Abstract
Purpose
Cardiopulmonary bypass (CPB) induces a significant inflammatory response that may increase the risk for delirium. We hypothesized that exposure to CPB during coronary artery bypass grafting surgery would correlate with an increased risk of delirium and would be associated with several other outcomes.
Methods
We reviewed clinical data from two databases at our medical center, the Cardiac Surgery Perioperative Outcomes Database and the Society of Thoracic Surgeons Database. Patients undergoing elective coronary artery bypass grafting surgery (on-pump and off-pump) from November 1, 2009 to September 30, 2015 were included in the study. Delirium was defined as any positive CAM-ICU exam following surgery during the ICU course. We performed logistic regression to isolate the association between CPB exposure and delirium adjusted for predetermined risk factors and potential confounders.
Results
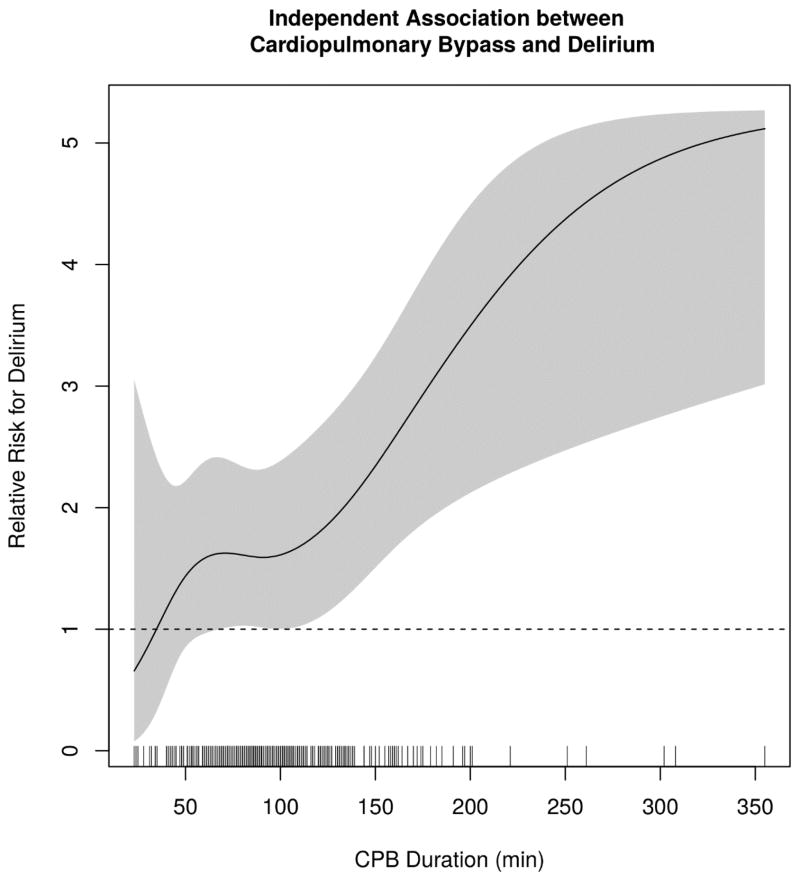
During the study period, a total of 2,280 patients underwent elective coronary artery bypass grafting surgery with 384 patients (16.9%) exposed to CPB. Delirium was diagnosed in 451 patients (19.8%). CPB exposure demonstrated a significant independent association with delirium (P = 0.002). The adjusted relative risk (RR) of delirium was 2.18 (95% CI, 1.39 to 3.07; P = 0.002) among patients exposed to CPB for 142 minutes (90th percentile of CPB duration), compared to a RR of only 1.51 (95% CI, 0.92 to 2.29; P = 0.10) for those on CPB for 54 minutes (10th percentile).
Conclusions
CPB use and duration of use were associated with an increased risk of delirium in patients undergoing coronary artery bypass grafting surgery.
Introduction
Background
Up to 50% of patients older than 60 years of age experience postoperative delirium following cardiac surgery (1). Delirium is associated with many adverse hospital outcomes, including increased mortality and nosocomial complications, poor one year functional recovery, and even postoperative cognitive decline (POCD) (2–4). Studies investigating medications and other interventions to reduce the incidence of delirium have been conducted (5), although the results have yet to truly influence clinical practice. A theory behind the development of delirium is that systemic inflammation causes disruption of the blood-brain barrier (BBB) leading to a neuroinflammatory process in which neurons are susceptible to injury and dysfunction (6). Therefore, a condition or exposure which produces an inflammatory response, such as cardiopulmonary bypass (CPB), may increase the risk for delirium.
Several biomarkers implicated in the neuroinflammatory pathway have been investigated in POCD and also delirium after cardiac surgery (6–8). Studies have shown increases in biomarker levels, such as S100β for BBB disruption and neuron specific enolase for neuronal injury, to be indicative of cerebral damage in patients undergoing on-pump cardiac surgery compared to off-pump cases (9–11) which may lead to a lower prevalence of delirium (12). These findings suggest a greater inflammatory response with exposure to CPB.
