Abstract
An. culicifacies is the major vector of malaria in tribal community and tribal dominated areas in India. Development of resistance to insecticides is the major challenge to curb the transmission. Gadchiroli (Maharashtra) is a tribal district in central India where incidence of malaria increased from 2012 to 2015 despite indoor space spray with synthetic pyrethroids. To determine the susceptibility status of An. culicifacies against commonly used insecticides in public health program in Gadchiroli. standard WHO method and test kit were used. The insecticide impregnated papers were procured from vector control unit Malaysia. An. culicifacies found resistance to three major groups of pesticides i.e. organochlorine (DDT 4%), organophosphorous (Malathion 5%) and pyrethroids (Cyfluthrin 0.15%, Deltametherin 0.05% and Lambdacyhalothrin 0.05%). The susceptibility status in Permethrin 0.75% needs further confirmation. Development of resistance to different insecticides of varied groups is an adverse finding for the elimination of malaria, explaining the recent increase in malaria incidence in Gadchiroli. The phenomenon further needs to be studied in different locations and the susceptibility needs to test against other insecticides. The findings may have significant implications to the choice of insecticides in the malaria control program in tribal areas.
Keywords: An. culicifacies, insecticide resistance, malaria vector, Gadchiroli
Introduction
Malaria is a major public health challenge in India despite serious efforts to tackle the transmission at national and international level. Though malaria morbidity and mortality has been halved between 2003 and 2014, World Health Organization (WHO) estimated, 214 million malaria cases with 438,000 deaths globally while in India around 1.17 million malaria cases and 384 deaths reported in 2015 [1]. Nearly 104 million populations belong to ethnic tribe in India living in extreme situation [2]. Eighty percent of the 1.1 million malaria cases in India were contributed by 20% population of India, in which tribal population is dominant [3]. Hence, the malaria control in tribal area remains key element to eliminate malaria from India. Gadchiroli (Maharashtra) is a tribal district in central India having 0.95% of the state’s population. In the year 2015, this district reported 60% of total malaria cases and 87% total falciparum cases of the states [4]. Malaria burden in Gadchiroli district represent the gravity of malaria situation in tribal areas of India. The district reported 6436 malaria cases in 2013 which increased to 24,469 in 2014 and subsequently to 34,206 in 2015 [5]. An. culicifacies and An. fluviatilis are the two main vector prevalent in the district [6,7]. An. culicifacies is the predominant anopheline species which is prevalent throughout the year while An. fluviatilis found in winter. An. culicifacies is the complex of sibling species and species B and C are prevalent sibling species. Species C is predominant species(8%) and known malaria vector while species B is only about 15% and non vector [6]. Insecticide residual spray (IRS) remained as important tool for reducing vector population and transmission of the disease since 1958. In 1998, the synthetic pyrethroids were introduced in IRS on pilot basis and after 2008 these are insecticides mainly use to prevent malaria transmission. In Gadchiroli deltamethrin was used in IRS since 1998 [6], Alphcypermethrin, Cyfluthrin and Lambda-cyhalothrin (newer pyrethroids) were used after 2009. Along with IRS, the Insecticide Treated Net (ITN) and Long-Lasting Insecticide Treated Nets (LLINs) were distributed in few selected areas of Gadchiroli which also contains synthetic pyrethroid [5]. Since the malaria incidence has been increased despite malaria control activity, particularly with IRS using synthetic pyrethroid it was necessary to monitor the vector population particularly An. culicifacies for its susceptibility status against the commonly used insecticides.
