Abstract
Background
2-Methylene-19-nor-(20S)-1α,25-dihydroxyvitamin D3 (DP001 or 2MD) is a novel, potent 1α-hydroxylated vitamin D analog that binds to the vitamin D receptor and suppresses parathyroid hormone synthesis and secretion with potential for an improved safety profile compared to existing active vitamin D analogs. The purpose of this study was to evaluate the pharmacokinetics of DP001 given orally after hemodialysis.
Methods
DP001 (550 ng) was given orally to 11 hemodialysis patients with secondary hyperparathyroidism after each dialysis session (3 times/week) for 4 weeks. Pharmacokinetic analyses were performed after the first and final dose.
Results
After the first and final dose, the half-life of DP001 was similar (55.8 ± 13.0 and 50.8 ± 8.2 h, respectively). At 4 weeks, the time to maximum plasma concentration was 4.0 ± 0.8 h, with a concentration maximum of 3.4 ± 0.3 pg/mL. The area under the curve (0 to infinity) after the final dose was 204.3 ± 23.9 pg h/mL, and apparent volume of distribution was 2.03 ± 0.22 L/kg. At week 4, mean intact parathyroid hormone was suppressed 33% from the baseline (pre-dose) value (313 ± 52 vs 462 ± 39 pg/mL, respectively). No clinically significant changes from baseline values were found for vital signs, electrocardiogram measurements, or other laboratory parameters, including serum calcium and phosphorus.
Conclusions
In hemodialysis patients, DP001 has a longer half-life than existing vitamin D therapies and enables control of parathyroid hormone when administered every 2–3 days on the day of dialysis. It is effective at a lower concentration maximum and area under the curve than other clinically available vitamin D compounds. DP001 may represent a therapeutic improvement over existing compounds due to rapid and extensive distribution to its target and its long half-life enabling sustained parathyroid hormone suppression. These studies support further evaluation of DP001 in longer-term treatment of secondary hyperparathyroidism.
Key Points
| The elimination half-life of DP001 given orally to end-stage renal disease patients on hemodialysis is 51 h and is much longer than the clinically available vitamin D receptor agonists. |
| Compared to baseline, after 4 weeks of DP001, mean intact parathyroid hormone (iPTH) post-dose was suppressed 33% and no clinically significant changes in serum calcium, phosphorus, or calcium X phosphorus product were observed. |
| DP001 is a novel and potent vitamin D receptor analog that may represent a therapeutic improvement in the control of PTH suppression in hemodialysis patients due to its long half-life and tissue distribution. |
Introduction
Secondary hyperparathyroidism (SHPT) is a common complication of progressive chronic kidney disease. Elevated intact parathyroid hormone (iPTH) levels can be found early in the course of the disease, i.e., when glomerular filtration rate declines to about 60 mL/min or sometimes even earlier [1]. This rise in iPTH level is multifactorial, and is contributed to by decreased concentration of 1α,25-dihydroxyvitamin D3 and phosphorus retention. SHPT leads to osteitis fibrosa, which is a high bone turnover state resulting in disordered bone formation. Chronically elevated iPTH levels also promote efflux of calcium and phosphorus from bones, and may promote vascular calcification.
Nearly 75% of dialysis patients receive vitamin D receptor (VDR) agonists for the treatment of SHPT. Commercially available synthetic calcitriol (1α,25-dihydroxyvitamin D3) is an effective treatment for SHPT, but often leads to hypercalcemia because of its effect on increasing intestinal calcium and phosphorus absorption along with increasing bone calcium mobilization [2–4]. Frequent hypercalcemia and hyperphosphatemia limit continuation and/or dose escalation of calcitriol. Vitamin D analogs such as paricalcitol (19-nor-1α,25-dihydroxyvitamin D2) and doxercalciferol (1α-hydroxyvitamin D2) have been useful in such patients, as they continue to have an iPTH-suppressing action with reportedly less calcemic and phosphatemic side effects [5, 6, 7]. However, even with these improved analogs, the ability to reach a clinically effective dose may be limited by hypercalcemia [8]. Thus, in some cases a calcimimetic is added to help suppress iPTH; however, this drug class carries with it the risk of producing hypocalcemia and other gastrointestinal side effects [2, 8, 9].
DP001 (2-methylene-19-nor-(20S)-1α,25-dihydroxyvitamin D3, also known as 2MD) is a new VDR activator (VDRA) with high selectivity for bone and parathyroid gland [10–13]. DP001 produces potent suppression of serum iPTH levels both in humans and animal models of renal failure. DP001 has less calcemic activity at effective doses than paricalcitol in the uremic rat model of SHPT and has been shown to lower iPTH levels in osteopenic women [11]. In two phase 2 studies in patients with end-stage renal disease (ESRD), DP001 was shown to be effective in managing SHPT in patients on hemodialysis, including those previously treated with both pharmaceutical vitamin D and a calcimimetic [14, 15]. In a double-blind phase 2b trial, approximately 80% of those administered DP001 achieved the primary endpoint (two consecutive ≥30% decreases in iPTH from baseline), whereas only 5% of the placebo group responded. DP001 reduced iPTH levels by at least 30% by week 4, and this reduction was maintained throughout the remainder of the 12-week study. Clinical studies to date indicate that DP001 is efficacious and has an excellent safety profile.
