the first time but use medicinal plants for minor, common or chronic ailments. Informant 22 (45 years old) explained: ‘I usually prefer to use medicinal plants to treat my family for diseases that happen continuously such as headache, abdominal pains and menstruation, as well as those that occur due to climate changes such as flu and cough. I use biomedical resources with infectious and psychological diseases, such as depression’. A similar observation was made by Ghazanfar [36] when describing medicinal plant use in the Arabian Peninsula as a whole.
Medicinal plants used among urban, Muslim women are vastly under-documented
Four books and seven scientific articles published between 1985 and 2014 were retrieved from the literature search (Table 5). Most literature sources on medicinal plants from Saudi Arabia did not provide information on the ethnobotanical methods used nor cite robust plant identification procedures (Table 5), including six studies that did not mention the geographical area in which they were conducted. Of the 11 studies reviewed, plants were identified by experts in nine of them and only four cited one or more botanical keys used to identify collected taxa; eight studies reported the collection of voucher specimens. However, only four of these eight studies reported the voucher numbers in the publications. Four of the studies were identified as rigorous, hence suitable to compare with medicinal plant uses with the list of medicinal plants collected during fieldwork: Ghazanfar [36], Al-Sodany et al. [41], El-Ghazali et al. [58] and Abdulafatih [59] (Table 5). Although studies were selected if there was evidence for accurate plant identification, several plant synonyms were found to be used in these publications (according to The Plant List [54]) and misspelled plant names were not infrequent. Three plant names (8%) used in these literature sources could not be found when cross-checking with The Plant List [54], and six plants cited were identified only at the genus level.
Table 5.
Reviewed Saudi Arabian medicinal plant literature
| Reference | Study area | N plant species identified | Ethnobotanical data collection | Botanical keys used | Botanical identification by experts | Herbaria | Vouchers | Voucher numbers reported |
|---|---|---|---|---|---|---|---|---|
| Shalaby et al (1985)—book in English [68] | Not specified | 160 | Fieldwork to collect plant specimens and records local names | Yes | Yes | Umm Al-Qura University | No | No |
| Mossa et al (1987)—book in English [35] | Not specified | 150 | Not reported | No | No | King Saud University | No | No |
| Abdulafatih (1987)—journal article in English [59] | Asir region and surrounding areas (SW KSA) | 61 | Fieldwork documentation: local names, plant parts used and medicinal uses, reported | No | Yes | King Saud University (College of Education, Abha Branch) | Yes | Yes |
| Al-Yaha et al (1990)—book in English [63] | Not specified | 150 | Not reported | No | Yes | King Saud University | Yes | No |
| Ghazanfar (1994)—book in English [36] | Arabian peninsula | 260 | Fieldwork documentation and literature sources (1982–1993) | No | Yes | Sultan Qaboos University (Department of Biology; Sultanate of Oman) | Yes | No |
| Rahman et al (2004)—journal article in English [69] | Not specified | 254 | Literature and herbarium sources (College of Pharmacy, King Saud University, National Herbarium of Saudi Arabia) | No | No | King Saud University (College of Pharmacy, King Saud University, National Herbarium of Saudi Arabia) | Yes | No |
| El-Ghazali et al (2010)—journal article in English [58] | Al-Rass province, Qassim area | 47 | Fieldwork documentation: interviews with local healers and knowledgeable Bedouin; local names, plant parts used and medicinal uses, reported | No | Yes | Qassim University (Museum of Science, College of Science and Arts, Al-Rass) | Yes | Yes |
| Al-Sodany et al (2013)—journal article in English [41] | Taif | 261 (165 medicinal) | Fieldwork documentation: interviews with local environments. Literature review | Yes | Yes | Kafr El-Sheikh University (Herbarium of Biology Department, Faculty of Science, Taif) | Yes | No |
| Youssef (2013)—journal article in English [70] | Qassim and central Saudi Arabia | 83 | Fieldwork documentation: open-ended interviews. Literature review | Yes | Yes | Qassim University | No | No |
| Shahat et al (2015)—journal article in English [71] | Tanhat protected area, Riyadh | 7 | Not reported | No | Yes | King Sud University (Medicinal and Aromatic Plants Research Department, National Research Centre; Herbarium of the Faculty of Pharmacy) | Yes | Yes |
| Yusuf et al (2014)—journal article in English [72] | Not specified | 61 | Literature review | Yes | Yes | King Saud University (Herbarium of the College of Pharmacy) | Yes | Yes |
The four selected literature sources, all documenting medicinal plant knowledge in rural areas, cited 486 different medicinal plant species, compared to the 95 plants we identified at the species level cited by the 32 women interviewed (Table 2). Combining literature and fieldwork sources results in 525 different species used in Saudi Arabia in total. Five plants identified at the genus level were also new citations of these genera used medicinally in Saudi Arabia. Table 6 presents a comparison between Meccan women’s knowledge and each literature source (taking into account only the plants that could be identified at the species level). Medicinal plants known to the Meccan women interviewed contributed 7.4% of the total list: 39 species (41%) cited by women in Mecca were not reported in the selected Saudi Arabian medicinal plant literature (Table 6; indicated by ‘*’ in Table 5), whereas 56 species (59%) had been previously documented. Of the 56 species already cited in the literature, we documented new vernacular names for nine plants (10%). Forty plants were documented in the literature and were cited for different therapeutic applications by the Meccan women interviewed in this study.