Previous studies have supported a link between delirium and POCD, suggesting that the cognitive disturbance seen in each condition may be related (13, 14). Investigators have evaluated whether or not differences in POCD exist between patients exposed to CPB and those not exposed during cardiac surgery. The results are inconclusive with some suggesting greater POCD in CPB patients (15), while others found no difference (16, 17). An association between CPB and delirium has yet to be studied and is the main objective of our study.
Accordingly, we completed the study to test the hypothesis that exposure to CPB during coronary artery bypass surgery would be associated with an increased incidence of postoperative delirium.
Methods
The Society of Thoracic Surgeons National Adult Cardiac Database (STS-NCD) was established in 1989 to compile perioperative data on patients undergoing cardiac surgery. Data are collected quarterly from Vanderbilt University Medical Center (VUMC) and entered into the STS-NCD. The Cardiac Surgery Perioperative Outcomes Database (POD) at VUMC is an institutional review board (IRB) approved data registry of cardiac surgical patients. The POD links and stores patient information from the VUMC electronic medical record. Information included in the POD is extensive including laboratory values, medical conditions, patient history, and some perioperative information such as medications administered and surgical times. Both databases contain prospectively collected data on cardiac surgery patients at VUMC stored and managed using REDCap electronic data capture tools (18).
Data from the STS database at VUMC and the POD were linked using electronic medical record numbers and date of surgery to create a unique identifier. The data quality was verified by independent investigators (J.B.O. and F.T.B.) with frequent crosschecks for completeness and consistency of the datasets. The STS database for VUMC also undergoes both internal and external audits with internal audits occurring quarterly to crosscheck data for accuracy. This paper has been structured according to the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) criteria for cohort studies (19). The study was reviewed and approved on 09/14/2015 by the VUMC IRB under protocol #151362. The study was registered at ClinicalTrials.gov (NCT02548975) prior to data extraction.
Study Design
This was a historical cohort study of patients undergoing either elective on-pump coronary artery bypass grafting (CABG) or off-pump coronary artery bypass grafting (OPCAB) cardiac surgery at VUMC from November 1, 2009 to September 30, 2015.
Variables
CABG surgeries were defined by the use of CPB at any time during coronary artery bypass grafting. OPCAB surgeries were defined as surgeries in which CPB was not used during coronary artery bypass grafting. Only elective procedures were included in the study, and patients undergoing combined CABG and valve operations were excluded.
Primary Outcome
Delirium was defined as any postoperative positive confusion assessment method for the intensive care unit (CAM-ICU) exam during the ICU course. At our institution, ICU standard practice directs bedside nurses to perform a CAM-ICU twice per 12-hour shift. Delirium is a major emphasis within our institution, and nurses are extensively trained to complete an accurate CAM-ICU exam at bedside. Completing CAM-ICU twice per 12-hour shift is considered standard of care within the ICU, and this frequency was initiated at our institution in 2007. Duration of delirium was defined as total number of days with CAM-ICU positive recorded in the patient’s chart (if a patient was positive for either one or both of the daily assessments, this was still considered a day of delirium). Delirium was not assessed after patients were transferred to the floor.
Secondary Outcomes
In-hospital, 30 day, 60 day, 90 day, and 1-year mortality data were obtained from the POD. Acute kidney injury (AKI) was defined using Kidney Disease: Improving Global Outcome Group (KDIGO) stage 1, 2 or 3 serum creatinine (SCr) criteria (20). The development of postoperative atrial fibrillation (AF) was defined as a report of newly diagnosed AF in the patient’s medical record after surgery. Hospital length of stay (LOS) was reported in days. Postoperative stroke was defined as any confirmed neurological deficit of abrupt onset caused by a disturbance in blood supply to the brain that did not resolve within 24 hours per STS-NCD guidelines.
Statistical Analysis
All patient demographic and clinical data were summarized using counts and percentiles, means and standard deviations (SD), or medians [interquartile range (IQR)] by group (CABG/OPCAB). The Pearson chi-square and Deuchler-Wilcoxon tests were used to make unadjusted comparisons between groups. Logistic regression was performed to determine the adjusted association between exposure to CPB and the risk of delirium, KDIGO stage 1, KDIGO stage 2, atrial fibrillation, and 1-year mortality, adjusting for the following pre-specified risk factors and potential confounders: history of cerebrovascular disease, age, race, body mass index (BMI), current tobacco use, chronic lung disease, history of diabetes, dyslipidemia, end stage renal disease, hypertension, congestive heart failure, myocardial infarction, peripheral arterial disease, cerebrovascular disease, previous cardiac surgery, preoperative hematocrit, SCr, and glomerular filtration rate. The effects of CPB were summarized using an adjusted relative risk (RR) with 95% confidence intervals (CI). The adjusted RR was computed from the adjusted odds ratio using the method of Zhang J and Yu KF (21), where the baseline risk was taken as the marginal risk among OPCAB patients. Goodness-of-fit for logistic regression analyses was examined using the C-statistic. Linear regression was used to quantify the association between CPB exposure and log-transformed LOS while adjusting for the same set of risk factors and confounders. Continuous covariates including CPB duration and age were modeled using restricted cubic splines with four evenly spaced knots. Given the nested relationship between CPB exposure (CABG group) and CPB duration, a multiple degree-of-freedom likelihood ratio test (22) was performed to test for overall associations with the outcomes. The effect of CPB duration versus OPCAB was further summarized by computing the adjusted RR at a sequence of percentiles of CPB duration (10th%=54 minutes, 25th%=73 minutes, 50th%=91 minutes, 75th%=113 minutes, 90th%=142 minutes), with pointwise Wald-type 95% confidence intervals (CI). Normal QQ-plots were used to examine the residuals of linear regression analyses. The normal QQ plots for all the models did not show obvious deviations from the assumption of the normal distribution of the outcomes. The remaining binary outcomes of postoperative stroke, death in hospital, death within 30 days, 60 days, and 90 days were rare, and thus were not analyzed using regression analysis. The statistical significance threshold (P < 0.05) was selected to preserve a 5% testwise type-I error rate. We did not attempt to control the familywise type-I error probability.
