Abstract
Objective
Racial/ethnic differences in palliative care resource use after stroke have been recognized, but it is unclear whether patient or hospital characteristics drive this disparity. We sought to determine whether palliative care use after intracerebral hemorrhage (ICH) and ischemic stroke differs between hospitals serving varying proportions of minority patients.
Design
Population-based cross-sectional study.
Setting
Inpatient hospital admissions from the Nationwide Inpatient Sample between 2007 and 2011.
Patients
A total of 46,735 intracerebral hemorrhage and 331,521 ischemic stroke cases.
Interventions
Palliative care use.
Measurements and Main Results
Intracerebral hemorrhage and ischemic stroke admissions were identified from the Nationwide Inpatient Sample between 2007 and 2011. Hospitals were categorized based on the percentage of ethnic minority stroke patients (<25% minorities [“white hospitals”], 25–50% minorities [“mixed hospitals”], or >50% minorities [“minority hospitals”]). Logistic regression was used to evaluate the association between race/ethnicity and palliative care use within and between the different hospital strata. Stroke patients receiving care in minority hospitals had lower odds of palliative care compared to those treated in white hospitals, regardless of individual patient race/ethnicity (adjusted odds ratio [OR] 0.65, 95% CI 0.50–0.84 for ICH, and OR 0.62, 95% CI 0.50–0.77 for ischemic stroke). Ethnic minorities had a lower likelihood of receiving palliative care compared to whites in any hospital stratum, but the odds of palliative care for both white and minority ICH patients was lower in minority compared to white hospitals (OR 0.66, 95% CI 0.50–0.87 for white, and OR 0.64, 95% CI 0.46–0.88 for minority patients). Similar results were observed in ischemic stroke.
Conclusions
The odds of receiving palliative care for both white and minority stroke patients is lower in minority compared to white hospitals, suggesting system-level factors as a major contributor to explain race disparities in palliative care use after stroke.
Keywords: healthcare disparities, palliative care, terminal care, minority health, stroke, cerebral hemorrhage
Introduction
Intracerebral hemorrhage (ICH) and ischemic stroke are leading causes of mortality, with case-fatality rates as high as 50%(1–3). Withdrawal of life-sustaining treatment is common after both ICH and ischemic stroke(4, 5), and access to palliative and end-of-life care has been recognized as an important component of high-quality stroke care(6, 7).
Ethnic minority stroke patients have lower utilization rates of palliative care services compared to their white counterparts(5, 8–10). Previous studies on race/ethnic disparities in the use of palliative care services have largely focused on individual-level racial and ethnic differences in knowledge(11, 12), cultural and spiritual beliefs(13, 14), communication barriers(15), and treatment preferences(16–18); however, system-level contributions to racial/ethnic differences in palliative care utilization after stroke have been insufficiently explored(6).
Some hospitals, especially those located in urban neighborhoods, serve a substantially higher proportion of minority patients, and may differ from hospitals serving predominantly white populations in their organizational structure, availability of equipment and specialists, and funding(19, 20). Between-hospital variation in the use of end-of-life care after stroke results in substantial variability of early “Do Not Resucitate” (DNR) orders ranging from 0% in some, and up to 70% in other, hospitals(21–23). It is presently unclear whether the racial makeup of the patient population in a given hospital, an example of a system-level hospital characteristic, contributes to racial/ethnic differences in palliative care use after stroke.
In order to disentangle the contributions of individual patient race versus hospital racial composition as determinants of race disparities in palliative care use after stroke, we sought to ascertain whether palliative care use differs between hospitals serving varying proportions of minority patients. Similarly, we aimed to explore whether patient-level use of palliative care differs between and within hospitals serving varying proportions of minority patients.
Methods
Data source
Data were obtained from the Nationwide Inpatient Sample (NIS), part of the Healthcare Cost and Utilization Project (HCUP), sponsored by the Agency for Healthcare Research and Quality(24). The NIS is the largest all-payer inpatient database in the US, representing a 20% stratified sample of all admissions to non-federal US hospitals. All diagnoses and procedures are recorded using International Classification of Diseases version 9 Clinical Modification (ICD9-CM) codes. Because NIS data contain no personal identifying information, this study was exempt from institutional review board approval.
Case selection
We identified adult cases with a primary diagnosis of non-traumatic ICH by using ICD9-CM code 431 between 2007 and 2011. We excluded cases with a secondary ICD9-CM code for arteriovenous malformation, traumatic brain injury, malignant brain tumor, and those undergoing aneurysm clipping and coiling to restrict our population to those with primary ICH. Only admissions to hospitals with at least 10 annual ICH cases were included (Supplemental Figure 1). Adult ischemic stroke cases were identified by using ICD9-CM codes 433.01, 433.11, 433.21, 433.31, 433.81, 433.91, 434.01, 434.11, 434.91, and 436(25, 26). Admissions to hospitals with fewer than 50 annual ischemic stroke cases were excluded (Supplemental Figure 2).
The unit of observation in NIS is discharge after hospitalization. In order to prevent double counting of transferred patients who may have multiple acute care inpatient records pertaining to the same stroke event, cases transferred to another hospital were excluded; cases transferred in from another hospital were included. We also excluded patients enrolled in a clinical trial (ICD9-CM code V70.7). This algorithm has been shown to identify acute ischemic stroke with high sensitivity and specificity(27–29). Cases with missing information on race/ethnicity, sex, and age were excluded for the primary analysis; however, sensitivity analysis after multiple imputation of missing values of the race variable was performed.
