Abstract
Early life is a period of particular susceptibility to respiratory infections and symptoms are frequently more severe in infants than in adults. The neonatal immune system is generally held to be deficient in most compartments; responses to innate stimuli are weak, antigen-presenting cells have poor immunostimulatory activity and adaptive lymphocyte responses are limited, leading to poor immune memory and ineffective vaccine responses. For mucosal surfaces such as the lung, which is continuously exposed to airborne antigen and to potential pathogenic invasion, the ability to discriminate between harmless and potentially dangerous antigens is essential, to prevent inflammation that could lead to loss of gaseous exchange and damage to the developing lung tissue. We have only recently begun to define the differences in respiratory immunity in early life and its environmental and developmental influences. The innate immune system may be of relatively greater importance than the adaptive immune system in the neonatal and infant period than later in life, as it does not require specific antigenic experience. A better understanding of what constitutes protective innate immunity in the respiratory tract in this age group and the factors that influence its development should allow us to predict why certain infants are vulnerable to severe respiratory infections, design treatments to accelerate the development of protective immunity, and design age specific adjuvants to better boost immunity to infection in the lung.
Keywords: respiratory, neonatal, infection, respiratory syncytial virus, innate immunity
Introduction
Respiratory infection is one of the leading causes of mortality in children under 5 years of age (1, 2). Early life respiratory viral infections are most commonly caused by rhinovirus, respiratory syncytial virus (RSV), influenza, parainfluenza virus, and coronavirus (3). Infection is frequently restricted to the upper respiratory tract but may develop into severe lower respiratory tract infection, such as RSV bronchiolitis, the leading cause of hospitalization of infants worldwide (4–7). Bacterial pneumonia in infants, caused by agents such as Haemophilus influenzae and Streptococcus pneumoniae, is estimated to cause a million deaths in infants under 5 years of age annually (8, 9). Maternal antibodies afford some protection against infection but wane over the first months of life, and neonates and infants respond poorly to vaccination, leaving early life as a window of particular vulnerability to respiratory infection (10, 11). Experiences during the crucial neonatal and infant window may shape respiratory health in the long term (12–14). Severe RSV infection in infants is associated with the development of wheeze and asthma in childhood (15–19) and even respiratory disease that occur late in life, such as chronic obstructive pulmonary disease, are associated with early life events (20–24).
At birth, the neonate emerges from the sheltered intrauterine environment into a plethora of antigenic challenges from pathogens, commensals, and harmless environmental antigens. Neonatal immunity is, in general, attenuated compared to that of adults (4, 25–29). Differences in immunity in early life are due to tissue leukopenia, cell intrinsic hyporesponsiveness, and inhibitory mechanisms, such as CD71+ immunosuppressive erythroid cells and high levels of adenosine in extracellular fluids (26, 28–31). Protective Th1 polarized responses and antibodies are produced less well in early life than in adults, along with a propensity to develop unwanted, Th2 or Th17 biased, or dysregulated inflammation (28, 31–33), for example, following vaccination or allergen exposure (34, 35). TLR stimulation of cord blood leukocytes results in a lower production of proinflammatory, Th1-associated cytokines (IL-12p70, TNF-α, IFN-α), and greater production of IL-10 and the Th17-promoting IL-6 and IL-23 when compared to stimulation of adult blood cells, although equivalent responses to TLR 7/8 ligand R848 occur (29, 36, 37). Over the first few years of life, antiviral and Th1-biasing cytokine production increases (38, 39).
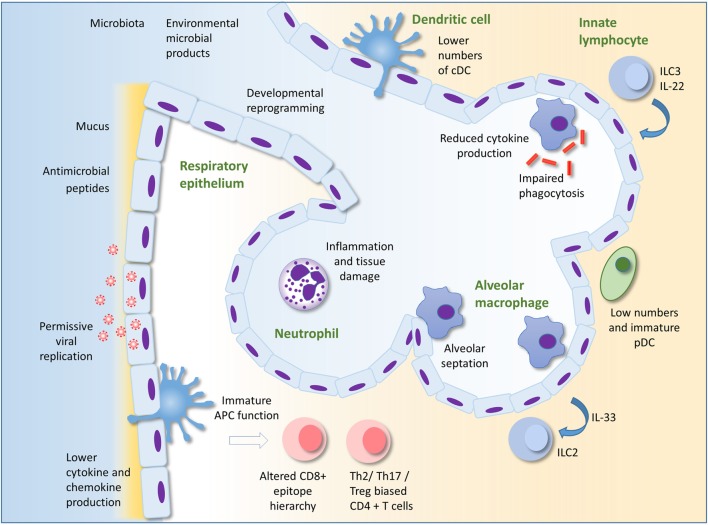
In the face of an inexperienced adaptive response, innate immunity is likely to play a more dominant role in protection against infection in early life than in adulthood. This is supported by the findings that many gene polymorphisms associated with severe RSV infection in infants encode components of the innate immune response (4, 40–43). The importance of TLR signaling in early life is illustrated by individuals with genetic deficiencies in components of the TLR signaling pathway such as MyD88 or IRAK-4. These patients are at high risk of bacterial infection in childhood, including in the respiratory tract; however, their condition improves dramatically with age (44). This review will focus on describing our current knowledge of innate immunity in the neonatal lung as a first line of defense against infection. Some potentially important mechanisms underlying susceptibility to lung infection in infants are summarized in Figure 1.
Figure 1.
Innate immunity to infection in the lung in early life. Alveolar macrophages (AM) are the most numerous leukocyte in the lungs in early life. Reduced cytokine production and phagocytic ability in AM in early life compared to those of adults could underlie susceptibility to infection. AM also promote pre- and post-natal lung development and remodeling. The respiratory epithelium protects against infection through the production of mucus and antimicrobial peptides. Production of type I IFNs may be lower in infant than adult epithelial cells, perhaps permitting greater viral replication. Epithelial cells may interact with innate lymphocytes to both initiate and regulate inflammation. Developmental reprograming in the epithelium in early life may also alter the nature of the epithelial response to infection. There are low numbers of pDC in the lungs compared to adults. Recruitment of neutrophils to the lung occurs less readily in early life compared to adults in some circumstances, but in other situations, excessive recruitment of inflammatory cells can lead to lung inflammation, tissue damage, and impairment of gaseous exchange. Immaturity and lower numbers of dendritic cells, the environment as well as intrinsic differences in T cells in early life may result in the development of skewed helper T cell responses and an altered epitope hierarchy in CD8+ T cells. Innate immunity in the lung in early life is influenced by acquisition of the microbiota, exposure to microbial products and other environmental factors, as well as the infant genome. Adapted by permission from Macmillan Publishers Ltd: Nature Reviews Immunology (45), copyright 2014.
Respiratory Immunity in Early Life
It is relatively difficult to obtain samples from the lower airways of healthy infant subjects, so many studies have been carried out in murine and other animal models. Information on the cellular composition of the neonatal lung in humans has come from analysis of bronchoalveolar lavage fluid composition (46–49), immunohistochemistry (50), and more recently, extensive phenotypic analysis of leukocyte subsets in pediatric tissues (51–53).
Adaptive Immunity
Fetal airways are essentially devoid of lymphocytes, they are seeded from birth, and lymphocytes increase as a proportion of airway cells over the first few years of life (48, 54). There is a relative paucity in CD4+ cells (46, 50), and memory T cells are less abundant in infant lungs than in adults, though they are more abundant in the lungs than many other tissues (51). Tregs are relatively abundant in pediatric tissues and may have a higher suppressive capacity than those from adults (28, 51) and a transient increase in regulatory T cells, associated with microbial colonization, protects from hyperresponsiveness to allergen (35). A failure of regulation may underlie excessive inflammation in infection, as in RSV bronchiolitis (43), and RSV infection in early life can increase susceptibility to allergic inflammation in the mouse model through an impairment of regulatory T cells (4, 55). CD8+ T cells in the lung correlate with disease severity in infants with respiratory failure due to respiratory viral infection (52) and in neonatal mice infected with RSV, a CD8+ T cell epitope hierarchy emerges, which is distinct to that of adults (56). Distinct phenotypes of adaptive lymphocytes are found in early life. A subset of Th cells in human cord blood produce the neutrophil chemoattractant interleukin-8 upon activation (57) and, during RSV infection, a regulatory phenotype in the neonatal B cell compartment may dampen protective immunity (58).