The pharmacokinetics of DP001 in dialysis patients has not been studied. Thus, the present study was conducted in order to understand the lifetime of the drug in the blood, as well as to explore the relationship of plasma concentration to therapeutic effect. We report the results of a pharmacokinetic study of this new agent in stage 5 hemodialysis patients after the first dose and after 4 weeks of therapy. The pharmacodynamic change in iPTH and safety analyses are also presented.
Methods
Study Design and Objectives
Study Location and Objective
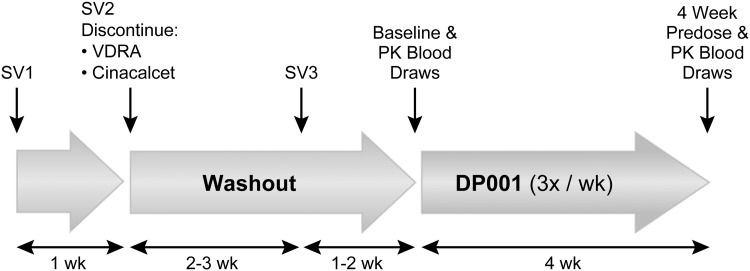
This phase 2a, open label study (Fig. 1) was conducted at two dialysis centers in the USA (Washington University School of Medicine, St Louis, MO, and Orange County Research Center, Tustin, CA). The institutional review board at each site approved this study. The specific objective of this study was to evaluate the pharmacokinetics of oral DP001 in ESRD patients on hemodialysis after the first and last dose (4 weeks) of drug.
Fig. 1.
General schematic of the PK study. Eligible patients who met the criteria set for SV1 proceeded to SV2 and discontinued their active vitamin D and cinacalcet, if applicable, and underwent a drug washout period. Subjects entered the treatment phase if serum values at SV3 were as follows: iPTH ≥300 pg/mL, albumin-corrected serum calcium ≤9.8 mg/dL and phosphorus ≤6.5 mg/dL. PK plasma samples were collected after the first dose and before the last dose and at various times after that dose. The treatment period lasted 4 weeks, with the first and final visits scheduled to occur on the same day of the week. Additional blood samples were collected at 4, 12 and 48 h after the final dose for analysis of iPTH, corrected calcium, and phosphorus. iPTH intact parathyroid hormone, PK pharmacokinetic, SV screening visit, VDRA vitamin D receptor activator, wk week
Study Participants
The eligible study population consisted of men and women at least 18 years of age who were diagnosed with ESRD and SHPT. Eligible patients were receiving hemodialysis 3 times per week and a VDRA (calcitrol or paricalcitol) or prodrug (doxercalciferol) for the treatment of SHPT for at least 3 months prior to screening. The main exclusion criteria were concomitant use of medications known to interfere with vitamin D metabolism, aluminum-based phosphorus binders, recent surgery, active malignancy, or determination by the investigator that the patient was an unsuitable candidate.
During the screening phase, patients underwent a washout of active vitamin D and cinacalcet (if applicable) for a minimum of 2 weeks. After washout, the serum laboratory values required to enroll in the study and proceed to the treatment phase were iPTH ≥300 pg/mL, corrected calcium ≤9.8 mg/dL {corrected for albumin using the equation [0.8 × (4 − patient’s albumin; g/dL)] + serum Ca level; mg/dL}, and phosphorus ≤6.5 mg/dL.
Study Treatment Phase
Baseline measurements were collected prior to the dialysis session and prior to the administration of study drug. The treatment phase started with the first dose of study drug. Drug product was in the form of softgel capsules. A dose of 550 ng of DP001 was administered orally by study personnel at the end of each dialysis session (3 times per week) for 4 weeks. This dose was chosen based on a prior dose-finding study in which the majority of patients receiving the 550-ng dose responded with iPTH reduction (≥30%) without safety concerns [14].
Sample Collection for Chemistry Panel and Intact Parathyroid Hormone (iPTH)
Blood samples for the evaluation of iPTH and other chemistry parameters were collected prior to dialysis at screening visits and the pre-baseline, baseline, week 2 and week 4 visits. Blood was collected into serum separator tubes and allowed to clot undisturbed for 30–60 min. Within 60 min of collection, the tubes were centrifuged for 10–15 min at 1800g until clot and serum were separated by a well-formed polymer barrier. Approximately 2 mL of red cell-free serum was transferred to a cryovial for measurement of iPTH, and a second 2-mL aliquot was prepared for the chemistry panel. Serum aliquots were frozen and sent on dry ice to a central laboratory (LabConnect, LLC) for analysis. The iPTH assay utilized was Beckman Coulter Access®.
Blood samples for hematology were collected into potassium EDTA tubes, inverted to mix, then shipped in the primary collection vial under ambient conditions to the central laboratory for analysis.
Sample Collection for Pharmacokinetic Studies
Blood samples for plasma concentration–time profiles of DP001 were collected at two times during the study. The first collection was made after the first dose of study drug at 1, 2, 4, 8, 24 and 40–48 h following the dose, with the 40–48 h collection immediately preceding the next scheduled dose. The final collection of pharmacokinetic blood samples took place at week 4: pre-dose and 1, 2, 4, 8, 24, 40–48, 64–72 and 88–96 h following the final dose of study drug. Blood samples were collected into sodium heparin tubes, immediately stored in an ice/water bath (~5 °C) for up to 45 min, followed by separation by centrifugation (~2000g × 15 min at ~5 °C). Within 90 min of blood collection, plasma aliquots were layered with argon gas, frozen on dry ice, then shipped to the central laboratory for storage at −70 °C until analyzed.
