Abstract
Objectives
We investigated the prevalence of and sociodemographic associations with receiving prenatal and postpartum contraceptive counseling, including counseling on IUDs and implants.
Methods
We used data from a prospective cohort study of 803 postpartum women in El Paso and Austin, Texas. We examined prevalence of prenatal and postpartum counseling, provider discouragement of IUDs and implants, and associated sociodemographic characteristics using χ2 tests and logistic regression.
Results
Half of participants received any prenatal contraceptive counseling, and 13% and 37% received counseling on both IUDs and implants prenatally and postpartum, respectively. Women with more children were more likely to receive any contraceptive counseling prenatally (OR 1.99, p<0.01). Privately-insured women (OR 0.53, p<0.05) had lower odds of receiving prenatal counseling on IUDs and implants than publicly-insured women. Higher education (OR 2.16, p<0.05) and attending a private practice (OR 2.16, p<0.05) were associated with receiving any postpartum counseling. Older age (OR 0.61, p<0.05) was negatively associated with receiving postpartum counseling about IUDs and implants and a family income of $10,000–$19,000 (OR 2.21, p<0.01) was positively associated. Approximately 20% of women receiving prenatal counseling and 10% receiving postpartum counseling on IUDs and implants were discouraged from using them. The most common reason providers restricted use of these methods was inaccurate medical advice.
Conclusion
Prenatal and postpartum counseling, particularly about IUDs and implants was infrequent and varied by sociodemographics.
Practice implications
Providers should implement evidenced-based prenatal and postpartum contraceptive counseling to ensure women can make informed choices and access their preferred method of postpartum contraception.
Postpartum contraceptive use has the potential to reduce unintended pregnancy and short inter-pregnancy intervals, both of which may be associated with poorer health outcomes for women and infants (DeFranco, Ehrlich, & Muglia, 2014; Rodriguez, Chang, & Thiel de Bocanegra, 2015; White, Teal, & Potter, 2015). Despite these benefits, postpartum use of highly effective contraception (i.e. intrauterine devices (IUDs) and implants) remains low in the U.S. (White et al., 2015; Zapata et al., 2015). Barriers to postpartum contraceptive use include lack of access to postpartum care, loss of public insurance at 60 days postpartum, lack of availability of IUDs and implants at healthcare practices, lack of clinician knowledge and training, and a lack of contraceptive counseling; both prenatally and postpartum (Biggs, Arons, Turner, & Brindis, 2013; Potter et al., 2014; Zerden et al., 2015).
The American Academy of Pediatrics and The American College of Obstetricians and Gynecologists (2012) recommend contraceptive counseling on the full range of methods both prenatally and postpartum. Although receipt of prenatal and postpartum contraceptive counseling are independently associated with increased likelihood of postpartum contraceptive use (Hernandez, Sappenfield, Goodman, & Pooler, 2011; Wilson, Fowler, & Koo, 2013; Zapata et al., 2015), prevalence of postpartum contraceptive use is highest when women receive both prenatal and postpartum contraceptive counseling (Zapata et al., 2015). Prenatal counseling is particularly important because women who are not exclusively breastfeeding are at risk for unintended pregnancy as early as 27 days postpartum (Glasier, Logan, & McGlew, 1996; Speroff & Mishell Jr., 2008), and many low-income women lose their emergency (pregnancy) Medicaid at 60 days postpartum making the postpartum visit the last opportunity for contraception. Additionally, prenatal contraceptive counseling is crucial to ensuring women can make an informed choice if they desire contraception immediately after delivery or at the six week postpartum visit (ACOG, 2016a). And in-hospital counseling may not be an ideal time for contraceptive counseling because women are either in active labor or recovering from labor and caring for a newborn. Despite these benefits, prenatal contraceptive counseling occurs less frequently than postpartum contraceptive counseling. A retrospective multistate study found 78% of women received prenatal contraceptive counseling and 86% received postpartum contraceptive counseling (Zapata et al., 2015).
In an effort to improve access to postpartum contraception, a number of states have expanded Medicaid coverage to include reimbursement for immediate postpartum IUDs and implants (ACOG, 2016b) and Texas expanded this coverage beginning January 1, 2016. Improving access to immediate postpartum contraception is most useful if women have information to choose a method prior to delivery. The majority of studies examining prenatal and postpartum counseling have used Pregnancy Risk Assessment Monitoring System (PRAMS) data and were unable to examine whether women were counseled specifically on IUDs and implants or whether the provider discouraged them. Despite sociodemographic differences in postpartum contraceptive use, most studies do not examine sociodemographic differences in contraceptive counseling.
To address these gaps, we conducted a prospective cohort study of 803 women recruited postpartum from hospitals in Austin and El Paso, Texas to meet three objectives: (1) To assess prevalence of any contraceptive counseling during prenatal care as well as counseling on and provider discouragement of IUDs and implants, during prenatal care or prior to hospital discharge; (2) to assess prevalence of any contraceptive counseling as well as counseling on and provider discouragement of IUDs and implants, after delivery; and (3) to examine sociodemographic associations with receipt of any prenatal and postpartum contraceptive counseling and counseling on IUDs and implants. We focus on IUDs and implants because women frequently experience barriers accessing these methods due to cost (to patient and provider), provider misinformation related to medical eligibility, provider availability for immediate postpartum or same-day placement at a clinic (Biggs et al., 2013; Zerden et al., 2015), and because several studies have demonstrated an unmet demand for these methods postpartum (Potter et al., 2014; Tang et al., 2014).
Materials and methods
Sample
We recruited women on the postpartum unit of one hospital in Austin between April and July 2012, and two in El Paso between July and November 2012. We enrolled 400 women in each city: 300 women with public insurance and 100 women with private insurance at the time of delivery. None of the hospitals had protocols for contraceptive counseling or provided immediate postpartum IUDs and implants. Participants were between 18 and 44 years old, did not desire more children for at least 2 years, delivered a healthy singleton infant, spoke English or Spanish, and lived in the U.S. within 50 miles of the hospital. After the in-person baseline interview, follow-up interviews took place by telephone at 3, 6 and 9 months postpartum. Additional study procedures have been reported elsewhere (Potter et al., 2014). All 803 women were included in the baseline sample and 706 women (88%) completed the 6-month follow-up interview. We also excluded 96 women who were sterilized by 3 months postpartum for a final sample size of 613 at the 6-month follow-up.