Primary exposures, hospital strata, and outcome of interest
The primary exposures of interest were self-identified ethnic minority race and hospitals serving varying proportions of minority patients with ICH and ischemic stroke. Among stroke admissions, we compared differences in palliative care use among, and by patient race within, hospitals serving predominantly white or predominantly ethnic minority patients. In order to determine patient racial composition as a system-level hospital characteristic of palliative care use after stroke, hospitals were stratified into 3 groups based on the proportion of minority patients: hospitals serving predominantly white stroke patients (<25% minority patients; “white hospitals”); hospitals serving both minority and white stroke patients (25–50% minority patients; “mixed hospitals”); and hospitals serving predominantly minority stroke patients (>50% minority patients; “minority hospitals”), as has been described previously(30, 31).
The outcome of interest was use of palliative care resources as identified by ICD9-CM code V66.7. This code identifies documented use of palliative care measures (32), irrespective of the delivery mode (i.e. via a palliative care consultation service or integrated into routine clinical practice by the care team). The Coding Clinic first addressed the code V66.7 in 1996, and in 1998, the Coding Clinic(32) provided additional clarification regarding the use of code V66.7 (Vol. 15, No. 1, p. 11): “Terms such as comfort care, end-of-life care, and hospice care are all synonymous with palliative care and these, or similar terms, need to be written in the record to support the use of code V66.7. The physician should be queried if the treatment record seems to indicate that palliative care is being given but the documentation is unclear. The care provided must be aimed only at relieving pain and discomfort for the palliative care code to be applicable”(32). Further clarification regarding the incorporation of palliative care codes by several national healthcare databases has been described by Cassel et al.(33). ICD9-CM code V66.7 has previously been shown to accurately identify palliative care services in stroke patients with 81% sensitivity and 97% specificity(5).
Comorbidity and severity adjustment
We calculated the Charlson Comorbidity Index, a weighted score of 17 different comorbidities validated for outcome adjustment for analyses of administrative data sets using ICD9-CM codes(34, 35), for each patient. Case severity was determined using the All Patient Refined-Diagnosis Related Groups (APR-DRGs), a 4-point ordinal scale (minor, moderate, major, and extreme risk of mortality) derived from age, primary and secondary diagnoses, and procedures. The APR-DRG algorithm is a validated and reliable indicator of mortality, and is commonly used as a severity indicator in studies relating to stroke(35, 36).
Statistical analysis
Clinical and hospital-level characteristics in the different hospital strata were compared using Pearson chi-square test for categorical variables and Kruskal-Wallis tests for continuous variables. Multivariable logistic regression was performed to determine the association of palliative care use with hospital strata and race differences within strata of minority versus white hospitals. Models were adjusted for age, hospital characteristics (teaching status, bed size, location, region, and annual volume of stroke cases), discharge quarter, weekend admission, modified Charlson Comorbidity Index, APR-DRG severity subclass, insurance status, median household income per patient’s ZIP code, hypertension, diabetes mellitus, dyslipidemia, coronary artery disease, peripheral vascular disease, congestive heart failure, atrial fibrillation, valvular disease, anemia, thrombocytopenia, coagulopathy, alcohol abuse, drug abuse, and chronic kidney disease. Our models also included hospital-acquired complications, such as sepsis, gastrointestinal bleeding, pneumonia, urinary tract infection, deep vein thrombosis, dysphagia, and pulmonary embolism. In addition, we adjusted for mechanical ventilation, gastrostomy, tracheostomy, craniotomy/craniectomy, and cerebral angiography as measures of intensity of care. Models for ICH were additionally adjusted for placement of an external ventricular drain, and models for ischemic stroke were adjusted for IV thrombolysis. We used a Generalized Estimation Equations (GEE) approach to account for clustering of patients within hospitals. In order to reduce potential bias as a result of missing data for race, we performed sensitivity analyses after multiple imputation by chained equations (MICE) in order to impute missing values of the race variable. Statistical analysis was performed using STATA version 13 (Stata Statistical Software: Release 13. College Station, TX). A p-value of <0.05 was considered statistically significant, and 95% confidence intervals are reported.
Results
Patient characteristics
A total of 46,735 ICH cases and 331,521 ischemic stroke cases met inclusion criteria (Supplemental Figures 1 and 2). Among cases presenting with ICH, 17,914 (38.3%) were treated at 374 white hospitals, 15,769 (33.7%) were treated at 259 mixed hospitals, and 13,052 (27.9%) received care at 214 hospitals serving predominantly minority stroke patients. Among ischemic stroke cases, 170,015 (51.3%) were admitted to 727 white hospitals, 95,642 (28.9%) were treated at 363 mixed hospitals, and 65,864 (19.9%) received care at 264 minority hospitals. Patient and hospital characteristics of ICH and ischemic stroke cases treated in hospitals with varying proportion of minority patients are summarized in Table 1.
Table 1.
Baseline characteristics of the study population stratified by stroke subtype and hospital type (white, mixed, and minority). Numbers given are n (%) unless stated otherwise. APR-DRG: all patient refined diagnosis-related group; PI: Pacific Islander.