Table 6.
Comparison of medicinal plants used by Meccan women (MW) identified at the species level (n = 95) with the inventories from selected literature sources. NA indicates that a source did not provide vernacular names or therapeutic uses
| Reference (rural/urban) | Total number of species listed | New citations by MW | Species with different vernacular names | Species with different therapeutic uses |
|---|---|---|---|---|
| Abdulafatih 1987 (rural) [59] | 61 | 81 (85%) | 84 (88%) | 85 (89%) |
| Al-Sodany et al. 2013 (rural) [41] | 165 | 82 (86%) | NA | NA |
| El-Ghazali et al. 2010 (rural) [58] | 47 | 87 (92%) | 88 (93%) | 90 (95%) |
| Ghazanfar 1994 (not specified) [36] | 260 | 43 (45%) | 53 (56%) | 55 (58%) |
| Total literature | 486 | 39 (41%) | 48 (51%) | 79 (83%) |
Discussion
Edible, traded and Muslim medicinal plants
Urbanisation is often considered an aspect of modernisation that leads to the erosion of medicinal plant knowledge [6], but urban contexts may have vibrant medicinal plant use traditions [3–7]. In the Middle East, urban male herbalists are acclaimed for their specialist medicinal plant knowledge [43]. In this study, we evidence a rich body of female, lay medicinal plant knowledge, supporting the observation by Elolemy and AlBedah [33] that women commonly use herbal therapies in Saudi Arabian cities. Although only 32 Meccan women participated in this study, more than 100 medicinal plants were documented to treat a wide range of health complaints. The knowledge held by women in cities is markedly different from knowledge previously documented, with 41% of the plants cited by Meccan women not in the literature we sourced. This points to the under-documentation of knowledge of medicinal plants in Saudi Arabia but cannot be attributed to male versus female knowledge or urban versus rural knowledge in the absence of further studies. Existing studies may also exclude foods, spices and culinary herbs from ethnobotanical listings of medicinal plants, making less visible knowledge held by women and contributing to the difference we find between published studies and our results.
A third (32%) of the medicinal plants used by the Meccan women interviewed are food plants. Salient food plants cited in this study include onion, celery, cabbage, coriander, lemon, olive oil and dates (Table 2). The use of food plants as medicines by urban populations is widespread [6] and may be due to the easy access to these plants. Medicinal foods are also an important feature of the Mediterranean medical tradition, observed specifically in the Greek Hippocratic texts that influenced Dioscorides’ Materia Medica [60], which in turn influenced Arabic medicinal texts [36]. Specific health beliefs associated with foods have also been observed in Arabia [36]. Along with food plants, many medicinal plants reported are spices (17%), which have played a double role as flavouring and medicinal products since the Middle Ages [61]. The most salient medicinal plants identified here are also all spices (Trigonella foenum-graecum, Cuminum cyminum, Pimpinella anisum, Cinnamomum verum and Zingiber officinale). Spices are both grown in the Middle East and imported from Africa and Southeast Asia (including plants from the Zingiberaceae, Piperaceae, Theaceae, Costaceae, Fucaceae and Musaceae families). This use of imported spices may be a legacy from trade Roman times, when black pepper, ginger, turmeric and cardamom were transported from Southeast Asia into the Mediterranean through Arabian incense trade routes [18, 20]. Moreover, medicinal plant use in urban environments biased towards exotic plants has been observed in Brazil [5] and could also be attributed to easier access to these plants in urban areas. The important use of foods and spices medicinally in cities may be a global characteristic of urban ethnobotanical knowledge, since these are often easily available in urban environments.