Results
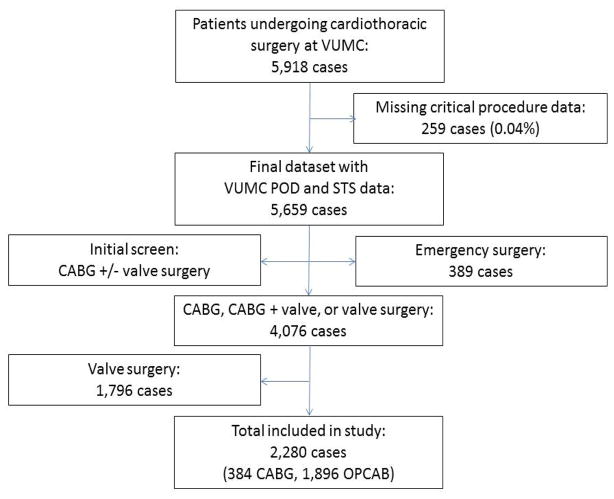
A total of 5,659 cardiac surgery cases met inclusion criteria and were included in the final dataset. Emergency cases (designated by American Society of Anesthesiologists [ASA] physical status classification) and valve surgery cases were excluded leaving 2,280 cases for the study (Figure 1).
Figure 1.
Patient flow diagram. POD = Perioperative Outcome Database. STS = Society of Thoracic Surgeons. CABG = Coronary artery bypass grafting. OPCAB = Off-pump coronary artery bypass grafting.
A total of 386 patients (16.9%) were exposed to CPB and 1,894 patients (83.9%) were not. Delirium was diagnosed in 451 patients (19.8%) during their ICU stay. Median [IQR] age in the cohort was 63 [55,70] years with 22.9% female patients (Table 1). The demographics, including age, gender, and BMI were similar between the groups. The CABG group had more comorbidities than the OPCAB group including history of myocardial infarction, history of congestive heart failure, and current tobacco use. Other comorbidities and baseline laboratory values were similar across both groups.
Table 1.
Patient Demographics by Type of Surgery. Statistical significance for categorical variables tested using Pearson test and Deuchler-Wilcoxon procedure for continuous variables.
| Characteristics | CABG | OPCAB | Combined |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Demographics | |||
|
| |||
| Overall | 386 (16.9) | 1894 (83.1) | 2280 (100) |
| Age, years | 63 (11) | 63 (11) | 63 (11) |
| BMI, kg/m2 | 29.9 (7.9) | 30.1 (6.8) | 30.1 (7.0) |
| Male | 284 (73.6) | 1474 (77.9) | 1728 (77.1) |
|
| |||
| Past Medical History | |||
|
| |||
| Myocardial infarction | 199 (54.1)* | 852 (45.0) | 1051 (46.1) |
| Congestive heart failure | 46 (11.9)† | 106 (5.6) | 152 (6.7) |
| Hypertension | 308 (79.8) | 1497 (79.1) | 1805 (79.2) |
| Cardiac surgery | 12 (3.1) | 64 (3.4) | 76 (3.3) |
| Dyslipidemia | 205 (53.1) | 968 (51.1) | 1173 (51.5) |
| ESRD | 17 (4.4) | 53 (2.8) | 70 (3.1) |
| Peripheral artery disease | 46 (11.9) | 209 (11.0) | 255 (11.2) |
| Diabetes | 166 (43.0) | 848 (44.8) | 1014 (44.5) |
| Chronic lung disease | 77 (19.9) | 408 (21.6) | 485 (21.3) |
| Current tobacco use | 33 (8.5)† | 67 (3.5) | 100 (4.4) |
| Cerebrovascular disease | 75 (19.4) | 322 (17.0) | 397 (17.3) |
| Number of diseased vessels | |||
| 0 | 5 (1.3) | 6 (0.3) | 11 (0.5) |
| 1 | 19 (4.9) | 133 (7.0) | 152 (6.7) |
| 2 | 98 (25.5) | 500 (26.4) | 598 (26.2) |
| 3 | 263 (68.3) | 1255 (66.2) | 1518 (66.6) |
|
| |||
| Baseline Laboratory Values | |||
|
| |||
| SCr | 1.40 (1.78) | 1.24 (1.21) | 1.26 (1.32) |
| eGFR | 71 (26) | 74 (24) | 73 (25) |
| Hematocrit | 38.9 (5.9) | 39.2 (5.4) | 39.2 (5.5) |
SD = standard deviation; BMI = body mass index; ESRD = end stage renal disease; SCr = serum creatinine; eGFR = estimated glomerular filtration rate OPCAB = off-pump coronary bypass grafting surgery; CABG = on-pump coronary artery bypass grafting surgery.
