Abstract
Purpose
Over one million patients seek care in an Emergency Department (ED) for kidney stones annually, but a minority require admission or urologic procedure. We aim to describe predictors of hospital admission or urologic intervention.
Materials and Methods
This secondary analysis of prospective data includes ED patients with CT-confirmed obstructing ureteral stone. All patients also received a point-of-care limited renal ultrasound (PLUS). Need for urologic intervention at 90 days was assessed by follow-up interview. Logistic regression was used to identify predictors of admission and urologic intervention, which were further stratified by disposition. Separate regression models with and without CT findings (PLUS only) were compared using the c-statistic.
Results
Among a cohort of 475 patients with symptomatic stone on CT, 95 (20%) were admitted and 68 had an intervention (72%). Of 380 discharged patients, 66 (17%) required urologic intervention. Admitted patients were more likely to have had a prior procedure, evidence of kidney injury or infection, need opiate analgesia, have larger stones or hydronephrosis on PLUS. Predictors of intervention varied by disposition, though regression models with and without CT findings demonstrated similar c-statistics. Discharged patients with larger stones, a longer duration of pain at presentation, and prior procedures were more likely to undergo intervention.
Conclusions
Intervention was common among admitted patients but occurred in a minority of those discharged. Predictors of intervention varied by disposition and models incorporating CT findings were similar to those without. These data support ultrasound-first or delayed-CT diagnostic pathways for patients deemed clinically suitable for discharge.
Keywords: Kidney Calculi, Diagnostic Imaging, Ultrasound
Introduction
Urolithiasis is a common disease, afflicting approximately 1 in 11 persons in the United States.1 The prevalence of this disease, as well as visits to the emergency department for pain associated with urolithiasis, is increasing.2 Urologic intervention is mandatory for an obstructing stone with infection.3,4 In the uninfected patient, the majority of renal calculi pass spontaneously, and current consensus guidelines recommend conservative initial management for patients with stones <10mm and adequate pain control.5,6
Despite guidelines, significant variation in admission and intervention patterns exist.7,8 Predictors of hospital admission and/or subsequent need for urologic intervention in patients presenting with acute renal colic are not well defined. Prior studies on this topic have proposed numerous clinical, laboratory or radiologic variables as predictors, but have been limited by their small sample sizes, retrospective design or failed validation.9–14 As a recent randomized controlled trial demonstrated the non-inferiority of an ultrasound-first pathway for the diagnosis of renal colic in the ED,15 the ability to predict the need for a future intervention could help clinicians determine which patients are more likely to benefit from an immediate CT scan. Additionally, the American College of Emergency Physicians’ “Choosing Wisely” campaign recommends avoiding CT scan in young patients with a history of renal colic, as these patients are at high risk for significant lifetime radiation exposure.16 Taken together, a better understanding of which patients are likely to need admission and urologic intervention could guide efforts to decrease the radiation burden in this population.
The objective of the current study is to identify clinical predictors of admission and urologic intervention. We hypothesized that prediction models for urologic intervention would differ based on whether or not patients were admitted from the ED, as patients admitted for kidney stones are usually clinically distinguishable from those who are discharged. Thus, in the process of building regression models, we stratified our models by patient disposition. Finally, in light of recent evidence suggesting the non-inferiority of renal ultrasound compared to CT,15 we a priori derived and compared models both including and excluding CT results, using instead the presence of hydronephrosis on renal ultrasound.
Materials and Methods
This study utilized data from a prospective, observational study conducted to determine predictors of ureteral stone on CT.17 Patients were enrolled at two centers: Yale-New Haven Hospital (an urban, academic, level I trauma center and teaching hospital) and the Shoreline Medical Center (a free-standing, suburban ED). Eligible patients were those aged 18 years or older presenting to the emergency department between May, 2011 and February, 2013 and undergoing an unenhanced CT scan of the abdomen and pelvis for suspected renal colic. Patients were excluded if they were pregnant, currently incarcerated or in police custody, or if English was not their primary language. The Human Investigation Committee of the Yale Institutional Review Board approved this study and written informed consent was obtained from all enrolled patients. This study was registered with www.clinicaltrials.gov (NCT01352676).
The methods for this study have been described previously.17 Briefly, trained research assistants (RAs) enrolled consecutive patients undergoing unenhanced CT for suspected renal colic. The protocol included renal point-of-care limited ultrasound (PLUS) performed and interpreted by an emergency clinician (resident or attending physician) prior to the patient undergoing CT scan. RAs recorded provider interpretations of renal PLUS including the presence and degree of hydronephrosis (none, mild, moderate or severe). CT imaging results, including the presence, size, and location of any stones, presence and degree of hydronephrosis (none, mild, moderate or severe), and presence of perinephric stranding, were abstracted from dictated attending radiologist reports after the visit by RAs blinded to clinical variables and patient outcome.
The primary outcomes in this study were need for (1) hospital admission during the index ED visit and (2) urologic intervention within 90 days of the index visit in patients with a CT-confirmed symptomatic ureteral stone. A symptomatic stone was considered present on non-enhanced CT if it was located in the collecting system from the renal pelvis to the uretero-vesicular junction on the same side as the patient’s presenting pain based on the dictated CT report. Parenchymal and bladder stones were noted, but were not considered symptomatic for this analysis. CT reports explicitly stating “signs of a passed stone” were analyzed as having had a symptomatic stone.
All patients enrolled in this study received both a CT scan and an ultrasound, however all other management, including administration of analgesics, hydration, antibiotics, urologic consultation/intervention and the decision to admit or discharge were left to the discretion of the treating physicians.