Material and methods
Study setting
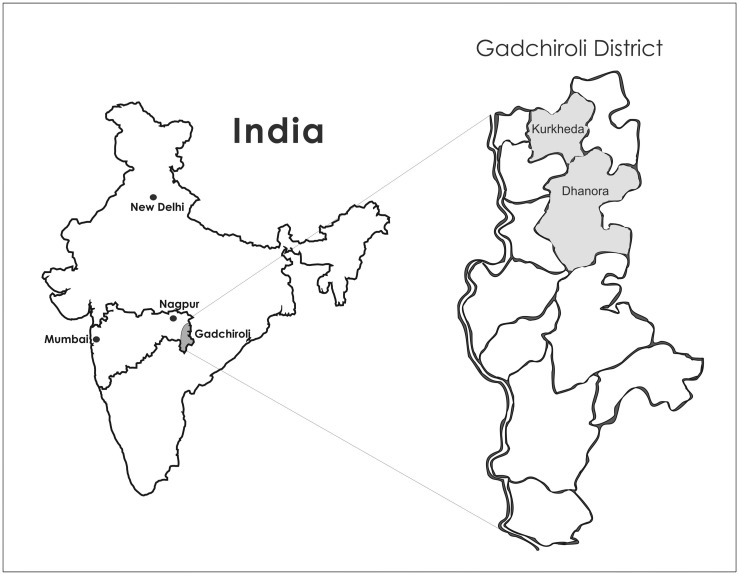
Gadchiroli district was created in 1982 after separation from Chandarpur district. The district is spread over in 14,412 sq. km. having a population of 10,72,942. With 78% of the surface under forest covered, 39% population being tribal, it is the most backward districts in the state. The district is divided in 12 talukas. Gond is the main tribe along with Rajgond, Madia and Pardhan. The tribal people in this district live in forested areas and their livelihood depends upon farming, gathering forest produce such as bamboo, leaves, and medicinal herbs. The area is infested with left wing extremism [8]. The study was carried out in the villages of two blocks of Gadchiroli district- Dhanora, Kurkheda (Refer Figure 1). The susceptibility status of An. culicifacies was monitored in August 2016 and February 2017 against different insecticides being used in public health program for control of malaria.
Figure 1.
Map of India, Maharashtra showing study sites.
Mosquito collections
The mosquitoes were collected by standard hand catch method using torch and aspirator in the morning hours between 6.00 am and 9.00 am from cattle sheds and human dwelling and brought in clothes cage to the base camp. Mosquitoes were brought to base camp and segregated to species level and further to different abdominal conditions of the vector species.
Susceptibility status
The susceptibility status was determined using standard WHO method [9]. The impregnated papers (test kit) of different insecticide were procured from vector control unit Malaysia (a unit of WHO). For determining the susceptibility status, only wild caught fully fed specimens of Anopheles culicifacies were used. The fully fed specimen of An. culicifacies were exposed to insecticide paper for one hour in experimental tubes and then transferred to holding tubes for 24 h. In each experimental (exposed) tube 10 to 20 mosquitoes were exposed. Two to three replicates were kept for each insecticide in experiment. One to two replicate of control were also kept similar to experimental tubes. During the holding period of 24 h, mosquitoes were provided glucose cotton padding. The mortality in holding tubes was recorded after 24 h. The experiment was discarded if mortality in control tubes was 20% or more. If the mortality in control was less than 5%, then the control mortality was ignored. Experimental mortality was corrected using abbott formula [10] if mortality in control ranged from 5 to 20%.
Results
The result of susceptibility test is summarized in Table 1. As per the WHO criteria (2016), Confirmed resistance (R) refers to mortality <90%, 90–97% as possible resistance (PR) and ≥98% as susceptible (S). The corrected mortality rate was 37.1% for DDT 4%, 59.9% for Lambda Cyhalothrin 0.05%, 70.2% for Cyfluthrin 0.15%, 74% for Malathion 5%, 83.8% for Deltametherin 0.05% and 91.3% for Permethrin 0.75%. (Table 1). An. culicifacies found resistance to three major groups of pesticides i.e. organochlorine (DDT 4%), organphosphorous (Malathion 5%) and pyrethroids (Cyfluthrin 0.15% and Lambda cyhalothrin 0.05%). There is possible resistance in Permethrin 0.75% which needs to be confirmed from the repeat test. The susceptibility status report has been shared with Joint director Malaria, Govt. of Maharashtra and director National Vector Borne Disease Control Programme (NVBDCP), India.
Table 1.