P < 0.05,
P < 0.01.
Outcomes
The unadjusted univariate analyses are outlined in Table 2. After adjusting for risk factors and potential confounders, the estimated effect of CPB was unfavorable for each outcome (Table 3). There was strong evidence that CPB use and duration were associated with an increased risk of postoperative delirium (P = 0.002), after adjusting for potential confounders. There was also an association between CPB use and hospital length of stay (P = 0.047), though without adjusting for an interaction with CPB time itself or other potential covariates, its strength is uncertain. There was no evidence of association between CPB and other outcomes, after adjustment.
Table 2.
Outcome events. Statistical significance for categorical variables tested using Pearson test and Deuchler-Wilcoxon procedure for continuous variables.
| Outcome | CABG | OPCAB | Overall |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Delirium incidence | 92 (23.8)* | 359 (19.0) | 451 (19.8) |
| Delirium duration, days | 0.5 (1.1)* | 0.3 (1.0) | 0.4(1.0) |
| KDIGO | |||
| Stage 1 | 101 (26.9)* | 389 (21.4) | 490 (22.3) |
| Stage 2 | 21 (5.6) | 100 (5.5) | 121 (5.5) |
| Stage 3 | 15 (4.0) | 56 (3.1) | 71 (3.2) |
| Atrial fibrillation | 115 (29.8) | 480 (25.3) | 595 (26.1) |
| Length of stay (days) | |||
| Mean (SD) | 8.3 (5.4)† | 6.9 (3.7) | 7.2 (4.0) |
| Mortality | |||
| In hospital | 4 (1.0) | 9 (0.5) | 13 (0.6) |
| 30 days | 9 (2.3) | 25 (1.1) | 34 (1.5) |
| 60 days | 13 (3.4)* | 28 (1.5) | 41 (1.8) |
| 90 days | 17 (4.4)† | 35 (1.8) | 52 (2.3) |
| 1-year | 21 (5.4)* | 58 (3.1) | 79 (3.5) |
| Stroke | 6 (1.6) | 28 (1.5) | 34 (1.5) |
SD = standard deviation; KDIGO = Kidney Disease: Improving Global Outcome; OPCAB = off-pump coronary bypass grafting surgery; CABG = on-pump coronary artery bypass grafting surgery.
P ≤ 0.05,
P < 0.01.
Table 3.
Adjusted relative risk or relative change in length of stay (e.g., 1.03 corresponds to 3% greater length of stay) for outcomes by percentiles of CPB duration relative to off-pump (10th%=54 minutes, 25th%=73 minutes, 50th%=91 minutes, 75th%=113 minutes, 90th%=142 minutes).
| Outcome | 10th% | 25th% | 50th% | 75th% | 90th% | Overall P-value |
|---|---|---|---|---|---|---|
| RR/ΔLOS (95% CI) | RR/ΔLOS (95% CI) | RR/ΔLOS (95% CI) | RR/ΔLOS (95% CI) | RR/ΔLOS (95% CI) | ||
| Delirium incidence | 1.51 (0.92 to 2.29) | 1.62* (1.02 to 2.39) | 1.59* (1.01 to 2.32) | 1.71* (1.04 to 2.55) | 2.18† (1.39 to 3.07) | 0.002 |
| KDIGO | ||||||
| Stage 1 | 1.09 (0.61 to 1.81) | 1.14 (0.66 to 1.82) | 1.28 (0.76 to 1.98) | 1.46 (0.84 to 2.28) | 1.66 (0.97 to 2.54) | 0.44 |
| Stage 2 | 0.11 (0.01 to 6.06) | 0.55 (0.09 to 3.00) | 0.78 (0.16 to 3.56) | 1.04 (0.19 to 4.93) | 1.55 (0.27 to 7.21) | 0.12 |
| Atrial fibrillation | 0.61 (0.32 to 1.08) | 0.87 (0.50 to 1.40) | 1.03 (0.62 to 1.58) | 1.71 (0.69 to 1.81) | 1.28 (0.75 to 1.95) | 0.07 |
| Mortality | ||||||
| 1-year | 1.49 (0.44 to 4.64) | 1.92 (0.64 to 5.30) | 2.52 (0.92 to 6.38) | 3.23 (0.97 to 9.25) | 3.78* (1.08 to 10.91) | 0.41 |
| LOS | 1.03 (0.93 to 1.14) | 1.05 (0.95 to 1.16) | 1.04 (0.94 to 1.15) | 1.06 (0.94 to 1.18) | 1.12 (1.00 to 1.25) | 0.047 |
RR = relative risk; LOS = length of stay; CI = confidence interval; KDIGO = Kidney Disease: Improving Global Outcome.
P < 0.05,
P < 0.01.