| Characteristic | Intracerebral Hemorrhage (n=46,735) | Ischemic Stroke (n=331,521) | ||||
|---|---|---|---|---|---|---|
| Patients in white hospitals (n=17,914) | Patients in mixed hospitals (n=15,769) | Patients in minority hospitals (n=13,052) | Patients in white hospitals (n=170,015) | Patients in mixed hospitals (n=95,642) | Patients in minority hospitals (n=65,864) | |
|
| ||||||
| Age – years: median (IQR) | 75 (62–83) | 71 (57–81) | 66 (54–78) | 75 (63–84) | 72 (60–82) | 69 (57–80) |
|
| ||||||
| Female | 9,158 (51.1) | 7,751 (49.2) | 6,114 (46.8) | 90,201 (53.1) | 50,298 (52.6) | 34,222 (52.0) |
|
| ||||||
| Race/Ethnicity | ||||||
|
| ||||||
| White | 15,601 (87.1) | 9,955 (63.1) | 4,124 (31.6) | 149,180 (87.8) | 60,917 (63.7) | 19,918 (30.2) |
|
| ||||||
| Black | 1,241 (6.9) | 2,953 (18.7) | 4,180 (32.0) | 12,280 (7.2) | 20,981 (21.9) | 24,245 (36.8) |
|
| ||||||
| Hispanic | 418 (2.3) | 1,436 (9.1) | 2,675 (20.5) | 4,081 (2.4) | 7,504 (7.9) | 13,004 (19.7) |
|
| ||||||
| Asian/PI | 312 (1.7) | 787 (5.0) | 1,199 (9.2) | 1,817 (1.1) | 3,175 (3.3) | 4,098 (6.2) |
|
| ||||||
| Other | 342 (1.9) | 638 (4.1) | 874 (6.7) | 2,657 (1.6) | 3,065 (3.2) | 4,599 (7.0) |
|
| ||||||
| All minorities | 2,313 (12.9) | 5,814 (36.9) | 8,928 (68.4) | 20,835 (12.3) | 34,725 (36.3) | 45,946 (69.8) |
|
| ||||||
| Health Insurance | ||||||
|
| ||||||
| Private | 3,487 (19.5) | 3,424 (21.7) | 2,753 (21.1) | 33,127 (19.5) | 20,706 (21.7) | 13,031 (19.8) |
|
| ||||||
| Medicaid | 1,081 (6.0) | 1,347 (8.5) | 2,024 (15.5) | 7,663 (4.5) | 6,819 (7.1) | 8,230 (12.5) |
|
| ||||||
| Medicare | 11,977 (66.9) | 9,365 (59.4) | 6,372 (48.8) | 118,810 (69.9) | 59,443 (62.2) | 37,134 (56.4) |
|
| ||||||
| Self-pay | 867 (4.8) | 1,088 (6.9) | 1,324 (10.1) | 6,326 (3.7) | 5,386 (5.6) | 4,836 (7.3) |
|
| ||||||
| Median household income per zip code | ||||||
|
| ||||||
| Quartile 1 | 4,275 (23.9) | 4,324 (27.4) | 4,608 (35.3) | 39,825 (23.4) | 26,444 (27.7) | 25,721 (39.1) |
|
| ||||||
| Quartile 2 | 4,847 (27.1) | 3,628 (23.0) | 2,665 (20.4) | 45,388 (26.7) | 22,586 (23.6) | 12,873 (19.5) |
|
| ||||||
| Quartile 3 | 4,415 (24.7) | 3,333 (21.1) | 2,905 (22.3) | 41,741 (24.6) | 21,752 (22.7) | 14,424 (21.9) |
|
| ||||||
| Quartile 4 | 4,051 (22.6) | 4,124 (26.2) | 2,424 (18.6) | 39,975 (23.5) | 22,768 (23.8) | 11,091 (16.8) |
|
| ||||||
| Teaching Hospital | 9,591 (53.5) | 10,228 (64.9) | 9,785 (75.0) | 67,020 (39.4) | 49,715 (52.0) | 41,032 (62.3) |
|
| ||||||
| Hospital Region | ||||||
|
| ||||||
| Northeast | 5,029 (28.1) | 2,038 (12.9) | 2,332 (17.9) | 42,824 (25.2) | 11,339 (11.9) | 15,195 (23.1) |
|
| ||||||
| Midwest | 4,134 (23.1) | 1,340 (8.5) | 1,058 (8.1) | 35,776 (21.0) | 8,939 (9.4) | 6,647 (10.1) |
|
| ||||||
| South | 6,086 (34.0) | 7,652 (48.5) | 6,015 (46.1) | 61,876 (36.4) | 52,015 (54.4) | 29,712 (45.1) |
|
| ||||||
| West | 2,665 (14.9) | 4,739 (30.1) | 3,647 (27.9) | 29,539 (17.4) | 23,349 (24.4) | 14,310 (21.7) |
|
| ||||||
| Hospital Location | ||||||
|
| ||||||
| Rural | 806 (4.5) | 273 (1.7) | 43 (0.3) | 17,942 (10.6) | 4,149 (4.3) | 3,209 (4.9) |
|
| ||||||
| Urban | 16,759 (93.6) | 15,435 (97.9) | 12,622 (96.7) | 150,587 (88.6) | 90,877 (95.0) | 61,453 (93.3) |
|
| ||||||
| Hospital Bed Size | ||||||
|
| ||||||
| Small | 649 (3.6) | 703 (4.5) | 727 (5.6) | 15,192 (8.9) | 6,713 (7.0) | 4,52 (6.2) |
|
| ||||||
| Medium | 3,446 (19.2) | 3,412 (21.6) | 2,141 (16.4) | 40,748 (24.0) | 21,991 (23.0) | 15,755 (23.9) |
|
| ||||||
| Large | 13,470 (75.2) | 11,593 (73.5) | 9,797 (75.1) | 112,589 (66.2) | 66,322 (69.3) | 44,855 (68.1) |
|
| ||||||
| Hospital stroke case volume/year | ||||||
|
| ||||||
| Quartile 1 | 5,521 (30.8) | 3,664 (23.2) | 2,889 (22.1) | 47,067 (27.7) | 20,344 (21.3) | 15,722 (23.9) |
|
| ||||||
| Quartile 2 | 5,364 (29.9) | 3,380 (21.4) | 2,840 (21.8) | 42,246 (24.9) | 22,355 (23.4) | 18,471 (28.0) |
|
| ||||||
| Quartile 3 | 3,596 (20.1) | 4,527 (28.7) | 3,929 (26.0) | 42,739 (25.1) | 25,179 (16.3) | 14,801 (22.5) |
|
| ||||||