Lung Dendritic Cells (DCs)
There is some evidence that neonatal T cells have the capacity to mount adult-like protective responses to lung infection. Adoptive transfer of neonatal CD4+ T cells into Pneumocystis carinii-infected adult SCID mice allowed for adult-level pathogen clearance and cytokine production (59, 60), suggesting that the neonatal environment in the lung influences T cell responses. This may be due in part to the function of neonatal antigen-presenting cells. Neonatal mouse lungs contain relatively fewer conventional DCs (cDCs), which are immature and poorly functional (56, 61, 62), although mature functions ex vivo have been reported (63). During neonatal RSV infection, migratory cDCs are dominated by CD103+ DCs, while the CD11b+ contribution increases with age (64). These CD103+ DCs are phenotypically immature and poorly functional (65), and this may influence the magnitude and epitope hierarchy of the CD8+ T cell response (64–66), although these are also influenced by T cell intrinsic differences and regulatory T cells (56, 67). As well as stimulating protective responses, lung DCs in neonates must promote tolerance to harmless environmental antigens. CD11b+ cDCs in the lung induce Th2 responses to allergens, but transiently express high levels of PD-L1, which promotes tolerance, following acquisition of the microbiota (35, 68). In contrast to murine studies, the relative frequency of different DC subsets in the human lung appears to be relatively stable over the life course (53).
In the murine neonatal lung, potent IFN-α-producing pDC cells are scarce (61), and there is limited recruitment of pDCs and IFN-α production following RSV infection (69).
Alveolar Macrophages (AM)
Lung resident macrophages, which include AM and the less well-characterized interstitial macrophages (70–72), are an important component of the first line of defense in the lung. In the steady state, AMs remove debris and maintain a tolerogenic environment; during infection, they secrete proinflammatory cytokines and contribute to pathogen clearance; and after infection, they aid resolution of inflammation (45). AMs are the predominant cell type in the neonatal airway, they appear in the alveolar compartment from just before birth and throughout the first week of life, and are relatively abundant and self-renewing, persisting for at least 11 weeks in mice (47–50, 73, 74).
Stimulation of cultured cells has been used to interrogate the relative antimicrobial functions of neonatal and adult AMs. LPS stimulation of rodent or ovine AMs results in similar or even enhanced upregulation of TNF-α and CXC-chemokines in neonatal compared to adult cells (75–77), though others demonstrated a reduced translocation of NF-κB to the nucleus of AM from neonatal mice (78). Enhanced phagocytosis by neonatal compared to adult rat AM has been observed (75), but others have reported impaired phagocytosis and subsequent killing of yeast particles in neonatal rhesus monkey AMs; and impaired phagocytosis of opsonized red blood cells in neonatal rat AMs in comparison to adults (79, 80). In a murine model of Pneumocystis infection, neonatal AMs were delayed in their expression of activation markers in vivo in comparison to adults (81). Similarly, during murine neonatal RSV infection, there was reduced and delayed AM activation compared to adult infection (82), but intranasal IFN-γ was able to promote AM maturation (82). Little is known about responses in human infant AMs. Cultured cells obtained by bronchoalveolar lavage from infants <2 years of age produce lower IL-1 and TNF-α following LPS stimulation compared with cells from children aged 2–17 (54). The apparent contradictions in the data on AM function in early life may reflect differences in the species, age, experimental conditions, and assays used. Various macrophage functions are likely to mature at different rates. Neonatal and adult AMs are likely to behave differently in their respective lung environments, which is a limitation of these in vitro studies.
Respiratory Epithelial Cells
The respiratory epithelium is the principal site of replication of respiratory viruses. It is in close communication with AM and acts an immune sentinel producing inflammatory mediators, such as type I and III interferons, mucus, and antimicrobial proteins (45, 83). Relatively little is known about the immunological functions of the airway epithelium in early life. In cultured tracheobronchial epithelial cells from Rhesus macaques of different ages (infant, juvenile, and adult), IL-8 production on exposure to LPS positively correlated with age (84). Furthermore, epithelial cells from juveniles housed in filtered air produced higher cytokine responses than those in conventional housing suggesting the microbial richness of the environment may influence epithelial responsiveness. The same group demonstrated that infant Rhesus monkey primary epithelial cell cultures are more permissive for the H1N1 influenza virus than those from adult airways, while producing less IL-1α (85).
In humans, type I IFNs are detected at only low levels in the airways of RSV-bronchiolitic infants. This may be due to inhibition of the host anti-viral response by the viral non-structural proteins but alternatively may reflect the timing of sampling, and an IFN-induced gene signature is detectable in blood (86–88). Pediatric nasal and airway epithelial cells cultured from bronchial brushings are readily infected with RSV (89–91) and poor induction of type I IFNs by RSV is reflected in these cultures (92, 93). Instead, the type III interferon IL-29 (IFN-λ) is detected both in the airways of bronchiolitic infants and in cultures of RSV infected airway epithelial cells, and IL-29 pretreatment of cultured epithelial cells attenuates RSV growth (92, 93). Epithelial cells are probably a key source of inflammatory cytokines in respiratory tract secretions of infants with acute RSV (92, 94, 95), including the type-2 immunity promoting cytokine IL-33 (96). The cells used in many in vitro experiments on pediatric respiratory epithelial cells were originally taken from the conducting airway and data surrounding lower airway and ATII cells in early life is even sparser.
Antimicrobial proteins are a first line of defense at barrier sites and are produced primarily by epithelial cells and innate leukocytes, particularly neutrophils (97, 98). In the lung, they include surfactants as well as S100s, β-defensins, and cathelicidin and they may provide protection against important infant respiratory infections, including RSV (99–102). Cathelicidin has direct antiviral activity against RSV, can prevent infection in vitro and in vivo and in children hospitalized with bronchiolitis, those with low serum cathelicidin were significantly more likely to have RSV infection and a longer hospital stay (97, 103–107).
Innate Lymphocytes
Neonatal murine lungs show no quantitative deficiency in γδ T cells as a proportion of CD3+ T cells (61, 108). Exposure to allergen in neonatal mice can stimulate innate ILC2 lymphocytes, a major source of type 2 cytokines (109). Colonization by the microbiota in neonates protects against the accumulation of potentially pro-inflammatory mucosal iNKT cells in the lung and gut (110). Colonization of the gut of neonatal mice can also lead to intestinal DC mediated upregulation of CCR4 on IL-22 producing ILC3, which allows their migration into the lungs of neonatal mice, and promotes protection against bacterial pneumonia (111).
Neutrophils
Recruitment of innate leukocytes and, in particular, neutrophils, is likely to play an important role in the innate response to infection in the neonatal lung following microbial recognition. Both TLR4 gene and protein expression are present in the murine lung in the fetus and increase with age through to adulthood (112, 113). TLR2 expression is also present in the human fetal lung and increases with gestational age (114). It appears that there is an immaturity of chemokine production at baseline in the respiratory mucosa. Expression of CXCL2 is low in neonatal mice compared with adults (115) and in uninfected infants (newborn to 18 months), the concentration of IL-8 in nasal washes positively correlates with age (116). There is a dramatically reduced and delayed neutrophil influx in neonatal lung in response to administration of LPS or bacteria in comparison to adult animals (75, 117–119). In the neonatal murine lung, infection with the paramyxovirus Sendai virus results in a minimal early influx of neutrophils and low production of pro-inflammatory cytokines compared with the adult lung; similarly in murine RSV infection, early pro-inflammatory cytokine production is impaired (108, 115). Diminished recruitment of neutrophils may also be due to an impaired chemotaxic ability of infant neutrophils (25, 120, 121).