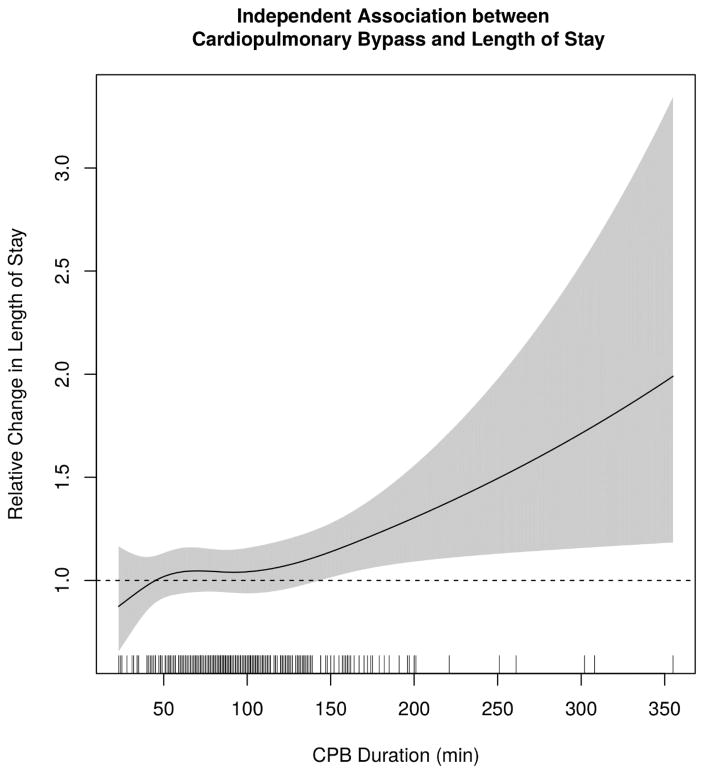
Extended CPB duration was associated with an increased risk of delirium and potentially prolonged hospital stay. Relative to an off-pump procedure, the risk of delirium was more than two times greater (RR, 2.18; 95% CI, 1.39 to 3.07; P = 0.002) among patients who were exposed to CPB for 142 minutes (90th percentile of CPB duration). This compared to adjusted RR that was only 1.51 (95% CI, 0.92 to 2.29; P = 0.10) for those on CPB for 54 minutes (10th percentile) (Figure 2). Hospital LOS was prolonged by 12% (95% CI, 0% to 25%; P = 0.05) and 3% (95% CI, −7% to 14%; P = 0.59) for patients on CPB for 142 and 54 minutes, respectively (Figure 3).
Figure 2.
Independent Association between CPB duration and risk of Delirium. The figure illustrates the adjusted relative risk of delirium as a function of CPB time for on-pump versus off-pump CABG cases (P = 0.002) with pointwise 95% confidence band. The rug plot along the horizontal axis shows the distribution of CPB times in this cohort. CPB = cardiopulmonary bypass; min = minutes.
Figure 3.
Independent Association between CPB duration and relative hospital length of stay. The figure illustrates the relative hospital length of stay as a function of CPB time for on-pump versus off-pump CABG cases (P = 0.047) with pointwise 95% confidence band. The rug plot along the horizontal axis shows the distribution of CPB times in this cohort. CPB = cardiopulmonary bypass; min = minutes.
Discussion
In our study, CPB exposure and duration were significantly associated with the incidence of delirium following cardiac surgery. As duration of CPB increased, hospital LOS also increased though we could not rule out an interaction with delirium itself (or other covariates). Other secondary outcomes, including mortality, postoperative AF and AKI stages 1 and 2, showed increasing odds with prolonged CPB duration although these findings were not statistically significant.
The overall incidence of delirium was 19.8% which corresponds to previous studies (23, 24). The potential effect of CPB on postoperative delirium has yet to be directly studied, but several studies have investigated an association between CPB exposure and POCD which may be linked to postoperative delirium (13, 15–17). A study conducted by Baba et al. found that OPCAB reduced POCD in elderly patients with severe systemic atherosclerosis when neuropsychological dysfunction was measured one week postoperatively as compared to patients undergoing CABG (15). In a meta-analysis including eight randomized trials, no difference was found between OPCAB and CABG patients when evaluating for POCD (16). A pilot study investigating postoperative delirium and POCD found that patients undergoing valve surgery with or without CABG had higher rates of both delirium and POCD than patients undergoing CABG alone (25). This study did not directly analyze the effects of CPB duration with either outcome although the valve surgery with or without CABG group had significantly longer runs on CPB compared to the CABG alone group (173 (53) min vs. 139 (37) min, P = 0.01) (25). Another study which aimed to construct a predictive model for delirium in cardiac surgery patients showed increased odds for delirium with increased duration of surgery (OR, 1.3; 95% CI, 1.1 to 1.5; P < 0.001, per 30 minutes). In our study, as CPB duration increased, the odds of delirium also increased suggesting prolonged CPB duration may contribute to an increased risk of delirium postoperatively.
AKI occurs in up to 30% of cardiac surgery patients (26). A link between on-pump coronary artery grafting cardiac surgery and AKI has been investigated, but previous studies have shown marginal benefit with OPCAB in preventing this insult (27–29). Our study is consistent with these finding as no stage of AKI was significantly different between the CABG and OPCAB groups. Thus our results do not suggest an advantage to avoiding the use of CPB and/or limiting the duration of exposure to CPB for the outcome of AKI in patients undergoing coronary artery bypass grafting surgery.