Urologic intervention was determined at 90-day follow-up interview and subjects were asked whether or not they had undergone any procedures since ED discharge including lithotripsy, ureteral stenting, or surgical stone removal. Enrolled patients were initially called by RAs at 90 days to determine if urologic intervention was performed after discharge. If patients were not reached on initial call, a follow-up phone call and follow-up letter was sent to the patient’s home address. For patients unable to be reached by initial call, follow-up call or letter, chart review was performed to assess for urologic intervention. Patients who could not be contacted or had no subsequent visits after index visit in their chart were considered lost to follow-up. RAs performing follow-up interviews and chart extractions to determine need for urologic intervention were blinded to clinical data and potential predictor variables collected during the index ED visit.
Descriptive statistics were calculated using proportions for categorical variables and medians with interquartile ranges for continuous data. We used analysis of the descriptive data, literature review, and consensus of the authors to select candidate predictor variables for hospital admission and urologic intervention. Odds ratios with associated 95% confidence intervals and p-values were calculated by the Fisher Exact Method. Dichotomous variables were created for abnormal serum white blood cell counts (>11.0 × 109/L) and serum creatinine (>1.5 mg/dL). Two separate variables were created for presence of hydronephrosis on renal PLUS or CT scan: any hydronephrosis (mild, moderate or severe versus none) and moderate or greater hydronephrosis (moderate or severe versus none or mild). Two nominal logistic regression models examined predictors independently associated with hospital admission from the ED and were constructed including all candidate variables: Model (1) included both CT and renal PLUS findings. Model (2) excluded CT findings and included only emergency provider-performed renal PLUS assessment for presence and degree of hydronephrosis. Next we constructed two nominal logistic regression models to assess for predictors independently associated with urologic intervention: Model (3) includes CT findings while Model (4) included only renal PLUS results. Finally, Models (3) and (4) were stratified by disposition (admit or discharge). For all models, collinearity was assessed through calculation of variance inflation factors and variable tolerance. No variable possessed a tolerance of <0.1 or VIF>10, therefore all variables were retained in the model. Significance testing was conducted at the alpha=0.05 level. Goodness of fit was assessed through Akaike information criterion (AIC) and Hosmer-Lemeshow tests. The c-statistic, or area under the receiver operator curve (AUC), was calculated and used to compare various models. Data analyses were performed using JMP ® Pro (version 12.0, SAS Institute, Inc. Cary, NC).
Results
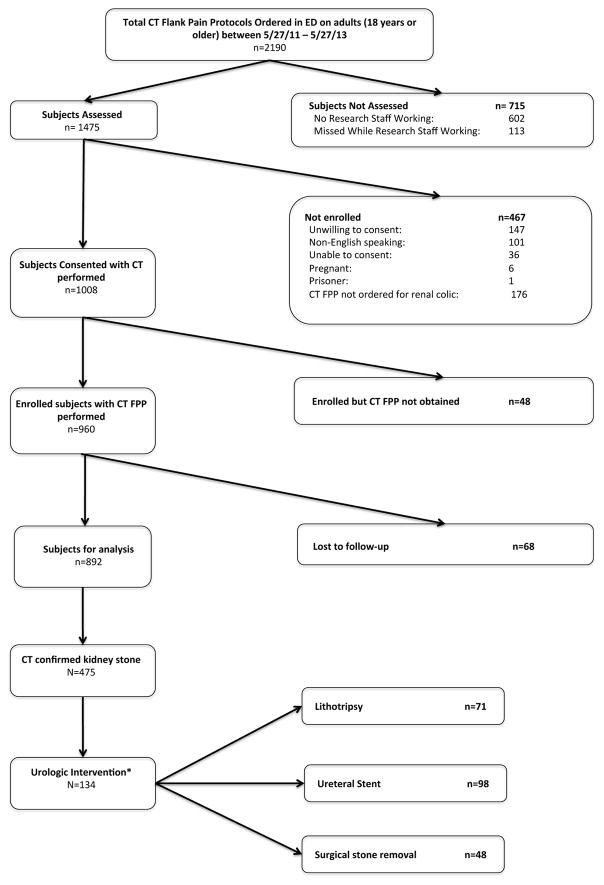
We enrolled 960 patients who received a non-contrast CT of the abdomen and pelvis for suspected renal colic, of which 892 completed follow-up (93%). A CT-confirmed symptomatic ureteral stone was identified in 475 (53%, Table 1). Twenty percent (95/475) of patients diagnosed with renal colic were admitted from the ED including three taken directly to the operation room for a procedure. One or more urologic interventions was performed in 28% (134/475) within 90 days of the index visit (Figure 1) with stent placement being the most common (73%, 98/134) followed by lithotripsy (53%, 71/134) and surgical stone removal (36%, 48/134).
Table 1.
