Abstract
Objective
Adenomyosis and endometriosis are relatively common gynecological diseases that exhibit many common features. This study identified gynecological and non-gynecological diseases that exhibited comorbidity with adenomyosis and endometriosis in Korean women.
Methods
We used Health Insurance Review and Assessment data from 2009 to 2011 and searched for adenomyosis and endometriosis (coded as N80.1 and D25 in International Classification of Disease, 10th revision [ICD-10], respectively). We selected records from patients who had independent disease occurrences in each year, and comorbidities were estimated using Fisher's exact test. We computed each year's similarities and combined 3 years' results using Fisher's P-value summation method.
Results
A total of 61,516 patients' data were collected during the study period. The prevalence of adenomyosis and endometriosis were similar each year: 12.4% and 9.3% in 2009, 12.5% and 9.4% in 2010 and 13.3% and 9.1% in 2011, respectively. Meta-analysis revealed that 31 ICD-10 codes were significantly related with adenomyosis, and 44 ICD-10 codes were related with endometriosis. Gynecological diseases, such as leiomyoma and benign ovarian tumor, were significantly related to adenomyosis and endometriosis. Non-gynecological diseases, such as anemia and hypercholesterolemia, were also related to adenomyosis and endometriosis.
Conclusion
We must monitor for the presence of gynecological and non-gynecological diseases with co-morbidities during evaluations and follow-up of patients with adenomyosis or endometriosis.
Keywords: Adenomyosis, Anemia, Comorbidity, Endometriosis, Hypercholesterolemia
Introduction
Adenomyosis and endometriosis are relatively common gynecological disorders that are prevalent in reproductive aged women. The average age of symptomatic women with adenomyosis are generally older than 40 years, although it is occasionally noted in young women [1]. The prevalence of adenomyosis ranges from 5% to 70%, and the rate of diagnosis of adenomyosis during hysterectomy is approximately 20% to 30% [2]. Endometriosis occurs in approximately 10% of the general population, but it as high as 40% in infertile women and 30%–87% in women with chronic pelvic pain [1,3,4].
These 2 disease entities are similar pathologically because of the presence of endometrial glands outside the uterine endometrium [1]. Adenomyosis is defined as the presence of endometrial stroma and glands within the myometrium at least one low-power field from the basis of the endometrium. Endometriosis is also characterized by ectopic endometrium outside the uterus, generally within the peritoneal cavity, especially in the cul-de-sac, ovaries, pelvic visceral, or parietal peritoneum [1]. Symptomatically, these 2 diseases are also similar because the most common causes of chronic pelvic pain are adenomyosis and endometriosis. Therefore, the possibility of an inter-relationship between these 2 diseases was investigated. Leyendecker et al. [5] reported that the prevalence of endometriosis in adenomyosis was 80.6%, and the prevalence of adenomyosis in endometriosis was 91.1%.
Comorbidity is commonly understood as the coexistence of 2 or more diseases in the same individual. Comorbidity is most often defined in relation to a specific index condition [6], “Any distinct additional entity that has existed or may occur during the clinical course of a patient who has the index disease under study” [7]. Demonstration of disease comorbidity is important because comorbidity may provide additional information regarding the possible link between the diseases in molecular pathophysiology or causality. Comorbidity may also be used to identify other related diseases in patients with an index disease. Diseases would be expected to cluster in an individual if they shared a common pattern of influence or if the resilience or vulnerability of the individual was altered. For example, up to 75% of adults with diabetes also have hypertension [8]. Hypertension and diabetes are commonly intertwined conditions that share a significant overlap in underlying risk factors, including ethnicity, familial tendency, dyslipidemia, and lifestyle [8]. Another example of comorbidity is most chronic obstructive pulmonary disease patients have other chronic medical problems, including high blood pressure, hypercholesterolemia, heart disease, diabetes, osteoporosis, depression, and cancer [9].
There are several reports regarding the comorbidity of adenomyosis and endometriosis. Adenomyosis exhibits comorbidity with leiomyoma, endometrial hyperplasia, endometrial cancer, and breast cancer [10,11]. Endometriosis exhibits comorbidity with immunological disorders, such as rheumatoid arthritis, systemic lupus erythematosus, hypothyroidism, hyperthyroidism, and multiple sclerosis [12,13]. Therefore, the present study identified specific diseases or pathological conditions that were closely linked to adenomyosis and endometriosis by analyzing Korean Health Insurance Review and Assessment (HIRA) data from 2009 to 2011.