In addition to plasma collected for the pharmacokinetic analysis of DP001, additional serum samples were collected at 4, 24 and 48 h after the final dose of DP001 at week 4 to evaluate the relationship of study drug concentration to iPTH, albumin-corrected calcium, and phosphorus levels in blood.
Bioanalysis of DP001
DP001 concentrations were measured in plasma samples using a previously described method [11]. This method combines the use of extraction, high pressure liquid chromatography (HPLC) separation and a cell reporter bioassay to determine the amount of DP001 (<5 pg/mL) that is present in plasma after the oral dose. Briefly, plasma samples (0.25–1.5 mL) were subjected to solid phase extraction to remove basic compounds by cation exchange. Sample clean up by solid phase extraction was followed by concentration and application to a C18 HPLC column and collection of DP001-containing fractions. The fractions collected for the measurement of DP001 were selected based on the elution position of radiolabeled DP001 in parallel samples. This HPLC method separates DP001 from other endogenous forms of vitamin D. The DP001-containing fractions were taken to dryness, re-suspended in cell culture medium, and applied to ROS17/2.8 cells stably transfected with a luciferase reporter gene under the control of the 25-hydroxyvitamin D3 24-hydroxylase promoter [16]. The assay for DP001 has a lower limit of quantitation of 0.15 pg/mL plasma and an upper limit of quantitation of 4.49 pg/mL plasma.
Statistical Methods
Pharmacokinetic analyses were performed using Phoenix WinNonlin Version 6.4 (Centara USA, Princeton, NJ). The pharmacokinetic parameters analyzed were maximum plasma concentration (C max), time of C max (T max), area under the plasma concentration–time curve from time zero to 48 h post-dose (AUC0–48), area under the plasma concentration–time curve from time zero extrapolated to infinity (AUC0–inf), apparent clearance (CL/F) per kg body weight (kgBW), terminal phase rate constant (lambdaz), elimination half-life (t ½), and apparent volume of distribution (Vz/F) per kgBW assuming complete absorption. AUC values were calculated using the linear trapezoidal rule. The exponential rate constant of the terminal phase (lambda) was estimated by linear regression of the log concentration versus time for the data associated with the terminal phase of the plasma concentration–time profile. The number of data points included in the regression were determined by visual inspection, with a minimum of three data points used, excluding C max. The difference between means of pharmacokinetic parameters after the first and final (multiple) dose was analyzed using a paired t test and SAS 9.4 software using a 95% confidence interval (P ≤ 0.05). Descriptive statistics are presented for other study variables. For continuous variables, these descriptive statistics include number, mean, standard error of the mean, minimum, median, and maximum. For categorical variables, counts and percentages are presented.
Efficacy and pharmacokinetic analyses are presented for the per protocol set (PPS), defined as all subjects who enrolled, completed the treatment phase of the study without any major protocol violations, were compliant with study visits (100% of all scheduled study visits completed within an allowed ±3 day window and not more than one dose of study medication missed or more than 14 doses taken), and had sufficient plasma concentration data for the estimation of at least one pharmacokinetic parameter.
Safety analyses were performed on the safety set (defined as all subjects who enrolled and received at least one dose of study drug), which was the same as the full analysis set (FAS). Safety was assessed by adverse events, vital signs and electrocardiogram (ECG) results, changes in serum calcium and serum phosphorus from baseline, and other clinical laboratory values. The following three laboratory values were used as safety thresholds: two consecutive iPTH values of <150 pg/mL, two consecutive albumin-corrected total serum calcium values of >10.6 mg/dL, and two consecutive albumin-corrected total serum calcium × serum phosphorus product values of >62 mg2/dL2. Treatment emergent adverse events (TEAEs) were defined as adverse events that occurred after study drug administration began at baseline through 30 days after the last study visit.
Results
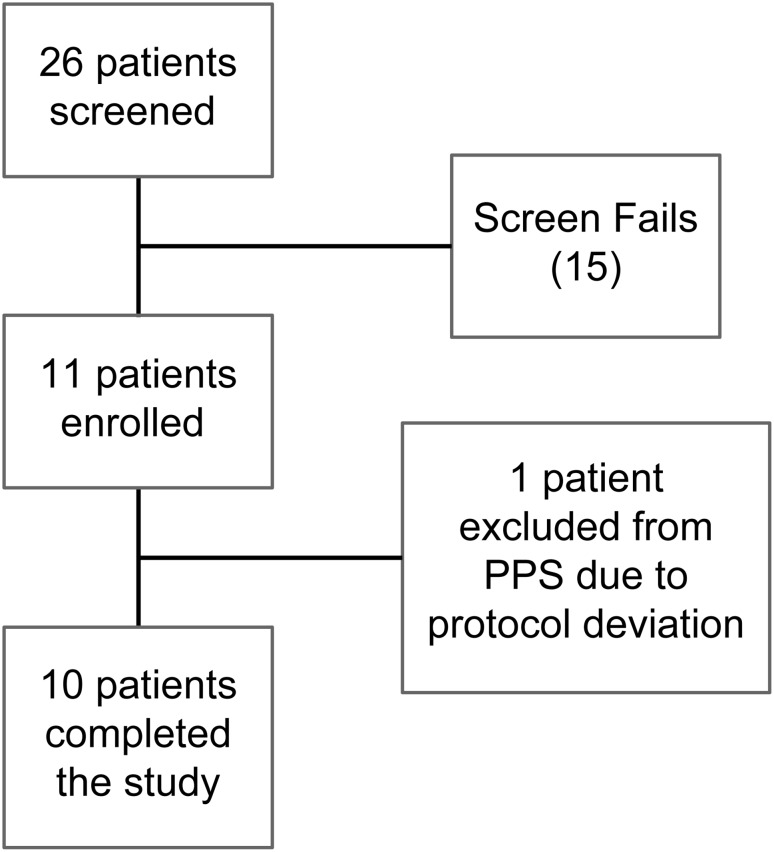
The general study outline and patient disposition are shown in Figs. 1 and 2, respectively. A total of 26 patients were screened and 11 were enrolled, completed the study, and constitute the FAS (see Fig. 2 for study patient disposition). One enrolled patient was excluded from the PPS and pharmacokinetic analysis because of a major protocol deviation, consisting of non-compliance with the schedule of required study visits (the treatment period extended longer than the specified 4 weeks). Thus, ten of the 11 enrolled subjects constituted the PPS.