Baseline characteristics for enrolled patients by disposition and need for urologic intervention within 90 days of index visit. IQR: interquartile range, CVA: costovertebral angle, ED: emergency department, hpf: high-powered field, RBC: red blood cell, WBC: white blood cell, CT: computed tomography scan, PLUS: renal point-of-care limited ultrasound, UTI: urinary tract infection
| Characteristic | All Patients (n = 475) | Disposition | Urologic Intervention | ||
|---|---|---|---|---|---|
| Discharge (n=380, 80%) | Admit (n=95, 20%) | No (n=341, 71.8%) | Yes (n=134, 28.2%) | ||
| Demographics | |||||
|
| |||||
| Age, median (IQR) | 46 (35 – 57) | 45 (34 – 56) | 48 (38 – 59) | 45 (33.5 – 57) | 48 (39 – 57) |
| Female gender | 185 (38.9) | 139 (36.6) | 46 (48.4) | 121 (35.5) | 64 (47.8) |
| Race | |||||
| White | 418 (88) | 338 (89) | 80 (84.2) | 302 (88.6) | 116 (86.6) |
| Black | 39 (8.2) | 27 (7.1) | 12 (12.6) | 25 (7.3) | 14 (10.5) |
| Other | 18 (3.8) | 15 (4) | 3 (3.2) | 14 (4.1) | 4 (3) |
|
| |||||
| Physical Exam and Vital Signs | |||||
|
| |||||
| Documented hemodynamic instability | 26 (5.5) | 14 (3.7) | 12 (12.6) | 12 (3.5) | 14 (10.5) |
| CVA tenderness to palpation | 281 (59.2) | 212 (55.8) | 69 (72.6) | 188 (55.1) | 93 (69.4) |
|
| |||||
| Presenting Symptoms | |||||
|
| |||||
| Pain duration at presentation | |||||
| No pain | 1 (0.2) | 0 (0) | 1 (1.1) | 1 (0.3) | 0 (0) |
| < 6 hours | 187 (39.3) | 162 (42.6) | 25 (26.3) | 154 (45.2) | 33 (24.6) |
| 6 hours – 1 day | 181 (38.1) | 148 (39) | 33 (34.7) | 122 (35.8) | 59 (44) |
| >1 day – 1 week | 90 (18.9) | 57 (15) | 33 (34.7) | 58 (17) | 32 (23.9) |
| >1 week | 16 (3.3) | 13 (3.4) | 3 (3.2) | 6 (1.8) | 10 (7.5) |
| >=6 hours | 287 (60) | 218 (57.4) | 69 (72.6) | 186 (54.6) | 101 (75.4) |
| Nausesa and/or vomiting | |||||
| None | 89 (18.7) | 76 (20) | 13 (13.7) | 67 (19.7) | 22 (16.4) |
| Nausea alone | 131 (27.6) | 109 (28.7) | 22 (23.2) | 100 (29.3) | 31 (23.1) |
| Nausea and vomiting | 255 (53.7) | 195 (51.3) | 60 (63.2) | 174 (51) | 81 (60.5) |
| Subjective fever and/or chills | 155 (45.5) | 114 (30) | 41 (43.2) | 100 (29.3) | 55 (41) |
|
| |||||
| Prior Urologic History | |||||
|
| |||||
| Prior History of kidney stones | 204 (42.9) | 135 (35.5) | 68 (71.6) | 116 (34) | 87 (64.9) |
| History of urologic procedure | 79 (16.6) | 42 (11.1) | 37 (39) | 27 (7.9) | 52 (38.8) |
|
| |||||
| Laboratory Test Results | |||||
|
| |||||
| Results of urinanalysis available | 441 (92.8) | 356 (93.7) | 85 (89.5) | 317 (93) | 124 (92.5) |
| Presence of leukocyte esterase | 113 (23.8) | 72 (19) | 41 (43.2) | 66 (19.4) | 47 (35.1) |
| Presence of nitrites | 21 (4.4) | 12 (3.2) | 9 (9.5) | 9 (2.6) | 12 (9) |
| RBC count on microscopy (cells/hpf) | |||||
| <2 to none | 79 (16.6) | 50 (13.2) | 29 (30.5) | 43 (12.6) | 36 (26.9) |
| 2 – 5 | 73 (15.4) | 58 (15.3) | 15 (15.8) | 53 (15.5) | 20 (14.9) |
| 6 – 10 | 59 (12.4) | 49 (12.9) | 10 (10.5) | 45 (13.2) | 14 (10.5) |
| 11 – 30 | 87 (18.3) | 69 (18.2) | 18 (19) | 64 (18.8) | 23 (17.2) |
| >30/many | 143 (30.1) | 130 (34.2) | 13 (13.7) | 112 (32.8) | 31 (23.1) |
| WBC count on microscopy (cells/hpf) | |||||
| <2 to none | 269 (56.6) | 229 (60.3) | 40 (42.1) | 206 (60.4) | 63 (47) |
| 2 – 5 | 106 (22.3) | 93 (24.5) | 13 (13.7) | 80 (23.5) | 26 (19.4) |
| 6 – 10 | 28 (5.9) | 19 (5) | 9 (9.5) | 16 (4.7) | 12 (9) |
| 11 – 30 | 27 (5.7) | 10 (2.6) | 17 (17.9) | 11 (3.2) | 16 (11.9) |
| >30/many | 11 (2.3) | 5 (1.3) | 6 (6.3) | 4 (1.2) | 7 (5.2) |
| >= 6 | 66 (14) | 34 (9) | 32 (33.7) | 31 (9.1) | 35 (26.1) |
| Creatinine (mg/dL), median (IQR) | 1 (0.8 – 1.2) | 1 (0.8 – 1.2) | 1.1 (0.8 – 1.5) | 1 (0.8 – 1.2) | 1 (0.8 – 1.2) |
| Peripheral WBC, median (IQR) | 9.9 (7.8 – 12.1) | 9.7 (7.7 – 11.8) | 10.6 (8.3 – 13.1) | 9.8 (8 – 11.8) | 10.1 (7.7 – 13) |
|
| |||||
| Findings on Imaging | |||||
|
| |||||
| Any hydronephrosis on CT scan | 413 (86.9) | 325 (85.5) | 88 (92.6) | 292 (85.6) | 121 (90.3) |
| Moderate or greater hydro on CT | 107 (22.5) | 74 (19.5) | 33 (34.7) | 66 (19.4) | 41 (30.6) |
