Abstract
We aimed to evaluate levels of amino-terminal pro-brain natriuretic peptid (NT-proBNP) in prediction of left ventricular ejection fraction (LVEF) in heart failure patients. Prospective study on 60 consecutive patients with symptoms and signs of heart failure was performed. Blood samples for NT-proBNP analysis was taken from all test subjects and echocardiography was also done in all of them. According to LVEF value, patients were divided into four groups; those with <30%, 31 to 39%, 40 to 49% and >50%. NT-proBNP values correlated with LVEF value. Regression analyis was used to evaluate how well NT-proBNP values predict LVEF. We used Receiver Operating Characteristic Curve calculation to evaluate diagnostic performance of NT-proBNP in estimation of LVEF. Average value of NT-proBNP in test group was 3191,69±642,89 pg/ml (p<0,001). Average value of NT-proBNP decreased with higher LVEF categories with significant (p<0,001) and high negative correlation (r = -0,75). Stepwise multivariate linear regression analysis showed that logarithmic value of NT-proBNP was excellent predictor of LVEF value (p<0,05). Model equation based on regression analysis was LVEF=88,645-15,311 x log (NT-proBNP). Predictive model for LVEF yielded from regression analysis had sensitivities of 98% and 81%, specificities of 20% and 90%, positive predictive values of 86% and 78% and negative predictive values of 67% and 92% for predicting patients with LVEF<50% and LVEF<40%, respectively. There was negative linear correlation between NT-proBNP and LVEF. NT-proBNP was excellent predictor of LVEF value (p<0,05).
Keywords: natriuretic peptides, heart failure, LVEF, prediction
INTRODUCTION
The clinical diagnosis of chronic heart failure syndrome in absence of left ventricle dysfunction (LVEF) is often insignificant, especially when there are no evident clinical symptoms (1). Echocardiography is routinely used method for confirmation of left ventricle systolic dysfunction. But, it is expensive; the doctors are not trained for this method and is often unavailable for outhospital patients. So, what would be the alternative to echocardiograph diagnostics of left ventricle dysfunction? The answer is natriuretic peptides and their use in routine practice should reduce the other diagnostic methods in cardiology, especially in outhospital patients. This study explores the possibilities of aminoterminal pro-brain natriuretic peptid (NT-proBNP) as noninvasive indicator of left ventricle dysfunction. The aims of the study were to correlate the levels of NT-proBNP and LVEF in patients with chronic heart failure and to test the sensitivity, specificity and accuracy of NT-proBNP as a predictor for LVEF.
PATIENTS AND METHODS
This study was conducted on 60 consecutive selected patients with symptoms and signs of heart failure hospitalized at the Department for Internal Diseases in University Clinical Center Tuzla. Excluded criteria were as follows: elderly patients (over 75 years of age) and clinically significant renal insufficiencies (plasma creatinin level >3,5mg/dl). All the patients were examined, history taken, as well as blood and urine tests, chest X-ray and electrocardiogram. Transthoracal, two-dimensional echocardiography was also done in order to calculate global systolic ventricular function through ejection fraction. Based on echocardiography maintained levels of LVEF, patients were divided into four groups: LVEF<30%, LVEF 31-39%, LVEF 40-49% and LVEF>50%. When the echocardiography measures were taken, there was no knowledge of serum levels of NT-proBNP. The blood from peripheral vein was taken to all patients 24 hours after the echocardiography. NTproBNP test for all samples was done on Dimension RL MAX (Dade Behring) and the technician did not know the values of LVEF. The values of NT-proBNP were re-checked in our laboratory using the blood of 27 healthy donors (normal value 125 pg/ml for patients under 75 years of age). Plasma level of NT-proBNP was correlated with the LVEF levels in all groups of patients.
RESULTS
The sample was consisted of 60 patients with mean age of 60,3±10,7 years. There were 40% of females i 60% of males. Average value of NT-proBNP was 3191,69±642,89 pg/ml (p<0,001) and average LVEF value was 41,3±13,4 %. We have found significant difference between LVEF categories in NT-proBNP levels (Table 1).
TABLE 1.