In severe RSV bronchiolitis in infants, neutrophils can account for the majority of cells recovered from the airways, associated with increased neutrophil elastase (122–125) and IL-8 (94, 126), although others have reported a lower inflammatory cytokine response in infants with severe vs mild RSV bronchiolitis (127). There is a considerable influx of neutrophils into S. pneumoniae-infected lungs of neonatal and adult mice, with the neonatal influx even occurring at a lower bacterial dose (128). It is unclear under what circumstances the neonatal lung will produce an equivalent or exacerbated inflammatory response compared to that of adults, whether this simply requires a high level of stimulation or whether additional factors are involved.
Factors Influencing the Development and Maturation of Lung Immunity
Despite the apparent absence of a mature adult-like immune system, neonates are able to produce effective immune responses that defend against infection and indeed excessive inflammation can occur. The neonate must strike a balance between protection against infection and potential damage to the developing lung and may use alternative mechanisms of protection against infection to those that predominate in adults.
Exposure to microbial products from the environment, the microbiota, or infection may be beneficial in terms of their ability to promote immune maturation and more adult like innate and adaptive immunity (28, 30). Treatment with TLR agonists CpG or LPS during RSV infection alters the CD8+ T cell response toward a more adult-like immunodominance (66) and treatment of neonatal mice with CpG prior to RSV infection shifts the secondary response to re-infection away from a type 2 response (129). Furthermore, administration of BCG shifts lung CD4+ responses away from a Th2 bias and cDC from BCG treated lungs promote Th1 responses (61).
The microbiota is acquired from the mother at birth and in early life and an adult-like microbiome is established by around 3 years of age (130). The composition of the microbiota and microbial richness of the environment in which children develop have been linked to susceptibility to severe respiratory infections and the development of wheeze and asthma (131–133). Environmental microbial exposure may influence lung health by establishing the set-point of immunological responsiveness of the lung, as seen by the attenuation of allergic lung inflammation by airway exposure to LPS or endotoxin rich dust samples (133, 134). Additionally, commensal bacteria may influence neonatal respiratory immunity indirectly. For example, sensing of commensal bacteria by gut DCs promotes resistance to bacterial pneumonia in neonatal mice (111). Factors that shape the microbiota, such as delivery by cesarean section and antibiotic use in early life and pregnancy, are likely to profoundly influence the developing immune system (14, 135). Other environmental factors that regulate the balance of immunity in the infant respiratory tract may include diet, vitamin D status, breast feeding, maternal immunity, and exposure to environmental pollutants.
Significant stages of lung development occur both before and after birth and hyporesponsiveness to immune stimuli may have evolved to protect the developing lung from the disruptive and damaging effects of inflammation (136, 137). This is evidenced in mouse models of chorioamnionitis, where exposure of the fetal lung to LPS results in abnormal development of the distal airways (138, 139). In addition, IL-1β expression in the fetal or newborn lung impairs normal postnatal development (140). Reciprocally, the developmental programmes active in resident lung cells, which drive cell growth and differentiation may also influence immune responses (141, 142). Macrophages take on important roles in lung development and remodeling including septation and vascularization of the alveoli after birth (137, 143). Macrophages associate with sites of branching morphogenesis where they assume a tissue remodeling phenotype and promote development through production of growth factors and matrix metalloproteases (143). Polarization of macrophages away from this phenotype might, therefore, be a mechanism by which pro-inflammatory signals disrupt lung development (138, 140). As with lung macrophages, the respiratory epithelium will be subject to lung developmental programmes extending into the postnatal period, which regulate epithelial cell proliferation and differentiation, and these may potentially also alter epithelial immunological function. Foxa2 is an epithelially expressed member of the forkhead family of transcription factors. In the developing lung, it regulates epithelial differentiation and controls goblet cell hyperplasia. It also has immunoregulatory functions and limits type-2 immunity through inhibition of the cysteinyl LT signaling pathway (83, 141, 144).
Conclusion
The mechanisms that regulate inflammatory responses to microbial stimulation in the lung need to be more fully elucidated. Increasing our knowledge of how the developing immune system responds to infectious challenge is of importance for development of neonatal vaccines and treatments for exaggerated respiratory inflammation during infection. In certain circumstances, the immune system in early life is capable of adult-level responses, and perhaps boosting responses in at-risk infants—in treatment for acute infectious disease or as adjuvant for vaccination—would be a beneficial protective strategy. Additionally, selectively harnessing the protective innate mechanisms that are already expressed at adult or greater than adult levels in the neonate could be a safe therapeutic method. Thus, while early life is clearly a period of immunological vulnerability for the developing lung, it is also an opportunity for effective intervention strategies, which could benefit respiratory health not only in infancy, but into adulthood.
Author Contributions
LL researched the literature and wrote the review. FC wrote the review, edited, and updated it.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Some of the content of this manuscript first appeared in Lambert (2015) (145), Immunology of the Neonatal Lung and the Long Term Consequences of Neonatal Respiratory Virus Infection for Pulmonary Innate Immunity. Ph.D. thesis: Imperial College London. We thank Dr. Spiros Makris for critical reading of the manuscript. This work was supported by a Medical Research Council New Investigator Research Grant to FC (G1001763).
References
- 1.Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE, et al. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet (2015) 385(9966):430–40. 10.1016/S0140-6736(14)61698-6 [DOI] [PubMed] [Google Scholar]