| Stone size >5mm on CT | 104 (21.9) | 58 (15.3) | 46 (48.4) | 28 (8.2) | 76 (43.2) |
| Location of stone on CT | |||||
| Uretero-pelvic junction | 37 (7.8) | 22 (5.8) | 15 (15.8) | 12 (3.5) | 25 (18.7) |
| Proximal ureter | 76 (16) | 58 (15.3) | 18 (19) | 44 (12.9) | 32 (23.9) |
| Mid ureter | 52 (10.9) | 34 (9) | 18 (19) | 32 (9.4) | 20 (14.9) |
| Distal ureter | 97 (20.4) | 75 (19.7) | 22 (23.2) | 71 (20.8) | 26 (19.4) |
| uretero-vesicular junction | 179 (37.7) | 159 (41.8) | 20 (21.1) | 149 (43.7) | 30 (22.4) |
| Mid ureter or higher | 165 (34.7) | 114 (30) | 51 (53.7) | 88 (25.8) | 77 (57.5) |
| Signs of passed stone | 34 (7.2) | 32 (8.4) | 2 (2.1) | 24 (7) | 1 (0.8) |
| Any hydronephrosis on renal PLUS | 285 (60) | 224 (59) | 61 (64.2) | 201 (58.9) | 84 (62.7) |
| Moderate or greater hydro on PLUS | 121 (25.5) | 85 (22.4) | 36 (37.9) | 74 (21.7) | 47 (35.1) |
|
| |||||
| Treatments given | |||||
|
| |||||
| Antibiotics given in the ED | 80 (16.8) | 38 (10) | 42 (44.2) | 37 (10.9) | 43 (32.1) |
| Opiates given in the ED | 345 (72.6) | 266 (70) | 79 (83.2) | 242 (71) | 103 (76.9) |
Figure 1.
Prospective enrollment process for ED patients with suspected renal colic undergoing non-contrast CT of the abdomen and pelvis (CT flank pain protocol, CT FPP). *Note: Patients may have had more than one type of urologic intervention.
Hospital Admission
Characteristics associated with admission are shown in Table 2. In the adjusted model patients with stones >5mm on CT were more likely to be admitted as were those with a history of a prior urologic procedure and administration of opiate analgesia or antibiotics in the ED. Predictors of admission were similar if CT findings were not included the model. In the PLUS-only model, moderate or greater hydronephrosis was associated with an increased odds of admission. The AUCs for models predicting admission, both without and without CT findings, were similar (0.871 and 0.842, respectively).
Table 2.
Predictors of admission for patients with CT-confirmed ureteral stone with and without CT findings.
| Unadjusted (n=475) | Adjusted Estimates with CT findings (n=445) | Adjusted Estimates without CT results (n=445) | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Characteristic | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | ||
| History of urologic procedure | 5.1 (3 – 8.7) | <0.001 | 2.8 (1.4 – 5.4) | 0.003 | *** | 4.2 (2.2 – 8) | <0.001 | *** |
| Pain duration >=6 hours on presentation | 2 (1.2 – 3.2) | 0.007 | 0.9 (0.5 – 1.8) | 0.811 | 1.1 (0.6 – 2.1) | 0.668 | ||
| Hemodynamic instability | 3.8 (1.7 – 8.5) | 0.002 | 1.9 (0.5 – 6.4) | 0.326 | 2 (0.7 – 6) | 0.21 | ||
| CVA tenderness to palpation on exam | 2.1 (1.3 – 3.4) | 0.003 | 1.6 (0.9 – 3.2) | 0.128 | 1.6 (0.9 – 3.1) | 0.112 | ||
| Subjective fever or chills | 3.8 (2.2 – 6.8) | <0.001 | 1.4 (0.8 – 2.6) | 0.273 | 1.5 (0.8 – 2.7) | 0.183 | ||
| Evidence of UTI* | 3 (1.7 – 5.1) | <0.001 | 1.2 (0.5 – 2.5) | 0.694 | 1.1 (0.5 – 2.4) | 0.728 | ||
| Serum WBC > 11 × 109/L | 1.7 (1 – 2.7) | 0.037 | 1.2 (0.7 – 2.3) | 0.51 | 1.1 (0.6 – 2) | 0.699 | ||
| Serum creatinine > 1.5 mg/dL | 11 (4.6 – 25) | <0.001 | 16 (5.6 – 50) | <0.001 | *** | 12 (4.6 – 35) | <0.001 | *** |
| Moderate or greater hydronephrosis on CT | 2.2 (1.3 – 3.6) | 0.002 | 1.9 (1 – 3.7) | 0.056 | -- | -- | ||
| Large stone (>5mm) on CT | 5.2 (3.2 – 8.5) | <0.001 | 3.4 (17 – 6.8) | <0.001 | *** | -- | -- | |
| Proximal stone location on CT (midureter or above) | 2. 7 (1.7 – 4.3) | <0.001 | 1.8 (0.9 – 3.4) | 0.075 | -- | -- | ||
| Moderate or greater hydronephrosis on renal PLUS | (1.3 – 3.4) | 0.004 | 1.8 (0.9 – 3.4) | 0.083 | 2.2 (1.2 – 4.1) | 0.012 | *** | |
| Antibiotics given in the ED | 7.1 (4.2 – 12) | <0.001 | 6 (3.1 – 12) | <0.001 | *** | 6 (3.1 – 12) | <0.001 | *** |
| Opiates given in the ED | 2.1 (1.2 – 3.8) | 0.01 | 2.7 (1.3 – 6.1) | 0.008 | *** | 2 (1 – 4.3) | 0.049 | *** |
|
|
|
|||||||
| Model AUC | 0.871 | 0.842 | ||||||
|
|
|
|||||||
Indicates statistically significant predictors in multivariable analysis.