Fig. 2.
Patient disposition. Of the 26 patients screened, 11 completed the study (FAS), and one of these patients was excluded due to a protocol deviation (PPS = 10). Fifteen patients failed screening for the following reasons: iPTH level not within the specified range (n = 8), withdrew consent (n = 3), inappropriate pharmaceutical vitamin D (active vitamin D) history (n = 2), unacceptable serum calcium levels (n = 1), and not having hemodialysis 3 times per week (n = 1). FAS full analysis set, iPTH intact parathyroid hormone, PPS per protocol set
Patient demographic characteristics at baseline for the FAS are described in Table 1. All patients were receiving active vitamin D (VDRA or prodrug) prior to screening, and one was also receiving a calcimimetic (cinacalcet). Mean iPTH levels at baseline (after washout) were about 5 times the upper limit of normal of the assay (88 pg/mL).
Table 1.
Baseline demographics
| Characteristic or parameter | Full analysis set (n = 11) | Per protocol set (n = 10) |
|---|---|---|
| Median age, years (range) | 51 (39–68) | 50 (39–68) |
| Male, n (%) | 6 (55%) | 5 (50%) |
| Median BMI, kg/m2 (range)a | 35.3 (18.9–54.1) | 36.5 (18.9–54.1) |
| African American, n (%) | 6 (55%) | 6 (60%) |
| Caucasian, n (%) | 5 (45%) | 4 (40%) |
aBody mass index (BMI) kg/m2 = [weight at baseline (kg)]/[height at baseline (m)2]
Pharmacokinetic Analysis
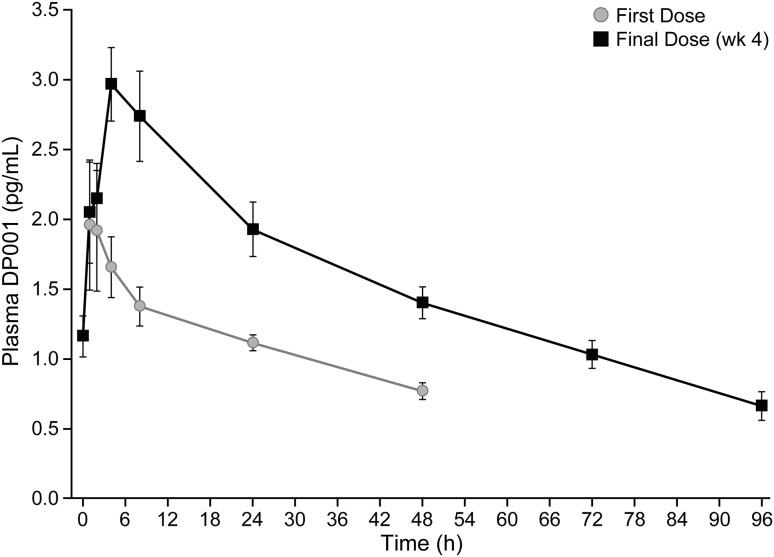
The mean DP001 plasma concentration over time curves after the first and final doses are displayed in Fig. 3, and the pharmacokinetic parameters are shown in Table 2. The calculated half-lives (t ½) of DP001 after the first and final dose were similar (55.8 ± 13.0 and 50.8 ± 8.2 h, respectively). At 4 weeks, 9 of 10 subjects had a t ½ between 30 and 61 h. Given a t ½ of approximately 2 days, steady-state levels of DP001 would be reached by 2 weeks of dosing. As expected, the AUC0–48 increased after 4 weeks of dosing compared to values after one dose. The accumulation index for a drug with a half-life of 2 days given every 2–3 days should be approximately 2, in agreement with the 1.9-fold increase in AUC0–48 observed after the first dose compared to that after 4 weeks of dosing. After 4 weeks of dosing, the AUC0–inf was 204.3 ± 23.9 pg h/mL. DP001 and vitamin D analog bioavailability is known to be high based on oral bioavailability studies conducted in rats with tritiated DP001 (unpublished) and from studies of the structurally related 19-nor vitamin D analog paricalcitol (72–86%); for this reason, the dose of DP001 administered was used to calculate the volume of distribution [17]. DP001 showed a large volume of distribution, indicating that only a small fraction of the dose remained in the plasma and the drug was highly distributed into tissue.
Fig. 3.
DP001 plasma concentration in relation to time (PPS). Blood was collected at multiple times after the first oral dose of DP001 and prior to and after the final oral dose at week 4. Values shown are mean ± standard error of the mean. PPS per protocol set, wk week
Table 2.