- 2.Walker CLF, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta ZA, et al. Global burden of childhood pneumonia and diarrhoea. Lancet (2013) 381(9875):1405–16. 10.1016/S0140-6736(13)60222-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tregoning JS, Schwarze J. Respiratory viral infections in infants: causes, clinical symptoms, virology, and immunology. Clin Microbiol Rev (2010) 23(1):74–98. 10.1128/CMR.00032-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lambert L, Sagfors AM, Openshaw PJM, Culley FJ. Immunity to RSV in early-life. Front Immunol (2014) 5:466. 10.3389/fimmu.2014.00466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nair H, Nokes DJ, Gessner BD, Dherani M, Madhi SA, Singleton RJ, et al. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet (2010) 375(9725):1545–55. 10.1016/S0140-6736(10)60206-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall CB, Weinberg GA, Iwane MK, Blumkin AK, Edwards KM, Staat MA, et al. The burden of respiratory syncytial virus infection in young children. N Engl J Med (2009) 360(6):588–98. 10.1056/NEJMoa0804877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meissner HC. Viral bronchiolitis in children. N Engl J Med (2016) 374(1):62–72. 10.1056/NEJMra1413456 [DOI] [PubMed] [Google Scholar]
- 8.O’Brien KL, Wolfson LJ, Watt JP, Henkle E, Deloria-Knoll M, McCall N, et al. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: global estimates. Lancet (2009) 374(9693):893–902. 10.1016/S0140-6736(09)61204-6 [DOI] [PubMed] [Google Scholar]
- 9.Watt JP, Wolfson LJ, O’Brien KL, Henkle E, Deloria-Knoll M, McCall N, et al. Burden of disease caused by Haemophilus influenzae type b in children younger than 5 years: global estimates. Lancet (2009) 374(9693):903–11. 10.1016/S0140-6736(09)61203-4 [DOI] [PubMed] [Google Scholar]
- 10.Mohr E, Siegrist C-A. Vaccination in early life: standing up to the challenges. Curr Opin Immunol (2016) 41:1–8. 10.1016/j.coi.2016.04.004 [DOI] [PubMed] [Google Scholar]
- 11.Heath PT, Culley FJ, Jones CE, Kampmann B, Le Doare K, Nunes MC, et al. Group B streptococcus and respiratory syncytial virus immunisation during pregnancy: a landscape analysis. Lancet Infect Dis (2017) 17(7):e223–34. 10.1016/S1473-3099(17)30232-3 [DOI] [PubMed] [Google Scholar]
- 12.Renz H, Brandtzaeg P, Hornef M. The impact of perinatal immune development on mucosal homeostasis and chronic inflammation. Nat Rev Immunol (2011) 12(1):9–23. 10.1038/nri3112 [DOI] [PubMed] [Google Scholar]
- 13.Lloyd CM, Marsland BJ. Lung homeostasis: influence of age, microbes, and the immune system. Immunity (2017) 46(4):549–61. 10.1016/j.immuni.2017.04.005 [DOI] [PubMed] [Google Scholar]
- 14.Man WH, de Steenhuijsen Piters WAA, Bogaert D. The microbiota of the respiratory tract: gatekeeper to respiratory health. Nat Rev Microbiol (2017) 15(5):259–70. 10.1038/nrmicro.2017.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biesbroek G, Tsivtsivadze E, Sanders EAM, Montijn R, Veenhoven RH, Keijser BJF, et al. Early respiratory microbiota composition determines bacterial succession patterns and respiratory health in children. Am J Respir Crit Care Med (2014) 190(11):1283–92. 10.1164/rccm.201407-1240OC [DOI] [PubMed] [Google Scholar]
- 16.De Steenhuijsen Piters WAA, Heinonen S, Hasrat R, Bunsow E, Smith B, Suarez-Arrabal M-C, et al. Nasopharyngeal microbiota, host transcriptome, and disease severity in children with respiratory syncytial virus infection. Am J Respir Crit Care Med (2016) 194(9):1104–15. 10.1164/rccm.201602-0220OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sigurs N, Gustafsson PM, Bjarnason R, Lundberg F, Schmidt S, Sigurbergsson F, et al. Severe respiratory syncytial virus bronchiolitis in infancy and asthma and allergy at age 13. Am J Respir Crit Care Med (2005) 171(2):137–41. 10.1164/rccm.200406-730OC [DOI] [PubMed] [Google Scholar]
- 18.Sigurs N, Aljassim F, Kjellman B, Robinson PD, Sigurbergsson F, Bjarnason R, et al. Asthma and allergy patterns over 18 years after severe RSV bronchiolitis in the first year of life. Thorax (2010) 65(12):1045–52. 10.1136/thx.2009.121582 [DOI] [PubMed] [Google Scholar]
- 19.Caballero MT, Serra ME, Acosta PL, Marzec J, Gibbons L, Salim M, et al. TLR4 genotype and environmental LPS mediate RSV bronchiolitis through Th2 polarization. J Clin Invest (2015) 125(2):571–82. 10.1172/JCI75183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Svanes C, Sunyer J, Plana E, Dharmage S, Heinrich J, Jarvis D, et al. Early life origins of chronic obstructive pulmonary disease. Thorax (2010) 65(1):14–20. 10.1136/thx.2008.112136 [DOI] [PubMed] [Google Scholar]
- 21.Shaheen SO, Barker DJ, Holgate ST. Do lower respiratory tract infections in early childhood cause chronic obstructive pulmonary disease? Am J Respir Crit Care Med (1995) 151(5):1649–51. 10.1164/ajrccm/151.5_Pt_1.1649 [DOI] [PubMed] [Google Scholar]
- 22.Narang I, Bush A. Early origins of chronic obstructive pulmonary disease. Semin Fetal Neonatal Med (2012) 17(2):112–8. 10.1016/j.siny.2012.01.002 [DOI] [PubMed] [Google Scholar]
- 23.Bui DS, Burgess JA, Lowe AJ, Perret JL, Lodge CJ, Bui M, et al. Childhood lung function predicts adult chronic obstructive pulmonary disease and asthma-chronic obstructive pulmonary disease overlap syndrome. Am J Respir Crit Care Med (2017) 196(1):39–46. 10.1164/rccm.201606-1272OC [DOI] [PubMed] [Google Scholar]
- 24.Martinez FD. The origins of asthma and chronic obstructive pulmonary disease in early life. Proc Am Thorac Soc (2009) 6(3):272–7. 10.1513/pats.200808-092RM [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Levy O. Innate immunity of the newborn: basic mechanisms and clinical correlates. Nat Rev Immunol (2007) 7(5):379–90. 10.1038/nri2075 [DOI] [PubMed] [Google Scholar]
- 26.Siegrist C-A, Aspinall R. B-cell responses to vaccination at the extremes of age. Nat Rev Immunol (2009) 9(3):185–94. 10.1038/nri2508 [DOI] [PubMed] [Google Scholar]
- 27.Prendergast AJ, Klenerman P, Goulder PJR. The impact of differential antiviral immunity in children and adults. Nat Rev Immunol (2012) 12(9):636–48. 10.1038/nri3277 [DOI] [PubMed] [Google Scholar]
- 28.Kollmann TR, Kampmann B, Mazmanian SK, Marchant A, Levy O. Protecting the newborn and young infant from infectious diseases: lessons from immune ontogeny. Immunity (2017) 46(3):350–63. 10.1016/j.immuni.2017.03.009 [DOI] [PubMed] [Google Scholar]
- 29.Kollmann TR, Levy O, Montgomery RR, Goriely S. Innate immune function by Toll-like receptors: distinct responses in newborns and the elderly. Immunity (2012) 37(5):771–83. 10.1016/j.immuni.2012.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Torow N, Marsland BJ, Hornef MW, Gollwitzer ES. Neonatal mucosal immunology. Mucosal Immunol (2017) 10(1):5–17. 10.1038/mi.2016.81 [DOI] [PubMed] [Google Scholar]
- 31.Adkins B, Leclerc C, Marshall-Clarke S. Neonatal adaptive immunity comes of age. Nat Rev Immunol (2004) 4(7):553–64. 10.1038/nri1394 [DOI] [PubMed] [Google Scholar]
- 32.Zaghouani H, Hoeman CM, Adkins B. Neonatal immunity: faulty T-helpers and the shortcomings of dendritic cells. Trends Immunol (2009) 30(12):585–91. 10.1016/j.it.2009.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.PrabhuDas M, Adkins B, Gans H, King C, Levy O, Ramilo O, et al. Challenges in infant immunity: implications for responses to infection and vaccines. Nat Immunol (2011) 12(3):189–94. 10.1038/ni0311-189 [DOI] [PubMed] [Google Scholar]
- 34.Saglani S, Mathie SA, Gregory LG, Bell MJ, Bush A, Lloyd CM. Pathophysiological features of asthma develop in parallel in house dust mite-exposed neonatal mice. Am J Respir Cell Mol Biol (2009) 41(3):281–9. 10.1165/rcmb.2008-0396OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gollwitzer ES, Saglani S, Trompette A, Yadava K, Sherburn R, McCoy KD, et al. Lung microbiota promotes tolerance to allergens in neonates via PD-L1. Nat Med (2014) 20(6):642–7. 10.1038/nm.3568 [DOI] [PubMed] [Google Scholar]
