Abstract
For older adults, managing medications can be a burden and could lead to medication non-adherence. To decrease risks associated with medication non-adherence, healthcare providers may recommend medication reminder apps as an assistive tool. However, these apps are often not designed with consideration of older adults’ needs, capabilities, and limitations. To identify whether available apps are suitable for older adults, we conducted an in-depth cognitive walkthrough and a heuristic evaluation of the most commonly downloaded medication reminder app. Findings revealed three main issues: 1) difficulty in navigation, 2) poor visibility, and 3) a lack of transparency. We also selected the top five downloaded medication reminder apps and categorized user reviews to assess app functionality and usability problems. The results of our analysis provide guidance for app design for older adult users to provide effective tools for managing medications and supporting patient/user health.
INTRODUCTION
The older adult population is growing in the United States and worldwide, which increases the need to develop solutions for the challenges this aging population faces (WHO 2016). Many older adults take three or more prescription medications (Wilson et al., 2007), which can be a challenge to manage. One result of this challenge is nonadherence to medications with 41% of older adults being non-adherent (Sirey et al. 2013). Non-adherence has associated risks such as increases in overall health costs and risk of hospitalization (Sokol et al. 2005).
Approximately 88 percent of older adults are living with one or more chronic conditions (Wilson et al., 2007). The most common treatment for chronic conditions involves taking regular oral medications (Wilson et al., 2007). Managing pill taking is a key component of health self-management and failing to adhere to the proper medication regimen can increase hospitalization and health costs or lead to negative drug effects from over or under dose (Gurwitz et al. 2003). One study found that 21 percent of negative drug effects in older adults occurred due to patient non-adherence (Gurwitz et al. 2003). These negative drug effects ranged from minor ailments, such as dizziness or skin rashes, to fatalities (Gurwitz et al. 2003). Medication nonadherence is the main reason older adults have to move into nursing homes (Marek & Antle, 2008).
Older adults are susceptible to medication non-adherence due to a variety of reasons. Firstly, some older adults have a limited ability to read and understand vital health information relating to their prescribed medications (MacLaughlin, Raehl, Treadway, Sterling, Zoller, & Bond, 2005). This, along with poor doctor/patient communication, has been shown to negatively impact medication adherence.
Secondly, memory is an important aspect of managing medications, thus reduced memory ability associated with aging may affect medication adherence (Mitzner et al., 2013). Medication management not only entails remembering when to take the medications, but also includes remembering the proper instructions for taking the medication. Research in this area has identified some key aspects of memory in relation to medication adherence. Insel, Morrow, Brewer, and Figeuredo (2006) found that executive function and working memory were related to better adherence. Likewise, Zogg, Woods, Sauceda, Wiebe, and Simoni (2012) found that a decline in prospective memory was associated with an increased risk in non-adherence.
Due to older adults’ vulnerability to medication non-adherence and the negative impacts of non-adherence, doctors or family members may recommend older adults use health management apps to support their medication adherence. Although such apps may be useful, they have not been designed specifically for older adults and thus may have usability issues specific to older adults. In a study that tested the usability of five medication management mobile apps, three of the creators of the medication management apps stated that they had never conducted usability testing with older adults (Grindrod, Li, & Gates, 2014). Accommodations should be made for individuals experiencing age-related changes in hearing, vision, cognition, and mobility (Hawthorn, 2002). App designers of health management apps should ensure good usability for older users by including large fonts, clear buttons, and high-contrast text. For first time users, it is recommended that the apps provide clear instructions and examples of how to use different features. Although some apps have such instructions and examples, often the font size is small, the contrast is low, and the examples are easily misinterpreted as pre-entered information (Grindrod et al., 2014).
In addition to usability issues within apps, the platform on which the app is used may have specific usability issues for older adults. For example, a study that investigated the usability of touchscreen mobile phones found that older adults had difficulty navigating through menus, understanding the scroll feature, and were confused by the QWERTY keyboard (Page, 2014). When older adults use medication management apps on touchscreen mobile devices, they are likely to experience these issues in addition to issues created by the apps.