Pharmacokinetic parameters after the first dose (baseline) and final dose (week 4) (per protocol set)
| Parameter (units) | Statistic | First dose (n = 8–10)a | Final dose (n = 10) |
|---|---|---|---|
| C max (pg/mL) | Mean ± SEM | 2.5 ± 0.4 | 3.4 ± 0.3 |
| Median (min, max) | 2.0 (1.4, 5.0) | 3.8 (2.0, 4.4) | |
| T max (h) | Mean ± SEM | 2.1 ± 0.4 | 4.0 ± 0.8 |
| Median (min, max) | 1.5 (1.0, 4.0) | 4.0 (1.0, 8.0) | |
| AUC0–48 (pg h/mL) | Mean ± SEM | 50.6 ± 5.9b | 97.5 ± 8.3b |
| Median (min, max) | 49.9 (10.0, 82.3) | 87.6 (74.1, 146.9) | |
| t ½ (h) | Mean ± SEM | 55.8 ± 13.0 | 50.8 ± 8.2 |
| Median (min, max) | 40.6 (26.1, 131.2) | 44.6 (30.3, 116.7) | |
| (CL/F)/kg [(mL/h)/kg] | Mean ± SEM | 50.2 ± 11.0 | 32.8 ± 5.6 |
| Median (min, max) | 58.0 (3.5, 87.5) | 31.6 (12.4, 68.2) | |
| (Vz/F)/kg (L/kg) | Mean ± SEM | 3.53 ± 0.41b | 2.03 ± 0.22b |
| Median (min, max) | 3.15 (2.60, 6.09) | 1.90 (1.16, 3.32) |
AUC 0–48 area under the plasma concentration–time curve from time zero to 48 h post-dose, (CL/F)/kg apparent clearance per kg body weight, C max maximum plasma concentration, SEM standard error of the mean, t ½ elimination half-life, T max time of C max, (Vz/F)/kg apparent volume of distribution per kg body weight
aSome parameters could not be derived for two subjects at baseline. For one subject, the terminal phase had not been reached, and for the other, there were not three observable values after C max
bFirst dose and final dose values differ significantly, P ≤ 0.05
iPTH, Calcium and Phosphorus Levels
Serum levels of iPTH, calcium, and phosphorus were measured prior to the first dose (baseline), and at several points surrounding the week 4 evaluation (pre-dose and at 4, 24 and 48 h post-dose, see Table 3). At week 4, 50% of the study subjects achieved at least a 30% reduction in serum iPTH. There were no changes in corrected calcium, phosphorus or their product from baseline to the week 4 pre-dose value, and these serum chemistry measures remained unchanged 4, 24 and 48 h after the final dose.
Table 3.
Serum biochemical parameters at baseline and week 4a (per protocol set)
| First dose (baseline) pre-doseb | Final dose (week 4) | ||||
|---|---|---|---|---|---|
| Pre-doseb | 4 hc | 24 hc | 48 hc | ||
| iPTH (pg/mL) | 462 ± 39d | 313 ± 52 | 386 ± 83 | 311 ± 45 | 336 ± 57 |
| Corrected calcium (mg/dL) | 9.0 ± 0.1 | 9.2 ± 0.2 | 9.0 ± 0.1 | 9.3 ± 0.2 | 9.3 ± 0.1 |
| Phosphorus (mg/dL) | 4.7 ± 0.5 | 4.9 ± 0.3 | 3.7 ± 0.2 | 4.6 ± 0.4 | 5.1 ± 0.3 |
| Corrected calcium × phosphorus product (mg2/dL2) | 42.3 ± 5.4 | 45.9 ± 3.6 | 33.8 ± 2.3 | 43.4 ± 4.0 | 47.5 ± 3.3 |
aValues are mean ± standard error of the mean (n = 10 with the exception of one missing sample for corrected calcium, phosphorus, and the product of the two at baseline)
bPre-dose = pre-dialysis determination
cMeasurements at 4, 24 and 48 h are times after the final dose administered at the end of hemodialysis
dIntact parathyroid hormone (iPTH) prior to the first dose (baseline) = average of the pre-baseline iPTH value and the baseline iPTH value
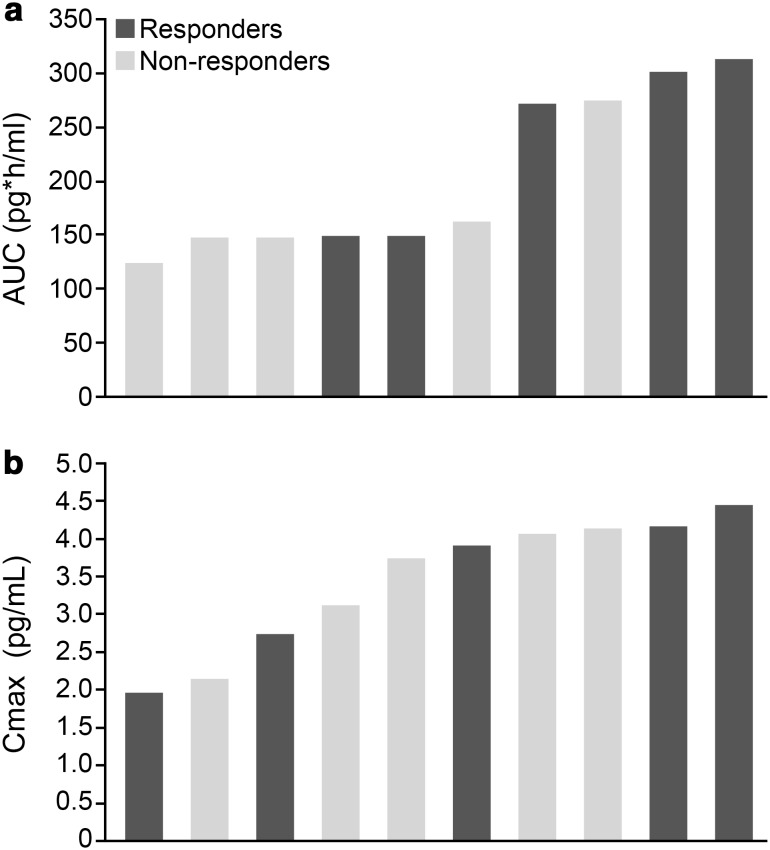
Changes in iPTH in Relation to Drug Concentration
We performed several exploratory analyses of the relationship of DP001 levels to PTH responsiveness. Patients who achieved a ≥30% decrease in their iPTH level from baseline to week 4 at predialysis (five of ten in the PPS) were classified as responders, and the remaining patients were considered non-responders. When AUC0–inf was examined in relationship to iPTH response in a waterfall analysis, 3 out of 5 responders had an AUC0–inf between 272 and 313 pg h/mL, whereas 4 of the 5 non-responders had lower values, between 124 and 162 pg h/mL (Fig. 4a). There appeared to be no relationship between C max and response (Fig. 4b). The serum level of iPTH in the responders was suppressed in a sustained fashion when measured 4, 24 and 48 h after the final dose (−47, −47 and −58% from baseline, respectively), whereas the levels of DP001 rose from the predose level (1.31 pg/mL at 0 h) to a level of 3.03 pg/mL at 4 h, followed by a gradual decline by 24 h and 48 h to 2.22 and 1.45 pg/mL, respectively. The mean DP001 blood value 4 h after the dose in the non-responders (2.90 pg/mL) was similar to that in the responders, whereas iPTH was +5, −18 and +10% of baseline at 4, 24 and 48 h after the dose. The inability to define a discrete blood level or range as predictive of response may be due to the fact that DP001 distributes extensively from blood into the tissue, as evidenced by the large volume of distribution (approximately five times the volume of body water at week 4).