Plant availability is a key factor shaping traditional plant use. In urban areas, this does not necessarily reflect the region’s native plant diversity but the plant diversity traded and available in shops and markets. Differences in plant availability between rural and urban contexts may also account for the differences in plant lists reported in this study and published literature. El-Ghazali et al. [58] observed that native plants used by rural populations in Al-Rass province are not traded in domestic markets, and traded plants in shops and markets form the bulk of the medicinal plants available to Meccan women.
Food plants and spices represented half of the medicinal plants used by the Meccan women interviewed (49%), and many of these are plants cited in the Quran or the Hadith. Among Muslims, knowledge of a plant being mentioned in the Quran is often sufficient to validate its medicinal use [62]. Some medicinal plants cited in interviews are mentioned in the ‘the Medicine of the Prophet’: helba (Trigonella foenum-graecum), haba sawda (Nigella sativa), safarjil (Cydonia oblonga), rashad (Lepidium sativum), hana (Lawsonia inermis), zanajabil (Zingiber officinale), sana (Senna alexandrina), khull (Ammi visnaga) and sabr (Aloe vera), according to the list provided by Al-Yahya [63]. Of these, only safarjil (Cydonia oblonga) had not been documented already in the Saudi Arabian medicinal plant literature, which indicates a widespread influence of the Hadith in traditional Saudi Arabian medicine both in urban and rural environments. Moreover, the common use of mixtures among the research participants matches the recommendation made in ‘the Medicine of the Prophet’ that ‘city dwellers’ require the use of compound drugs (according to Deuraseh [39]). Specific modes of administration recorded among women in Mecca are also recommended by prophetic medicine [37], specifically the use of food, milk, honey and dates as excipients. This further evidences the influence of Islamic medicine in lay medicinal plant use.
Dynamic female knowledge
As in other Islamic countries, Meccan women are responsible for dealing with most health issues within the household and their medicinal plant knowledge is gender-specific. Gynaecological problems were frequently mentioned and toxicology and remarks about side effects often concerned women’s reproductive or children’s health, which are all references to gender-specific knowledge.
Meccan women may learn about medicinal plants from their family and social networks, but increasingly, written sources and mass media are becoming important sources of knowledge. This, along with a higher preference for biomedical services amongst the younger generation, could result in the erosion of medicinal plant knowledge. Ethnobotanical knowledge erosion has been observed in the Middle East both among herbalists [43] and the general population [36]. The diffusion of non-local knowledge about medicinal plants through mass media is characteristic to urban settings [64] and has a homogenizing effect on oral pharmacopoeias [65]. Mass media often disseminates information on the uses and properties of commercial plants, increasing their visibility [66] and, alongside availability factors, could also contribute to explain the high proportion of food and spices used among the Meccan women interviewed.
Mass media is also used in Saudi Arabia to communicate biomedical education programs [34]. Although these campaigns may be necessary, they favour biomedical knowledge over traditional therapies. Loss of ethnomedicinal and ethnobotanical knowledge may result from different treatment preferences between generations. Higher preference for biomedical treatments among younger Meccan women reflects the same trend among rural Arabic populations elsewhere in Saudi Arabia [36, 43, 58]. Although Press [2] argues that the disregard of faith and the role of family in biomedical diagnosis and treatment are often sufficient to hamper the utilisation of biomedicine, Ghazanfar notes that in the Arabian Peninsula, ‘modern and traditional medicine may be tried [simultaneously], or if one fails the other will be tried – but where modern medicine achieves results, traditional medicine tends to disappear’ [36, p. 1]. Biomedicine in Islamic countries integrates faith and has a religious viewpoint on caring [38], but people may still prefer home remedies for treating minor ailments [30, 36] as observed in this study. Even when biomedicine is growing and herbal remedies may be in decline, medicinal plant use still plays an important role in urban health care [2, 29, 30].