- 36.Levy O, Zarember KA, Roy RM, Cywes C, Godowski PJ, Wessels MR. Selective impairment of TLR-mediated innate immunity in human newborns: neonatal blood plasma reduces monocyte TNF-alpha induction by bacterial lipopeptides, lipopolysaccharide, and imiquimod, but preserves the response to R-848. J Immunol (2004) 173(7):4627–34. 10.4049/jimmunol.173.7.4627 [DOI] [PubMed] [Google Scholar]
- 37.Kollmann TR, Crabtree J, Rein-Weston A, Blimkie D, Thommai F, Wang XY, et al. Neonatal innate TLR-mediated responses are distinct from those of adults. J Immunol (2009) 183(11):7150–60. 10.4049/jimmunol.0901481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Corbett NP, Blimkie D, Ho KC, Cai B, Sutherland DP, Kallos A, et al. Ontogeny of Toll-like receptor mediated cytokine responses of human blood mononuclear cells. PLoS One (2010) 5(11):e15041. 10.1371/journal.pone.0015041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Belderbos ME, van Bleek GM, Levy O, Blanken MO, Houben ML, Schuijff L, et al. Skewed pattern of Toll-like receptor 4-mediated cytokine production in human neonatal blood: low LPS-induced IL-12p70 and high IL-10 persist throughout the first month of life. Clin Immunol (2009) 133(2):228–37. 10.1016/j.clim.2009.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Faber TE, Schuurhof A, Vonk A, Koppelman GH, Hennus MP, Kimpen JLL, et al. IL1RL1 gene variants and nasopharyngeal IL1RL-a levels are associated with severe RSV bronchiolitis: a multicenter cohort study. PLoS One (2012) 7(5):e34364. 10.1371/journal.pone.0034364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Janssen R, Bont L, Siezen CLE, Hodemaekers HM, Ermers MJ, Doornbos G, et al. Genetic susceptibility to respiratory syncytial virus bronchiolitis is predominantly associated with innate immune genes. J Infect Dis (2007) 196(6):826–34. 10.1086/520886 [DOI] [PubMed] [Google Scholar]
- 42.Tulic MK, Hurrelbrink RJ, Prêle CM, Laing IA, Upham JW, Le Souef P, et al. TLR4 polymorphisms mediate impaired responses to respiratory syncytial virus and lipopolysaccharide. J Immunol (2007) 179(1):132–40. 10.4049/jimmunol.179.1.132 [DOI] [PubMed] [Google Scholar]
- 43.Openshaw PJM, Chiu C, Culley FJ, Johansson C. Protective and harmful immunity to RSV infection. Annu Rev Immunol (2017) 35(1):501–32. 10.1146/annurev-immunol-051116-052206 [DOI] [PubMed] [Google Scholar]
- 44.Picard C, Casanova J-L, Puel A. Infectious diseases in patients with IRAK-4, MyD88, NEMO, or IκBα deficiency. Clin Microbiol Rev (2011) 24(3):490–7. 10.1128/CMR.00001-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hussell T, Bell TJ. Alveolar macrophages: plasticity in a tissue-specific context. Nat Rev Immunol (2014) 14(2):81–93. 10.1038/nri3600 [DOI] [PubMed] [Google Scholar]
- 46.Ratjen F, Bredendiek M, Zheng L, Brendel M, Costabel U. Lymphocyte subsets in bronchoalveolar lavage fluid of children without bronchopulmonary disease. Am J Respir Crit Care Med (1995) 152(1):174–8. 10.1164/ajrccm.152.1.7599820 [DOI] [PubMed] [Google Scholar]
- 47.Riedler J, Grigg J, Robertson CF. Role of bronchoalveolar lavage in children with lung disease. Eur Respir J (1995) 8(10):1725–30. 10.1183/09031936.95.08101725 [DOI] [PubMed] [Google Scholar]
- 48.Grigg J, Riedler J. Developmental airway cell biology. The “normal” young child. Am J Respir Crit Care Med (2000) 162(2 Pt 2):S52–5. 10.1164/ajrccm.162.supplement_1.maic-14 [DOI] [PubMed] [Google Scholar]
- 49.Ratjen F, Bredendiek M, Brendel M, Meltzer J, Costabel U. Differential cytology of bronchoalveolar lavage fluid in normal children. Eur Respir J (1994) 7(10):1865–70. 10.1183/09031936.94.07101865 [DOI] [PubMed] [Google Scholar]
- 50.Dos Santos ABG, Binoki D, Silva LFF, de Araujo BB, Otter ID, Annoni R, et al. Immune cell profile in infants’ lung tissue. Ann Anat (2013) 195(6):596–604. 10.1016/j.aanat.2013.05.003 [DOI] [PubMed] [Google Scholar]
- 51.Thome JJC, Bickham KL, Ohmura Y, Kubota M, Matsuoka N, Gordon C, et al. Early-life compartmentalization of human T cell differentiation and regulatory function in mucosal and lymphoid tissues. Nat Med (2016) 22(1):72–7. 10.1038/nm.4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Connors TJ, Ravindranath TM, Bickham KL, Gordon CL, Zhang F, Levin B, et al. Airway CD8(+) T cells are associated with lung injury during infant viral respiratory tract infection. Am J Respir Cell Mol Biol (2016) 54(6):822–30. 10.1165/rcmb.2015-0297OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Granot T, Senda T, Carpenter DJ, Matsuoka N, Weiner J, Gordon CL, et al. Dendritic cells display subset and tissue-specific maturation dynamics over human life. Immunity (2017) 46(3):504–15. 10.1016/j.immuni.2017.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Grigg J, Riedler J, Robertson CF, Boyle W, Uren S. Alveolar macrophage immaturity in infants and young children. Eur Respir J (1999) 14(5):1198–205. 10.1183/09031936.99.14511989 [DOI] [PubMed] [Google Scholar]
- 55.Krishnamoorthy N, Khare A, Oriss TB, Raundhal M, Morse C, Yarlagadda M, et al. Early infection with respiratory syncytial virus impairs regulatory T cell function and increases susceptibility to allergic asthma. Nat Med (2012) 18(10):1525–30. 10.1038/nm.2896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ruckwardt TJ, Malloy AMW, Gostick E, Price DA, Dash P, McClaren JL, et al. Neonatal CD8 T-cell hierarchy is distinct from adults and is influenced by intrinsic T cell properties in respiratory syncytial virus infected mice. PLoS Pathog (2011) 7(12):e1002377. 10.1371/journal.ppat.1002377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gibbons D, Fleming P, Virasami A, Michel M-L, Sebire NJ, Costeloe K, et al. Interleukin-8 (CXCL8) production is a signatory T cell effector function of human newborn infants. Nat Med (2014) 20(10):1206–10. 10.1038/nm.3670 [DOI] [PubMed] [Google Scholar]
- 58.Zhivaki D, Lemoine S, Lim A, Morva A, Vidalain P-O, Schandene L, et al. Respiratory syncytial virus infects regulatory B cells in human neonates via chemokine receptor CX3CR1 and promotes lung disease severity. Immunity (2017) 46(2):301–14. 10.1016/j.immuni.2017.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Qureshi MH, Garvy BA. Neonatal T cells in an adult lung environment are competent to resolve Pneumocystis carinii pneumonia. J Immunol (2001) 166(9):5704–11. 10.4049/jimmunol.166.9.5704 [DOI] [PubMed] [Google Scholar]
- 60.Garvy BA, Qureshi MH. Delayed inflammatory response to Pneumocystis carinii infection in neonatal mice is due to an inadequate lung environment. J Immunol (2000) 165(11):6480–6. 10.4049/jimmunol.165.11.6480 [DOI] [PubMed] [Google Scholar]
- 61.Roux X, Remot A, Petit-Camurdan A, Nahori M-A, Kiefer-Biasizzo H, Marchal G, et al. Neonatal lung immune responses show a shift of cytokines and transcription factors toward Th2 and a deficit in conventional and plasmacytoid dendritic cells. Eur J Immunol (2011) 41(10):2852–61. 10.1002/eji.201041224 [DOI] [PubMed] [Google Scholar]
- 62.Nelson DJ, Holt PG. Defective regional immunity in the respiratory tract of neonates is attributable to hyporesponsiveness of local dendritic cells to activation signals. J Immunol (1995) 155(7):3517–24. [PubMed] [Google Scholar]
- 63.Fach SJ, Brockmeier SL, Hobbs LA, Lehmkuhl HD, Sacco RE. Pulmonary dendritic cells isolated from neonatal and adult ovine lung tissue. Vet Immunol Immunopathol (2006) 112(3–4):171–82. 10.1016/j.vetimm.2006.02.012 [DOI] [PubMed] [Google Scholar]