Average levels of NT-proBNP according to LVEF
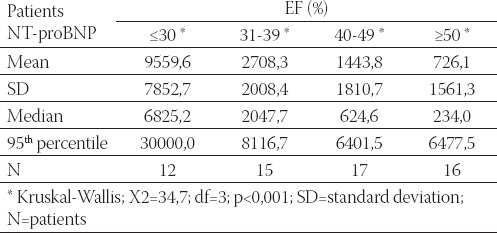
Pairwise comparison between LVEF categories demonstrated that NT-proBNP levels are decreasing from lower to higher LVEF values (p<0,001). Spearman’s rank order correlation showed significant and high negative correlation of ps= -0,75 between NT-proBNP and LVEF values. Graphical representation of NT-proBNP declining in categories with higher LVEF is depicted in Figure 1.
FIGURE 1.
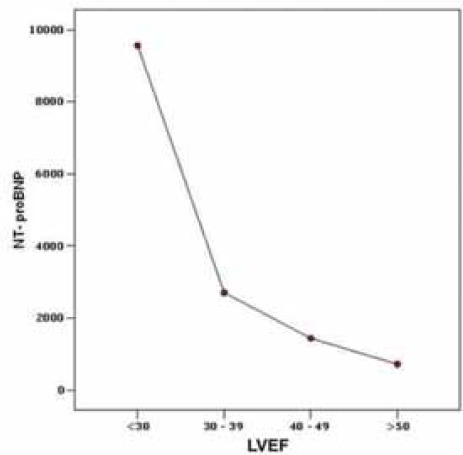
NT-proBNP Ievels according to LVEF categories
Total of 50 (83,3%) patients had LVEF<50% thus having echocardiographic criteria for systolic disfunction. Patients with EF<50% (3766,26±746,06) had significantly higher NT-proBNP levels than those with with EF>50% (318,82±69,78 pg/ml; p<0,001), as seen in Figure 2.
FIGURE 2.
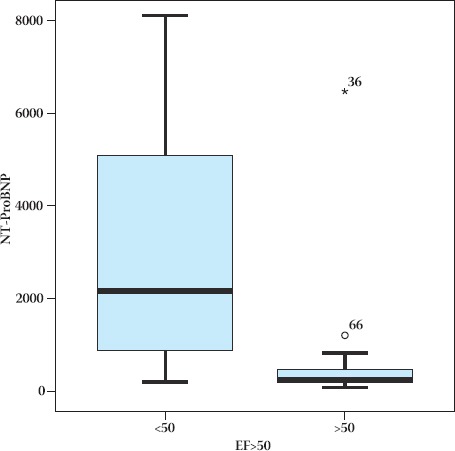
Difference in average NT-proBNP values between patients with LVEF<50% and patients with LVEF>50%
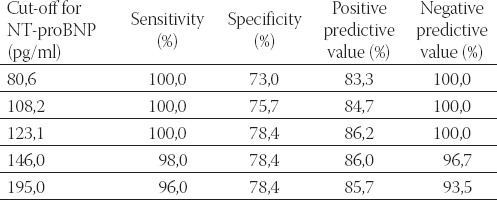
Receiver Operating Characteristics (ROC) curve evaluating diagnostic and predictive power of NT-proBNP in detection of patients with EF<50% is displayed in Figure 3. Area under the ROC curve (AUROC) was 0,96 (%95 CI=0,93-0,99; p<0,05). Best sensitivity and specificity values had threshold level of 123,1 pg/ml (Table 2).
FIGURE 3.

Receiver Operating Characteristics curve of diagnostic accuracy of NT-proBNP in detecting patients with EF<50%
TABLE 2.
Diagnostic accuracy for different cutt-off values of NT-proBNP in detection of patients with EF<50%
Receiver Operating Characteristics (ROC) curve evaluating diagnostic and predictive power of NT-proBNP in detection of patients with EF<40% is displayed in Figure 4. Area under the ROC curve (AUROC) was 0,94 (%95 CI=0,90-0,99; p<0,05). Best sensitivity and specificity values had threshold level of 841,8 pg/ml, with sensitivity of 100%, specificity of 85% and positive and negative predicitive values of 75% and 100%, respectivelly.
FIGURE 4.