The goal of the present study was to review the functionality and usability of several medicine management apps specifically for older adult users.
METHOD
In this study, we reviewed medication management phone apps. We conducted a cognitive walkthrough and heuristic evaluation of the most commonly downloaded medication management (Medisafe). In addition to this, we summarized usability issues that were identified by reviews for both the five most commonly used medication management apps currently available on the Android App Store. These evaluations were carried out by two evaluators.
Cognitive Walkthrough
The cognitive walkthrough was informed by Nielson’s principles (1994) and was conducted on the app using an iPhone 6. All the tasks were chosen with the idea in mind that they would be functions an older adult would be interested in using if they knew that the functionality existed. For more details about the persona and the tasks for the cognitive walkthrough, refer to Table 1.
Table 1.
Cognitive Walkthrough Details
| Persona | Task List |
|---|---|

|
|
Heuristic Evaluation
For the heuristic evaluation, we used both an iPhone and an Android phone to identify further potential usability issues. For the heuristic evaluation, we used Nielson’s usability heuristics (Nielson & Molich, 1990) and evaluated the apps’ various main screens for each of these 10 criteria.
App User Reviews
First, we selected the most popular medication reminder apps from the Android app store using the following criteria: more than 50,000 downloads and with a higher than 4.2 out of 5 overall review score. Then, for the top five most commonly used medication management apps we gathered information about the apps’ functionality from the app store and compiled information from users’ reviews we retrieved from the app store in February 2016. We conducted a high-level thematic analysis to identify common issues from the reviews that would be most related to older adult users.
The five apps (Dosecast, Med Helper, My PillBox, Pill Organizer, & PocketNurse) were all similar in functionality. The functionality included reminding users to take medications, allowing users to input medication dosage, track user’s medication adherence, allow for flexible pill scheduling, and allow for manual entry of vital signs.
RESULTS
Cognitive Walkthrough
The cognitive walkthrough identified several usability issues with Medisafe. Some of these related to layout of the app and the interface design, whereas others related to specific functions of the app, such as adding a dependent and the Medfriend option.
General issues identified were as follows. First, functionalities were confusing, not intuitive, or the available settings were not visible. These created difficulties in navigation of the app. Another reason navigation was difficult was that there was no set “Home” screen. This could create complications when the user is simply trying to access the general representation of the pill schedule. Even for an experienced smart phone user, many of the functions were difficult to find. In addition, many of the buttons were small and thus difficult to see, potentially making them difficult for an older adult with fine motor impairment and visual acuity limitations to select.
Usability issues directly related to the special functions of the app that allowed for adding a dependent and the option of having a “Medfriend.” Adding a dependent was an unclear option, and it was listed under the user’s profile, which was both difficult to find and non-intuitive. In addition, once a dependent was added, there was not any clear indication of whose profile and medications list were being shown (the primary user’s or the dependent’s). This could create issues if an older adult were unaware of whether they were looking at their own medications or their partner’s, possibly resulting in misuse of medications.
“Medfriend” was ill defined in the app; thus older adults may not understand why they might want to add a Medfriend. In addition, this function allowed users to share their information without realizing it and they have limited control over what information they share. There were two different options for sharing the information: email and text. If emailing the invitation code, the email provided information about sharing information, however, the text message option did not, which could result in older adults accidently sharing their private prescription information without realizing it. The access codes for adding the Medfriend were not unique enough so a user could access another user’s information by mistake (or could be easily hacked). This option, while potentially very useful, had many privacy and security issues.
Heuristic Evaluation
The heuristic evaluation of the app identified strengths and weaknesses of the design. Strengths were that the apps matched the normal interface settings of each type of phone (iPhone vs Android). The app also offered hints to help with the app usage, which could help with error prevention. Another strength was that the app offered tutorials and informative videos about the medications the user has added so that not only was the app helping keep track of the medication, but also assisting in the person’s knowledge of the medication itself. The app also offered many options for personal customization, from the primary functions (adjusting pill reminder times, pill images, etc.) to additive functions (adjusting the text for the reminder, customizable reminders, etc.).