- 64.Ruckwardt TJ, Malloy AMW, Morabito KM, Graham BS. Quantitative and qualitative deficits in neonatal lung-migratory dendritic cells impact the generation of the CD8+ T cell response. PLoS Pathog (2014) 10(2):e1003934. 10.1371/journal.ppat.1003934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ruckwardt TJ, Morabito KM, Bar-Haim E, Nair D, Graham BS. Neonatal mice possess two phenotypically and functionally distinct lung-migratory CD103(+) dendritic cell populations following respiratory infection. Mucosal Immunol (2017). 10.1038/mi.2017.28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Malloy AMW, Ruckwardt TJ, Morabito KM, Lau-Kilby AW, Graham BS. Pulmonary dendritic cell subsets shape the respiratory syncytial virus-specific CD8+ T cell immunodominance hierarchy in neonates. J Immunol (2017) 198(1):394–403. 10.4049/jimmunol.1600486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ruckwardt TJ, Bonaparte KL, Nason MC, Graham BS. Regulatory T cells promote early influx of CD8+ T cells in the lungs of respiratory syncytial virus-infected mice and diminish immunodominance disparities. J Virol (2009) 83(7):3019–28. 10.1128/JVI.00036-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Herbst T, Sichelstiel A, Schär C, Yadava K, Bürki K, Cahenzli J, et al. Dysregulation of allergic airway inflammation in the absence of microbial colonization. Am J Respir Crit Care Med (2011) 184(2):198–205. 10.1164/rccm.201010-1574OC [DOI] [PubMed] [Google Scholar]
- 69.Cormier SA, Shrestha B, Saravia J, Lee GI, Shen L, DeVincenzo JP, et al. Limited type I interferons and plasmacytoid dendritic cells during neonatal respiratory syncytial virus infection permit immunopathogenesis upon reinfection. J Virol (2014) 88(16):9350–60. 10.1128/JVI.00818-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Guilliams M, Lambrecht BN, Hammad H. Division of labor between lung dendritic cells and macrophages in the defense against pulmonary infections. Mucosal Immunol (2013) 6(3):464–73. 10.1038/mi.2013.14 [DOI] [PubMed] [Google Scholar]
- 71.Bedoret D, Wallemacq H, Marichal T, Desmet C, Quesada Calvo F, Henry E, et al. Lung interstitial macrophages alter dendritic cell functions to prevent airway allergy in mice. J Clin Invest (2009) 119(12):3723–38. 10.1172/JCI39717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sabatel C, Radermecker C, Fievez L, Paulissen G, Chakarov S, Fernandes C, et al. Exposure to bacterial CpG DNA protects from airway allergic inflammation by expanding regulatory lung interstitial macrophages. Immunity (2017) 46(3):457–73. 10.1016/j.immuni.2017.02.016 [DOI] [PubMed] [Google Scholar]
- 73.Alenghat E, Esterly JR. Alveolar macrophages in perinatal infants. Pediatrics (1984) 74(2):221–3. [PubMed] [Google Scholar]
- 74.Guilliams M, De Kleer I, Henri S, Post S, Vanhoutte L, De Prijck S, et al. Alveolar macrophages develop from fetal monocytes that differentiate into long-lived cells in the first week of life via GM-CSF. J Exp Med (2013) 210(10):1977–92. 10.1084/jem.20131199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lee PT, Holt PG, McWilliam AS. Role of alveolar macrophages in innate immunity in neonates: evidence for selective lipopolysaccharide binding protein production by rat neonatal alveolar macrophages. Am J Respir Cell Mol Biol (2000) 23(5):652–61. 10.1165/ajrcmb.23.5.4016 [DOI] [PubMed] [Google Scholar]
- 76.Empey KM, Hollifield M, Garvy BA. Exogenous heat-killed Escherichia coli improves alveolar macrophage activity and reduces Pneumocystis carinii lung burden in infant mice. Infect Immun (2007) 75(7):3382–93. 10.1128/IAI.00174-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fach SJ, Olivier A, Gallup JM, Waters TE, Ackermann MR, Lehmkuhl HD, et al. Differential expression of cytokine transcripts in neonatal and adult ovine alveolar macrophages in response to respiratory syncytial virus or toll-like receptor ligation. Vet Immunol Immunopathol (2010) 136(1–2):55–64. 10.1016/j.vetimm.2010.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kurkjian C, Hollifield M, Lines JL, Rogosky A, Empey KM, Qureshi M, et al. Alveolar macrophages in neonatal mice are inherently unresponsive to Pneumocystis murina infection. Infect Immun (2012) 80(8):2835–46. 10.1128/IAI.05707-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ballinger MN, Peters-Golden M, Moore BB. Impaired neonatal macrophage phagocytosis is not explained by overproduction of prostaglandin E2. Respir Res (2011) 12:155. 10.1186/1465-9921-12-155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kurland G, Cheung AT, Miller ME, Ayin SA, Cho MM, Ford EW. The ontogeny of pulmonary defenses: alveolar macrophage function in neonatal and juvenile rhesus monkeys. Pediatr Res (1988) 23(3):293–7. 10.1203/00006450-198803000-00013 [DOI] [PubMed] [Google Scholar]
- 81.Empey KM, Hollifield M, Schuer K, Gigliotti F, Garvy BA. Passive immunization of neonatal mice against Pneumocystis carinii f. sp. muris enhances control of infection without stimulating inflammation. Infect Immun (2004) 72(11):6211–20. 10.1128/IAI.72.11.6211-6220.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Empey KM, Orend JG, Peebles RS, Egaña L, Norris KA, Oury TD, et al. Stimulation of immature lung macrophages with intranasal interferon gamma in a novel neonatal mouse model of respiratory syncytial virus infection. PLoS One (2012) 7(7):e40499. 10.1371/journal.pone.0040499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Whitsett JA, Alenghat T. Respiratory epithelial cells orchestrate pulmonary innate immunity. Nat Immunol (2015) 16(1):27–35. 10.1038/ni.3045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Maniar-Hew K, Clay CC, Postlethwait EM, Evans MJ, Fontaine JH, Miller LA. Innate immune response to LPS in airway epithelium is dependent on chronological age and antecedent exposures. Am J Respir Cell Mol Biol (2013) 49(5):710–20. 10.1165/rcmb.2012-0321OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Clay CC, Reader JR, Gerriets JE, Wang TT, Harrod KS, Miller LA. Enhanced viral replication and modulated innate immune responses in infant airway epithelium following H1N1 infection. J Virol (2014) 88(13):7412–25. 10.1128/JVI.00188-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hall CB, Kopelman AE, Douglas RG, Geiman JM, Meagher MP. Neonatal respiratory syncytial virus infection. N Engl J Med (1979) 300(8):393–6. 10.1056/NEJM197902223000803 [DOI] [PubMed] [Google Scholar]
- 87.Isaacs D. Production of interferon in respiratory syncytial virus bronchiolitis. Arch Dis Child (1989) 64(1):92–5. 10.1136/adc.64.1.92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mejias A, Dimo B, Suarez NM, Garcia C, Suarez-Arrabal MC, Jartti T, et al. Whole blood gene expression profiles to assess pathogenesis and disease severity in infants with respiratory syncytial virus infection. PLoS Med (2013) 10(11):e1001549. 10.1371/journal.pmed.1001549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Villenave R, Thavagnanam S, Sarlang S, Parker J, Douglas I, Skibinski G, et al. In vitro modeling of respiratory syncytial virus infection of pediatric bronchial epithelium, the primary target of infection in vivo. Proc Natl Acad Sci U S A (2012) 109(13):5040–5. 10.1073/pnas.1110203109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fonceca AM, Flanagan BF, Trinick R, Smyth RL, McNamara PS. Primary airway epithelial cultures from children are highly permissive to respiratory syncytial virus infection. Thorax (2012) 67(1):42–8. 10.1136/thoraxjnl-2011-200131 [DOI] [PubMed] [Google Scholar]