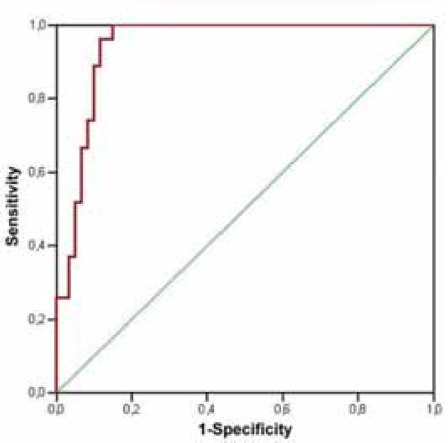
Receiver Operating Characteristics curve of diagnostic accuracy of NT-proBNP in detecting patients with EF<40%
We used stepwise linear regression analysis to evaluate impact of age, sex and NT-proBNP on LVEF value. Value of NT-proBNP due to its nonparametric nature was log-transformed. We have found that log NT-proBNP was significant predicive factor for EF value (B=-15,31; t=-7,87; df=58; p<0,001) Age and sex were not significant predictors of EF (p>0,05).
Using parameters gained through regression analysis we constructed predicitive model for prediciting LVEF based on NT-proBNP value. The equation gained was EF = 88,645 - 15,311 x log (NT-proBNP). This model was capable to predict EF values based solely on NT-proBNP with average difference of ±9,3 between observed and predicted values of EF. Correlation between observed and predicted values 0,72 (p>0,05) and is depicted in Figure 5.
FIGURE 5.
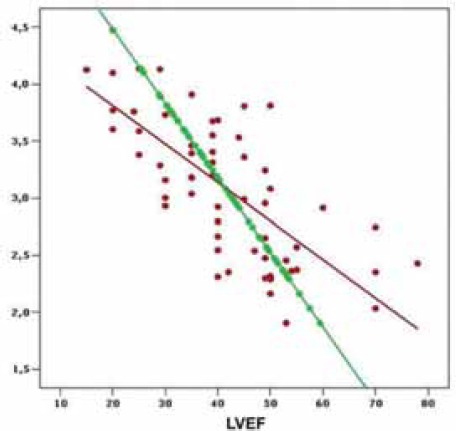
Correlation between observed (red) and predicted values (green) of EF (r=0,72; p<0,05)
DISCUSSION
The values of ejection fraction are being used as absolutely valid criteria for diagnosis of left ventricle systolic dysfunction in routine practice. The decrease of its values can be transient usually in “stunning” myocardium with spontaneous recovery after surgical bypass (2). The credibility of echocardiography evaluation of systolic dysfunction leaves no doubts. But, it is not always available as a screening method in general population. The determination of ventricle peptide substances significantly increases the diagnostic accuracy of heart failure and also helps in dividing the patients according to their symptoms (4). The American Cardiology Association and American Heart Association have given the instructions for use of natriuretic peptides in differentiation of dyspnea caused by heart failure or some other diseases (5). Our study has shown the neurohormonal activity with the significant increase of NT-proBNP plasma levels in patients with heart failure. Similar results are shown in many other studies (6, 7, 8, 9, 10, 11, 12). This study has correlated the plasma levels of NT-proBNP with the values of LVEF and significant negative linear correlation was the main result (p<0,001). 83,3% of examined patients had ejection fraction less than 50%, so they had the criteria for systolic dysfunction and their values of NT-proBNP were significantly higher comparing to the patients with EF>50% (p<0,001). Our results are comparable with the results of Januzi and al. (6), as well as with the results of other similar studies (12, 14, 15, 16, 17). Normal values of NT-proBNP practically exclude the diagnosis of left ventricle dysfunction. Border value of 123pg/ml is highly significant (87,5%) for detection of normal left ventricle function (EF>50%) and is comparable with the results of above quoted studies. Using the ROC curve for evaluation of NT-proBNP as a predictor of left ventricle systolic dysfunction (EF<50%), AUC value was 0,96 (0,95 CI 0,93-0,99; p<0,05). The best specificity and sensitivity ratio had the result of 123,1 pg/ml (100% and 78,4%), which is comparable with the results of other similar studies (17, 18, 19). Using NT-proBNP for detection of patients with EF<40%, AUC value was 0,94. The highest sensitivity was at the result of 841,8 pg/ml, with the sensitivity ratio of 100%. Hobbs et al. (13) used the border value of 40 pmol/l (336 pg/ml) for determining the EF<40% with the sensitivity ratio of 80% and 73% for specificity and AUC value was 76% with credibility of 95%. Bay et al. (20) used the increase of NT-proBNP value (>357 pmol/l) in identification of patients with EF<40% with sensitivity ratio of 73%, specificity ratio 82% and AUC 0,85. Using the parameters based on multivariate linear regression a predictive model was build in order to predict the values of EF. This model correctly predict up to 85% of patients with EF less than 50% and up to 87% of patients with EF less than 40%. Similar model has been used in many other studies on this topic (6, 7, 20, 21, 22). The above described model can be important in everyday practice because of its predictive power. Based on one laboratory parameter and a simple formula, it gives us the opportunity to evaluate the values of EF without echocardiography. Certainly, it is not sufficient as isolated, but it should be estimated together with the clinical findings and other tests.