Conclusion
We join Emery and Hurley [67] in highlighting the vibrant botanical knowledge and practices in urban areas. Women in Mecca are the primary household health carers and hold a singular, lay body of medicinal plant knowledge to treat mostly common ailments. Plant availability in shops and markets, as well as religious texts, seem to play an important role shaping the urban medicinal flora of women in Mecca; we highlight the important medicinal role in urban environments of foods, spices and traded plants in general. Much of this knowledge had not yet been documented, and gender and geographical biases in research may account for the under-representation of urban women’s knowledge in Saudi Arabian medicinal plant literature.
However, medicinal plant knowledge among Meccan women may be eroded and changed with the spread of new knowledge through mass media and preference for biomedical care. Documentation efforts are urgent for the preservation of the diversity of medicinal plant knowledge in the Arabian Peninsula. We propose that scientifically rigorous ethnobotanical and ethnomedicinal research ‘acknowledging the sociocultural heterogeneity within the community being researched’ [32, p. 242] in Islamic settings can be achieved by teams with both female and male ethnobiologists. Al-Sodany et al. [41] have reported that medicinal plants in rural Saudi Arabia are vastly under-documented, but so far, ethnobotanical enquiry of women’s medicinal plants has been even more overlooked.
Acknowledgements
We are truly thankful to the 32 adult women who participated in this study and for sharing their time and knowledge. The authors would like to thank the members of the Umm Al-Qura University Herbarium and the University of Reading Herbarium (RNG) for their collaboration and support, especially Professor Kadry Abdel Khalik in the Umm Al-Qura University for validating plant identifications. We would also like to express our gratitude to the two anonymous reviewers whose comments helped improve the original manuscript.
Funding
This research has received support of the Saudi Arabian Cultural Bureau (SACB; Reference U590, Beneficiary: Afnan Mohammad Hazim Alqethami). During this research, researcher I. Teixidor-Toneu was funded by the European Union's Framework Programme for research, technological development and demonstration under grant agreement no. 606895.
Availability of data and materials
Herbarium specimens are available in the herbarium of the Umm Al-Qura University (Mecca, Saudi Arabia). All datasets on which the conclusions of the paper are based are made available as Tables 1, 2, 3 and 5 in this manuscript.
Abbreviations
- MW
Meccan women
- NA
Not available
Authors’ contributions
AA contributed to the conception and design, acquisition of the data, plant identification, analysis and interpretation of data and writing of the manuscript; JAH contributed to the conception and design, interpretation of the data and writing of the manuscript and IT-T contributed to the conception and design, analysis and interpretation of the data and writing of the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Ethics approval was obtained from the Ethics Committee of the School of Biological Sciences, University of Reading (Research Ethics Project Submission SBS15-16 11), and all participants freely consented to participate after being informed of the aims and methods of the project, as mentioned in the “Methods” section.
Consent for publication
Consent for the publication of this study was obtained verbally from all research participants. The manuscript does not include personal details, images or videos of the research participants; hence, a consent form has not been submitted.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Afnan Alqethami, Email: af14102009@hotmail.com.
Julie A. Hawkins, Email: j.a.hawkins@reading.ac.uk
Irene Teixidor-Toneu, Email: i.teixidor-toneu@reading.ac.uk.