Materials and methods
1. Sources of data and data selection
Health care institutions (i.e., hospitals and clinics) ask the Korean national health insurance (International Classification of Disease, 10th revision [ICD-10]) service to pay for incurred medical expenses. HIRA reviews the ICD-10 claims, and the ICD-10 service reimburses the health care institutions for medical expenses. HIRA data were obtained from the payment claims form that is generated from each inpatient or outpatient visit to a health care institution. The HIRA data provides information on age, sex, diagnoses, therapeutic procedures, and prescribed drugs. Surrogate identification numbers replaced personal identifiers for research analyses to protect personal information. Researchers may combine data from multiple claims into a single entry for each patient. We filtered 3 years of HIRA data for adenomyosis and endometriosis (coded as N80.1 and D25 in ICD-10, respectively). We calculated the annual prevalence of adenomyosis and endometriosis from 2009 to 2011 and analyzed the presence of gynecological and non-gynecological diseases for comorbidity. We used the patient's management history for a more accurate determination of adenomyosis and endometriosis. We selected females who received gynecological ultrasonography for more confident diagnoses of the 2 diseases, and we confirmed adenomyosis and endometriosis using the diagnosis codes.
2. Statistics
We used Fisher's exact test to determine whether 2 diseases occurred independently. To compare a pair of diseases, 2 vectors containing the presence or absence of disease were obtained from the original data. One vector contained the presence/absence of the target disease (endometriosis or adenomyosis). The other vector contained information about the presence or absence of ICD code. A 2-by-2 table was constructed, and Fisher's test was applied. Odds ratio (OR) for disease comorbidity was estimated from the table.
We obtained 3 P-values from the 2009, 2010 and 2011 HIRA data after Fisher's exact tests. We applied the Fisher's P-value summation method for meta-analysis of the results of the 3-different data. As in equation X, P-values were summed.
Here, k indicates the number of P-values. The statistics were tested using χ2 distribution. All computations were performed in the R statistical program (R Foundation for Statistical Computing, Vienna, Austria; http://www.R-project.org/) [14].
Results
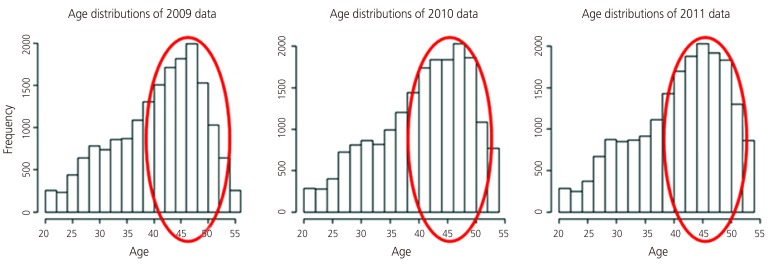
The HIRA data for 2009 to 2011 contained billing records of 3,417,841 patients from inpatient and outpatient clinics. We selected the data of 61,516 patients who received diagnosis codes based on gynecological ultrasonography. The study populations per year included 19,706 patients in 2009, 20,726 patients in 2010 and 21,084 patients in 2011. The prevalence of adenomyosis in the study populations were 12.4% in 2009, 12.5% in 2010 and 13.3% in 2011. The prevalence of endometriosis was 9.3% in 2009, 9.4% in 2010, and 9.1% in 2011. There were no significant differences in disease prevalence between the 3 consecutive study years (Table 1), and the prevalence of adenomyosis and endometriosis was similar to previous reports [1,7]. Adenomyosis and endometriosis were most prevalent in women in their forties and fifties during the study period, which was expected and consistent with previous reports (Fig. 1).
Table 1. Disease prevalence in the study population.
| Year | Adenomyosis (%) | Endometriosis (%) |
|---|---|---|
| 2009 | 12.4 | 9.3 |
| 2010 | 12.5 | 9.4 |
| 2011 | 13.3 | 9.1 |
Fig. 1.
Age distributions of adenomyosis, endometriosis, and benign ovarian tumor.