- 91.Villenave R, Shields MD, Power UF. Respiratory syncytial virus interaction with human airway epithelium. Trends Microbiol (2013) 21(5):238–44. 10.1016/j.tim.2013.02.004 [DOI] [PubMed] [Google Scholar]
- 92.Villenave R, Broadbent L, Douglas I, Lyons JD, Coyle PV, Teng MN, et al. Induction and antagonism of antiviral responses in respiratory syncytial virus-infected pediatric airway epithelium. J Virol (2015) 89(24):12309–18. 10.1128/JVI.02119-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Okabayashi T, Kojima T, Masaki T, Yokota S-I, Imaizumi T, Tsutsumi H, et al. Type-III interferon, not type-I, is the predominant interferon induced by respiratory viruses in nasal epithelial cells. Virus Res (2011) 160(1–2):360–6. 10.1016/j.virusres.2011.07.011 [DOI] [PubMed] [Google Scholar]
- 94.McNamara PS, Flanagan BF, Hart CA, Smyth RL. Production of chemokines in the lungs of infants with severe respiratory syncytial virus bronchiolitis. J Infect Dis (2005) 191(8):1225–32. 10.1086/428855 [DOI] [PubMed] [Google Scholar]
- 95.McNamara PS, Fonceca AM, Howarth D, Correia JB, Slupsky JR, Trinick RE, et al. Respiratory syncytial virus infection of airway epithelial cells, in vivo and in vitro, supports pulmonary antibody responses by inducing expression of the B cell differentiation factor BAFF. Thorax (2013) 68(1):76–81. 10.1136/thoraxjnl-2012-202288 [DOI] [PubMed] [Google Scholar]
- 96.Saravia J, You D, Shrestha B, Jaligama S, Siefker D, Lee GI, et al. Respiratory syncytial virus disease is mediated by age-variable IL-33. PLoS Pathog (2015) 11(10):e1005217. 10.1371/journal.ppat.1005217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hasegawa K, Mansbach JM, Ajami NJ, Petrosino JF, Freishtat RJ, Teach SJ, et al. Serum cathelicidin, nasopharyngeal microbiota, and disease severity among infants hospitalized with bronchiolitis. J Allergy Clin Immunol (2017) 139(4):1383.e–6.e. 10.1016/j.jaci.2016.09.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Starner TD, Agerberth B, Gudmundsson GH, McCray PB. Expression and activity of beta-defensins and LL-37 in the developing human lung. J Immunol (2005) 174(3):1608–15. 10.4049/jimmunol.174.3.1608 [DOI] [PubMed] [Google Scholar]
- 99.Schaller-Bals S, Schulze A, Bals R. Increased levels of antimicrobial peptides in tracheal aspirates of newborn infants during infection. Am J Respir Crit Care Med (2002) 165(7):992–5. 10.1164/ajrccm.165.7.200110-020 [DOI] [PubMed] [Google Scholar]
- 100.LeVine AM, Gwozdz J, Stark J, Bruno M, Whitsett J, Korfhagen T. Surfactant protein-A enhances respiratory syncytial virus clearance in vivo. J Clin Invest (1999) 103(7):1015–21. 10.1172/JCI5849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Derscheid RJ, Ackermann MR. The innate immune system of the perinatal lung and responses to respiratory syncytial virus infection. Vet Pathol (2013) 50(5):827–41. 10.1177/0300985813480216 [DOI] [PubMed] [Google Scholar]
- 102.Battersby AJ, Khara J, Wright VJ, Levy O, Kampmann B. Antimicrobial proteins and peptides in early life: ontogeny and translational opportunities. Front Immunol (2016) 7:309. 10.3389/fimmu.2016.00309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mansbach JM, Piedra PA, Stevenson MD, Sullivan AF, Forgey TF, Clark S, et al. Prospective multicenter study of children with bronchiolitis requiring mechanical ventilation. Pediatrics (2012) 130(3):e492–500. 10.1542/peds.2012-0444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Mansbach JM, Piedra PA, Borregaard N, Martineau AR, Neuman MI, Espinola JA, et al. Serum cathelicidin level is associated with viral etiology and severity of bronchiolitis. J Allergy Clin Immunol (2012) 130(4):1007.e–8.e. 10.1016/j.jaci.2012.07.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Currie SM, Gwyer Findlay E, McFarlane AJ, Fitch PM, Böttcher B, Colegrave N, et al. Cathelicidins have direct antiviral activity against respiratory syncytial virus in vitro and protective function in vivo in mice and humans. J Immunol (2016) 196(6):2699–710. 10.4049/jimmunol.1502478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Currie SM, Findlay EG, McHugh BJ, Mackellar A, Man T, Macmillan D, et al. The human cathelicidin LL-37 has antiviral activity against respiratory syncytial virus. PLoS One (2013) 8(8):e73659. 10.1371/journal.pone.0073659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Harcourt JL, McDonald M, Svoboda P, Pohl J, Tatti K, Haynes LM. Human cathelicidin, LL-37, inhibits respiratory syncytial virus infection in polarized airway epithelial cells. BMC Res Notes (2016) 9(1):11. 10.1186/s13104-015-1836-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Huang H, Saravia J, You D, Shaw AJ, Cormier SA. Impaired gamma delta T cell-derived IL-17A and inflammasome activation during early respiratory syncytial virus infection in infants. Immunol Cell Biol (2015) 93(2):126–35. 10.1038/icb.2014.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Castanhinha S, Sherburn R, Walker S, Gupta A, Bossley CJ, Buckley J, et al. Pediatric severe asthma with fungal sensitization is mediated by steroid-resistant IL-33. J Allergy Clin Immunol (2015) 136(2):312.e–22.e. 10.1016/j.jaci.2015.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Olszak T, An D, Zeissig S, Vera MP, Richter J, Franke A, et al. Microbial exposure during early life has persistent effects on natural killer T cell function. Science (2012) 336(6080):489–93. 10.1126/science.1219328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gray J, Oehrle K, Worthen G, Alenghat T, Whitsett J, Deshmukh H. Intestinal commensal bacteria mediate lung mucosal immunity and promote resistance of newborn mice to infection. Sci Transl Med (2017) 9(376):eaaf9412. 10.1126/scitranslmed.aaf9412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Harju K, Glumoff V, Hallman M. Ontogeny of Toll-like receptors Tlr2 and Tlr4 in mice. Pediatr Res (2001) 49(1):81–3. 10.1203/00006450-200101000-00018 [DOI] [PubMed] [Google Scholar]
- 113.Harju K, Ojaniemi M, Rounioja S, Glumoff V, Paananen R, Vuolteenaho R, et al. Expression of toll-like receptor 4 and endotoxin responsiveness in mice during perinatal period. Pediatr Res (2005) 57(5 Pt 1):644–8. 10.1203/01.PDR.0000156212.03459.A9 [DOI] [PubMed] [Google Scholar]
- 114.Petrikin JE, Gaedigk R, Leeder JS, Truog WE. Selective Toll-like receptor expression in human fetal lung. Pediatr Res (2010) 68(4):335–8. 10.1203/PDR.0b013e3181ed1134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bhattacharya S, Beal BT, Janowski AM, Shornick LP. Reduced inflammation and altered innate response in neonates during paramyxoviral infection. Virol J (2011) 8:549. 10.1186/1743-422X-8-549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gern JE, Martin MS, Anklam KA, Shen K, Roberg KA, Carlson-Dakes KT, et al. Relationships among specific viral pathogens, virus-induced interleukin-8, and respiratory symptoms in infancy. Pediatr Allergy Immunol (2002) 13(6):386–93. 10.1034/j.1399-3038.2002.01093.x [DOI] [PubMed] [Google Scholar]