| Quartile 4 | 3,433 (19.2) | 4,198 (26.6) | 3,929 (30.1) | 37,963 (22.3) | 27,764 (29.0) | 16,870 (25.6) |
|
| ||||||
| Charlson Comorbidity Index | ||||||
|
| ||||||
| 1 | 6,296 (35.2) | 5,527 (35.1) | 4,283 (32.8) | 48,415 (28.5) | 26,224 (27.4) | 16,808 (25.5) |
|
| ||||||
| 2 | 3,508 (19.6) | 3,030 (19.2) | 2,506 (19.2) | 38,069 (22.4) | 21,745 (22.7) | 15,166 (23.0) |
|
| ||||||
| 3 | 4,076 (22.8) | 3,548 (22.5) | 3,093 (23.7) | 36,163 (21.3) | 20,381 (21.3) | 13,613 (20.7) |
|
| ||||||
| ≥4 | 4,034 (22.5) | 3,664 (23.2) | 3,170 (24.3) | 47,368 (27.9) | 27,292 (28.5) | 20,277 (30.8) |
|
| ||||||
| APR-DRG | ||||||
|
| ||||||
| Minor | 1,278 (7.1) | 1,092 (6.9) | 1,006 (7.7) | 15,545 (9.1) | 8,936 (9.3) | 6,369 (9.7) |
|
| ||||||
| Moderate | 5,718 (31.9) | 4,606 (29.2) | 3,635 (27.9) | 81,898 (48.2) | 45,007 (47.1) | 31,407 (47.7) |
|
| ||||||
| Major | 7,056 (39.4) | 5,952 (37.7) | 4,574 (35.0) | 58,283 (34.3) | 32,170 (33.6) | 21,016 (31.9) |
|
| ||||||
| Extreme | 3,862 (21.6) | 4,119 (26.1) | 3,837 (29.4) | 14,289 (8.4) | 9,529 (10.0) | 7,072 (10.7) |
|
| ||||||
| Length of stay – days: median (IQR) | 5 (2–8) | 5 (3–10) | 6 (3–12) | 4 (2–6) | 4 (2–6) | 4 (3–7) |
Among all ICH patients, 10.6% received palliative care, while 3.2% of patients with ischemic stroke received palliative care services. Inpatient mortality rates were 71.5% and 48.7% for ICH and ischemic stroke, respectively, among palliative care users; and 21.1% and 3.7% for ICH and ischemic stroke, respectively, among patients who did not receive palliative care. The discharge disposition in the palliative care vs. non-palliative care users is presented in Supplemental Table 1. ICH and ischemic stroke patients who received palliative care and who were discharged alive were older than those who died in the hospital, were less likely to be treated at teaching and high case volume hospitals, and had lower APR-DRG risk of mortality compared to palliative care users with in-hospital deaths (Supplemental Table 2).
Palliative care use is lower in hospitals with a high proportion of minority patients
Among hospitals included for ICH analysis, the median rate of palliative care use in white hospitals was 8.5 (IQR 1.3–17.4) per 100 ICH admissions, while in mixed and minority hospitals the median palliative care use rates were 6.3 (IQR 0–14.1) and 2.5 (IQR 0–11.0) per 100 ICH admissions, respectively (p<0.001). Among hospitals included for analysis of ischemic stroke, the median palliative care use rate in white hospitals was 2.2 (IQR 0.3–5.1) per 100 ischemic stroke admissions, while the median rates of palliative care use in mixed and minority hospitals were 1.5 (IQR 0–4.4) and 0.5 (IQR 0–2.4) per 100 admissions, respectively (p<0.001).
Patient-level palliative care use rates among ICH and ischemic stroke cases were lower in mixed and minority hospitals, compared to white hospitals (Table 2). In adjusted models, the odds of palliative care use among ICH cases were lower in mixed (OR 0.87, 95% CI 0.70–1.07; Table 2) and minority hospitals (OR 0.65, 95% CI 0.50–0.84), compared to white hospitals (p for trend 0.001). Similarly, among ischemic stroke admissions, the adjusted odds of palliative care were lower in mixed (OR 0.93, 95% CI 0.79–1.10; Table 2) and minority hospitals (OR 0.62, 95% CI 0.50–0.77), compared to white hospitals (p for trend <0.001). Individual patient race was adjusted for in the analyses, suggesting that a stroke patient at a minority hospital has lower odds of receiving palliative care than a patient at a white hospital, regardless of individual patient race/ethnicity. To confirm these findings and to reduce the potential bias from discharge data with missing information on race, we repeated the analysis after multiple imputation of the missing values for race; the results were materially unchanged (Supplemental Table 3).
Table 2.
Rates and odds of palliative care utilization among patients presenting to hospitals serving varying proportions of minority stroke patients.