Variables
We examined four main outcomes; two prenatal and two postpartum. The two prenatal outcomes—receipt of any prenatal contraceptive counseling and receipt of prenatal or hospital discharge counseling about IUDs and implant methods—were assessed at baseline. To assess receipt of any prenatal contraceptive counseling, women were asked, “During your pregnancy, did you talk to a doctor, nurse or other health care provider about using birth control methods?” To assess counseling on IUDs and implants, women were asked two separate sets of questions. First, women were asked, “What method would you prefer to be using by six months postpartum?” Those who selected IUD or implant as their preferred method were asked whether their provider discouraged or encouraged its use, neither discouraged nor encouraged it or didn’t discuss it. Second, women who did not chose an IUD or implant as their preferred method were asked, “At any point during your pregnancy or since delivery, did you and your {doctor/nurse} discuss any of the following birth control methods?” Women who reported talking with their provider about both IUDs and implants were considered to have received counseling on IUDs and implants.
The two postpartum outcomes—receipt of any postpartum contraceptive counseling since delivery and receipt of postpartum counseling about IUDs and implants—were assessed at the 6-month follow-up survey. Receipt of any postpartum contraceptive counseling since leaving the hospital was assessed through two questions: (1) women who had a postpartum check-up were asked, “At your postpartum check-up, did you talk to your provider about options for birth control?”, and (2) women who responded no or who did not have a postpartum check-up were asked, “Have you talked to a health-care provider about birth control at any time since you had your new baby?” Women who responded yes to either question were considered to have received postpartum contraceptive counseling. Receipt of postpartum counseling about IUDs and implants was also assessed using two questions. First, women who were using an implant or IUD at the 6-month follow-up were asked if they had discussed the method with a provider. Second, women who were not using an IUD or implant at the 6-month interview were asked whether their provider discouraged or encouraged its use, neither discouraged nor encouraged it, or didn’t discuss it. Women who had discussed both implants and IUDs with a provider were considered to have received postpartum counseling on IUDs and implants. Finally, all women who were not using and did not prefer an IUD or implant were asked if their provider gave reasons for “restricting” the implant or IUD and if those reasons included age, sexually transmitted infections, method cost and availability, other medical reasons, or other reasons. Among women who reported their provider gave a reason for “restricting” the method, we calculated the frequency of each reason and categorized open-ended “other” reasons into inaccurate medical advice, cost, availability, and other medical reasons.
For our analysis, we chose sociodemographic covariates from the range of survey topics that were associated with contraceptive preferences and use in prior literature (Potter et al., 2014, 2016). These included city (Austin or El Paso), age (18–24 years, 25–29 years, 30+ years), number of living biological children (1, 2, 3 or more), relationship status (single, cohabitating, married), ethnicity (Hispanic and non-Hispanic), nativity (U.S. or foreign-born), language of interview (English or Spanish), education (less than high school, high school, more than high school), insurance status (public or private) and annual family income (<$10,000, $10,000–19,999, $20,000–34,999, $35,000–74,999, $75,000 and above). Insurance status was asked again at the 6-month follow-up (lost or maintained insurance) along with the woman’s usual source of health care (none, private practice, clinic, hospital based, or receiving care in Mexico). We categorized future childbearing intentions at baseline and 6 months dichotomously (want no more children versus want or may want more children).
Analysis
We compared sociodemographic characteristics among each of the four outcomes: received any prenatal contraceptive counseling; received prenatal or hospital discharge IUD and implant counseling; received any postpartum contraceptive counseling; and received postpartum IUD and implant counseling. We used χ2 tests to test for significant differences between groups.
We used logistic regression to examine sociodemographic associations with each of the four outcomes. We tested each sociodemographic variable, including receipt of prenatal contraceptive counseling in the models predicting postpartum counseling, using likelihood ratio tests to identify the most parsimonious models. Final models include covariates that improved model fit based on a likelihood ratio test with a significance level of <0.05. Models 1 and 2 examine factors associated with receipt of prenatal counseling; Model 1 includes insurance type, number of living biological children, and pregnancy intentions and Model 2 includes insurance type. Models 3 and 4 examine factors associated with receipt of postpartum counseling; Model 3 includes usual source of health care, education, and received prenatal counseling and Model 4 includes age, city, usual source of health care, family income, and received prenatal IUD and implant counseling. Finally, we examined prevalence of provider discouragement and encouragement of IUDs and implants and reasons providers restricted use of these methods.
We used list-wise deletion, removing observations with missing data from models. None of the variables were missing observations for more than 2.5% of participants. Analyses were performed using Stata version 14.0. The University of Texas at Austin and all participating hospital institutional review boards approved the study.
Results
Approximately half of the women in our sample received any prenatal contraceptive counseling, but only 13% received counseling on IUDs and implants during prenatal care or prior to hospital discharge (Table 1). Examining bivariate sociodemographic associations, public insurance and not desiring more children were each associated with receipt of any prenatal contraceptive counseling and with receipt of prenatal counseling on IUDs and implants. Higher parity was associated with receipt of any prenatal contraceptive counseling alone and less education was associated with receipt of prenatal IUD and implant counseling.
Table 1.