Fig. 4.
Waterfall plot of iPTH responders and non-responders at week 4 in the PPS in relation to DP001 AUC0–inf (a) and C max (b). AUC 0–inf area under the plasma concentration–time curve from time zero extrapolated to infinity, C max maximum plasma concentration, iPTH intact parathyroid hormone, PPS per protocol set
In summary, the pharmacodynamic assessment at week 4 showed iPTH remains suppressed throughout a 48-h period during the time when drug levels in the blood are changing. Further, drug levels in the blood are not predictive of iPTH response.
Safety
None of the patients in the 4-week pharmacokinetic study of DP001 withdrew from the trial, none were discontinued, and no TEAEs were reported. Only one patient had two consecutive iPTH values below 150 pg/mL during the study drug treatment period. DP001 had no effect on other clinical laboratory or hematology values, vital signs or ECG results. No subjects reached or exceeded the safety threshold for albumin-corrected total serum calcium or albumin-corrected total serum calcium × serum phosphorus product, and serum calcium and phosphorus levels remained within acceptable limits after 4 weeks of therapy with DP001, as shown in Table 3.
Discussion
SHPT is a common complication of progressive chronic kidney disease. Although the pathogenesis of SHPT is complex, deficiency of calcitriol is a central issue. Treatment of SHPT is centered on treatment with calcitriol or its analogs to suppress PTH production and improve bone turnover.
Calcitriol, although effective in suppressing PTH, results in hypercalcemia and hyperphosphatemia by enhancing intestinal calcium and phosphorus absorption and increasing bone resorption [18]. Calcitriol analogs were developed to reduce hypercalcemia. Paricalcitol is three times less potent than calcitriol for PTH suppression, but also ten times less calcemic [19]. In an animal model of renal failure, DP001 suppressed iPTH at a dose 300-fold less than that of paricalcitol, and unlike paricalcitol, DP001 produced no increase in serum calcium at that dose [11]. This improvement in therapeutic window may be related to the selective localization of DP001 to the parathyroid and more favorable pharmacokinetics.
This report describes the first pharmacokinetic data available to understand the clinical benefits of DP001 in dialysis patients. The present study indicates that the pharmacokinetics of DP001 differ markedly from those of other VDRAs such as calcitriol and paricalcitol in hemodialysis patients [17, 20]. The C max and AUC of DP001 are much lower, and the volume of distribution is larger than the values for oral calcitriol and paricalcitol in hemodialysis patients, even after adjusting for dose differences. DP001’s interaction with serum vitamin D binding protein is very weak (unpublished data) and may contribute to its low C max and AUC, and large volume of distribution. Thus, it appears that little DP001 remains in the blood; rather, it may be rapidly distributed to peripheral targets such as the parathyroid, where it can act. Studies in vivo in the rat show that DP001 localizes to the greatest extent in the thyroid/parathyroid glands [11]. Perhaps the most dramatic finding in the present pharmacokinetic study is that the elimination half-life of DP001 in dialysis patients is much longer than that of the other agents (51 h for DP001 vs 20 h for paricalcitol [17] and 27 h for calcitriol [20]).