The number of patients diagnosed with these diseases in study group was approximately 4,000–5,000 per year. We analyzed the diagnostic codes that were entered in addition to adenomyosis or endometriosis, and 2,425 types of diseases existed in common with adenomyosis and endometriosis. Tables 2 and 3 list the diseases with significant comorbidity with adenomyosis. Dysmenorrhea (ICD-10 code N946) and female genital organs and menstrual cycle (ICD-10 code N948) revealed an OR over 1, which indicates a higher presence of these 2 codes (N946 and N948) in women with adenomyosis than women without adenomyosis. However, ICD-10 code D25.1 (intramural leiomyoma) and D25.0 (submucosal leiomyoma) revealed ORs less than 1, which indicates a low possibility of comorbidity with adenomyosis. Benign neoplasm of ovary (ICD-10 code D27) revealed an OR greater than 1 in 2009 but less than 1 in 2010 and 2011, which provides inconclusive results for the comorbidity of this condition with adenomyosis and endometriosis.
Table 2. Significant comorbidity with adenomyosis.
| ICD-10 code | 2009 | 2010 | 2011 | Meta P-value | |||
|---|---|---|---|---|---|---|---|
| OR | P-value | OR | P-value | OR | P-value | ||
| D27 | 2.2 | 1.38E-34 | 0.2 | 3.79E-123 | 0.2 | 1.33E-05 | 2.07E-281 |
| D251 | 0.2 | 9.84E-54 | 0.4 | 5.44E-37 | 0.4 | 6.67E-44 | 5.79E-109 |
| N946 | 2.8 | 2.97E-08 | 3.3 | 3.37E-27 | 3.4 | 1.72E-27 | 1.57E-75 |
| D250 | 0.1 | 1.09E-25 | 0.4 | 6.33E-19 | 0.3 | 8.13E-24 | 7.36E-68 |
| N948 | 3.0 | 0.004383 | 5.4 | 8.52E-12 | 7.1 | 1.07E-17 | 1.41E-39 |
ICD-10, International Classification of Disease, OR, odds ratio.
Table 3. Detail of comorbidity with adenomyosis.
| ICD-10 code | Name | Mean OR | P-value |
|---|---|---|---|
| C56 | Malignant neoplasm of ovary | 0.2 | 1.07E-06 |
| D25 | Leiomyoma of uterus | 0.3 | 7.85E-12 |
| D250 | Submucous leiomyoma of uterus | 0.3 | 7.82E-66 |
| D251 | Intramural leiomyoma of uterus | 0.3 | 7.04E-132 |
| D252 | Subserosal leiomyoma of uterus | 0.3 | 3.18E-21 |
| D259 | Leiomyoma of uterus, unspecified | 0.3 | <0.01 |
| D27 | Benign neoplasm of ovary | 0.9 | 1.52E-160 |
| D391 | Neoplasm of uncertain behavior of unspecified ovary | 0.8 | 2.19E-05 |
| D508 | Other iron deficiency anemias | 1.6 | 1.01E-11 |
| D509 | Iron deficiency anemia, unspecified | 1.4 | 5.40E-31 |
| D649 | Anemia, unspecified | 1.3 | 8.78E-15 |
| E780 | Pure hypercholesterolemia | 0.4 | 1.08E-04 |
| N72 | Inflammatory disease of cervix uteri | 1.1 | 2.95E-04 |
| N801 | Endometriosis of ovary | 0.7 | <0.01 |
| N803 | Endometriosis of pelvic peritoneum | 2.8 | 2.61E-18 |
| N830 | Follicular cyst of ovary | 1.3 | 2.80E-13 |
| N831 | Corpus luteum cyst | 1.1 | 2.71E-05 |
| N832 | Other and unspecified ovarian cysts | 1.9 | 2.84E-92 |
| N835 | Torsion of ovary, ovarian pedicle and fallopian tube | 0.5 | 2.99E-05 |
| N850 | Benign endometrial hyperplasia | 1.7 | 7.33E-15 |
| N851 | Other noninflammatory disorders of uterus, except cervix | 2.3 | 1.76E-07 |
| N852 | Hypertrophy of uterus | 5.5 | 2.94E-11 |
| N920 | Excessive and frequent menstruation with regular cycle | 1.8 | 1.12E-12 |
| N921 | Excessive and frequent menstruation with irregular cycle | 1.6 | 2.88E-06 |
| N938 | Other specified abnormal uterine and vaginal bleeding | 1.2 | 4.88E-18 |
| N939 | Abnormal uterine and vaginal bleeding, unspecified | 1.1 | 1.38E-15 |
| N944 | Primary dysmenorrhea | 3.2 | 1.38E-12 |
| N945 | Secondary dysmenorrhea | 3.3 | 2.76E-26 |
| N946 | Dysmenorrhea, unspecified | 3.2 | 2.31E-60 |
| N948 | Other specified conditions associated with female genital organs and menstrual cycle | 5.1 | 3.80E-30 |
| O800 | Encounter for full-term uncomplicated delivery | 0.4 | 4.90E-15 |
ICD-10, International Classification of Disease, 10th revision; OR, odds ratio.