Receipt of prenatal contraceptive counseling and receipt of prenatal counseling on IUDs and implants, by sociodemographics (N=803)
| N | Proportion receiving prenatal contraceptive counseling | χ2 p-value | Proportion receiving prenatal IUD and implant counseling | χ2 p-value | |
|---|---|---|---|---|---|
|
|
|||||
| City | |||||
| Austin | 403 | 0.50 | 0.12 | ||
| El Paso | 400 | 0.50 | 0.972 | 0.13 | 0.789 |
| Age | |||||
| 18–24 | 267 | 0.49 | 0.16 | ||
| 25–29 | 229 | 0.52 | 0.11 | ||
| 30+ | 307 | 0.49 | 0.806 | 0.11 | 0.198 |
| Health insurance | |||||
| Private insurance | 201 | 0.41 | 0.08 | ||
| Public insurance | 602 | 0.53 | 0.004 | 0.14 | 0.024 |
| Ethnicity | |||||
| Hispanic | 615 | 0.51 | 0.13 | ||
| Non-Hispanic | 188 | 0.47 | 0.411 | 0.12 | 0.649 |
| Nativity | |||||
| U.S.-born | 404 | 0.47 | 0.11 | ||
| Foreign-born | 399 | 0.53 | 0.143 | 0.14 | 0.173 |
| Language of interview | |||||
| English | 420 | 0.47 | 0.11 | ||
| Spanish | 383 | 0.53 | 0.093 | 0.14 | 0.249 |
| Education | |||||
| <HSD | 262 | 0.52 | 0.16 | ||
| HSD | 212 | 0.55 | 0.13 | ||
| >HSD | 328 | 0.45 | 0.052 | 0.09 | 0.042 |
| Income | |||||
| $10,000 | 264 | 0.51 | 0.16 | ||
| $10,000–$19,999 | 197 | 0.56 | 0.13 | ||
| $20,000–$34,999 | 122 | 0.54 | 0.11 | ||
| $35,000–$74,999 | 112 | 0.46 | 0.14 | ||
| $75,000 or more | 94 | 0.39 | 0.054 | 0.04 | 0.055 |
| Marital status | |||||
| Single | 165 | 0.48 | 0.13 | ||
| Cohabitating | 244 | 0.50 | 0.14 | ||
| Married | 391 | 0.50 | 0.884 | 0.11 | 0.574 |
| Living biological children | |||||
| 1 child | 249 | 0.39 | 0.13 | ||
| 2 children | 248 | 0.47 | 0.11 | ||
| 3+ children | 306 | 0.62 | 0.000 | 0.14 | 0.452 |
| Future childbearing | |||||
| Does not want more children | 376 | 0.58 | 0.15 | ||
| Wants or may want more children | 427 | 0.43 | 0.000 | 0.10 | 0.030 |
The majority (83%) of women received any postpartum contraceptive counseling and approximately one-third received postpartum counseling on IUDs and implants. Retaining insurance, having a regular source of healthcare (particularly at a private practice or clinic), self-identifying as non-Hispanic, being U.S.-born, speaking English, having more education, having higher income, and receiving prenatal contraceptive counseling were each associated with receipt of any postpartum contraceptive counseling (Table 2). In contrast, associations were reversed for receipt of postpartum counseling on IUDs and implants. Women with a usual source of care at a clinic, hospital system or in Mexico, Hispanic women, Spanish-speaking women, foreign-born women, or lower income women were each more likely to have received counseling on IUDs and implants postpartum. Additionally, women in El Paso and younger women were more likely to have received counseling on IUDs and implants than women in Austin and older women.
Table 2.
Receipt of contraceptive counseling by 6 months postpartum and receipt of IUD and implant counseling by 6 months postpartum, by sociodemographics among women who were not sterilized by 3 months postpartum (N=613)
| N | Proportion receiving postpartum contraceptive counseling | χ2 p-value | Proportion receiving postpartum IUDs and implant counseling | χ2 p-value | |
|---|---|---|---|---|---|
|
|
|||||
| City | |||||
| Austin | 321 | 0.85 | 0.31 | ||
| El Paso | 292 | 0.81 | 0.124 | 0.42 | 0.003 |
| Age | |||||
| 18–24 | 225 | 0.81 | 0.43 | ||
| 25–29 | 179 | 0.84 | 0.34 | ||
| 30+ | 209 | 0.84 | 0.635 | 0.30 | 0.012 |
| Health insurance | |||||
| Lost insurance | 322 | 0.78 | 0.39 | ||
| Retained insurance | 291 | 0.89 | 0.000 | 0.33 | 0.119 |
| Usual source of care at 6 months | |||||
| None | 55 | 0.59 | 0.19 | ||
| Clinic | 240 | 0.81 | 0.40 | ||
| Private practice | 235 | 0.93 | 0.32 | ||
| Hospital system | 28 | 0.75 | 0.46 | ||
| Mexico | 55 | 0.78 | 0.000 | 0.49 | 0.003 |
| Ethnicity | |||||
| Hispanic | 455 | 0.81 | 0.40 | ||
| Non-Hispanic | 158 | 0.91 | 0.004 | 0.25 | 0.001 |
| Nativity | |||||
| U.S.-born | 313 | 0.88 | 0.31 | ||
| Foreign-born | 300 | 0.78 | 0.001 | 0.41 | 0.008 |
| Language of interview | |||||
| English | 343 | 0.89 | 0.32 | ||
| Spanish | 270 | 0.76 | 0.000 | 0.42 | 0.011 |
| Education | |||||
| <HSD | 183 | 0.76 | 0.40 | ||
| HSD | 166 | 0.78 | 0.34 | ||
| >HSD | 263 | 0.91 | 0.000 | 0.34 | 0.378 |
| Income | |||||
| $10,000 | 203 | 0.75 | 0.38 | ||
| $10,000–$19,999 | 142 | 0.88 | 0.52 | ||
| $20,000–$34,999 | 89 | 0.83 | 0.33 | ||
| $35,000–$74,999 | 92 | 0.89 | 0.27 | ||
| $75,000 or more | 77 | 0.92 | 0.001 | 0.18 | 0.000 |
| Marital status | |||||
| Single | 123 | 0.76 | 0.36 | ||
| Cohabitating | 183 | 0.85 | 0.41 | ||
| Married | 304 | 0.85 | 0.077 | 0.33 | 0.190 |
| Living biological children | |||||
| 1 child | 215 | 0.85 | 0.36 | ||
| 2 children | 202 | 0.86 | 0.38 | ||
| 3+ children | 196 | 0.78 | 0.097 | 0.35 | 0.813 |
| Future childbearing: | |||||
| Does not want more children | 215 | 0.82 | 0.33 | ||
| Wants or may want more children | 398 | 0.84 | 0.508 | 0.38 | 0.205 |
| Prenatal contraceptive counseling | |||||
| Received prenatal contraceptive counseling | 281 | 0.87 | 0.42 | ||
| Did not receive prenatal contraceptive counseling | 321 | 0.79 | 0.015 | 0.29 | 0.002 |
| Postpartum check | |||||
| Did not receive a postpartum check | 73 | 0.18 | 0.06 | ||
| Received a postpartum check | 540 | 0.92 | 0.000 | 0.40 | 0.000 |
Multivariate models show that women with three or more children (OR 1.99, p<0.01) had greater odds of receiving contraceptive counseling than women with one child, after controlling for insurance type and childbearing intentions (Table 3, Model 1). Model 2 shows that women with private insurance (OR 0.53, p<0.05) had lower odds of receiving prenatal counseling on IUDs and implants than women with public insurance.