CONCLUSION
The negative linear correlation exists between the serum levels of NT-proBNP and EFLV in patients with heart failure. The plasma level of NT-proBNP is a good predictor of EFLV.
List of Abbreviations
NT - proBNP - amino-terminal pro-brain natriuretic peptid
LVEF - left ventricular ejection fraction
ROC - Receiver Operating Characteristics
AUROC - Area under the ROC curve
REFERENCES
- 1.Omland T. N-Terminal ProBNP: Marker of Systolic Dysfunction or Nonspecific Indicator of Cardiac Disease? Heart Drug. 2003;3:122–124. [Google Scholar]
- 2.Struthers AD. The diagnosis of heart failure. Heart. 2000;84:334–338. doi: 10.1136/heart.84.3.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davie AP, Francis CM, Love MP, et al. Value of the electrocardiogram in identifyng heart failure duo to left ventricular systolic dysfunction. BMJ. 1996;312:222–225. doi: 10.1136/bmj.312.7025.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O’Donoughue M, Chen A, Baggish A, et al. NT-pro BNP is superior for the evaluation of patients with dyspnea and non-systolic congestive heart failure: A proBNP Investigation of Dyspnea in the Emergency Department (PRIDE) substudy. J. Am. Coll. Cardiol. 2005;45(suppl A):139A. [Google Scholar]
- 5.Januzi J, Camago C, Anwaruddin S, et al. The N-terminal Pro-BNP investigation of dyspnea in the emergency department (PRIDE) study. Am. J. Cardiol. 2002;95:948–954. doi: 10.1016/j.amjcard.2004.12.032. [DOI] [PubMed] [Google Scholar]
- 6.Januzzi JL, Kimmenade R, Lainchbury J, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilised heart failure: an international pooled analysis of 1256 patients. Eur. J. Heart. 2005;27:330–337. doi: 10.1093/eurheartj/ehi631. [DOI] [PubMed] [Google Scholar]
- 7.Rhidian JS, Andrew LC, Kevin G, et al. The diagnostic utility of N-terminal pro-B-type natriuretic peptide for the detection of major structural heart disease in patients with atrial fibrillation. Eur. J. Heart. 2006;27:2353–2361. doi: 10.1093/eurheartj/ehl233. [DOI] [PubMed] [Google Scholar]
- 8.Hammerer-Lercher A, Ludwig W, Falkensammer G, et al. Natriuretic peptides as marcers og mild forms of left ventricular dysfunction: efects of assays on diagnostic performance of markers. Clin. Chem. Lab. Med. 2004;50:1174–1183. doi: 10.1373/clinchem.2003.028316. [DOI] [PubMed] [Google Scholar]
- 9.Jacob VJ, Satya NG, Dhayakani S. Utility of N-Terminal ProBrain Natriuretic Peptide for the diagnosis of heart failure. Indian Heart J. 2003;55:35–39. [PubMed] [Google Scholar]
- 10.Tschöpe C, Kasner M, Westermann D, et al. The role of NTproBNP in the diagnostics of isolated diastolic dysfunction: corelation with echocardiographic and invasive measurements. Eur. J. Heart. 2005;26:2277–2284. doi: 10.1093/eurheartj/ehi406. [DOI] [PubMed] [Google Scholar]
- 11.McDonagh TA, Holmer S, Raymond I, et al. NT-proBNP and the diagnosis of heart failure: a pooled analysis of three European epidemiological studies. Eur. J. Heart. 2004;6:269–273. doi: 10.1016/j.ejheart.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 12.Redfield MM, Rodeheffer RJ, Jacobsen SJ, et al. Plasma brain natriuretic peptide concentration: impact of age and gender. J. Am. Coll. Cardiol. 2002;40:976–982. doi: 10.1016/s0735-1097(02)02059-4. [DOI] [PubMed] [Google Scholar]