Studies in vitro and in vivo demonstrate DP001 is a highly potent vitamin D analog [10, 12, 21]. Consistent with this, a 550 ng dose of DP001 administered orally 3 times weekly to dialysis patients led to suppression of iPTH over 4 weeks, and half of the treated patients responded to this dose with at least a 30% reduction in iPTH. The DP001 C max was similar for responders and non-responders, suggesting that the drug concentration in blood is not a good predictor of response. When levels of DP001 were examined at 4, 24 and 48 h in responders at 4 weeks, the value was highest at the 4-h time point and declined thereafter, whereas, iPTH was effectively suppressed to a similar extent at all these times. Therefore, DP001 effectively suppresses iPTH in a prolonged fashion when given every 2–3 days. In the case of the non-responders, it is possible the concentration of DP001 needed to suppress iPTH was not achieved at the parathyroid gland, and higher doses or longer duration of treatment is necessary. Additional studies in larger numbers of patients at higher doses and/or for longer time periods are needed to address this question.
Among dialysis patients, endogenous calcitriol levels are usually quite low, and correlate with increased mortality [22]. Conversely, supplementation with active or pharmaceutical vitamin D has been shown to improve survival compared to untreated patients [23]. Additionally, use of paricalcitol, a vitamin D analog, is associated with improved survival compared to calcitriol in hemodialysis patients [24]. The ability of DP001 to suppress iPTH without adversely affecting serum calcium and phosphorus, and to maintain such suppression between doses may also offer clinical benefits beyond control of SHPT in dialysis patients. In addition, studies in vitro and in vivo demonstrate DP001 has significant anabolic actions on bone [10, 12].
In conclusion, DP001 has a long half-life and effectively suppresses iPTH without increasing serum calcium or phosphorus. Further studies of this novel VDRA are needed to determine the optimal dose range and time needed to control SHPT in dialysis patients.
Acknowledgements
We thank Dr. P. Hutson in the School of Pharmacy at the University of Wisconsin-Madison for his helpful advice regarding pharmacokinetic analysis and for carefully reading the manuscript. We thank E. Lake in the Department of Biochemistry at the University of Wisconsin-Madison for her important contribution to the analysis of PK samples. We also thank L. Vanderploug in the Media Lab in the Department of Biochemistry at the University of Wisconsin-Madison for her help with the artwork.
Compliance with Ethical Standards
Conflict of interest
DWC has been a paid advisor for Deltanoid and a speaker for Abbvie. HFD and MCD have financial interests in Deltanoid Pharmaceuticals, Inc., and along with LAP, JBZ, JGZ, WJB and WB, have worked as part-time employees of Deltanoid Pharmaceuticals, Inc., the sponsor of these studies. Pharmacokinetic sample analyses were supported by a research sponsored agreement from Deltanoid Pharmaceuticals, Inc. provided to the University of Wisconsin-Madison. RP has no conflicts of interest to declare.
References
- 1.Levin A, Bakris GL, Molitch M, Smulders M, Tian J, Williams LA, et al. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: results of the study to evaluate early kidney disease. Kidney Int. 2007;71(1):31–38. doi: 10.1038/sj.ki.5002009. [DOI] [PubMed] [Google Scholar]
- 2.Mittman N, Desiraju B, Meyer KB, Chattopadhyay J, Avram MM. Treatment of secondary hyperparathyroidism in ESRD: a 2-year, single-center crossover study. Kidney Int Suppl. 2010;117:S33–S36. doi: 10.1038/ki.2010.191. [DOI] [PubMed] [Google Scholar]
- 3.Ong LM, Narayanan P, Goh HK, Manocha AB, Ghazali A, Omar M, et al. Randomized controlled trial to compare the efficacy and safety of oral paricalcitol with oral calcitriol in dialysis patients with secondary hyperparathyroidism. Nephrology (Carlton). 2013;18(3):194–200. doi: 10.1111/nep.12029. [DOI] [PubMed] [Google Scholar]
- 4.Quarles LD, Yohay DA, Carroll BA, Spritzer CE, Minda SA, Bartholomay D, et al. Prospective trial of pulse oral versus intravenous calcitriol treatment of hyperparathyroidism in ESRD. Kidney Int. 1994;45(6):1710–1721. doi: 10.1038/ki.1994.223. [DOI] [PubMed] [Google Scholar]
- 5.Martin KJ, Gonzalez EA. Vitamin D analogs: actions and role in the treatment of secondary hyperparathyroidism. Semin Nephrol. 2004;24(5):456–459. doi: 10.1016/j.semnephrol.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 6.Brown AJ, Slatopolsky E. Drug insight: vitamin D analogs in the treatment of secondary hyperparathyroidism in patients with chronic kidney disease. Nat Clin Pract Endocrinol Metab. 2007;3(2):134–144. doi: 10.1038/ncpendmet0394. [DOI] [PubMed] [Google Scholar]