Table 3.
Odds ratios (95% confidence intervals) for receipt of prenatal contraceptive counseling and receipt of prenatal IUD and implant counseling
| Model 1 | Model 2 | |
|---|---|---|
| Prenatal contraceptive counseling (N=785) | Prenatal IUD and implant counseling (N=798) | |
|
|
||
| Insurance type | ||
| Public | Ref. | Ref. |
| Private | 0.73† (0.52 – 1.02) | 0.53* (0.30 – 0.93) |
| Living biological children | ||
| 1 child | Ref. | |
| 2 children | 1.28 (0.88 – 1.86) | |
| 3+ children | 1.99** (1.32 – 3.02) | |
| Childbearing intentions | ||
| Wants or may want more children | Ref. | |
| Doesn’t want more children | 1.36† (0.97 – 1.91) | |
| Constant | 0.67** (0.50 – 0.88) | 0.16*** (0.13 – 0.21) |
p<0.001,
p<0.01,
p<0.05,
p<0.10
Compared with women who received their usual source of healthcare at a clinic, women at private practices had higher odds of receiving any postpartum contraceptive counseling (OR 2.16, p<0.05, Table 4, Model 3) and women with no usual source of care had lower odds of receiving postpartum contraceptive counseling (OR 0.36, p<0.01). Women with more education than a high school diploma had higher odds of receiving any postpartum contraceptive counseling than women with less than a high school education (OR 2.16, p<0.05). Older age (OR 0.61, p<0.05) and having no usual source of health care (OR 0.31, p<0.01) were associated with lower odds of receiving postpartum counseling on IUDs and implants. Living in El Paso rather than Austin (OR 1.54, p<0.05) and having a family income of $10,000–$19,000 (OR 2.21, p<0.01), were associated with higher odds of receiving postpartum counseling on IUDs and implants (Model 4).
Table 4.
Odds ratios (95% confidence intervals) for receipt of contraceptive counseling by 6 months postpartum and receipt of IUD and implant counseling by 6 months postpartum among non-sterilized women
| Model | 3 Model 4 | |
|---|---|---|
|
| ||
| Postpartum contraceptive counseling (N=599) | Postpartum IUD and implant counseling (N=596) | |
|
| ||
| Age | ||
| 18–24 | Ref. | |
| 25–29 | 0.67† (0.42 – 1.06) | |
| 30+ | 0.61* (0.37 – 0.99) | |
| City | ||
| Austin | Ref. | |
| El Paso | 1.54* (1.03 – 2.32) | |
| Nativity | ||
| Foreign-born | Ref. | |
| U.S.-born | 0.67† (0.43 – 1.04) | |
| Usual source of healthcare | ||
| Clinic | Ref. | Ref. |
| None | 0.36** (0.19 – 0.68) | 0.31** (0.15 – 0.68) |
| Private practice | 2.16* (1.13 – 4.15) | 1.23 (0.75 – 2.03) |
| Hospital system | 0.58 (0.23 – 1.50) | 1.03 (0.43 – 2.44) |
| Mexico | 0.71 (0.34 – 1.50) | 0.86 (0.44 – 1.68) |
| Education | ||
| <HS edu | Ref. | |
| HS | 0.89 (0.52 – 1.51) | |
| >HSD | 2.16* (1.17 – 4.00) | |
| Income | ||
| $10000 | Ref. | |
| $10,000–$19,999 | 2.21** (1.37 – 3.57) | |
| $20,000–$34,999 | 0.95 (0.53 – 1.68) | |
| $35,000–$74,999 | 0.70 (0.36 – 1.33) | |
| $75,000 or more | 0.55 (0.24 – 1.25) | |
| Had prenatal counseling | 1.86** (1.17 – 2.94) | |
| Had prenatal IUD and implant counseling | 3.18*** (1.86 – 5.44) | |
| Constant | 2.89*** (1.84 – 4.54) | 0.40* (0.18 – 0.86) |
p<0.001,
p<0.01,
p<0.05,
p<0.10
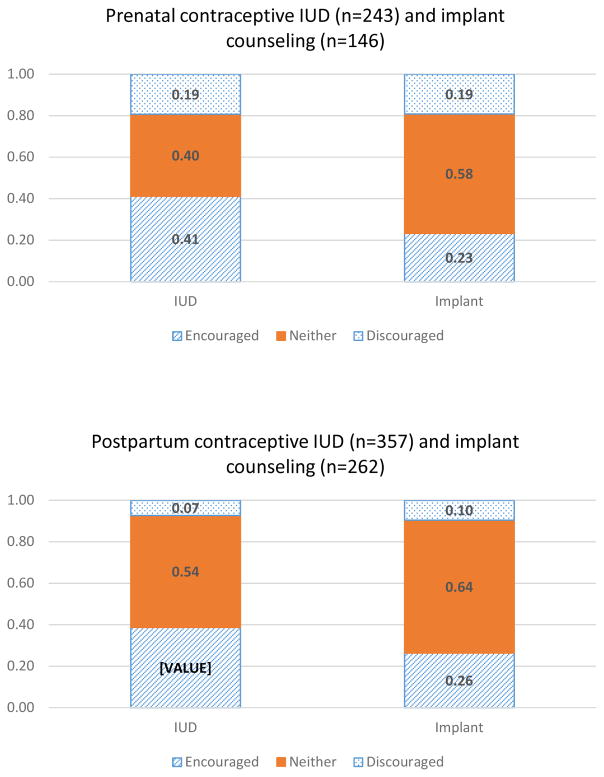
Figure 1 shows that more women received prenatal and postpartum counseling on IUDs than implants (243 vs. 146 and 357 vs. 262, respectively). The top panel shows that a larger proportion of women were encouraged to use the IUD than the implant and that almost 20% of women counseled on either the IUD or implant were discouraged from using it. The bottom panel reflects higher numbers of women receiving postpartum versus prenatal counseling on IUDs and implants (357 vs. 243 and 262 vs. 146, respectively). Similar to prenatal counseling, a larger proportion of women were encouraged to use the IUD rather than the implant, although the proportion of women who were discouraged from using either method during postpartum counseling was lower than for prenatal counseling.