References
- 1.United Nations . World urbanisation prospects: the 2014 revision highlights. New York: United Nations; 2014. [Google Scholar]
- 2.Press I Urban folk medicine: a functional overview. Am Anthropol. 1978;80:71–84. doi: 10.1525/aa.1978.80.1.02a00050. [DOI] [Google Scholar]
- 3.Wayland C, Walker LS. Length of residence, age and patterns of medicinal plant knowledge and use among women in the urban Amazon. J Ethnobiol Ethnomed. 2014;10:25. doi: 10.1186/1746-4269-10-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balick MJ, Kronenberg F, Ososki AL, Reiff M, Fugh-Berman A, O’Connor B, Roble M, Lohr P, Atha D. Medicinal plants used by Latino healers for women’s health conditions in New York city. Econ Bot. 2000;54:344–357. doi: 10.1007/BF02864786. [DOI] [Google Scholar]
- 5.Medeiros PM, Ladio AH, Albuquerque UP. Patterns of medicinal plant use by inhabitants of Brazilian urban and rural areas: a macroscale investigation based on available literature. J Ethnopharmacol. 2013;150:729–746. doi: 10.1016/j.jep.2013.09.026. [DOI] [PubMed] [Google Scholar]
- 6.Vandebroek I, Balick MJ. Globalisation and loss of plant knowledge: challenging the paradigm. PLoSONE. 2012;7:e37643. doi: 10.1371/journal.pone.0037643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Verma AK, Kumar M, Bussmann RW. Medicinal plants in an urban environment: the medicinal flora of Banares Hindu University, Varanasi, Uttar Pradesh. J Ethnobio Ethnomed. 2007;3:35. doi: 10.1186/1746-4269-3-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ceuterick M, Vandebroek I, Torry B, Pieroni A. Cross-cultural adaptation in urban ethnobotany: the Colombian folk pharmacopoeia in London. J Ethnopharmacol. 2007;120:342–359. doi: 10.1016/j.jep.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 9.Ososki AL, Balick MJ, Daly DC. Medicinal plants and cultural variation across Dominican rural, urban, and transnational landscapes. Travelling Cultures and Plants: Ethnobiol.Ethn. Migr. 2007;7:14–38. [Google Scholar]
- 10.Van Andel TR, Van’t Klooster CI. Medicinal plant use by surinamese immigrants in Amsterdam, the Netherlands. Travelling Cultures and Plants: Ethnobiol.Ethn. Migr. 2007;7:122–144. [Google Scholar]
- 11.Vandebroek I, Balick MJ, Yukes J, Durán L, Kronenberg F, Wade C, Ososki AL, Cushman L, Lantigua R, Mejia M, Robineau L. Use of medicinal plants by Dominican immigrants in New York City for the treatment of common health conditions: a comparative analysis with literature data from the Dominican Republic. Traveling Cultures and Plants Ethnobiol.Ethn. Migr. 2007;7:39–63. [Google Scholar]
- 12.Viladrich A. Between bellyaches and lucky charms: revealing Latinos’ plant-healing knowledge and practices in New York City. Traveling Cultures and Plants Ethnobiol.Ethn. Migr. 2007;7:64–85. [Google Scholar]
- 13.D’ Ambrosio U, Vallès J, Garnatje T. Food plants and transculturation in specialized stores at the metropolitan area of Barcelona, Spain. Córdoba: 6th International Congress of Ethnobotany. p. 2014.
- 14.Mati E, de Boer H. Ethnobotany and trade of medicinal plants in the Qaysari Market, Kurdish Autonomous Region, Iraq. J Ethnopharmacol. 2011;133:490–510. doi: 10.1016/j.jep.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 15.Van Andel T, Myren B, van Onselen S. Ghana’s herbal market. J Ethnopharmacol. 2012;140:368–378. doi: 10.1016/j.jep.2012.01.028. [DOI] [PubMed] [Google Scholar]