- 7.Sprague SM, Llach F, Amdahl M, Taccetta C, Batlle D. Paricalcitol versus calcitriol in the treatment of secondary hyperparathyroidism. Kidney Int. 2003;63(4):1483–1490. doi: 10.1046/j.1523-1755.2003.00878.x. [DOI] [PubMed] [Google Scholar]
- 8.Tonbul HZ, Solak Y, Atalay H, Turkmen K, Altintepe L. Efficacy and tolerability of intravenous paricalcitol in calcitriol-resistant hemodialysis patients with secondary hyperparathyroidism: 12-month prospective study. Ren Fail. 2012;34(3):297–303. doi: 10.3109/0886022X.2011.647298. [DOI] [PubMed] [Google Scholar]
- 9.Dyer CA. Safety and tolerability of paricalcitol in patients with chronic kidney disease. Expert Opin Drug Saf. 2013;12(5):717–728. doi: 10.1517/14740338.2013.791675. [DOI] [PubMed] [Google Scholar]
- 10.Sicinski RR, Prahl JM, Smith CM, DeLuca HF. New 1α,25-dihydroxy-19-norvitamin D3 compounds of high biological activity: synthesis and biological evaluation of 2-hydroxymethyl, 2-methyl, and 2-methylene analogues. J Med Chem. 1998;41(23):4662–4674. doi: 10.1021/jm9802618. [DOI] [PubMed] [Google Scholar]
- 11.Zella JB, Plum LA, Plowchalk DR, Potochoiba M, Clagett-Dame M, DeLuca HF. Novel, selective vitamin D analog suppresses parathyroid hormone in uremic animals and postmenopausal women. Am J Nephrol. 2014;39(6):476–483. doi: 10.1159/000362846. [DOI] [PubMed] [Google Scholar]
- 12.Shevde NK, Plum LA, Clagett-Dame M, Yamamoto H, Pike JW, DeLuca HF. A potent analog of 1α,25-dihydroxyvitamin D3 selectively induces bone formation. Proc Natl Acad Sci USA. 2002;99(21):13487–13491. doi: 10.1073/pnas.202471299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vanhooke JL, Tadi BP, Benning MM, Plum LA, DeLuca HF. New analogs of 2-methylene-19-nor-(20S)-1,25-dihydroxyvitamin D3 with conformationally restricted side chains: evaluation of biological activity and structural determination of VDR-bound conformations. Arch Biochem Biophys. 2007;460(2):161–165. doi: 10.1016/j.abb.2006.11.029. [DOI] [PubMed] [Google Scholar]
- 14.Pandey R, Zella J, Clagett-Dame M, Plum LA, DeLuca HF, Coyne DW. Use of 2MD, a novel oral calcitriol analog, in hemodialysis patients with secondary hyperparathyroidism. Am J Nephrol. 2016;43(3):213–220. doi: 10.1159/000445756. [DOI] [PubMed] [Google Scholar]
- 15.Thadhani R, Zella JB, Knutson DC, Blaser WJ, Plum LA, Clagett-Dame M, et al. 2MD (DP001), a single agent in the management of hemodialysis patients: a randomized trial. Am J Nephrol. 2017;45(1):40–48. doi: 10.1159/000452680. [DOI] [PubMed] [Google Scholar]
- 16.Arbour NC, Ross TK, Zierold C, Prahl JM, DeLuca HF. A highly sensitive method for large-scale measurements of 1,25-dihydroxyvitamin D. Anal Biochem. 1998;255(1):148–154. doi: 10.1006/abio.1997.2439. [DOI] [PubMed] [Google Scholar]
- 17.Abbott-Laboratories. Zemplar (paricalcitol) capsules [package insert]. North Chicago; 2009.
- 18.Slatopolsky E, Finch J, Brown A. New vitamin D analogs. Kidney Int. 2003;85(Supplement):S83–S87. doi: 10.1046/j.1523-1755.63.s85.20.x. [DOI] [PubMed] [Google Scholar]
- 19.Slatopolsky E, Finch J, Ritter C, Denda M, Morrissey J, Brown A, et al. A new analog of calcitriol, 19-nor-1,25-(OH)2D2, suppresses parathyroid hormone secretion in uremic rats in the absence of hypercalcemia. Am J Kidney Dis. 1995;26(5):852–860. doi: 10.1016/0272-6386(95)90455-7. [DOI] [PubMed] [Google Scholar]
- 20.Brandi L, Egfjord M, Olgaard K. Pharmacokinetics of 1,25(OH)(2)D-3 and 1 alpha(OH)D-3 in normal and uraemic men. Nephrol Dial Transplant. 2002;17(5):829–842. doi: 10.1093/ndt/17.5.829. [DOI] [PubMed] [Google Scholar]
- 21.Yamamoto H, Shevde NK, Warrier A, Plum LA, DeLuca HF, Pike JW. 2-Methylene-19-nor-(20S)-1,25-dihydroxyvitamin D3 potently stimulates gene-specific DNA binding of the vitamin D receptor in osteoblasts. J Biol Chem. 2003;278(34):31756–31765. doi: 10.1074/jbc.M304737200. [DOI] [PubMed] [Google Scholar]
- 22.Wolf M, Shah A, Gutierrez O, Ankers E, Monroy M, Tamez H, et al. Vitamin D levels and early mortality among incident hemodialysis patients. Kidney Int. 2007;72(8):1004–1013. doi: 10.1038/sj.ki.5002451. [DOI] [PubMed] [Google Scholar]
- 23.Teng M, Wolf M, Ofsthun MN, Lazarus JM, Hernan MA, Camargo CA, Jr, et al. Activated injectable vitamin D and hemodialysis survival: a historical cohort study. J Am Soc Nephrol. 2005;16(4):1115–1125. doi: 10.1681/ASN.2004070573. [DOI] [PubMed] [Google Scholar]
- 24.Teng M, Wolf M, Lowrie E, Ofsthun N, Lazarus JM, Thadhani R. Survival of patients undergoing hemodialysis with paricalcitol or calcitriol therapy. N Engl J Med. 2003;349(5):446–456. doi: 10.1056/NEJMoa022536. [DOI] [PubMed] [Google Scholar]