Figure 1.
Provider’s encouragement of IUDs and implants. The figure presents the number of women whose clinician encouraged (blue striped), discouraged (blue dots), or neither encouraged nor discouraged (solid orange) IUDs and implants among women who received counseling on IUDs and implants.
Among reported reasons providers restricted IUDs or implants, almost half were due to inaccurate medical advice; only one of the known medical reasons (uterus too small) were evidenced-based (Table 5).
Table 5.
Provider reasons for restricting use of the IUD or implant during postpartum counseling among women who were not using and did not prefer the method*
| IUD (N=24) | Implant (N=29) | |||
|---|---|---|---|---|
|
| ||||
| n | % | n | % | |
|
| ||||
| Inaccurate medical advice or provider personal opinion (e.g. cannot be used among breastfeeding women, those with a c-section, history of blood clots, or thyroid disease; not an effective method; too young) | 11 | 45.8 | 15 | 48.4 |
| Other unspecified medical reasons or side effects (includes one known health barrier: uterus too small) | 8 | 33.3 | 9 | 29.0 |
| Cost to patient or provider (e.g. not cost effective if wants “to have a kid in five years”) | 4 | 16.7 | 5 | 16.1 |
| Method not available at clinic | 1 | 4.1 | 2 | 6.5 |
Multiple responses valid
Discussion
Our results suggest that despite evidenced-based recommendations and well-documented benefits (AAP & ACOG, 2012; Zapata et al., 2015), the majority of women in El Paso and Austin are not receiving prenatal contraceptive counseling. Only half of study participants received any prenatal contraceptive counseling, substantially lower than 78.2% of women who reported prenatal counseling in a multistate study based on PRAMS data (Zapata et al., 2015). Moreover, our study is one of the first to show prenatal and postpartum counseling did not often involve discussion of the full range of contraceptive methods with their providers: only 13% and 37% of women received prenatal and postpartum counseling on IUDs and implants, respectively, and almost 20% of women who received prenatal counseling on IUDs and implants were discouraged from using them. This infrequent and insufficient counseling may place women at higher risk for contraceptive non-use, unintended pregnancy, and short inter-pregnancy intervals (Hernandez et al., 2011; Wilson et al., 2013; Zapata et al., 2015). Finally, we found that prevalence of contraceptive counseling varied by sociodemographic characteristics. Contraceptive counseling on IUDs and implants was less common among women of higher socioeconomic status (SES), women with less children, women who want more children, and older women.
There are several possible reasons for low rates of prenatal contraceptive counseling observed in our sample. Clinicians may not provide prenatal contraceptive counseling due to a number of health system and provider level barriers, including time and staffing constraints as health care systems face more economic pressure. Another possible explanation is that women did not report or recall the counseling they received. Women are given a large amount of health information during prenatal care and they may have been too preoccupied recovering from delivery to recall details of their prenatal care when asked after delivery. On the other hand, if a woman has forgotten having received counseling, this may be an indication that it was not effective, comprehensive, or patient-centered.
A number of barriers at health-system and provider levels may explain the low prevalence of counseling on IUDs and implants we observed. Clinic staff may not have sufficient knowledge and training on eligibility and safety of postpartum contraception, particularly on IUDs and implants (Zerden et al., 2015). Clinic protocols may not include contraceptive counseling as a standard part of prenatal care or clinicians may assume women are not interested in postpartum IUDs and implants (Tocce, Goldthwaite, Sheeder, Eichengreen, & Teal, 2015). However, multiple studies have documented significant interest and a substantial unmet demand for postpartum IUDs and implants (Ogburn, Espey, & Stonehocker, 2005; Potter et al., 2014; Tang et al., 2014; Tocce, Sheeder, & Teal, 2012).
Finally, inaccessibility of IUDs and implants may be a reason for infrequent prenatal and postpartum IUD and implant counseling and explain why we observed a lower proportion of women receiving prenatal contraceptive counseling on any method than reported in other studies (Hernandez et al., 2011; Zapata et al., 2015). Clinicians may not counsel on methods that the hospital or clinic does not have available or that insurance will not cover. Medicaid reimbursement for immediate postpartum IUDs and implants had not been implemented in Texas at the time of the study, nor were any of the study hospitals providing it. Indeed, our study was conducted in the wake of budget cuts in Texas. In 2011, a year prior to study recruitment, the Texas legislature cut the state family planning budget by two-thirds, particularly reducing availability of those methods with the highest upfront costs, such as IUDs and implants (White, Hopkins, et al., 2015; White, Grossman, Hopkins, & Potter, 2012).
There are two possible explanations for our finding that the frequency of IUD and implant counseling was higher among lower SES women, considering socioeconomic disparities in unintended pregnancies (Finer & Zolna, 2014), short inter-pregnancy intervals (DeFranco et al., 2014; White, Teal, et al., 2015), and contraceptive use (Kavanaugh, Jerman, & Finer, 2015). One is that even with good intentions, clinicians are often influenced by conscious or unconscious biases and may target lower SES women assuming they need more education and encouragement to use contraception (Dehlendorf et al., 2010; Gilliam, 2015). On the other hand, lower SES women may be more motivated to avoid a closely spaced pregnancy and thus more likely to request a discussion with their providers about contraception than higher SES women. Indeed, a prior study employing data from the same cohort as the current study, found that lower SES women were more likely to prefer IUDs and implants than higher SES women, but less likely to actually be using these methods (Potter et al., 2014).