The development of AF after cardiac surgery is fairly common and the incidence may be as high as 50% (30–32). Considering the significant amount of systemic inflammation generated during on-pump cardiac surgery, the use of CPB may be contributive as a risk factor for patients to develop AF following cardiac surgery (33). This theory was supported when Davoodi et al. showed a higher prevalence of postoperative AF in patients exposed to CPB compared to those who were not (34). In our study, the odds of postoperative AF steadily increased with longer bypass run; however, this finding was not statistically significant and does not support an association between CPB and AF.
The incidence of stroke in our cohort was similar among patients undergoing OPCAB in comparison to CABG patients. A meta-analysis of randomized trials comparing on-pump to off-pump coronary artery bypass grafting surgery demonstrated a 20.7% reduction in stroke incidence in off-pump patients (35). However, a Cochrane review of 86 randomized trials did not show a difference in stroke rates when comparing on-pump to off-pump patients (36). With such a low incidence of stroke in this patient population, finding a statistically significant difference may be difficult. Our results do not advocate a true benefit to OPCAB for a reduction in the rate of postoperative stroke.
Limitations
The cohort’s large population strengthens our study. The databases used in the study (VUMC POD and VUMC STS) contain prospectively collected data. Even so, limitations should be considered before interpreting our results.
Our study was completed at a single, tertiary medical center, and the generalizability of our findings should be considered. There is also an institutional bias towards OPCAB over CABG at VUMC. Another consideration is selection bias for or against on-pump surgery based on surgeon preference or known patient comorbidities. Other surgical techniques such as the use of single or partial aortic cross clamp, how the proximal anastomoses were implanted, the location and type of cannulae used for on-pump CABG, and other variances between surgeons were not accounted for in this study. The analyses were completed with adjusting for several confounders and risk factors; however, residual confounding could be present as the study was non-randomized. Known delirium risk factors such as dementia, decreased functional status, and psychiatric illness were not incorporated into the model (37). Hemodynamic data was not available for inclusion in our analysis, which may differ when comparing OPCAB to CABG patients and also deviations from optimal intraoperative blood pressure could be linked to delirium (38). Delirium was recorded by nurses in the ICU using the CAM-ICU method. Although using the CAM-ICU by nurses was previously validated (39), the consistency in which delirium was measured may not have been similar across all patients. Also, delirium is a waxing and waning condition and the times in which it was measured could have missed delirious episodes in some patients. Sedation protocols for patients included in the study were not standardized and the amount of opiates, benzodiazepines, and other sedatives varied in the study population and this data was not available for inclusion as covariates in the study.
Conclusions
In this large historical study of prospectively collected data, we found an association between CPB use and postoperative delirium in cardiac surgery patients. Given these findings, medical centers should consider avoiding the use of CPB when appropriate. Future studies which randomize patients to either an on-pump or off-pump group when undergoing coronary artery bypass grafting may further elucidate associations between CPB use and adverse outcomes following cardiac surgery.
Supplementary Material
Implication Statement.
Our study assessed the incidence of postoperative delirium following coronary artery bypass grafting surgery (CABG). On-pump surgery was associated with an increased risk of delirium compared to patients undergoing off-pump coronary artery bypass grafting (OPCAB). Prolonged durations of cardiopulmonary bypass also had stronger associations with delirium and other secondary adverse outcomes.
Acknowledgments
The authors thank Leslie Busbee (Department of Cardiac Surgery, Vanderbilt University Medical Center) for assistance with data retrieval.
Funding: This work was supported by the National Institutes of Health under award numbers T32GM108554 (J.B.O.), K23GM102676 (F.T.B.), and R01GM112871 (F.T.B.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Research reported in this publication was also supported by Vanderbilt Institute for Clinical and Translational Research grant support (UL1 TR000445 from NCATS/NIH).