The heuristic evaluation also identified several usability issues of the app. One of the main concerns was the poor contrast in the interface. Many of the text and button options were light grey on white background or dark grey on light grey background. In addition to poor contrast in certain parts of the app, the buttons for selection and navigation were very small and difficult to select. For examples, see Figure 1.
Figure 1.
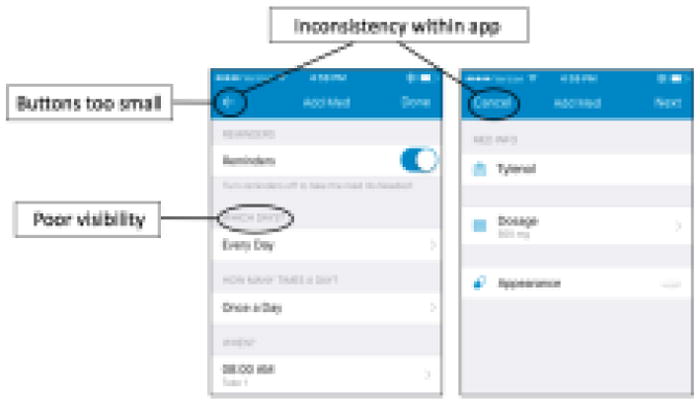
Consistency was another usability issue for the app. There were multiple options for selections and submission of selections. For example, for some entries the interface displayed a ‘Submit’ button, but for others the only option after entering information was to hit a back-arrow button to return to the previous screen.
Another consistency issue was between the app on the Android versus the iPhone. Both the app functionality and interface change depending on the platform being used. Android provided more information about Medfriend compared to the iPhone and also offered more control over medications shared. This issue was not directly pertinent to the older adult user, but could create issues for health care providers, family, or caregivers who wanted to help the older adult with use of the app or who were unaware that each platform functions slightly different.
App User Reviews
The app user reviews identified many usability issues with the medication reminder apps. The most commonly reported issues were related to inconsistent reminders, poor flexibility of setting reminders, difficulty navigating or using, desire for additional features, and easier input. For app specific usability issues, see Table 2.
Table 2.
App User Reviews
| Name of App | Major Usability Issues |
|---|---|
| Dosecast |
|
| Med Helper |
|
| My PillBox |
|
| Pill Organizer |
|
| PocketNurse |
|
DISCUSSION
Older adults face challenges related to properly managing multiple medications. Medication management apps are one way to mitigate these challenges. We evaluated current medication management apps for older adult use by conducting a cognitive walkthrough and heuristic evaluation of the top medication management app, and identifying major usability issues in the top five downloaded medication management apps.
Consistent with Grindrod’s (2014) usability study on medication management mobile apps with older adults, the top five commonly downloaded medication management apps had various usability issues and were not optimally designed for older users. Major issues identified by the cognitive walkthrough were unintuitive functionalities, problems with navigation, and small buttons. The heuristic evaluation identified issues, such as low color contrast and inconsistency within apps. Analyses of customer reviews from the app stores revealed additional usability concerns. One point frequently mentioned by customers was that reminders were not always reliable. Others expressed the desire for increased flexibility in setting reminders, functions that accommodated missed medications, and improved sharing and back-up features.
Findings from the current study have implications for the design of mobile apps that help people manage their medications. First, given the demographic trend of population aging and the need of older adults to take multiple medications, older adults should be engaged in the design and usability testing phases of the app development process. Designer should also use what is already known about aging and apply it to design. Moreover, there are age-specific design guidelines that can inform the development of apps that older adults are likely to use (e.g., Fisk et al., 2009; Pak & McLaughlin, 2010).