Finally, public clinics, particularly Title X family planning clinics may have greater provider knowledge about contraceptive eligibility and be more likely to provide IUDs and implants on-site, including same-day placement than private practices (Thiel de Bocanegra, Chang, Howell, & Darney, 2014; Thiel de Bocanegra, Cross Riedel, Menz, Darney, & Brindis, 2014). Our results showed that although women who received their usual care at a private practice were more likely to receive any postpartum contraceptive counseling, only 30% of women who received their usual care at a private practice received postpartum counseling on IUDs and implants, compared to 40% or more of women who received their usual care at a clinic, hospital based practice, or in Mexico. Further, women with public insurance were more likely to receive any prenatal contraceptive counseling and prenatal counseling on IUDs and implants than women with private insurance. Medicaid may reimburse for more comprehensive prenatal services that include contraceptive counseling, such as Nurse Family Partnership (“Nurse Family Partnership,” 2011), and publicly insured women receiving these services may have initiated contraceptive discussions with their prenatal providers.
In addition to SES, we also found differences in contraceptive counseling related to age and parity. Women with more children or younger women may also be targeted by clinicians to receive contraceptive counseling, but it is equally possible that these women are more likely to request contraceptive information to avoid an unintended pregnancy (Tang, Dominik, Re, Brody, & Stuart, 2013).
The lower prevalence of prenatal and postpartum counseling on the implant as compared to the IUD may reflect its shorter history in the U.S., its greater expense, or theoretical concerns of its effect on breastfeeding. Almost 20% of women who received IUD or implant counseling during prenatal care were discouraged from using them. Of the women who reported their provider gave a reason restricting use of the IUD or implant during postpartum counseling, only one of the medical restrictions was evidenced-based (Curtis et al., 2016). Similarly, Ogburn and colleagues (2005) found provider discouragement was a barrier to receiving an IUD immediately postpartum and none of the providers’ reasons were evidenced-based. Providers may also discourage IUDs and implants because their practice does not provide them, also a reported reason for provider restriction. Although we acknowledge concern regarding provider coercion or bias toward IUDs and implants (Gilliam, 2015; Gomez, Fuentes, & Allina, 2014), we do not have data to further speculate on whether providers who encouraged IUDs or implants encouraged them over or in addition to other methods. It is evident, however, that contraceptive counseling in this setting fails to reach all women and does not regularly include information on all contraceptive options, effectiveness, side effects, and benefits (Dehlendorf, Krajewski, & Borrero, 2014).
Our study is one of the first to document prevalence of prenatal and postpartum counseling on IUDs and implants and examine sociodemographic associations with contraceptive counseling. However, contraceptive counseling was measured by self-report and it is possible that women were counseled but did not report or remember it. Although we identified two methods about which women received counseling, we were unable to fully assess all dimensions of counseling, including quality measures (e.g. satisfaction with provider involvement). Our sample consists of women from hospitals in Austin and El Paso and may not be generalizable to the entire state. We did not assess reasons providers restricted use of IUDs or implants during prenatal counseling and only women who did not prefer the method postpartum were asked about provider reasons for restricting method use. Finally, survey questions did not differentiate if IUD and implant counseling occurred at prenatal visits or in the hospital prior to discharge and postpartum counseling may have occurred anytime during the postpartum period. Consequently, our results may underestimate the proportion of women receiving counseling on IUDs and implants at prenatal and 6-week postpartum visits because we included counseling received at any time during the prenatal and postpartum period.
Implications for practice and policy
Our results indicate the majority of women in El Paso and Austin are not receiving evidenced-based prenatal and postpartum contraceptive counseling on the full range of methods. Medicaid reimbursement of immediate postpartum IUDs and implants is an important opportunity that may go unrealized if women do not receive contraceptive counseling prior to delivery. Indeed, removing cost barriers along with providing comprehensive contraceptive counseling may increase preference for and use of IUDs and implants (Secura, Allsworth, Madden, Mullersman, & Peipert, 2010; Tocce et al., 2012).
There are several ways clinics can improve frequency and quality of contraceptive counseling. Clinics and hospitals can provide evidenced-based training on IUDs and implants, including eligibility and safety of postpartum insertion and breastfeeding to reduce inaccurate provider counseling (Curtis et al., 2016). They can also implement quality contraceptive counseling as described by the CDC (Gavin et al., 2014), including shared decision-making, an “interactive” approach when providers actively engage with the patient while respecting her preferences and autonomy (Dehlendorf et al., 2014; Stiggelbout et al., 2012). Research has also shown that shared decision-making and use of a check-list to ensure all methods are discussed may increase use of effective methods, and increase visit and method satisfaction (Harper et al., 2015; Madden, Mullersman, Omvig, Secura, & Peipert, 2013; Tang et al., 2014). Finally, contraceptive counseling may not improve until all women, regardless of race/ethnicity, insurance, or immigration status, can access the full range of contraceptive methods any time after delivery, at any healthcare practice or hospital. Contraceptive counseling and access are both crucial to reducing unintended pregnancies and short inter-pregnancy intervals.
Acknowledgments
We thank Chloe Dillaway and Natasha Mevs-Korff for excellent research assistance.
Funding support
This project was supported by grants from the Susan T. Buffett Foundation and the Society of Family Planning (SFPRF7-4). Infrastructural support was provided by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R24 042849) to the Population Research Center, University of Texas at Austin.
Biographies
Kate Coleman-Minahan, PhD, RN, FNP-BC, is an Assistant Professor in the College of Nursing at the University of Colorado Denver and an Affiliate of the Population Research Center at the University of Texas at Austin. Her work focuses on reproductive health decision-making and access to contraception and abortion among marginalized populations, specifically adolescents and Latina immigrants.
Abigail R.A. Aiken MD, MPH, PhD, is an Assistant Professor at the LBJ School of Public Affairs and a Faculty Associate at the Population Research Center at the University of Texas at Austin. Her research interests span several disciplines and include abortion outside the formal healthcare setting, unintended pregnancy, and contraceptive desires and access.
Joseph E. Potter, PhD, is a Professor of Sociology and a Faculty Associate at The University of Texas at Austin Population Research Center. His work focuses on issues related to population and reproductive health in the United States and Latin America, including the impact of changes in family planning funding on births, abortions, and contraceptive use.