- 13.Hobbs FD, Davis RC, Roalfe AK, et al. Reliability of N-terminal proBNP assay in diagnosis of left ventricular systolic dysfunction within representative and high risk populations. Heart. 2004;90(8):866–870. doi: 10.1136/hrt.2003.014258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gustafsson F, Badskjaer J, Hansen F, et al. Value of N-Terminal proBNP in the diagnosis of left ventrikular systolic dysfunction in primary care patients refered for cchocardiography. Heart Drug. 2003;3:141–146. [Google Scholar]
- 15.Wright SP, Doughty RN, Pearl A, et al. Plasma amino-terminal pro-brain natriuretic peptide and accuracy of heart-failure diagnosis in primary care: a randomized, controlled trial. J. Am. Coll. Cardiol. 2003;42:1793–1800. doi: 10.1016/j.jacc.2003.05.011. [DOI] [PubMed] [Google Scholar]
- 16.Groenning B, Raymond I, Hildebrandt P, et al. Diagnostic and prognostic evaluation of left ventricular systolic heart failure by plasma N-terminal pro-brain natriuretic peptide concentrations in a large sample of the general populattion. Heart. 2004;90:297–303. doi: 10.1136/hrt.2003.026021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Redfield MM, Rodeheffer RJ, Jacobsem SJ, et al. Plasma Brain Natriuretic Peptide to detect preclinical ventricular systolic or diastolic dysfunction. Circulation. 2004;109:3176–3181. doi: 10.1161/01.CIR.0000130845.38133.8F. [DOI] [PubMed] [Google Scholar]
- 18.Campbell DJ, Munir V, Hennessy OF, et al. Plasma amino terminal pro-brain natriuretic peptide levels in subjects presenting to the Emergency Department with suspected acute coronary syndrome: possible role in selecting patients for follow up. Intern. Med. 2001;31:211–219. doi: 10.1046/j.1445-5994.2001.00042.x. [DOI] [PubMed] [Google Scholar]
- 19.Mueller T, Gegenhuber A, Poelz W, Haltmayer M. Head-tohad comparison of the diagnostic utility of BNP and NT-proBNP in symptomatic and asymptomatic structural heart disease. Clin. Chim. Acta. 2004;341:41–48. doi: 10.1016/j.cccn.2003.10.027. [DOI] [PubMed] [Google Scholar]
- 20.Bay M, Kirk V, Parner J, et al. NT-proBNP: a new diagnostic screening tool to diferentiate between patients with normal and reduced left ventricular systolic function. Heart. 2003;89:150–154. doi: 10.1136/heart.89.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mueller T, Gegenhuber A, Poelz W, Haltmayer M. Diagnostic accuracy of B type natriuretic peptide and amino terminal proB-NP in the emergency diagnosis of heart failure. Heart. 2005;91:606–612. doi: 10.1136/hrt.2004.037762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clerico A, Prontera C, Emdin M, et al. Analytical performance and diagnostic accuracy for the measurement of Plasma B-Type Natriuretic Peptide(BNP) and N-Terminal proBNP. Clinical Chemistry. 2005;51:445–447. doi: 10.1373/clinchem.2004.038281. [DOI] [PubMed] [Google Scholar]
- 23.Juan CA, Amparo HM, Jose LD, et al. Value of NTproBNP concentration in an out-of-hospital adult population. Esp. Cardiol. 2003;56:236–244. doi: 10.1016/s0300-8932(03)76859-6. [DOI] [PubMed] [Google Scholar]