- 16.Jennings HM, Thompson JL, Merrell J, Bogin B, Heinrich M. Food, home and health: the meanings of food amongst Bengali women in London. J Ethnobiol Ethnomed. 2014;10:44. doi: 10.1186/1746-4269-10-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mosina GKE, Maroyi A, Potgieter MJ. Comparative analysis of plant use in peri-urban domestic gardens of the Limpopo Province, South Africa. J Ethnobiol Ethnomed. 2014;10:35. doi: 10.1186/1746-4269-10-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Groom N. Frankincense and myrrh: a study of the Arabian incense trade. London: Longman Group Ltd; 1981. [Google Scholar]
- 19.Touwaide A, Appetiti E. Knowledge of Eastern material medica (Indian and Chinese) in pre-modern Mediterranean medical traditions: a study in comparative historical ethnopharmacology. J Ethnopharmacol. 2013;148:361–378. doi: 10.1016/j.jep.2013.03.068. [DOI] [PubMed] [Google Scholar]
- 20.Van der Veen M, Morales J. The Roman and Islamic spice trade: new archeological evidence. J Ethnopharmacol. 2015;167:54–63. doi: 10.1016/j.jep.2014.09.036. [DOI] [PubMed] [Google Scholar]
- 21.Voeks RA. Are women reservoirs of traditional plant knowledge? Gender, ethnobotany and globalization in northeast Brazil. SJTG. 2007;28:7–20. [Google Scholar]
- 22.Howard P. The major importance of “minor” resources: women and plant biodiversity. London: International Institute for Environment and Development; 2003. [Google Scholar]
- 23.Coe FG, Anderson GJ. Ethnobotany of the Garífuna of eastern Nicaragua. Econ Bot. 1996;50:71–107. doi: 10.1007/BF02862114. [DOI] [Google Scholar]
- 24.Gollin L. The taste and smell of Taban Kenyah (Kenyah medicine): an exploration of chemosensory selection criteria for medicinal plants among the Kenyah Leppo’Ke of East Kalimantan, Borneo, Indonesia. PhD dissertation. Ann Arbor: Bell & Howell; 1997. [Google Scholar]
- 25.Kainer KA, Duryea ML. Tapping women’s knowledge: plant resource use in extractive reserves, Acre Brazil. Econ Bot. 1992;46:408–425. doi: 10.1007/BF02866513. [DOI] [Google Scholar]
- 26.Razafindraibe M, Kuhlman AR, Rabarison H, Rakotoarimanana V, Rajeriarison C, Rakotoarivelo N, Randrianarivony T, Rakotoarivony F, Ludovic R, Randrianasolo A, Bussmann RW. Medicinal plants used by women from Agnalazaha littoral forest (Southeastern Madagascar) J Ethnobiol Ethnomed. 2013;9:73. doi: 10.1186/1746-4269-9-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Begossi A, Hanazaki N, Tamashiro JY. Medicinal plants in the Atlantic Forest (Brazil): knowledge, use, and conservation. Hum Ecol. 2002;30:281–299. doi: 10.1023/A:1016564217719. [DOI] [Google Scholar]
- 28.Qureshi RA, Ghufran MA, Gilani SA, Yousaf Z, Abbas G, Batool A. Indigenous medicinal plants used by local women in southern Himalayan regions of Pakistan. Pak J Bot. 2009;41:19–25. [Google Scholar]
- 29.Teixidor-Toneu I, Martin GJ, Puri RK, Ouhammou A, Hawkins JA. Treating infants with frigg: linking disease aetiologies, medicinal plant use and care-seeking behaviour in southern Morocco. J Ethnobiol Ethnomed. 2017;13:4. doi: 10.1186/s13002-016-0129-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wayland C. Gendering local knowledge: medicinal plant use and primary health care in the Amazon. Med Anthropol Q. 2001;15:171–188. doi: 10.1525/maq.2001.15.2.171. [DOI] [PubMed] [Google Scholar]
- 31.Kothari B. Women and plants: gender relations in biodiversity management and conservation. London: Zed Books; 2003. The invisible queen in the plant kingdom: gender perspectives in medical ethnobotany; pp. 150–164. [Google Scholar]
- 32.Pfeiffer JM, Butz RJ. Assessing cultural and ecological variation in ethnobiological research: the importance of gender. J Ethnobiol. 2005;25:240–278. doi: 10.2993/0278-0771(2005)25[240:ACAEVI]2.0.CO;2. [DOI] [Google Scholar]