The ORs for benign neoplasm of the ovary (ICD-10 code D27) and ovarian cyst (ICD-10 code N83.2) were greater than 1 for endometriosis, which was expected because most surgeries for endometriosis are for ovarian semisolid cystic masses. Preoperative imaging studies, such as ultrasonography or computed tomography, often suggest ovarian endometrioma. However, leiomyoma (ICD-10 codes D259 and D251) and submucosal leiomyoma (ICD-10 code D250) did not exhibit comorbidity with endometriosis with ORs less than 1. Tables 4 and 5 list 44 diseases that exhibited significant comorbidity with endometriosis.
Table 4. Significant comorbidity with endometriosis.
| ICD-10 code | 2009 | 2010 | 2011 | Meta P-value | |||
|---|---|---|---|---|---|---|---|
| OR | P-value | OR | P-value | OR | P-value | ||
| D259 | 0.2 | 1.75E-219 | 0.2 | 4.10E-257 | 0.1 | 2.72E-256 | 0 |
| D251 | 0.2 | 1.01E-70 | 0.2 | 2.53E-86 | 0.1 | 7.97E-110 | 3.79E-260 |
| D250 | 0.2 | 1.30E-30 | 0.2 | 2.24E-29 | 0.1 | 1.52E-37 | 1.08E-91 |
| D27 | 1.5 | 2.32E-14 | 1.6 | 4.06E-17 | 0.9 | 0.774509 | 1.81E-27 |
| N832 | 3.7 | 1.44E-63 | 4.4 | 1.34E-92 | 3.6 | 2.32E-63 | 5.63E-213 |
ICD-10, International Classification of Disease, OR, odds ratio.
Table 5. Detail of comorbidity with endometriosis.
| ICD-10 code | Name | Mean OR | P-value |
|---|---|---|---|
| M170 | Bilateral primary osteoarthritis of knee | 0.3 | 7.02E-17 |
| I10 | Primary hypertension | 0.4 | 3.28E-25 |
| D251 | Intramural leiomyoma of uterus | 0.2 | 5.67E-264 |
| D259 | Leiomyoma of uterus, unspecified | 0.2 | 0 |
| M511 | Thoracic, thoracolumbar and lumbosacral intervertebral disc disorders with radiculopathy | 0.6 | 4.03E-11 |
| N832 | Other and unspecified ovarian cysts | 3.9 | 1.13E-216 |
| N393 | Stress incontinence | 0.3 | 2.03E-13 |
| D27 | Benign neoplasm of ovary | 1.3 | 6.90E-30 |
| C73 | Malignant neoplasm of thyroid gland | 0.5 | 7.45E-11 |
| D509 | Iron deficiency anemia, unspecified | 0.5 | 5.70E-19 |
| B351 | Tinea unguium | 0.6 | 1.07E-07 |
| N736 | Female pelvic peritoneal adhesions | 4.7 | 7.71E-24 |
| M179 | Osteoarthritis of knee, unspecified | 0.4 | 1.41E-11 |
| D250 | Submucous leiomyoma of uterus | 0.2 | 7.42E-95 |
| M4806 | Spinal stenosis, lumbar region | 0.5 | 1.35E-06 |
| D252 | Subserosal leiomyoma of uterus | 0.3 | 4.10E-18 |
| E119 | Type 2 diabetes mellitus without complications | 0.4 | 1.07E-13 |
| R100 | Acute abdomen | 1.7 | 8.46E-10 |
| M171 | Unilateral primary osteoarthritis of knee | 0.3 | 3.39E-12 |
| N830 | Follicular cyst of ovary | 2.7 | 1.79E-16 |
| I119 | Hypertensive heart disease without heart failure | 0.3 | 2.24E-04 |
| N951 | Menopausal and female climacteric states | 0.4 | 3.65E-22 |
| E780 | Pure hypercholesterolemia | 0.4 | 9.00E-05 |
| R104 | Other and unspecified abdominal pain | 1.7 | 2.37E-09 |
| M750 | Adhesive capsulitis of shoulder | 0.5 | 7.41E-14 |
| N926 | Irregular menstruation, unspecified | 1.9 | 1.18E-08 |
| N952 | Postmenopausal atrophic vaginitis | 0.3 | 8.50E-08 |
| O200 | Threatened abortion | 1.9 | 1.77E-06 |
| N979 | Female infertility, unspecified | 3.7 | 6.08E-62 |
| A099 | Infectious gastroenteritis and colitis, unspecified | 1.4 | 7.58E-08 |
