Angiocentric glioma is defined in the 2016 WHO Classification as “an epilepsy-associated, stable or slow-growing cerebral tumour primarily affecting children and young adults; histologically characterized by an angiocentric pattern of growth, monomorphous bipolar cells, and features of ependymal differentiation” [5]. Since its initial description by Wang et al in 2005, fewer than 100 cases have been reported, nearly all of which were epilepsy-associated tumors located in the cerebral cortex [1, 8]. Recently, an in-frame MYB-QKI gene fusion was identified as the defining genetic alteration in the majority of tumors pathologically classified as angiocentric gliomas [2, 6]. To date, only rare examples of angiocentric glioma-like tumors located outside of the cerebral hemispheres have been reported, but none have been genetically characterized [3, 7]. Here we report the case of a young child with 6th cranial nerve palsy due to an angiocentric glioma with MYB-QKI fusion centered in the pons; as such, the definition of this tumor type should not be restricted to a location in the cerebral cortex or to seizures as the clinical presentation.
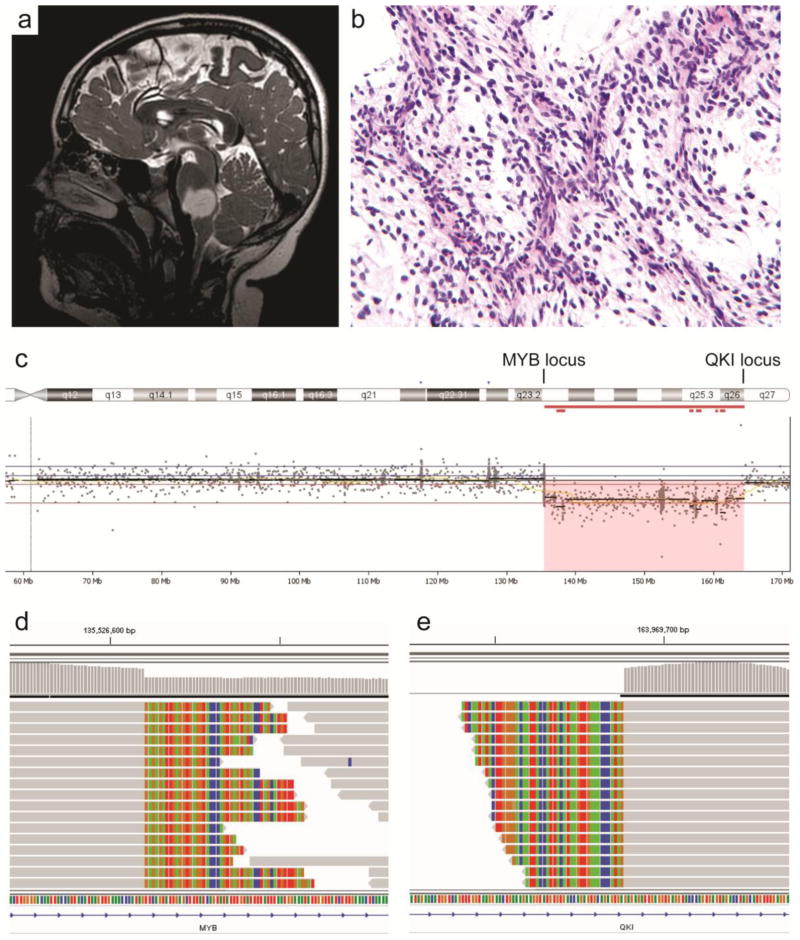
A seven year old boy in otherwise good health presented with several months of altered vision, described by his parents as difficulty fixating on objects and intermittent squinting, as well as problems with depth perception causing him to trip or stumble. He had not experienced any symptoms suggestive of seizure activity. Neurologic exam revealed a right 6th cranial nerve palsy but was otherwise intact. Magnetic resonance imaging revealed a well-circumscribed, T2-hyperintense, non-enhancing, 2.5 cm ovoid mass in the inferior pons (Fig. 1a, Supplemental Fig. 1). Stereotactic biopsy of the mass was performed. Intraoperative cytologic preparation and histologic sections revealed a low-grade glial neoplasm consisting of bland bipolar tumor cells with oval nuclei embedded in a myxoid stroma; a prominent angiocentric growth pattern was noted (Fig. 1b, Supplemental Figs. 2 and 3). No appreciable mitotic activity, necrosis, or microvascular proliferation were identified. Rosenthal fibers and eosinophilic granular bodies were not seen. Immunostaining for glial fibrillary acidic protein (GFAP) was positive in the tumor cells with accentuated perivascular staining. The Ki-67 labeling index was estimated at 2%. Immunostaining for IDH1-R132H and histone H3-K27M mutant proteins was negative. While the histologic features were considered most suggestive of pilomyxoid astrocytoma, targeted next-generation sequencing was performed on the UCSF500 Cancer Panel as previously described to help clarify the diagnosis [4]. This revealed an interstitial deletion on chromosome 6q with 5′ breakpoint in the MYB gene and 3′ breakpoint in the QKI gene (Fig. 1c), resulting in a MYB-QKI gene fusion. Sequencing reads demonstrated a fusion junction between intron 15–16 of MYB and intron 4–5 of QKI (Fig. 1d–e), predicted to result in an in-frame fusion protein where the N-terminal portion is composed of exons 1–15 of MYB and the C-terminal portion of exons 5–7 of QKI. No other chromosomal copy number alterations were seen (Supplemental Fig. 4), and no other pathogenic alterations were identified in genes known to be important in the pathogenesis of pediatric gliomas including those seen in pilocytic and pilomyxoid astrocytomas (e.g. BRAF, RAF1, FGFR1, NTRK2, NF1, and KRAS). Subsequent immunohistochemistry for epithelial membrane antigen (EMA) showed paranuclear dot-like staining in a subset of tumor cells (Supplemental Fig. 2f). An integrated diagnosis of angiocentric glioma with MYB-QKI fusion, WHO grade I, was rendered. The patient recovered well from the biopsy and is without additional deficits now one month later. Given the potential risks of surgical resection for a tumor in this location, observation alone versus chemotherapy are currently being contemplated as therapy options.