- 33.Elolemy AT, AlBedah AM. Public knowledge, attitude and practice of complementary and alternative medicine in Riyadh region, Saudi Arabia. Oman Med J. 2012;27:20–26. doi: 10.5001/omj.2012.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Al-Essa MA, Al-Mehaidib A, Al-Gain S. Parental awareness of liver disease among children in Saudi Arabia. Ann Saudi Med. 1998;18:79–81. doi: 10.5144/0256-4947.1998.79. [DOI] [PubMed] [Google Scholar]
- 35.Mossa JS, Al-Yahya MA, Al-Meshal IA. Medicinal plants of Saudi Arabia. Riyadh: King Saud University Libraries; 1987. [Google Scholar]
- 36.Ghazanfar SA. Handbook of Arabian medicinal plants. Boca Raton: CRC press; 1994. [Google Scholar]
- 37.Elgood C. Tibb-ul-Nabbi or medicine of the Prophet. Osiris. 1962;14:33–192. doi: 10.1086/368625. [DOI] [Google Scholar]
- 38.Rassool GH. The crescent and Islam: healing, nursing and the spiritual dimension. Some considerations towards an understanding of the Islamic perspectives on caring. J Adv Nurs. 2000;32:1476–1484. doi: 10.1046/j.1365-2648.2000.01614.x. [DOI] [PubMed] [Google Scholar]
- 39.Deuraseh N. Health and medicine in the Islamic tradition based on the book of medicine (Kitab Al-Tibb) of Sahih Al-Bukhari. JISHIM. 2006;5:2–14. [Google Scholar]
- 40.Greenwood B. Cold or spirits? Choice and ambiguity in Morocco’s pluralistic medical system. Soc Sci & Med. 1981;15:219–235. doi: 10.1016/0160-7987(81)90049-1. [DOI] [PubMed] [Google Scholar]
- 41.Al-Sodany YM, Salih AB, Mosallam HA. Medicinal plants in Saudi Arabia: I. Sarrwat Mountains at Taif, KSA. AJPS. 2013;6:134–145. [Google Scholar]
- 42.Yesilada E. Past and future contributions to traditional medicine in the health care system of the Middle-East. J Ethnopharmacol. 2005;100:135–137. doi: 10.1016/j.jep.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 43.Azaizeh H, Fulder S, Khalil K, Said O. Ethnobotanical knowledge of local Arab practitioners in the Middle Eastern region. Fitoterapia. 2003;74:98–108. doi: 10.1016/S0367-326X(02)00285-X. [DOI] [PubMed] [Google Scholar]
- 44.Walter H, Harnickell E, Mueller-Dombois D. Climate-diagram maps of the individual continents and the ecological climatic regions of the earth. Berlin: Springer-Verlag; 1975. [Google Scholar]
- 45.Al-Eisawi DM, Al-Ruzayza S. The flora of holy Mecca district, Saudi Arabia. J of Biodivers Conserv. 2015;7:173–189. doi: 10.5897/IJBC2014.0773. [DOI] [Google Scholar]
- 46.International Society of Ethnobiology. ISE Code of Ethics (with 2008 additions). 2006. http://www.ethnobiology.net/code-of-ethics [Accessed 10 Jan 2015].
- 47.World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 48.Newing H, Eagle CM, Puri RK, Watson CW. Conducting research in conservation: a social science perspective. London & NY: Routledge; 2011. [Google Scholar]
- 49.Bernard HR. Research methods in anthropology—qualitative and quantitative approaches. 5. New York: Altamira Press; 2011. [Google Scholar]
- 50.Staub PO, Geck MS, Weckerle CS, Casu L, Leonti M. Classifying diseases and remedies in ethnomedicine and ethnopharmacology. J Ethnopharmacol. 2015;174:514–519. doi: 10.1016/j.jep.2015.08.051. [DOI] [PubMed] [Google Scholar]
- 51.Borgatti SP. ANTHROPAC 4.0. Analytic Technologies: Natick; 1996. [Google Scholar]
- 52.Smith JJ. Using ANTHROPAC 3.5 and a spreadsheet to compute a free-listing salience index. Cult Anthrop Methods. 1993;5:1–2. [Google Scholar]
- 53.Migahid AM. Flora of Saudi Arabia. Riyadh: Riyadh University; 1978. [Google Scholar]
- 54.The Plant List. The Plant List, a working list of all known plant species. Version 1.1. 2013. http://www.theplantlist.org/ [Accessed 21 Nov 2016].
- 55.Thomas J. Flora of Saudi Arabia—checklist. 2017. Herbarium (KSU), Department of Botany & Microbiology, King Saud University, Riyadh, Saudi Arabia. http://www.plantdiversityofsaudiarabia.info/Biodiversity-Saudi-Arabia/Flora/Checklist/Cheklist.htm [Accessed 25 September 2017].