| D25 | Leiomyoma of uterus | 0.3 | 1.17E-15 |
| E782 | Mixed hyperlipidemia | 0.3 | 1.77E-06 |
| N978 | Female infertility of other origin | 4.0 | 6.00E-43 |
| R103 | Right lower quadrant pain | 2.0 | 5.57E-10 |
| N970 | Female infertility associated with anovulation | 3.2 | 1.05E-27 |
| E785 | Hyperlipidemia, unspecified | 0.4 | 1.94E-09 |
| K011 | Impacted teeth | 4.6 | 4.23E-15 |
| N959 | Unspecified menopausal and perimenopausal disorder | 0.4 | 3.08E-08 |
| N946 | Dysmenorrhea, unspecified | 2.9 | 1.05E-42 |
| H360 | Retinal disorders in diseases classified elsewhere | 0.5 | 1.52E-05 |
| E118 | Type 2 diabetes mellitus with unspecified complications | 0.1 | 9.08E-07 |
| L701 | Acne conglobata | 5.1 | 3.77E-10 |
| R102 | Pelvic and perineal pain | 1.8 | 8.29E-08 |
| N948 | Other specified conditions associated with female genital organs and menstrual cycle | 7.1 | 4.36E-34 |
| N831 | Corpus luteum cyst | 2.6 | 1.15E-11 |
| N944 | Primary dysmenorrhea | 3.0 | 1.95E-10 |
| N945 | Secondary dysmenorrhea | 2.3 | 1.46E-09 |
| N971 | Female infertility of tubal origin | 3.2 | 2.29E-12 |
ICD-10, International Classification of Disease, OR, odds ratio.
Meta-analysis revealed that adenomyosis correlated with 31 ICD-10 codes, and endometriosis was correlated with 44 ICD-10 codes. Uterine leiomyoma is the most common uterine benign tumor, and it was commonly related with benign ovarian tumor in previous studies [15]. However, uterine myoma was not related with adenomyosis or endometriosis in our study. Anemia, hypercholesterolemia and hyperlipidemia were significantly associated with adenomyosis and endometriosis. The P-value of the meta-analysis of 3 independent datasets was highly significant (mean OR, 0.4; P=1.11E-05), which indicates that hypercholesterolemia tended to occur in women without adenomyosis. Anemia also exhibited highly significant comorbidity with these 2 diseases. Iron deficiency anemia (D509) was more prevalent in the adenomyosis group (mean OR, 1.4; P=5.40E-31) However, D509 was less prevalent in the endometriosis group (mean OR, 0.5; P=5.70E-19). Hypercholesterolemia and hyperlipidemia exhibited low but significant comorbidity with adenomyosis and endometriosis (Tables 2, 3, 4, 5).
Discussion
Gynecological diseases, such as uterine myoma and benign ovarian tumor, and non-gynecological diseases, such as anemia and hypercholesterolemia, were significantly related with the diagnoses of adenomyosis and endometriosis in 61,516 Korean female patients across 3 years of HIRA data. Previous studies suggested a comorbidity relationship between adenomyosis/endometriosis and other diseases, but the results of these studies were not consistent [16]. Various studies reported the coexistence of adenomyosis and leiomyomas in the same uterus. Taran et al. [11] reported that the incidence of concomitant adenomyosis in hysterectomy specimens of women with leiomyomas was between 15% and 57% [12,13].
Endometriosis is associated with a higher risk of cutaneous melanoma [16], diabetes mellitus, pelvic inflammatory disease, cardiovascular diseases, chronic liver diseases, rheumatic disease, hypertension, hyperlipidemia, and depression [17].