Patients were considered to have evidence of UTI if leukocyte esterase and/or 6 or more WBCs were present on urinalysis.
AUC: area under the curve (c-statistic), OR: odds ratio, CI: confidence interval, CVA: costovertebral angle, ED: emergency department, hpf: high-powered field, WBC: white blood cell, CT: computed tomography scan, PLUS: renal point-of-care limited ultrasound, UA
Urologic Intervention
Multivariate predictors (Table 3) of urologic intervention included history and physical exam findings (CVA tenderness, longer duration of pain, prior urologic procedure) as well as imaging findings (large or proximal stone) and administration of opiates or antibiotics in the ED. In the PLUS-only model significant predictors of urologic intervention were again similar, though presence of moderate or greater hydronephrosis on renal PLUS was also significantly associated. The models with and without CT findings demonstrated AUCs of 0.887 and 0.804, respectively.
Table 3.
Predictors of urologic intervention at 90 days for patients with CT-confirmed ureteral stone with and without CT findings.
| Unadjusted Estimates (n=475) | Adjusted Estimates with CT findings (n=445) | Adjusted Estimates without CT results (n=445) | ||||||
|---|---|---|---|---|---|---|---|---|
| Predictors of Urologic Intervention | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | ||
| History of urologic procedure | 7.4 (4.4 – 12) | <0.001 | 5.7 (2.8 – 11) | <0.001 | *** | 7.5 (4.2 – 14) | <0.001 | *** |
| Pain duration >=6 hours on presentation | 2.6 (1.6 – 4) | <0.001 | 1.9 (1 – 3.5) | 0.042 | *** | 2.1 (1.3 – 3.7) | 0.005 | *** |
| Hemodynamic instability | 3.2 (1.4 – 7.1) | 0.006 | 2.6 (0.7 – 8.9) | 0.13 | 2.5 (0.9 – 7) | 0.076 | ||
| CVA tenderness to palpation on exam | 1.8 (1.2 – 2.8) | 0.005 | 2.6 (1.4 – 5.1) | 0.002 | *** | 1.8 (1.1 – 3.1) | 0.026 | *** |
| Subjective fever or chills | 1.7 (1 – 3) | 0.067 | 1.4 (0.8 – 2.5) | 0.28 | 1.5 (0.9 – 2.5) | 0.142 | ||
| Evidence of UTI | 2.5 (1.5 – 4.2) | <0.001 | 0.9 (0.4 – 2) | 0.86 | 1.1 (0.6 – 2.1) | 0.81 | ||
| Serum WBC > 11 × 109/L | 1.4 (0.9 – 2.1) | 0.154 | 1 (0.6 – 1.8) | 0.92 | 1 (0.6 – 1.6) | 0.896 | ||
| Serum creatinine > 1.5 mg/dL | 3.2 (1.4 – 7.1) | 0.006 | 2.5 (0.8 – 7.3) | 0.11 | 2.3 (0.9 – 5.9) | 0.07 | ||
| Moderate or greater hydronephrosis on CT | 1.8 (1.2 – 2.9) | 0.01 | 0.9 (0.5 – 1.8) | 0.85 | -- | -- | ||
| Large stone (>5mm) on CT | 15 (8.7 – 25) | <0.001 | 12 (6.3 – 25) | <0.001 | *** | -- | -- | |
| Proximal stone location on CT (mid-ureter or above) | 3.9 (2.6 – 5.9) | <0.001 | 2 (1.1 – 3.7) | 0.019 | *** | -- | -- | |
| Moderate or greater hydronephrosis on renal PLUS | 1.9(1.3 – 3) | 0.003 | 1.7 (0.9 – 3.1) | 0.101 | 2.1 (1.2 – 3.6) | 0.006 | *** | |
| Antibiotics given in the ED | 3.9 (2.4 – 6.4) | <0.001 | 2.2 (1.1 – 4.4) | 0.025 | *** | 2.7 (1.5 – 5.1) | 0.002 | *** |
| Opiates given in the ED | 1.4 (0.9 – 2.2) | 0.21 | 2 (1 – 4.1) | 0.043 | *** | 1.4 (0.8 – 2.6) | 0.235 | *** |
|
| ||||||||
| Model AUC | 0.887 | 0.804 | ||||||
Indicates statistically significant predictors in multivariable analysis.
Patients were considered to have evidence of UTI if leukocyte esterase and/or 6 or more WBCs were present on urinalysis.
AUC: area under the curve (c-statistic), OR: odds ratio, CI: confidence interval, CVA: costovertebral angle, ED: emergency department, hpf: high-powered field, WBC: white blood cell, CT: computed tomography scan, PLUS: renal point-of-care limited ultrasound, UA
Urologic Intervention by Disposition
Admitted patients were more likely to receive a urologic intervention (71.6% versus 17.4%, OR 12, 95% CI [7.1 – 20]) and represented half (68/134) of all interventions in the total cohort. The previous regression models were subsequently stratified by disposition. For admitted patients (Table 4a), a history of urologic procedure, CVA tenderness, evidence of UTI, larger, more proximal stones and hydronephrosis on renal PLUS were associated with need for intervention. Excluding CT results from the model, only history of urologic procedure remained significant. For discharged patients (Table 4b), prior procedure, CVA tenderness and larger stones were associated with subsequent procedure if CT findings were included. When only renal PLUS findings were used, history of urologic procedure and longer duration of pain at presentation were predictive of need for intervention. Notably, among 380 discharged patients, 58 (15.3%) had a stone larger than 5mm, and intervention occurred in 36 (62.1%) of these patients.