Footnotes
Declaration of interests: none
Trial Registry Number: NCT02548975
References
- 1.Rudolph JL, Jones RN, Levkoff SE, Rockett C, Inouye SK, Sellke FW, et al. Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation. 2009;119(2):229–36. doi: 10.1161/CIRCULATIONAHA.108.795260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saczynski JS, Marcantonio ER, Quach L, Fong TG, Gross A, Inouye SK, et al. Cognitive trajectories after postoperative delirium. The New England journal of medicine. 2012;367(1):30–9. doi: 10.1056/NEJMoa1112923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inouye SK. Delirium in older persons. The New England journal of medicine. 2006;354(11):1157–65. doi: 10.1056/NEJMra052321. [DOI] [PubMed] [Google Scholar]
- 4.Chaput AJ, Bryson GL. Postoperative delirium: risk factors and management: continuing professional development. Canadian journal of anaesthesia = Journal canadien d’anesthesie. 2012;59(3):304–20. doi: 10.1007/s12630-011-9658-4. [DOI] [PubMed] [Google Scholar]
- 5.Mariscalco G, Cottini M, Zanobini M, Salis S, Dominici C, Banach M, et al. Preoperative statin therapy is not associated with a decrease in the incidence of delirium after cardiac operations. The Annals of thoracic surgery. 2012;93(5):1439–47. doi: 10.1016/j.athoracsur.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 6.Rudolph JL, Ramlawi B, Kuchel GA, McElhaney JE, Xie D, Sellke FW, et al. Chemokines are associated with delirium after cardiac surgery. The journals of gerontology Series A, Biological sciences and medical sciences. 2008;63(2):184–9. doi: 10.1093/gerona/63.2.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramlawi B, Rudolph JL, Mieno S, Khabbaz K, Sodha NR, Boodhwani M, et al. Serologic markers of brain injury and cognitive function after cardiopulmonary bypass. Annals of surgery. 2006;244(4):593–601. doi: 10.1097/01.sla.0000239087.00826.b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khan BA, Zawahiri M, Campbell NL, Boustani MA. Biomarkers for delirium--a review. Journal of the American Geriatrics Society. 2011;59(Suppl 2):S256–61. doi: 10.1111/j.1532-5415.2011.03702.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yuan SM. S100 and S100beta: biomarkers of cerebral damage in cardiac surgery with or without the use of cardiopulmonary bypass. Revista brasileira de cirurgia cardiovascular : orgao oficial da Sociedade Brasileira de Cirurgia Cardiovascular. 2014;29(4):630–41. doi: 10.5935/1678-9741.20140084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zheng L, Fan QM, Wei ZY. Serum S-100beta and NSE levels after off-pump versus on-pump coronary artery bypass graft surgery. BMC cardiovascular disorders. 2015;15:70. doi: 10.1186/s12872-015-0050-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonacchi M, Prifti E, Maiani M, Bartolozzi F, Di Eusanio M, Leacche M. Does off-pump coronary revascularization reduce the release of the cerebral markers, S-100beta and NSE? Heart, lung & circulation. 2006;15(5):314–9. doi: 10.1016/j.hlc.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 12.Bucerius J, Gummert JF, Borger MA, Walther T, Doll N, Falk V, et al. Predictors of delirium after cardiac surgery delirium: effect of beating-heart (off-pump) surgery. The Journal of thoracic and cardiovascular surgery. 2004;127(1):57–64. doi: 10.1016/s0022-5223(03)01281-9. [DOI] [PubMed] [Google Scholar]
- 13.Rudolph JL, Marcantonio ER, Culley DJ, Silverstein JH, Rasmussen LS, Crosby GJ, et al. Delirium is associated with early postoperative cognitive dysfunction. Anaesthesia. 2008;63(9):941–7. doi: 10.1111/j.1365-2044.2008.05523.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liang CK, Chu CL, Chou MY, Lin YT, Lu T, Hsu CJ, et al. Interrelationship of postoperative delirium and cognitive impairment and their impact on the functional status in older patients undergoing orthopaedic surgery: a prospective cohort study. PloS one. 2014;9(11):e110339. doi: 10.1371/journal.pone.0110339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baba T, Goto T, Maekawa K, Ito A, Yoshitake A, Koshiji T. Early neuropsychological dysfunction in elderly high-risk patients after on-pump and off-pump coronary bypass surgery. Journal of anesthesia. 2007;21(4):452–8. doi: 10.1007/s00540-007-0538-6. [DOI] [PubMed] [Google Scholar]
- 16.Marasco SF, Sharwood LN, Abramson MJ. No improvement in neurocognitive outcomes after off-pump versus on-pump coronary revascularisation: a meta-analysis. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2008;33(6):961–70. doi: 10.1016/j.ejcts.2008.03.022. [DOI] [PubMed] [Google Scholar]
- 17.Fink HA, Hemmy LS, MacDonald R, Carlyle MH, Olson CM, Dysken MW, et al. Intermediate- and Long-Term Cognitive Outcomes After Cardiovascular Procedures in Older Adults: A Systematic Review. Annals of internal medicine. 2015;163(2):107–17. doi: 10.7326/M14-2793. [DOI] [PubMed] [Google Scholar]
- 18.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Journal of clinical epidemiology. 2008;61(4):344–9. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 20.KDIGO AK. Clinical Practice Guidelines for Acute Kidney Injury. Nephron Clin Pract. 2012;120:c79–c84. doi: 10.1159/000339789. [DOI] [PubMed] [Google Scholar]