The present study found significant comorbidity of diseases with adenomyosis and endometriosis. Anemia was easily anticipated as a comorbid disease of adenomyosis because menorrhagia is one of the primary symptoms. The comorbidity of leiomyoma may be explained by the high prevalence of this disease in reproductive-aged women. A recent retrospective study reported that 87.1% of patients with a chief concern of symptomatic fibroids who complained of abnormal uterine bleeding also had a diagnosis of histology-proven endometriosis [15]. These authors reinforced the need for a concomitant diagnosis and intraoperative treatment of both conditions and warned against overlooking the presence of endometriosis and preventing the persistence of pelvic pain after surgery for the symptomatic leiomyoma [15]. The current literature reports an incidence of concomitant fibroids and endometriosis ranging between 12% and 20%, based on 2 previously published studies of over 3,600 patients and 605 participants, respectively [18,19].
However, hypercholesterolemia and hyperlipidemia are newly discovered non-gynecological diseases that exhibited comorbidity with adenomyosis and endometriosis in the present study. The correlation was not strong, which may partially reflect the age factor because of the high prevalence of adenomyosis and endometriosis in women in their forties. Recent evidence also suggests higher serum levels of low-density lipoprotein in women with endometriosis [20]. The possibility of an increased risk of cardiovascular diseases in endometriosis patients was recently reported, and endometriosis and coronary heart disease may share a common genetic background [21]. The findings of this study support the possible increased risk of cardiovascular disease in endometriosis based on the comorbidity data.
There are several limitations in this study. This study was based on HIRA data, and we analyzed disease codes that were entered to the HIRA database when the clinicians examined their patients at an outpatient clinic and pathological confirmation was not always obtained. The diagnosis was generally made on the basis of physical examination and imaging studies, such as transvaginal ultrasonography or pelvic magnetic resonance imaging. Most diagnoses were made clinically, not pathologically. Therefore, there is the possibility of omitting or adding incorrect disease codes. Another inherent limitation was that the data evaluation relied solely on the electronic data interchange code input of individual hospitals, and the integrity of the information in the registry may vary between hospitals.
However, these limitations do not decrease the significance because of the large dataset analyzed. Analyses of big datasets offer the possibility to discover new insights about our approach to disease using a low-cost method and high volume of data. Cross-sectional studies of large datasets enable immediate feedback on new correlations or trends. Therefore, the potential benefits outweigh the countervailing limitations. To the best of our knowledge, this report is the first epidemiological study to report the nationwide incidence of adenomyosis and endometriosis in East Asia. The etiology and pathophysiology of adenomyosis and endometriosis and their interrelationship are not fully understood, but the present study has clinical significance. The results provide a novel view to assess diseases that may be used in the diagnosis or treatment plan via application to a checklist of criteria.
In conclusion, gynecological diseases, such as uterine myoma and benign ovarian tumor, and non-gynecological diseases, such as anemia and hypercholesterolemia, were comorbid with adenomyosis and endometriosis in Korean women. We must pay attention to the presence of these comorbid diseases in the diagnosis and follow-up of patients with adenomyosis and endometriosis.
Acknowledgements
This study was supported by a research grant from the National Research Foundation of Korea (NRF-2015R1C1A1A02038010).