Table 4.
Comparison of predictors of urologic intervention at 90 days with and without CT findings for admitted (4a) and discharged (4b) patients.
| Table 4a. Predictors of Urologic Intervention at 90 Days with CT-Confirmed Ureteral Stone With and Without CT Findings -- Admitted Patients
| ||||||
|---|---|---|---|---|---|---|
| Adjusted Estimates with CT findings (n=90) | Adjusted Estimates without CT results (n=90) | |||||
|
| ||||||
| Predictors of Urologic Intervention | OR (95% CI) | p-value | OR (95% CI) | p-value | ||
| History of urologic procedure | 7.4 (1.8– 41) | 0.004 | *** | 5.1 (1.5 – 21) | 0.007 | *** |
| Pain duration >=6 hours on presentation | 3 (0.8 – 12) | 0.11 | 2.8 (0.9– 9.7) | 0.082 | ||
| Hemodynamic instability | 5.9 (0.5 –155) | 0.156 | 3.1 (0.5 – 64) | 0.269 | ||
| CVA tenderness to palpation on exam | 6.1 (1.2 – 39) | 0.03 | *** | 2.3 (0.6 – 9.3) | 0.211 | |
| Subjective fever | 0.9 (0.2 – 3.6) | 0.88 | 0.8 (0.2 – 2.5) | 0.644 | ||
| Evidence of UTI | 0.2 (0.02 – 0.9) | 0.04 | *** | 0.6 (0.2 – 2.3) | 0.421 | |
| Serum WBC > 11 × 109/L | 2.3 (0.6 – 9) | 0.2 | 1.2 (0.4 – 3.6) | 0.71 | ||
| Serum creatinine > 1.5 mg/dL | 1.1 (0.2 – 5.4) | 0.91 | 0.8 (0.2 – 3) | 0.726 | ||
| Moderate or greater hydronephrosis on CT | 0.5 (0.1 – 2) | 0.332 | -- | -- | ||
| Large stone (>5mm) on CT | 5.4 (1.3 – 30) | 0.023 | *** | -- | -- | |
| Proximal stone location on CT (mid-ureter or above) | 4.2 (1.1 –18) | 0.033 | *** | -- | -- | |
| Moderate or greater hydronephrosis on renal PLUS | 4.9 (1.1 – 31) | 0.04 | *** | 3 (0.9 – 11) | 0.06 | |
| Antibiotics given in the ED | 1.5 (0.4 – 5.5) | 0.56 | 1.7 (0.5 – 5.5) | 0.391 | ||
| Opiates given in the ED | 1.2 (0.2 –6.8) | 0.828 | 1.3 (0.3 – 6.3) | 0.756 | ||
|
| ||||||
| Model AUC | 0.862 | 0.784 | ||||
| Table 4b. Predictors of Urologic Intervention at 90 Days with CT-Confirmed Ureteral Stone With and Without CT Findings -- Discharged Patients.
| ||||||
|---|---|---|---|---|---|---|
| Adjusted Estimates with CT findings (n=355) | Adjusted Estimates without CT results (n=355) | |||||
|
| ||||||
| Predictors of Urologic Intervention | OR (95% CI) | p-value | OR (95% CI) | p-value | ||
| History of urologic procedure | 4 (1.6 – 10) | 0.004 | *** | 6.1 (2.9 – 13) | <0.001 | *** |
| Pain duration >=6 hours on presentation | 2.1 (1 – 4. 6) | 0.056 | 2.2 (1.1 – 4.3) | 0.02 | *** | |
| Hemodynamic instability | 2.2 (1.3 – 11) | 0.396 | 1.8 (0.4 – 6.9) | 0.19 | ||
| CVA tenderness to palpation on exam | 2.9 (1.3 – 7) | 0.007 | *** | 1.5 (0.8 – 3) | 0.192 | |
| Subjective fever or chills | 1.9 (0.9 – 4) | 0.095 | 1.9 (1 – 3.6) | 0.05 | ||
| Evidence of UTI | 1.7 (0.6 – 4.4) | 0.285 | 1.5 (0.7 – 3.4) | 0.349 | ||
| Serum WBC > 11 × 109/L | 0.6 (0.3 – 1.4) | 0.281 | 0.9 (0.5 – 3.3) | 0.803 | ||
| Serum creatinine > 1.5 mg/dL | 2 (0.2 – 14) | 0.511 | 1.4 (0.2 – 8.3) | 0.759 | ||
| Moderate or greater hydronephrosis on CT | 0.7 (0.3 – 1.7) | 0.472 | -- | -- | ||
| Large stone (>5mm) on CT | 22 (9.1 – 57) | <0.001 | *** | -- | -- | |
| Proximal stone location on CT (mid-ureter or above) | 1.5 (0.7 – 3.3) | 0.26 | -- | -- | ||
| Moderate or greater hydronephrosis on renal PLUS | 1.1 (0.5 – 2.4) | 0.868 | 1.5 (0.7 – 3) | 0.271 | ||
| Antibiotics given in the ED | 1.3 (0.4 – 3.9) | 0.593 | 1.3 (0.5 – 3.3) | 0.576 | ||
| Opiates given in the ED | 1.5 (0.7 – 3.5) | 0.34 | 1.1 (0.6 – 2.2) | 0.814 | ||
|
| ||||||
| Model AUC | 0.877 | 0.754 | ||||
Indicates statistically significant predictors in multivariable analysis.