Footnotes
Conflicts of interest: none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- ACOG. Immediate postpartum long-acting reversible contraception. Washington, D.C: American College of Obstetricians and Gynecologists; 2016a. (Committee Opinion) Retrieved from https://www.acog.org/-/media/Committee-Opinions/Committee-on-Obstetric-Practice/co670.pdf?dmc=1&ts=20170107T1316288402. [Google Scholar]
- ACOG. Immediate Postpartum LARC Medicaid Reimbursement. 2016b Dec 14; Retrieved January 7, 2017, from http://www.acog.org/About-ACOG/ACOG-Departments/Long-Acting-Reversible-Contraception/Immediate-Postpartum-LARC-Medicaid-Reimbursement.
- American Academy of Pediatrics, & American College of Obstetricians and Gynecologists, editor. Guidelines for perinatal care. 7. Elk Grove Village, IL: Washington, DC: American Academy of Pediatrics; American College of Obstetricians and Gynecologists; 2012. [Google Scholar]
- Biggs MA, Arons A, Turner R, Brindis CD. Same-day LARC insertion attitudes and practices. Contraception. 2013;88(5):629–635. doi: 10.1016/j.contraception.2013.05.012. https://doi.org/10.1016/j.contraception.2013.05.012. [DOI] [PubMed] [Google Scholar]
- Curtis KM, Tepper NK, Jatlaoui TC, Berry-Bibee E, Horton LG, Zapata LB, … Whiteman MK. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. Morbidity and Mortality Weekly Report. 2016;65(3):1–103. doi: 10.15585/mmwr.rr6503a1. https://doi.org/10.15585/mmwr.rr6503a1. [DOI] [PubMed] [Google Scholar]
- DeFranco E, Ehrlich S, Muglia L. Influence of interpregnancy interval on birth timing. BJOG: An International Journal of Obstetrics & Gynaecology. 2014;121(13):1633–1640. doi: 10.1111/1471-0528.12891. https://doi.org/10.1111/1471-0528.12891. [DOI] [PubMed] [Google Scholar]
- Dehlendorf C, Krajewski C, Borrero S. Contraceptive Counseling: Best Practices to Ensure Quality Communication and Enable Effective Contraceptive Use. Clinical Obstetrics and Gynecology. 2014;57(4):659–673. doi: 10.1097/GRF.0000000000000059. https://doi.org/10.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehlendorf C, Ruskin R, Grumbach K, Vittinghoff E, Bibbins-Domingo K, Schillinger D, Steinauer J. Recommendations for intrauterine contraception: a randomized trial of the effects of patients’ race/ethnicity and socioeconomic status. American Journal of Obstetrics and Gynecology. 2010;203(4):319.e1–319.e8. doi: 10.1016/j.ajog.2010.05.009. https://doi.org/10.1016/j.ajog.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finer LB, Zolna MR. Shifts in Intended and Unintended Pregnancies in the United States, 2001–2008. American Journal of Public Health. 2014;104(S1):S43–S48. doi: 10.2105/AJPH.2013.301416. https://doi.org/10.2105/AJPH.2013.301416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavin L, Moskosky S, Carter M, Curtis K, Glass E, Godfrey E, … Zapata L. Providing quality family planning services: Recommendations of CDC and the U.S. Office of Population Affairs. Morbity and Mortality Weekly Report. 2014;63(RR04):1–29. [PubMed] [Google Scholar]
- Gilliam ML. Beyond Coercion: Let Us Grapple With Bias. Obstetrics & Gynecology. 2015 doi: 10.1097/AOG.0000000000001116. [DOI] [PubMed] [Google Scholar]
- Glasier AF, Logan J, McGlew TJ. Who gives advice about postpartum contraception? Contraception. 1996;53(4):217–220. doi: 10.1016/0010-7824(96)00040-6. https://doi.org/10.1016/0010-7824(96)00040-6. [DOI] [PubMed] [Google Scholar]
- Gomez AM, Fuentes L, Allina A. Women or LARC First? Reproductive Autonomy And the Promotion of Long-Acting Reversible Contraceptive Methods. Perspectives on Sexual and Reproductive Health. 2014;46(3):171–175. doi: 10.1363/46e1614. https://doi.org/10.1363/46e1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper CC, Rocca CH, Thompson KM, Morfesis J, Goodman S, Darney PD, … Speidel JJ. Reductions in pregnancy rates in the USA with long-acting reversible contraception: a cluster randomised trial. The Lancet. 2015;386(9993):562–568. doi: 10.1016/S0140-6736(14)62460-0. [DOI] [PubMed] [Google Scholar]
- Hernandez LE, Sappenfield WM, Goodman D, Pooler J. Is Effective Contraceptive Use Conceived Prenatally in Florida? The Association Between Prenatal Contraceptive Counseling and Postpartum Contraceptive Use. Maternal and Child Health Journal. 2011;16(2):423–429. doi: 10.1007/s10995-010-0738-9. https://doi.org/10.1007/s10995-010-0738-9. [DOI] [PubMed] [Google Scholar]
- Kavanaugh ML, Jerman J, Finer LB. Changes in Use of Long-Acting Reversible Contraceptive Methods Among U.S. Women, 2009–2012. Obstetrics & Gynecology. 2015:1. doi: 10.1097/AOG.0000000000001094. https://doi.org/10.1097/AOG.0000000000001094. [DOI] [PMC free article] [PubMed]
- Madden T, Mullersman JL, Omvig KJ, Secura GM, Peipert JF. Structured contraceptive counseling provided by the Contraceptive CHOICE Project. Contraception. 2013;88(2):243–249. doi: 10.1016/j.contraception.2012.07.015. https://doi.org/10.1016/j.contraception.2012.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurse Family Partnership. 2011 Retrieved March 20, 2017, from http://www.nursefamilypartnership.org/
- Ogburn JA(Tony), Espey E, Stonehocker J. Barriers to intrauterine device insertion in postpartum women. Contraception. 2005;72(6):426–429. doi: 10.1016/j.contraception.2005.05.016. https://doi.org/10.1016/j.contraception.2005.05.016. [DOI] [PubMed] [Google Scholar]