In sum, families and doctors should be careful when recommending health management apps, such as these medication management apps to older adults. Our assessments revealed that such apps do not accommodate will older adults’ capabilities and limitations. However, there is potential for these apps to benefit older adults. If the usability issues identified in our analysis are attended to, that potential is more likely to be realized.
Acknowledgments
This research was supported in part by a grant from the National Institutes of Health (National Institute on Aging) Grant P01 AG17211 under the auspices of the Center for Research and Education on Aging and Technology Enhancement (CREATE; www.create-center.org). We appreciate the insights of Kathie Insel on this project.
References
- Fisk AD, Rogers WA, Charness N, Czaja SJ, Sharit J. Designing for older adults: Principles and creative human factors approaches. 2. Boca Raton, FL: CRC Press; 2009. [Google Scholar]
- Grindrod KA, Li M, Gates A. Evaluating user perceptions of mobile medication management applications with older adults: a usability study. JMIR mHealth and uHealth. 2014;2(1):e11. doi: 10.2196/mhealth.3048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurwitz JH, Field TS, Harrold LR, Rothschild J, Debellis K, Seger AC, … Bates DW. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. Jama. 2003;289(9):1107–1116. doi: 10.1001/jama.289.9.1107. [DOI] [PubMed] [Google Scholar]
- Hawthorn D. How universal is good design for older users? ACM SIGCAPH Computers and the Physically Handicapped. 2002;(73–74):38–45. [Google Scholar]
- Insel K, Morrow D, Brewer B, Figueredo A. Executive function, working memory, and medication adherence among older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2006;61(2):P102–P107. doi: 10.1093/geronb/61.2.p102. [DOI] [PubMed] [Google Scholar]
- MacLaughlin EJ, Raehl CL, Treadway AK, Sterling TL, Zoller DP, Bond CA. Assessing medication adherence in the elderly. Drugs & aging. 2005;22(3):231–255. doi: 10.2165/00002512-200522030-00005. [DOI] [PubMed] [Google Scholar]
- Marek KD, Antle L. Medication management of the community-dwelling older adult. 2008 [PubMed] [Google Scholar]
- Mitzner TL, McBride SE, Barg-Walkow LH, Rogers WA. Self-management of wellness and illness in an aging population. In: Morrow DG, editor. Reviews of human factors and ergonomics. Vol. 8. Santa Monica: HFES; 2013. pp. 278–333. [Google Scholar]
- Nielsen J. Usability inspection methods. Conference companion on Human factors in computing systems; ACM; 1994. Apr, pp. 413–414. [Google Scholar]
- Nielsen J, Molich R. Heuristic evaluation of user interfaces. Proceedings of the SIGCHI conference on Human factors in computing systems; ACM; 1990. Mar, pp. 249–256. [Google Scholar]
- Page T. Touchscreen mobile devices and older adults: a usability study. International Journal of Human Factors and Ergonomics. 2014;3(1):65–85. [Google Scholar]
- Pak R, McLaughlin AC. Designing displays for older adults. Boca Raton, FL: CRC Press; 2010. [Google Scholar]
- Sirey JA, Greenfield A, Weinberger MI, Bruce ML. Medication beliefs and self-reported adherence among community-dwelling older adults. Clinical therapeutics. 2013;35(2):153–160. doi: 10.1016/j.clinthera.2013.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Medical care. 2005;43(6):521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- Wilson IB, Schoen C, Neuman P, Strollo MK, Rogers WH, Chang H, Safran DG. Physician–patient communication about prescription medication nonadherence: a 50-state study of America’s seniors. Journal of general internal medicine. 2007;22(1):6–12. doi: 10.1007/s11606-006-0093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zogg JB, Woods SP, Sauceda JA, Wiebe JS, Simoni JM. The role of prospective memory in medication adherence: a review of an emerging literature. Journal of behavioral medicine. 2012;35(1):47–62. doi: 10.1007/s10865-011-9341-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