Patients were considered to have evidence of UTI if leukocyte esterase and/or 6 or more WBCs were present on urinalysis.
AUC: area under the curve (c-statistic), OR: odds ratio, CI: confidence interval, CVA: costovertebral angle, ED: emergency department, hpf: high-powered field, WBC: white blood cell, CT: computed tomography scan, PLUS: renal point-of-care limited ultrasound, UA
Discussion
Using prospective data from emergency department patients with CT-confirmed symptomatic ureteral stones we have described factors associated with hospital admission and urologic intervention. Similar to prior studies, approximately 20% of patients were admitted.7 Guidelines for admitting patients with renal colic have not been well elucidated, though expert opinion recommends admission for stone emergencies such as co-existent obstructing stone and renal failure or evidence of urinary tract infection or uncontrolled pain.7,18 Our results reflect these recommendations as markers of kidney injury, infection, antibiotic use, and intravenous opiate analgesia remained significant in regression models. It is worth noting that regression models had similar c-statistics whether or not CT findings such as stone size were included. The presence of moderate or greater hydronephrosis on renal PLUS was significant in the model without CT findings suggesting the combination of clinical findings and US may be useful in the determining the need for admission and urologic consultation.
Although stone size was the strongest predictor of intervention, models substituting hydronephrosis on renal PLUS for CT findings displayed similar accuracy as estimated by the c-statistic (0.887 versus 0.804). This suggests immediate CT scan may offer little additional information with respect to need for urologic intervention compared to US. These results are in line with a recent randomized controlled trial in ED patients of CT versus renal US, which found US to be non-inferior (though need for admission or urologic intervention was not addressed in their study).15 In our analysis, clinical factors such as duration of pain, prior urologic procedures, CVA tenderness on exam and administration of analgesics and antibiotics were independently associated with subsequent intervention in both models. Further research is need to confirm whether such factors can be used to identify subsets of ED patients with ureteral colic that would most benefit from immediate CT and which would be more suitable for delayed CT for persistent symptoms after a trial of spontaneous passage.
Urologic intervention was performed in three out of four admitted patients, which accounted for approximately half of all interventions in our study. In analyses stratified by disposition, predictors of intervention differed. Among discharged patients, history of urologic procedure, CVA tenderness and large stone were associated with subsequent intervention. When CT findings were excluded, procedure history and duration of pain at presentation remained significant. Emergency providers should exercise caution discharging patients with these characteristics without sufficient characterization of the degree of obstruction or urologic consultation as appropriate.
Our study, which was conducted at a single academic center, has several limitations. Management of patients, including administration of antibiotics, type and route of pain medications, and disposition decisions vary considerably between emergency providers. Similarly, reasons for intervention in non-emergent cases may reflect several factors not captured in our study such as prior treatment by a given urologist, practice variation among urologists, and patient preferences. All patients underwent both renal ultrasound and CT scan, and providers were aware of CT findings when making management decisions. As stone size is generally known to be associated with lower likelihood of spontaneous passage,19 it is unknown whether study patients known to have larger stones received an adequate trial of spontaneous passage. Previous studies have shown significant variation in inpatient urologic procedures based on patients’ insurance status, race, day of presentation, and number of urologists operating at a hospital.7,20,21 As such, the generalizability of our results to regions and institutions with different health systems or practice patterns is limited. Additionally, our study did not take into account the availability of low-dose CT, which alters the risk-benefit relationship for CT use, and does not address the issue of operator variability in the performance of ultrasound. While admission was strongly associated with intervention, it may simply be that interventions were planned during admission for convenience rather than a patient being admitted because an intervention is needed. Lastly, the use of Medical Expulsive Therapy (MET) was left to the treating physician and may have affected procedure rate.
Conclusions
Urologic intervention was common among admitted patients and much less common among discharged patients. In renal colic patients that providers intend to discharge without a CT scan, a longer duration of pain at presentation and a history of prior urologic procedure may warrant further imaging or closer follow-up. Our data suggest that factors associated with urologic intervention differ for admitted and discharged patients, and that future research should consider study designs stratifying by disposition. Similarly, the high rate of intervention in admitted patients suggests the clinical factors that lead to admission may also play a role in determining which patients benefit from a CT scan. As discharged patients had a low rate of intervention compared to those admitted, these patients may be more appropriate for an ultrasound-first or delayed-CT diagnostic algorithm.
Acknowledgments
Funding: This study was funded through a grant from the Agency for Healthcare Research and Quality (5R01HS018322-03): Identifying unnecessary irradiation of patients with suspected renal colic. This funding provided resources to assist with the collection, management, analysis and interpretation of the data, and preparation and review of the manuscript. The AHRQ provided funding and oversight of funding, but was not directly involved in collection or cleaning of data, analysis of results, or drafting of the manuscript.