- 21.Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. Journal of the American Medical Association. 1998;280(19):1690–1. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 22.Frank E, Harrell J. Regression Modeling Strategies. New York, NY: Springer; 2010. [Google Scholar]
- 23.Tse L, Schwarz SK, Bowering JB, Moore RL, Barr AM. Incidence of and Risk Factors for Delirium After Cardiac Surgery at a Quaternary Care Center: A Retrospective Cohort Study. Journal of cardiothoracic and vascular anesthesia. 2015;29(6):1472–9. doi: 10.1053/j.jvca.2015.06.018. [DOI] [PubMed] [Google Scholar]
- 24.Andrejaitiene J, Benetis R, Sirvinskas E. Postoperative delirium following cardiac surgery: the incidence, risk factors and outcome. Journal of cardiothoracic surgery. 2015;10(Suppl 1):A298. [Google Scholar]
- 25.Hudetz JA, Iqbal Z, Gandhi SD, Patterson KM, Byrne AJ, Pagel PS. Postoperative delirium and short-term cognitive dysfunction occur more frequently in patients undergoing valve surgery with or without coronary artery bypass graft surgery compared with coronary artery bypass graft surgery alone: results of a pilot study. Journal of cardiothoracic and vascular anesthesia. 2011;25(5):811–6. doi: 10.1053/j.jvca.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 26.Lagny MG, Jouret F, Koch JN, Blaffart F, Donneau AF, Albert A, et al. Incidence and outcomes of acute kidney injury after cardiac surgery using either criteria of the RIFLE classification. BMC nephrology. 2015;16:76. doi: 10.1186/s12882-015-0066-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nigwekar SU, Kandula P, Hix JK, Thakar CV. Off-pump coronary artery bypass surgery and acute kidney injury: a meta-analysis of randomized and observational studies. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2009;54(3):413–23. doi: 10.1053/j.ajkd.2009.01.267. [DOI] [PubMed] [Google Scholar]
- 28.Seabra VF, Alobaidi S, Balk EM, Poon AH, Jaber BL. Off-pump coronary artery bypass surgery and acute kidney injury: a meta-analysis of randomized controlled trials. Clinical journal of the American Society of Nephrology : CJASN. 2010;5(10):1734–44. doi: 10.2215/CJN.02800310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheungpasitporn W, Thongprayoon C, Kittanamongkolchai W, Srivali N, OA, OC, Edmonds PJ, et al. Comparison of Renal Outcomes in Off-Pump Versus On-Pump Coronary Artery Bypass Grafting: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Nephrology (Carlton, Vic) 2015 doi: 10.1111/nep.12506. [DOI] [PubMed] [Google Scholar]
- 30.Hogue CW, Jr, Hyder ML. Atrial fibrillation after cardiac operation: risks, mechanisms, and treatment. The Annals of thoracic surgery. 2000;69(1):300–6. doi: 10.1016/s0003-4975(99)01267-9. [DOI] [PubMed] [Google Scholar]
- 31.Narducci ML, Pelargonio G, Rio T, Leo M, Di Monaco A, Musaico F, et al. Predictors of postoperative atrial fibrillation in patients with coronary artery disease undergoing cardiopulmonary bypass: a possible role for myocardial ischemia and atrial inflammation. Journal of cardiothoracic and vascular anesthesia. 2014;28(3):512–9. doi: 10.1053/j.jvca.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 32.Mathew JP, Parks R, Savino JS, Friedman AS, Koch C, Mangano DT, et al. Atrial fibrillation following coronary artery bypass graft surgery: predictors, outcomes, and resource utilization. MultiCenter Study of Perioperative Ischemia Research Group. Jama. 1996;276(4):300–6. [PubMed] [Google Scholar]
- 33.Lamm G, Auer J, Weber T, Berent R, Ng C, Eber B. Postoperative white blood cell count predicts atrial fibrillation after cardiac surgery. Journal of cardiothoracic and vascular anesthesia. 2006;20(1):51–6. doi: 10.1053/j.jvca.2005.03.026. [DOI] [PubMed] [Google Scholar]
- 34.Davoodi S, Karimi A, Ahmadi SH, Marzban M, Movahhedi N, Abbasi K, et al. Early outcome of off-pump versus on-pump coronary revascularization. The Pan African medical journal. 2014;17:309. doi: 10.11604/pamj.2014.17.309.1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sa MP, Ferraz PE, Escobar RR, Martins WN, Lustosa PC, Nunes Ede O, et al. Off-pump versus on-pump coronary artery bypass surgery: meta-analysis and meta-regression of 13,524 patients from randomized trials. Revista brasileira de cirurgia cardiovascular : orgao oficial da Sociedade Brasileira de Cirurgia Cardiovascular. 2012;27(4):631–41. doi: 10.5935/1678-9741.20120106. [DOI] [PubMed] [Google Scholar]
- 36.Moller CH, Penninga L, Wetterslev J, Steinbruchel DA, Gluud C. Off-pump versus on-pump coronary artery bypass grafting for ischaemic heart disease. The Cochrane database of systematic reviews. 2012;3:Cd007224. doi: 10.1002/14651858.CD007224.pub2. [DOI] [PubMed] [Google Scholar]
- 37.Bin Abd Razak HR, Yung WY. Postoperative Delirium in Patients Undergoing Total Joint Arthroplasty: A Systematic Review. The Journal of arthroplasty. 2015;30(8):1414–7. doi: 10.1016/j.arth.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 38.Hori D, Max L, Laflam A, Brown C, Neufeld KJ, Adachi H, et al. Blood Pressure Deviations From Optimal Mean Arterial Pressure During Cardiac Surgery Measured With a Novel Monitor of Cerebral Blood Flow and Risk for Perioperative Delirium: A Pilot Study. Journal of cardiothoracic and vascular anesthesia. 2016;30(3):606–12. doi: 10.1053/j.jvca.2016.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Critical care medicine. 2001;29(7):1370–9. doi: 10.1097/00003246-200107000-00012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.