- 56.Weckerle CS, de Boer HJ, Puri RK, van Andel T, Bussmann RW, Leonti M. Recommended standards for conducting and reporting ethnopharmacological field studies. J Ethnopharmacol. 2018;210:125–132. doi: 10.1016/j.jep.2017.08.018. [DOI] [PubMed] [Google Scholar]
- 57.World Health Organisation. Saudi Arabia: WHO statistical profile. WHO. 2015. http://www.who.int/gho/countries/sau.pdf Accessed 10 Sept 2017.
- 58.El-Ghazali GE, Al-Khalifa KS, Saleem GA, Abdallah EM. Traditional medicinal plants indigenous to Al-Rass province, Saudi Arabia. J Med Plants Res. 2010;4:2680–2683. doi: 10.5897/JMPR09.556. [DOI] [Google Scholar]
- 59.Abdulafatih HA. Medicinal plants in southwestern Saudi Arabia. Econ Bot. 1987;41:354–360. doi: 10.1007/BF02859051. [DOI] [Google Scholar]
- 60.Touwaide A, Appetiti E. Food and medicines in the Mediterranean tradition. A systematic analysis of the earliest extant body of textual evidence. J Ethnopharmacol. 2015;167:11–29. doi: 10.1016/j.jep.2014.10.035. [DOI] [PubMed] [Google Scholar]
- 61.Freedman P. Health, wellness and the allure of spices in the middle ages. J Ethnopharmacol. 2015;167:47–53. doi: 10.1016/j.jep.2014.10.065. [DOI] [PubMed] [Google Scholar]
- 62.Teixidor-Toneu I. The evolution of medicinal floras: insights from Moroccan medicinal plant knowledge transmission. PhD dissertation. Reading: University of Reading; 2017. [Google Scholar]
- 63.Al-Yahya MA. Saudi plants: a phytochemical and biological approach. Riyadh: King Abdulaziz City for Science and Technology; 1990. [Google Scholar]
- 64.Arenas PM. Etnobotánica en áreas urbanas. Bol Latinoam Caribe Plant Med Aromat. 2006;5:95. [Google Scholar]
- 65.Leonti M. The future is written: impact of scripts on the cognition, selection, knowledge and transmission of medicinal plant use and its implications for ethnobotany and ethnopharmacology. J Ethnopharmacol. 2011;134:542–555. doi: 10.1016/j.jep.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 66.Hurrell JA, Pochettino ML. Urban ethnobotany: theoretical and methodological contributions. Methods and Techniques Ethnobiol Ethnoecol. 2014:293–309.
- 67.Emery M, Hurley P. Ethnobiology in the city: embracing the urban ecological moment. J Ethnobiol. 2016;36:807–819. doi: 10.2993/0278-0771-36.4.807. [DOI] [Google Scholar]
- 68.Shalaby AF, Khodair AA, Organgi RA. Some Medicinal and aromatic plants of Saudi Arabia. Makkah: Umm Al-Qura University; 1985.
- 69.Rahman MA, Mossa JS, Al-Said MS, Al-Yahya MA. Medicinal plant diversity in the flora of Saudi Arabia 1: a report on seven plant families. Fitoterapia. 2004;75(2):149–161. [DOI] [PubMed]
- 70.Youssef SA. Medicinal and non-medicinal uses of some plants found in the middle region of Saudi Arabia. Journal of Medicinal Plants Research. 2013;7(34):2501–2517.
- 71.Shahat AA, Ibrahim AY, Alsaid MS. Antioxidant capacity and polyphenolic content of seven Saudi Arabian medicinal herbs traditionally used in Saudi Arabia. Indian Journal of Traditional Knowledge. 2015;14(1):28–35.
- 72.Yusuf M, Al-Oqail MM, Al-Sheddr ES, Al-Rehaily AJ, Rahman MA. Diversity of medicinal plants in the flora of Saudi Arabia 3: An inventory of 15 plant families and their conservation management. International Journal of Environment. 2014;3(3):312–320.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Herbarium specimens are available in the herbarium of the Umm Al-Qura University (Mecca, Saudi Arabia). All datasets on which the conclusions of the paper are based are made available as Tables 1, 2, 3 and 5 in this manuscript.