- 117.Martin TR, Ruzinski JT, Wilson CB, Skerrett SJ. Effects of endotoxin in the lungs of neonatal rats: age-dependent impairment of the inflammatory response. J Infect Dis (1995) 171(1):134–44. 10.1093/infdis/171.1.134 [DOI] [PubMed] [Google Scholar]
- 118.Martin TR, Rubens CE, Wilson CB. Lung antibacterial defense mechanisms in infant and adult rats: implications for the pathogenesis of group B streptococcal infections in the neonatal lung. J Infect Dis (1988) 157(1):91–100. 10.1093/infdis/157.1.91 [DOI] [PubMed] [Google Scholar]
- 119.McGrath-Morrow SA, Lee S, Gibbs K, Lopez A, Collaco JM, Neptune E, et al. Immune response to intrapharyngeal LPS in neonatal and juvenile mice. Am J Respir Cell Mol Biol (2015) 52(3):323–31. 10.1165/rcmb.2014-0100OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Anderson DC, Rothlein R, Marlin SD, Krater SS, Smith CW. Impaired transendothelial migration by neonatal neutrophils: abnormalities of Mac-1 (CD11b/CD18)-dependent adherence reactions. Blood (1990) 76(12):2613–21. [PubMed] [Google Scholar]
- 121.Harris MC, Shalit M, Southwick FS. Diminished actin polymerization by neutrophils from newborn infants. Pediatr Res (1993) 33(1):27–31. 10.1203/00006450-199301000-00006 [DOI] [PubMed] [Google Scholar]
- 122.Smith PK, Wang SZ, Dowling KD, Forsyth KD. Leucocyte populations in respiratory syncytial virus-induced bronchiolitis. J Paediatr Child Health (2001) 37(2):146–51. 10.1046/j.1440-1754.2001.00618.x [DOI] [PubMed] [Google Scholar]
- 123.McNamara PS, Ritson P, Selby A, Hart CA, Smyth RL. Bronchoalveolar lavage cellularity in infants with severe respiratory syncytial virus bronchiolitis. Arch Dis Child (2003) 88(10):922–6. 10.1136/adc.88.10.922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Abu-Harb M, Bell F, Finn A, Rao WH, Nixon L, Shale D, et al. IL-8 and neutrophil elastase levels in the respiratory tract of infants with RSV bronchiolitis. Eur Respir J (1999) 14(1):139–43. 10.1034/j.1399-3003.1999.14a23.x [DOI] [PubMed] [Google Scholar]
- 125.Everard ML, Swarbrick A, Wrightham M, McIntyre J, Dunkley C, James PD, et al. Analysis of cells obtained by bronchial lavage of infants with respiratory syncytial virus infection. Arch Dis Child (1994) 71(5):428–32. 10.1136/adc.71.5.428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Noah TL, Ivins SS, Murphy P, Kazachkova I, Moats-Staats B, Henderson FW. Chemokines and inflammation in the nasal passages of infants with respiratory syncytial virus bronchiolitis. Clin Immunol (2002) 104(1):86–95. 10.1006/clim.2002.5248 [DOI] [PubMed] [Google Scholar]
- 127.Nicholson EG, Schlegel C, Garofalo RP, Mehta R, Scheffler M, Mei M, et al. Robust cytokine and chemokine response in nasopharyngeal secretions: association with decreased severity in children with physician diagnosed bronchiolitis. J Infect Dis (2016) 214(4):649–55. 10.1093/infdis/jiw191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Garvy BA, Harmsen AG. Susceptibility to Pneumocystis carinii infection: host responses of neonatal mice from immune or naive mothers and of immune or naive adults. Infect Immun (1996) 64(10):3987–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Yamaguchi Y, Harker JA, Wang B, Openshaw PJ, Tregoning JS, Culley FJ. Preexposure to CpG protects against the delayed effects of neonatal respiratory syncytial virus infection. J Virol (2012) 86(19):10456–61. 10.1128/JVI.01082-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Yatsunenko T, Rey FE, Manary MJ, Trehan I, Dominguez-Bello MG, Contreras M, et al. Human gut microbiome viewed across age and geography. Nature (2012) 486(7402):222–7. 10.1038/nature11053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ege MJ, Bieli C, Frei R, van Strien RT, Riedler J, Ublagger E, et al. Prenatal farm exposure is related to the expression of receptors of the innate immunity and to atopic sensitization in school-age children. J Allergy Clin Immunol (2006) 117(4):817–23. 10.1016/j.jaci.2005.12.1307 [DOI] [PubMed] [Google Scholar]
- 132.Braun-Fahrländer C, Riedler J, Herz U, Eder W, Waser M, Grize L, et al. Environmental exposure to endotoxin and its relation to asthma in school-age children. N Engl J Med (2002) 347(12):869–77. 10.1056/NEJMoa020057 [DOI] [PubMed] [Google Scholar]
- 133.Stein MM, Hrusch CL, Gozdz J, Igartua C, Pivniouk V, Murray SE, et al. Innate immunity and asthma risk in amish and hutterite farm children. N Engl J Med (2016) 375(5):411–21. 10.1056/NEJMoa1508749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Schuijs MJ, Willart MA, Vergote K, Gras D, Deswarte K, Ege MJ, et al. Farm dust and endotoxin protect against allergy through A20 induction in lung epithelial cells. Science (2015) 349(6252):1106–10. 10.1126/science.aac6623 [DOI] [PubMed] [Google Scholar]
- 135.Schulfer A, Blaser MJ. Risks of antibiotic exposures early in life on the developing microbiome. PLoS Pathog (2015) 11(7):e1004903. 10.1371/journal.ppat.1004903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kramer BW, Kallapur S, Newnham J, Jobe AH. Prenatal inflammation and lung development. Semin Fetal Neonatal Med (2009) 14(1):2–7. 10.1016/j.siny.2008.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Warburton D, El-Hashash A, Carraro G, Tiozzo C, Sala F, Rogers O, et al. Lung organogenesis. Curr Top Dev Biol (2010) 90:73–158. 10.1016/S0070-2153(10)90003-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Blackwell TS, Hipps AN, Yamamoto Y, Han W, Barham WJ, Ostrowski MC, et al. NF-κB signaling in fetal lung macrophages disrupts airway morphogenesis. J Immunol (2011) 187(5):2740–7. 10.4049/jimmunol.1101495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Prince LS, Dieperink HI, Okoh VO, Fierro-Perez GA, Lallone RL. Toll-like receptor signaling inhibits structural development of the distal fetal mouse lung. Dev Dyn (2005) 233(2):553–61. 10.1002/dvdy.20362 [DOI] [PubMed] [Google Scholar]
- 140.Bry K, Whitsett JA, Lappalainen U. IL-1beta disrupts postnatal lung morphogenesis in the mouse. Am J Respir Cell Mol Biol (2007) 36(1):32–42. 10.1165/rcmb.2006-0116OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Whitsett JA, Haitchi HM, Maeda Y. Intersections between pulmonary development and disease. Am J Respir Crit Care Med (2011) 184(4):401–6. 10.1164/rccm.201103-0495PP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Wan H, Kaestner KH, Ang S-L, Ikegami M, Finkelman FD, Stahlman MT, et al. Foxa2 regulates alveolarization and goblet cell hyperplasia. Development (2004) 131(4):953–64. 10.1242/dev.00966 [DOI] [PubMed] [Google Scholar]
- 143.Jones CV, Williams TM, Walker KA, Dickinson H, Sakkal S, Rumballe BA, et al. M2 macrophage polarisation is associated with alveolar formation during postnatal lung development. Respir Res (2013) 14:41. 10.1186/1465-9921-14-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Tang X, Liu XJ, Tian C, Su Q, Lei Y, Wu Q, et al. Foxa2 regulates leukotrienes to inhibit Th2-mediated pulmonary inflammation. Am J Respir Cell Mol Biol (2013) 49(6):960–70. 10.1165/rcmb.2013-0122OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lambert L. Immunology of the Neonatal Lung and the Long Term Consequences of Neonatal Respiratory Virus Infection for Pulmonary Innate Immunity Ph.D. thesis, Imperial College London: (2015). [Google Scholar]