Abbreviations
- ED
Emergency Department
- CT
computed tomography
- CVA
costovertebral angle
- PLUS
point-of-care limited ultrasound
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Scales CD, Smith AC, Hanley JM. Prevalence of kidney stones in the United States. Eur Urol. 2012;62(1):160–165. doi: 10.1016/j.eururo.2012.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fwu C-W, Eggers PW, Kimmel PL. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;83(3):479–486. doi: 10.1038/ki.2012.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.MFL, KMA, UP Percutaneous nephrostomy and ureteric stent insertion for acute renal deobstruction. Consensus based guidance. Br J Med Surg Urol. 2008;1(3):120–125. doi: 10.1016/j.bjmsu.2008.09.002. [DOI] [Google Scholar]
- 4.Ramsey S, Robertson A, Ablett MJ. Evidence-based drainage of infected hydronephrosis secondary to ureteric calculi. J Endourol. 2010;24(2):185–189. doi: 10.1089/end.2009.0361. [DOI] [PubMed] [Google Scholar]
- 5.Preminger GM, Tiselius HG, Assimos DG. 2007 Guideline for the Management of Ureteral Calculi. Eur Urol. 2007;52(6):1610–1631. doi: 10.1016/j.juro.2007.09.107. [DOI] [PubMed] [Google Scholar]
- 6.Türk C, Petřík A, Sarica K. EAU Guidelines on Diagnosis and Conservative Management of Urolithiasis. Eur Urol. 2015:1–7. doi: 10.1016/j.eururo.2015.07.040. [DOI] [PubMed] [Google Scholar]
- 7.Schoenfeld EM, Pekow PS, Shieh M-S, Scales CD, Lagu T, Lindenauer PK. The Diagnosis and Management of Patients with Renal Colic across a Sample of US Hospitals: High CT Utilization Despite Low Rates of Admission and Inpatient Urologic Intervention. PLoS ONE. 2017;12(1):e0169160. doi: 10.1371/journal.pone.0169160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elder JW, Delgado MK, Chung BI, Pirrotta EA, Wang NE. Variation in the Intensity of Care for Patients with Uncomplicated Renal Colic Presenting to U.S. Emergency Departments. JEM. 2016;51(6):628–35. doi: 10.1016/j.jemermed.2016.05.037. [DOI] [PubMed] [Google Scholar]
- 9.Coll DM, Varanelli MJ, Smith RC. Relationship of spontaneous passage of ureteral calculi to stone size and location as revealed by unenhanced helical CT. AJR Am J Roentgenol. 2002;178(1):101–103. doi: 10.2214/ajr.l78.1.1780101. [DOI] [PubMed] [Google Scholar]
- 10.Papa L, Stiell IG, Wells GA. Predicting intervention in renal colic patients after emergency department evaluation. CJEM. 2005;7(2):78–86. doi: 10.1017/s1481803500013026. http://www.ncbi.nlm.nih.gov/pubmed/17355656. [DOI] [PubMed] [Google Scholar]
- 11.Yan JW, McLeod SL, Edmonds ML. Risk Factors Associated with Urologic Intervention in Emergency Department Patients with Suspected Renal Colic. J Emerg Med. 2015;49(July 2014):1–6. doi: 10.1016/j.jemermed.2014.12.085. [DOI] [PubMed] [Google Scholar]
- 12.Moon YJ, Kim HW, Kim JB. Distribution of ureteral stones and factors affecting their location and expulsion in patients with renal colic. Korean J Urol. 2015;56(10):717–721. doi: 10.4111/kju.2015.56.10.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmed A, Gabr AH, Emara A-A. Factors predicting the spontaneous passage of a ureteric calculus of · 10mm. Arab J Urol. 2015;13(2):84–90. doi: 10.1016/j.aju.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dean T, Crozier J, Klim S. Failed validation of risk prediction model for intervention in renal colic patients after emergency department evaluation. ANZ J Surg. 2015 doi: 10.1111/ans.13109. n/a–n/a. [DOI] [PubMed]
- 15.Smith-Bindman R, Aubin C, Bailitz J. Ultrasonography versus Computed Tomography for Suspected Nephrolithiasis. N Engl J Med. 2014;371(12):1100–1110. doi: 10.1056/NEJMoa1404446. [DOI] [PubMed] [Google Scholar]
- 16.Ferrandino MN, Bagrodia A, Pierre SA, et al. Radiation Exposure in the Acute and Short-Term Management of Urolithiasis at 2 Academic Centers. JURO. 2009;181(2):668–73. doi: 10.1016/j.juro.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 17.Moore CL, Bomann S, Daniels B. Derivation and validation of a clinical prediction rule for uncomplicated ureteral stone--the STONE score: retrospective and prospective observational cohort studies. BMJ. 2014;348(mar26_2):g2191. doi: 10.1136/bmj.g2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang RC. Managing Urolithiasis. Ann Emerg Med. 2016;67(4):449–454. doi: 10.1016/j.annemergmed.2015.10.021. [DOI] [PubMed] [Google Scholar]
- 19.Coll DM, Varanelli MJ, Smith RC. Relationship of spontaneous passage of ureteral calculi to stone size and location as revealed by unenhanced helical CT. American Journal of Roentgenology. 2002;178(1):101–3. doi: 10.2214/ajr.178.1.1780101. [DOI] [PubMed] [Google Scholar]
- 20.Blackwell RH, Barton GJ, Kothari AN, et al. Early Intervention during Acute Stone Admissions: Revealing “The Weekend Effect“” in Urological Practice. JURO. 2016:1–7. doi: 10.1016/j.juro.2016.01.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Strope SA, Ye Z, Hollingsworth JM, et al. Weekend Admission and Treatment of Patients With Renal Colic: A Case of Avoidable Variation? Urology. 2009;73(4):720–4. doi: 10.1016/j.urology.2008.09.073. [DOI] [PubMed] [Google Scholar]