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Rapkin AJ, Nathan L. Pelvic pain and dysmenorrhea. In: Berek JS, Novak E, editors. Berek & Novak's gynecology. 15th ed. Philadelphia (PA): Lippincott Williams & Wilkins; 2012. pp. 470–504. [Google Scholar]
- 2.Garcia L, Isaacson K. Adenomyosis: review of the literature. J Minim Invasive Gynecol. 2011;18:428–437. doi: 10.1016/j.jmig.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 3.Hemmings R, Rivard M, Olive DL, Poliquin-Fleury J, Gagné D, Hugo P, et al. Evaluation of risk factors associated with endometriosis. Fertil Steril. 2004;81:1513–1521. doi: 10.1016/j.fertnstert.2003.10.038. [DOI] [PubMed] [Google Scholar]
- 4.Renner SP, Strick R, Fasching PA, Oeser S, Oppelt P, Mueller A, et al. Single nucleotide polymorphisms in the progesterone receptor gene and association with uterine leiomyoma tumor characteristics and disease risk. Am J Obstet Gynecol. 2008;199:648.e1–648.e9. doi: 10.1016/j.ajog.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Leyendecker G, Bilgicyildirim A, Inacker M, Stalf T, Huppert P, Mall G, et al. Adenomyosis and endometriosis. Re-visiting their association and further insights into the mechanisms of auto-traumatisation. An MRI study. Arch Gynecol Obstet. 2015;291:917–932. doi: 10.1007/s00404-014-3437-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van den Akker M, Buntinx F, Metsemakers JF, Roos S, Knottnerus JA. Multimorbidity in general practice: prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol. 1998;51:367–375. doi: 10.1016/s0895-4356(97)00306-5. [DOI] [PubMed] [Google Scholar]
- 7.Feinstein AR. The pre-therapeutic classification of co-morbidity in chronic disease. J Chronic Dis. 1970;23:455–468. doi: 10.1016/0021-9681(70)90054-8. [DOI] [PubMed] [Google Scholar]
- 8.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 9.Long AN, Dagogo-Jack S. Comorbidities of diabetes and hypertension: mechanisms and approach to target organ protection. J Clin Hypertens (Greenwich) 2011;13:244–251. doi: 10.1111/j.1751-7176.2011.00434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vercellini P, Viganò P, Somigliana E, Daguati R, Abbiati A, Fedele L. Adenomyosis: epidemiological factors. Best Pract Res Clin Obstet Gynaecol. 2006;20:465–477. doi: 10.1016/j.bpobgyn.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 11.Taran FA, Stewart EA, Brucker S. Adenomyosis: epidemiology, risk factors, clinical phenotype and surgical and interventional alternatives to hysterectomy. Geburtshilfe Frauenheilkd. 2013;73:924–931. doi: 10.1055/s-0033-1350840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matalliotakis IM, Cakmak H, Fragouli YG, Goumenou AG, Mahutte NG, Arici A. Epidemiological characteristics in women with and without endometriosis in the Yale series. Arch Gynecol Obstet. 2008;277:389–393. doi: 10.1007/s00404-007-0479-1. [DOI] [PubMed] [Google Scholar]
- 13.McLeod BS, Retzloff MG. Epidemiology of endometriosis: an assessment of risk factors. Clin Obstet Gynecol. 2010;53:389–396. doi: 10.1097/GRF.0b013e3181db7bde. [DOI] [PubMed] [Google Scholar]
- 14.R Development Core Team (AT) R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2011. [Google Scholar]
- 15.Nezhat C, Li A, Abed S, Balassiano E, Soliemannjad R, Nezhat A, et al. Strong association between endometriosis and symptomatic leiomyomas. JSLS. 2016;20:e2016. doi: 10.4293/JSLS.2016.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kvaskoff M, Han J, Qureshi AA, Missmer SA. Pigmentary traits, family history of melanoma and the risk of endometriosis: a cohort study of US women. Int J Epidemiol. 2014;43:255–263. doi: 10.1093/ije/dyt235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teng SW, Horng HC, Ho CH, Yen MS, Chao HT, Wang PH, et al. Women with endometriosis have higher comorbidities: analysis of domestic data in Taiwan. J Chin Med Assoc. 2016;79:577–582. doi: 10.1016/j.jcma.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 18.Fuldeore M, Yang H, Du EX, Soliman AM, Wu EQ, Winkel C. Healthcare utilization and costs in women diagnosed with endometriosis before and after diagnosis: a longitudinal analysis of claims databases. Fertil Steril. 2015;103:163–171. doi: 10.1016/j.fertnstert.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 19.Uimari O, Järvelä I, Ryynänen M. Do symptomatic endometriosis and uterine fibroids appear together? J Hum Reprod Sci. 2011;4:34–38. doi: 10.4103/0974-1208.82358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Melo AS, Rosa-e-Silva JC, Rosa-e-Silva AC, Poli-Neto OB, Ferriani RA, Vieira CS. Unfavorable lipid profile in women with endometriosis. Fertil Steril. 2010;93:2433–2436. doi: 10.1016/j.fertnstert.2009.08.043. [DOI] [PubMed] [Google Scholar]
- 21.Kvaskoff M, Mu F, Terry KL, Harris HR, Poole EM, Farland L, et al. Endometriosis: a high-risk population for major chronic diseases? Hum Reprod Update. 2015;21:500–516. doi: 10.1093/humupd/dmv013. [DOI] [PMC free article] [PubMed] [Google Scholar]