| Variable | N | Palliative Care N (%) |
Unadjusted OR (95% CI) |
Adjusted* OR (95% CI) |
p for trend |
|---|---|---|---|---|---|
| ICH | |||||
| All Patients | 46,735 | 4,931 (10.6) | |||
| Hospital Strata | 0.001 | ||||
| White | 17,914 | 2,275 (12.7) | 1.00 (ref) | 1.00 (ref) | |
| Mixed | 15,769 | 1,706 (10.8) | 0.83 (0.68–1.02) | 0.87 (0.70–1.07) | |
| Minority | 13,052 | 950 (7.3) | 0.54 (0.43–0.68) | 0.65 (0.50–0.84) | |
| Ischemic Stroke | |||||
| All Patients | 321,521 | 10,641 (3.2) | |||
| Hospital Strata | <0.001 | ||||
| White | 192,960 | 6,215 (3.7) | 1.00 (ref) | 1.00 (ref) | |
| Mixed | 100,627 | 3,161 (3.3) | 0.90 (0.77–1.06) | 0.93 (0.79–1.10) | |
| Minority | 70,128 | 1,265 (1.9) | 0.52 (0.42–0.63) | 0.62 (0.50–0.77) |
Models were adjusted for age, sex, race/ethnicity, hospital characteristics (teaching status, bed size, location, region, and annual volume of stroke cases), discharge quarter, weekend admission, modified Charlson Comorbidity Index, APR-DRG severity subclass, insurance status, median household income per patient’s ZIP code, hypertension, diabetes mellitus, dyslipidemia, coronary artery disease, peripheral vascular disease, congestive heart failure, atrial fibrillation, valvular disease, anemia, thrombocytopenia, coagulopathy, cancer, alcohol abuse, drug abuse, chronic kidney disease, pneumonia, urinary tract infection, sepsis, gastrointestinal bleeding, deep vein thrombosis, pulmonary embolism, dysphagia, craniotomy/craniectomy, cerebral angiography, gastrostomy, mechanical ventilation, and tracheostomy. Models for ICH were additionally adjusted for placement of an external ventricular drain, and models for ischemic stroke were adjusted for IV thrombolysis.
Individual and system contributions to racial/ethnic differences in palliative care use
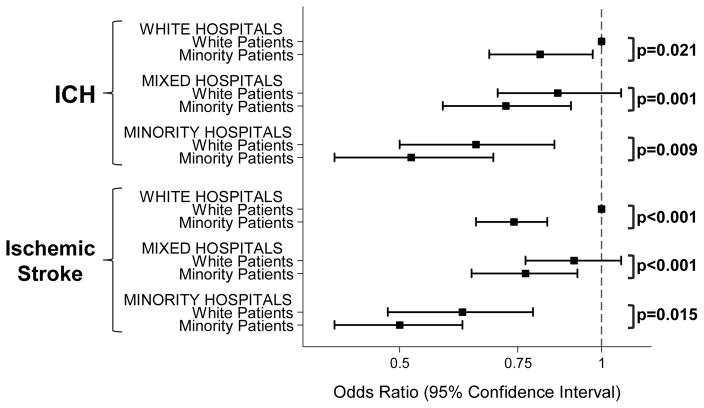
We investigated the odds of palliative care among minorities vs. whites within and between the three hospital strata (Figure 1 and Table 3). Compared to white ICH and ischemic stroke patients, ethnic minorities had significantly lower odds of palliative care use in any hospital strata (Figure 1). White and minority patients both had lower odds of receiving palliative care in mixed and minority compared to white hospitals (Table 3): white ICH patients had 34% lower odds of palliative care when receiving care in minority compared to white hospitals (OR 0.66, 95% CI 0.50–0.86); minority ICH patients treated in minority hospitals had significantly lower odds of palliative care use when compared to minority patients care for in white hospitals (OR 0.64, 95% CI 0.46–0.88; Table 3 and Figure 1). Similarly, among patients with ischemic stroke, the odds of receiving palliative care were lower in minority compared to white hospitals for either patient group (OR 0.63, 95% CI 0.49–0.80 comparing minority vs. white hospitals among whites, and OR 0.66, 95% CI 0.51–0.85 comparing minority vs. white hospitals among minorities; Table 3 and Figure 1). Sensitivity analysis after multiple imputation of missing values for race showed similar results (Supplemental Figure 3).
Figure 1.
Graphic representation of odds ratios of use of palliative care for minority versus white patients, stratified by hospitals and stroke subtype (upper panel: intracerebral hemorrhage (ICH); lower panel: ischemic stroke). White patients in white hospitals serve as the reference. P-values compare the odds of palliative care use for minority compared to white patients within each hospital strata.
Table 3.
Adjusted odds ratios of palliative care in white, mixed, and minority hospitals stratified by patient race/ethnicity. ICH: intracerebral hemorrhage.
| Variable | Adjusted OR (95% CI) of Palliative Care | p-value | p for trend |
|---|---|---|---|
| ICH | |||
| White patients | 0.004 | ||
| White hospitals | 1.00 (ref) | ||
| Mixed hospitals | 0.87 (0.70-1.08) | 0.205 | |
| Minority hospitals | 0.66 (0.50-0.86) | 0.002 | |
| Minority patients | 0.004 | ||
| White hospitals | 1.00 (ref) | ||
| Mixed hospitals | 0.87 (0.65-1.17) | 0.363 | |
| Minority hospitals | 0.64 (0.46-0.88) | 0.007 | |
| Ischemic Stroke | |||
| White patients | 0.002 | ||
| White hospitals | 1.00 (ref) | ||
| Mixed hospitals | 0.91 (0.77-1.08) | 0.286 | |
| Minority hospitals | 0.63 (0.49-0.80) | <0.001 | |
| Minority patients | <0.001 | ||
| White hospitals | 1.00 (ref) | ||
| Mixed hospitals | 1.03 (0.84-1.27) | 0.774 | |
| Minority hospitals | 0.66 (0.51-0.85) | 0.001 |
Discussion
In the present study we investigated differences in palliative care use among hospitals serving varying proportions of ethnic minority patients after ischemic stroke and ICH. We found that palliative care resources are underutilized in hospitals serving predominantly ethnic minority stroke patients. Patient-level racial/ethnic differences in the use of palliative care remained within each hospital strata; however, palliative care use for either racial/ethnic group was lower in minority compared to white hospitals.