- Potter JE, Hopkins K, Aiken ARA, Hubert C, Stevenson AJ, White K, Grossman D. Unmet demand for highly effective postpartum contraception in Texas. Contraception. 2014;90(5):488–495. doi: 10.1016/j.contraception.2014.06.039. https://doi.org/10.1016/j.contraception.2014.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter JE, Hubert C, Stevenson AJ, Hopkins K, Aiken ARA, White K, Grossman D. Barriers to Postpartum Contraception in Texas and Pregnancy Within 2 Years of Delivery. Obstetrics & Gynecology. 2016;127(2):289–296. doi: 10.1097/AOG.0000000000001201. https://doi.org/10.1097/AOG.0000000000001201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez MI, Chang R, Thiel de Bocanegra H. The impact of postpartum contraception on reducing preterm birth: findings from California. American Journal of Obstetrics and Gynecology. 2015 doi: 10.1016/j.ajog.2015.07.033. https://doi.org/10.1016/j.ajog.2015.07.033. [DOI] [PubMed]
- Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: Reducing Barriers to Long-Acting Reversible Contraception. American Journal of Obstetrics and Gynecology. 2010;203(2):115.e1–115.e7. doi: 10.1016/j.ajog.2010.04.017. https://doi.org/10.1016/j.ajog.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speroff L, Mishell DR., Jr The postpartum visit: it’s time for a change in order to optimally initiate contraception. Contraception. 2008;78(2):90–98. doi: 10.1016/j.contraception.2008.04.005. https://doi.org/10.1016/j.contraception.2008.04.005. [DOI] [PubMed] [Google Scholar]
- Stiggelbout AM, der Weijden TV, Wit MPTD, Frosch D, Légaré F, Montori VM, … Elwyn G. Shared decision making: really putting patients at the centre of healthcare. BMJ. 2012;344:e256. doi: 10.1136/bmj.e256. https://doi.org/10.1136/bmj.e256. [DOI] [PubMed] [Google Scholar]
- Tang JH, Dominik RC, Zerden ML, Verbiest SB, Brody SC, Stuart GS. Effect of an educational script on postpartum contraceptive use: a randomized controlled trial. Contraception. 2014;90(2):162–167. doi: 10.1016/j.contraception.2014.03.017. https://doi.org/10.1016/j.contraception.2014.03.017. [DOI] [PubMed] [Google Scholar]
- Tang JH, Dominik R, Re S, Brody S, Stuart GS. Characteristics associated with interest in long-acting reversible contraception in a postpartum population. Contraception. 2013;88(1):52–57. doi: 10.1016/j.contraception.2012.10.014. https://doi.org/10.1016/j.contraception.2012.10.014. [DOI] [PubMed] [Google Scholar]
- Thiel de Bocanegra H, Chang R, Howell M, Darney P. Interpregnancy intervals: impact of postpartum contraceptive effectiveness and coverage. American Journal of Obstetrics and Gynecology. 2014;210(4):311.e1, 8. doi: 10.1016/j.ajog.2013.12.020. https://doi.org/10.1016/j.ajog.2013.12.020. [DOI] [PubMed] [Google Scholar]
- Thiel de Bocanegra H, Cross Riedel J, Menz M, Darney PD, Brindis CD. Onsite Provision of Specialized Contraceptive Services: Does Title X Funding Enhance Access? Journal of Women’s Health. 2014;23(5):428–433. doi: 10.1089/jwh.2013.4511. https://doi.org/10.1089/jwh.2013.4511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tocce K, Goldthwaite L, Sheeder J, Eichengreen C, Teal S. Barriers to immediate postpartum LARC method use 1 year after Medicaid policy change. Contraception. 2015;92(4):379. https://doi.org/10.1016/j.contraception.2015.06.103. [Google Scholar]
- Tocce K, Sheeder JL, Teal SB. Rapid repeat pregnancy in adolescents: do immediate postpartum contraceptive implants make a difference? American Journal of Obstetrics and Gynecology. 2012;206(6):481.e1–481.e7. doi: 10.1016/j.ajog.2012.04.015. https://doi.org/10.1016/j.ajog.2012.04.015. [DOI] [PubMed] [Google Scholar]
- White K, Grossman D, Hopkins K, Potter JE. Cutting Family Planning in Texas. New England Journal of Medicine. 2012;367(13):1179–1181. doi: 10.1056/NEJMp1207920. https://doi.org/10.1056/NEJMp1207920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K, Hopkins K, Aiken ARA, Stevenson A, Hubert C, Grossman D, Potter JE. The impact of reproductive health legislation on family planning clinic services in Texas. American Journal of Public Health. 2015;105(5):851–858. doi: 10.2105/AJPH.2014.302515. https://doi.org/10.2105/AJPH.2014.302515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K, Teal SB, Potter JE. Contraception After Delivery and Short Interpregnancy Intervals Among Women in the United States. Obstetrics & Gynecology. 2015;125(6):1471–1477. doi: 10.1097/AOG.0000000000000841. https://doi.org/10.1097/AOG.0000000000000841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson EK, Fowler CI, Koo HP. Postpartum Contraceptive Use Among Adolescent Mothers in Seven States. Journal of Adolescent Health. 2013;52(3):278–283. doi: 10.1016/j.jadohealth.2012.05.004. https://doi.org/10.1016/j.jadohealth.2012.05.004. [DOI] [PubMed] [Google Scholar]
- Zapata LB, Murtaza S, Whiteman MK, Jamieson DJ, Robbins CL, Marchbanks PA, … Curtis KM. Contraceptive counseling and postpartum contraceptive use. American Journal of Obstetrics and Gynecology. 2015;212(2):171.e1–171.e8. doi: 10.1016/j.ajog.2014.07.059. https://doi.org/10.1016/j.ajog.2014.07.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zerden ML, Tang JH, Stuart GS, Norton DR, Verbiest SB, Brody S. Barriers to Receiving Long-acting Reversible Contraception in the Postpartum Period. Women’s Health Issues. 2015 doi: 10.1016/j.whi.2015.06.004. https://doi.org/10.1016/j.whi.2015.06.004. [DOI] [PubMed]