Figure 1.
Imaging, histologic, and genetic features of the angiocentric glioma located in the brainstem. a, T2-weighted magnetic resonance image demonstrating a sharply demarcated mass within the pons. b, H&E stained section of the tumor demonstrating a low-grade glial neoplasm with myxoid stroma and angiocentric growth pattern. c, Copy number scatter plot for chromosome 6q demonstrating an interstitial deletion with 5′ breakpoint in the MYB gene and 3′ breakpoint in the QKI gene. d–e, Next-generation sequencing reads aligning to intron 15–16 of MYB (d) and intron 4–5 of QKI (e) showing the fusion breakpoints of the MYB-QKI gene fusion.
To the best of our knowledge, a genetically confirmed angiocentric glioma arising outside of the cerebral cortex has not been previously reported prior to this case. While angiocentric gliomas in the cerebral cortex are generally benign and can be cured by surgical excision alone, the clinical behavior of angiocentric gliomas arising in structures that are not amenable to surgical resection, such as the brainstem, is uncertain. This case suggests the need to expand the operational definition of angiocentric glioma beyond those tumors which are epilepsy associated or located in the cerebral hemispheres.
Supplementary Material
Figure S1. Magnetic resonance imaging features of the angiocentric glioma located in the brainstem. Figure S2. Cytologic features of the angiocentric glioma located in the brainstem. Figure S3. Histologic features of the angiocentric glioma located in the brainstem. Figure S3. Chromosomal copy number plot for the angiocentric glioma located in the brainstem.
Acknowledgments
C.N.K. is supported by the Campini Foundation, Alex’s Lemonade Stand Foundation, and Cannonball Kids’ Cancer Foundation. D.A.S. is supported by NIH Director’s Early Independence Award (DP5 OD021403).
Footnotes
Authors’ contributions
EC, AWB, TT, AP, and DAS performed pathologic assessment. DS, JVZ, JPG, and DAS performed genomic analysis. CNK provided neuro-oncology management. NG provided neurosurgical management. EC and DAS wrote the manuscript and created the figures. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests related to this case report.
References
- 1.Ampie L, Choy W, DiDomenico JD, et al. Clinical attributes and surgical outcomes of angiocentric gliomas. J Clin Neurosci. 2016;28:117–122. doi: 10.1016/j.jocn.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 2.Bandopadhayay P, Ramkissoon LA, Jain P, et al. MYB-QKI rearrangements in angiocentric glioma drive tumorigenicity through a tripartite mechanism. Nat Genet. 2016;48:273–282. doi: 10.1038/ng.3500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Covington DB, Rosenblum MK, Brathwaite CD, Sandberg DI. Angiocentric glioma-like tumor of the midbrain. Pediatr Neurosurg. 2009;45:429–433. doi: 10.1159/000277616. [DOI] [PubMed] [Google Scholar]
- 4.Kline CN, Joseph NM, Grenert JP, et al. Targeted next-generation sequencing of pediatric neuro-oncology patients improves diagnosis, identifies pathogenic germline mutations, and directs targeted therapy. Neuro-Oncol. 2017;19:699–709. doi: 10.1093/neuonc/now254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Louis DN, Ohgaki H, Wiestler OD, et al. WHO Classification of Tumours of the Central Nervous System. IARC; Lyon, France: 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qaddoumi I, Orisme W, Wen J, et al. Genetic alterations in uncommon low-grade neuroepithelial tumors: BRAF, FGFR1, and MYB mutations occur at high frequency and align with morphology. Acta Neuropathol. 2016;131:833–845. doi: 10.1007/s00401-016-1539-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rivera-Zengotita M, Kresak J, Pincus D, Yachnis A. Pediatric brainstem tumors with features of angiocentric glioma: report of two cases. J Neuropathol Exp Neurol. 2014;73:634. Abstract 185. [Google Scholar]
- 8.Wang M, Tihan T, Rojiani AM, et al. Monomorphous angiocentric glioma: a distinctive epileptogenic neoplasm with features of infiltrating astrocytoma and ependymoma. J Neuropathol Exp Neurol. 2005;64:875–881. doi: 10.1097/01.jnen.0000182981.02355.10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Magnetic resonance imaging features of the angiocentric glioma located in the brainstem. Figure S2. Cytologic features of the angiocentric glioma located in the brainstem. Figure S3. Histologic features of the angiocentric glioma located in the brainstem. Figure S3. Chromosomal copy number plot for the angiocentric glioma located in the brainstem.