Factors contributing to racial/ethnic disparities in the use of palliative care resources are not well understood. Prior studies have largely focused on individual-level barriers to palliative care use in ethnic minority patients, including lack of knowledge about palliative care(11, 12), presence of spiritual and religious beliefs in conflict with goals of palliative care(13, 17), mistrust in the health system(14, 37), and greater preference for life-sustaining therapies, regardless of prognosis(16, 18, 38). These individual-level determinants may in part explain the observed within-hospital racial disparities; however, they are insufficient to explain differences in palliative care use between minority and white hospitals, i.e. they do not explain why palliative care use for any patient race/ethnic group is lower in minority compared to white hospitals.
System-level differences contributing to differences in palliative care utilization after stroke have been described previously, including variation by hospital location, region, size, and teaching status(5, 8); however, these hospital characteristics were included in our model and are therefore unlikely to explain the observed between-hospital differences in our study. Similarly, our models included annual hospital stroke case volume, individual patient comorbidities, insurance status, and common medical complications including hospital-acquired infections and mechanical ventilation. Structural differences, including specialists on staff, resource availabilities, and local hospital culture, may contribute to differences in the utilization or availability of palliative care in minority compared to white hospitals(19). Given the wide range of availability of palliative care services across US hospitals(39), hospitals predominantly serving ethnic minorities may lack palliative care specialists and resources dedicated to palliative care services. This might be particularly relevant considering that hospitals serving predominantly minority patients are commonly underfunded, understaffed, and located in medically underserved areas(40, 41). ICD-9 code V66.7 captures palliative care irrespective of how it was integrated into each hospital system, whether through a palliative care consultation service or incorporated into routine clinical practice by the care team itself. Therefore, local practice patterns and hospital “culture” regarding palliative care resource use or lower availability may differ in minority compared to white hospitals. Although the exact underlying causes for between-hospital variability in existing practice patterns cannot be determined from this study, it is possible that the preference of a majority of patients in a given hospital may influence the practice approach for all patients within that hospital(42). Thus, the preference of ethnic minority patients at minority hospitals to pursue aggressive life-sustaining treatments and interventions rather than palliative care services may in turn influence the counseling practices of the treating physicians and the overall practice pattern within those hospitals.
Our study is limited by the potential for miscoded data in an administrative dataset reliant on ICD9-CM coding; however, it is unlikely that there is differential miscoding of diagnoses or procedures by race. Although ICD9-CM code V66.7 identifies palliative care services use with high sensitivity and specificity(5), there is a possibility of under-reporting or under-coding patients who actually received palliative care. Furthermore, NIS does not collect information on the trigger, timing, and mode of palliative care delivery. Although there is no a priori reason to expect a change in the distribution of use and availability of palliative care, it should be recognized that data were collected from 2007 to 2011 when palliative care services and knowledge were nascent relative to now. In addition, use of the code V66.7 as a process measure of palliative care use is limited in that it does not capture the quality or the impact of the actual care delivered. While race/ethnicity is typically self-reported, it is possible that information captured in the race variable is not entirely accurate. We attempted to mitigate the absence of clinical and physiological stroke data in NIS, such as lack of hematoma/stroke volume, NIH Stroke Scale, and Glasgow Coma Scale, by adjusting all models for the Charlson Comorbiditity Index, a validated measure of patient comorbidities in stroke(35, 43), as well as medical complications. Since NIS lacks information on individual patient or provider decision-making, we were unable to directly investigate the contribution of implicit bias, provider attitudes, and individual patient preference to the observed racial/ethnic differences in palliative care resource use. Finally, although the ICD-9 code V66.7 is broadly defined for coding purposes, it is possible that the code captured predominantly those patients with comfort measures or withdrawal of care accounting for higher mortality in the palliative care group. However, we found that nearly 45% of combined ICH and ischemic stroke patients who received palliative care were discharged alive. Similarly, just under 20% of all patients who received palliative care were discharged to a non-comfort focused destination (home/self-care, rehab facility, or home health). Patients receiving palliative care who were discharged alive had lower APR-DRG risk of mortality, and in the case of ischemic stroke patients, lower mechanical ventilation rates compared to the mortality group that received palliative care. This suggests that these patients were perceived as less likely to die early (i.e. in-hospital death) and that palliative care use was not purely applied as a DNR order.
Despite these limitations, our data suggest that racial/ethnic differences in palliative care utilization and availability after stroke are explained by both individual as well as hospital-level factors. Future studies may determine the underlying drivers of the observed differences resulting in decreased palliative care use and availability in minority hospitals. Our study highlights that mere focus on individual-level determinants of care delivery and usage, such as individual preferences, are insufficient in fully understanding racial/ethnic differences in palliative care use after stroke.
Conclusions
Ethnic minority patients had lower palliative care use after both ischemic and hemorrhagic stroke compared to whites in any hospital strata. Palliative care use was lower in minority compared to white hospitals regardless of individual patient race, i.e. white patients and minority patients alike had lower odds of palliative care use in hospitals caring for predominantly minority patients compared to hospitals that treat predominantly white patients. Thus, clustering of ethnic minority stroke patients at relatively few hospitals with low overall palliative care administration may contribute to the overall lower rates of palliative care use in minority compared to white patients. Our data suggest that race differences in the use of palliative care may in part be explained by hospital racial composition, and future attempts to mitigate racial disparities in palliative care utilization and availability may be most effective by increasing use at hospitals serving predominantly minority patients.
Supplementary Material
Acknowledgments
Source of Funding
Dr Faigle is supported by an NINDS Career Development Award (K23 NS101124). Dr. Ziai is supported by NIH Grant Number 1U01NS08082. Dr. Cooper is supported by a grant from the National Heart, Lung, and Blood Institute (K24HL083113). Dr Gottesman is supported by K24AG052573 and is an Associate Editor for Neurology.
Footnotes
No reprints will be ordered.
Conflicts of Interest
Dr Urrutia reports no conflict of interest.
Copyright form disclosure: Dr. Faigle and Dr. Cooper received support for article research from the National Institutes of Health (NIH). Dr. Faigle’s institution received funding from the NIH, NIH/National Institute of Neurological Disorders and Stroke: 1U01NS08082, and National Heart, Lung, and Blood Institute (NHLBI): K24HL083113. Dr. Ziai received funding from a NIH grant for Minimally Invasive Surgery Plus r-tPA for Intracerebral Hemorrhage Evacuation (MISTIE) III 1U01NS08082, from Headsense, Inc., and from grant number 5U01NS062851 for Clot Lysis Evaluation of Accelerated Resolution of Intraventricular Hemorrhage III. Dr. Urrutia’s institution received funding from Genentech, Inc. funds for an investigator sponsored trial. Dr. Cooper’s institution received funding from the NHLBI. Dr. Gottesman received funding from Neurology journal (Associate Editor).
References
- 1.Koton S, Schneider AL, Rosamond WD, et al. Stroke incidence and mortality trends in US communities, 1987 to 2011. JAMA. 2014;312:259–268. doi: 10.1001/jama.2014.7692. [DOI] [PubMed] [Google Scholar]
- 2.van Asch CJ, Luitse MJ, Rinkel GJ, et al. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: A systematic review and meta-analysis. Lancet Neurol. 2010;9:167–176. doi: 10.1016/S1474-4422(09)70340-0. [DOI] [PubMed] [Google Scholar]
- 3.Feigin VL, Lawes CM, Bennett DA, et al. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: A systematic review. Lancet Neurol. 2009;8:355–369. doi: 10.1016/S1474-4422(09)70025-0. [DOI] [PubMed] [Google Scholar]
- 4.Naidech AM, Bernstein RA, Bassin SL, et al. How patients die after intracerebral hemorrhage. Neurocrit Care. 2009;11:45–49. doi: 10.1007/s12028-009-9186-z. [DOI] [PubMed] [Google Scholar]
- 5.Qureshi AI, Adil MM, Suri MF. Rate of utilization and determinants of withdrawal of care in acute ischemic stroke treated with thrombolytics in USA. Med Care. 2013;51:1094–1100. doi: 10.1097/MLR.0b013e3182a95db4. [DOI] [PubMed] [Google Scholar]
- 6.Holloway RG, Arnold RM, Creutzfeldt CJ, et al. Palliative and end-of-life care in stroke: A statement for healthcare professionals from the American Heart Association/American stroke association. Stroke. 2014;45:1887–1916. doi: 10.1161/STR.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 7.Frontera JA, Curtis JR, Nelson JE, et al. Integrating palliative care into the care of neurocritically ill patients: A report from the improving palliative care in the ICU project advisory board and the center to advance palliative care. Crit Care Med. 2015;43:1964–1977. doi: 10.1097/CCM.0000000000001131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murthy SB, Moradiya Y, Hanley DF, et al. Palliative care utilization in nontraumatic intracerebral hemorrhage in the United States. Crit Care Med. 2016;44:575–582. doi: 10.1097/CCM.0000000000001391. [DOI] [PubMed] [Google Scholar]
- 9.Shepardson LB, Gordon HS, Ibrahim SA, et al. Racial variation in the use of do-not-resuscitate orders. J Gen Intern Med. 1999;14:15–20. doi: 10.1046/j.1525-1497.1999.00275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zahuranec DB, Brown DL, Lisabeth LD, et al. Ethnic differences in do-not-resuscitate orders after intracerebral hemorrhage. Crit Care Med. 2009;37:2807–2811. doi: 10.1097/CCM.0b013e3181a56755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Born W, Greiner KA, Sylvia E, et al. Knowledge, attitudes, and beliefs about end-of-life care among inner-city african americans and latinos. J Palliat Med. 2004;7:247–256. doi: 10.1089/109662104773709369. [DOI] [PubMed] [Google Scholar]
- 12.Johnson KS, Kuchibhatla M, Tulsky JA. Racial differences in self-reported exposure to information about hospice care. J Palliat Med. 2009;12:921–927. doi: 10.1089/jpm.2009.0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson KS, Elbert-Avila KI, Tulsky JA. The influence of spiritual beliefs and practices on the treatment preferences of african americans: A review of the literature. J Am Geriatr Soc. 2005;53:711–719. doi: 10.1111/j.1532-5415.2005.53224.x. [DOI] [PubMed] [Google Scholar]
- 14.Cort MA. Cultural mistrust and use of hospice care: Challenges and remedies. J Palliat Med. 2004;7:63–71. doi: 10.1089/109662104322737269. [DOI] [PubMed] [Google Scholar]
- 15.Lorenz KA, Ettner SL, Rosenfeld KE, et al. Accommodating ethnic diversity: A study of California hospice programs. Med Care. 2004;42:871–874. doi: 10.1097/01.mlr.0000135830.13777.9c. [DOI] [PubMed] [Google Scholar]
- 16.Blackhall LJ, Frank G, Murphy ST, et al. Ethnicity and attitudes towards life sustaining technology. Soc Sci Med. 1999;48:1779–1789. doi: 10.1016/s0277-9536(99)00077-5. [DOI] [PubMed] [Google Scholar]
- 17.Kwak J, Haley WE. Current research findings on end-of-life decision making among racially or ethnically diverse groups. Gerontologist. 2005;45:634–641. doi: 10.1093/geront/45.5.634. [DOI] [PubMed] [Google Scholar]
- 18.Barnato AE, Anthony DL, Skinner J, et al. Racial and ethnic differences in preferences for end-of-life treatment. J Gen Intern Med. 2009;24:695–701. doi: 10.1007/s11606-009-0952-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baicker K, Chandra A, Skinner JS. Geographic variation in health care and the problem of measuring racial disparities. Perspect Biol Med. 2005;48:S42–53. [PubMed] [Google Scholar]
- 20.Jha AK, Orav EJ, Li Z, et al. Concentration and quality of hospitals that care for elderly black patients. Arch Intern Med. 2007;167:1177–1182. doi: 10.1001/archinte.167.11.1177. [DOI] [PubMed] [Google Scholar]
- 21.Hemphill JC, 3rd, Newman J, Zhao S, et al. Hospital usage of early do-not-resuscitate orders and outcome after intracerebral hemorrhage. Stroke. 2004;35:1130–1134. doi: 10.1161/01.STR.0000125858.71051.ca. [DOI] [PubMed] [Google Scholar]
- 22.Kelly AG, Zahuranec DB, Holloway RG, et al. Variation in do-not-resuscitate orders for patients with ischemic stroke: Implications for national hospital comparisons. Stroke. 2014;45:822–827. doi: 10.1161/STROKEAHA.113.004573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shepardson LB, Youngner SJ, Speroff T, et al. Variation in the use of do-not-resuscitate orders in patients with stroke. Arch Intern Med. 1997;157:1841–1847. [PubMed] [Google Scholar]
- 24.Steiner C, Elixhauser A, Schnaier J. The healthcare cost and utilization project: An overview. Eff Clin Pract. 2002;5:143–151. [PubMed] [Google Scholar]
- 25.Goldstein LB. Accuracy of ICD-9-CM coding for the identification of patients with acute ischemic stroke: Effect of modifier codes. Stroke. 1998;29:1602–1604. doi: 10.1161/01.str.29.8.1602. [DOI] [PubMed] [Google Scholar]
- 26.Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44:2064–2089. doi: 10.1161/STR.0b013e318296aeca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kokotailo RA, Hill MD. Coding of stroke and stroke risk factors using international classification of diseases, revisions 9 and 10. Stroke. 2005;36:1776–1781. doi: 10.1161/01.STR.0000174293.17959.a1. [DOI] [PubMed] [Google Scholar]
- 28.Tirschwell DL, Longstreth WT., Jr Validating administrative data in stroke research. Stroke. 2002;33:2465–2470. doi: 10.1161/01.str.0000032240.28636.bd. [DOI] [PubMed] [Google Scholar]
- 29.Jones SA, Gottesman RF, Shahar E, et al. Validity of hospital discharge diagnosis codes for stroke: The atherosclerosis risk in communities study. Stroke. 2014;45:3219–3225. doi: 10.1161/STROKEAHA.114.006316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haider AH, Ong’uti S, Efron DT, et al. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: A nationwide analysis of 434 hospitals. Arch Surg. 2012;147:63–70. doi: 10.1001/archsurg.2011.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Faigle R, Urrutia VC, Cooper LA, et al. Individual and system contributions to race and sex disparities in thrombolysis use for stroke patients in the United States. Stroke. 2017;48:990–997. doi: 10.1161/STROKEAHA.116.015056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brown F, Leon-Chisen N. ICD-9-CM coding handbook, with answers, 2012 revised edition. AHA Press; [Google Scholar]
- 33.Cassel JB, Jones AB, Meier DE, et al. Hospital mortality rates: How is palliative care taken into account? J Pain Symptom Manage. 2010;40:914–925. doi: 10.1016/j.jpainsymman.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 34.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 35.Bar B, Hemphill JC., 3rd Charlson comorbidity index adjustment in intracerebral hemorrhage. Stroke. 2011;42:2944–2946. doi: 10.1161/STROKEAHA.111.617639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xian Y, Holloway RG, Pan W, et al. Challenges in assessing hospital-level stroke mortality as a quality measure: Comparison of ischemic, intracerebral hemorrhage, and total stroke mortality rates. Stroke. 2012;43:1687–1690. doi: 10.1161/STROKEAHA.111.648600. [DOI] [PubMed] [Google Scholar]
- 37.Wicher CP, Meeker MA. What influences african american end-of-life preferences? J Health Care Poor Underserved. 2012;23:28–58. doi: 10.1353/hpu.2012.0027. [DOI] [PubMed] [Google Scholar]
- 38.Cagle JG, LaMantia MA, Williams SW, et al. Predictors of preference for hospice care among diverse older adults. Am J Hosp Palliat Care. 2016;33:574–584. doi: 10.1177/1049909115593936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Center to Advance Palliative Care. [accessed February 24, 2017];A state-by-state report card on access to palliative care in our nation’s hospitals. https://reportcard.capc.org/findings/Edition.
- 40.Gaskin DJ, Hadley J. Population characteristics of markets of safety-net and non-safety-net hospitals. J Urban Health. 1999;76:351–370. doi: 10.1007/BF02345673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shen YC, Hsia RY, Kuzma K. Understanding the risk factors of trauma center closures: Do financial pressure and community characteristics matter? Med Care. 2009;47:968–978. doi: 10.1097/MLR.0b013e31819c9415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barnato AE, Herndon MB, Anthony DL, et al. Are regional variations in end-of-life care intensity explained by patient preferences?: A study of the US medicare population. Med Care. 2007;45:386–393. doi: 10.1097/01.mlr.0000255248.79308.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goldstein LB, Samsa GP, Matchar DB, et al. Charlson index comorbidity adjustment for ischemic stroke outcome studies. Stroke. 2004;35:1941–1945. doi: 10.1161/01.STR.0000135225.80898.1c. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.