Susceptibility status of An. culicifacies against different insecticides following WHO methods* (2016) in Gadchiroli, Maharashtra, western India
| Diagnostic insecticide dose on impregnated papers | Mosquitoes exposed (n) | Dead mosquitoes after 24 h of exposure (n) | Mortality after 24 h of exposure | Corrected mortality | Susceptibility status# | |||
|---|---|---|---|---|---|---|---|---|
| Expt | Cont | Expt | Cont | Expt % (95% CI) | % Cont (95% CI) | % (95% CI) | ||
| August 2016 | ||||||||
| DDT 4% | 80 | 35 | 34 | 3 | 42.5 (31.5–54.1) | 8.6 (1.8–23.1) | 37.1 (27.5–47.2) | R |
| Lambda Cyhalothrin 0.05% | 160 | 105 | 102 | 10 | 63.7 (55.8–71.2) | 9.5 (4.7–16.8) | 59.9 (49.7–69.7) | R |
| Cyfluthrin 0.15% | 100 | 105 | 73 | 10 | 73.0 (63.2–81.4) | 9.5 (4.7–16.8) | 70.2 (60.0–78.7) | R |
| Malathion 5% | 80 | 35 | 61 | 3 | 76.3 (65.4–85.1) | 8.6 (1.8–23.1) | 74 (64.3–82.2) | R |
| Deltametherin 0.05% | 125 | 55 | 107 | 6 | 85.6 (78.2–91.2) | 10.9 (4.1–22.2) | 83.8 (75.3–90.6) | R |
| Permethrin 0.75% | 90 | 55 | 83 | 6 | 92.2 (84.6–96.8) | 10.9 (4.1 −22.2) | 91.3 (83.6–95.8) | PR |
Supplied by WHO
S – Susceptible (mortality ≥ 98%); R – Confirmed resistance (mortality < 90%); PR – Possible Resistance (mortality 90–97%).
Discussion
An. culicifacies is the most common vector which is responsible for 70% of the malaria transmission in India and has a vital role causing forest malaria [11]. It is an important vector in tribal setting except certain parts of Odisha and northeastern states of India. Major malaria epidemics are caused by An. culicifaices either alone or along with An. fluviatilis and An. stephensi [12]. In Gadchiroli, the most common vector for malaria is An. culicifacies though other vector An. fluviatilis is also prevalent in very less proportion. Vector management is the backbone of Indian malaria control program. Since insecticides are used in different formulations and in different mode for management of vectors, development of insecticide resistance in malaria vectors is a major barrier for achieving effective vector control. The IRS was begun with DDT in the early fifties of the last century and had impressive impact in reducing malaria incidence. Due to selection pressure, An. culicifacies developed resistance in 1959 after fifteen years of its use [13]. DDT resistance was one of the important causes for the malaria control program setback which occurred after 1962. Organophosphorous (malathion) group was introduced in 1969 in IRS. The resistance to malathion was reported after four years of use from Gujarat [14]. Synthetic pyrethroid (deltamethrin) pressed into service as IRS in 1996. Synthetic pyrethroids are used in IRS, impregnation of bed nets and making Long-Lasting Insecticidal Treated Nets (LLINs) as it is safe for human and the non-targeted organism.
An. culicifacies showed the first indication of resistance to pyrethroid (deltamethrin) in 2002 in Surat district, Gujarat, India [15]. In the present study, An. culicifacies found to resistant to six insecticides (DDT 4%, Malathion 5%, Deltametherin 0.05%, Lambdacyhalothrin 0.05% and Cyfluthrin 0.15%) of three groups (organochlorine, organphosphorous and pyrethroids). Probably this is the first documentation of multiple insecticide resistance in An. culicifacies from Maharashtra state, India. Similar results have been documented earlier in other parts of India and abroad. Earlier resistance of An. culicifacies to three insecticides (DDT 4%, Malathion 5% and Deltamethrin 0.05%) of three groups (organochlorine, organphosphorous and pyrethroid) were reported in Madhya Pradesh, central India [16] and in Odisha, northeastern of India [17]. Multiple insecticide resistance has been reported in An. gambiae [18,19], in An. funestus [20], in An. arabiensis [21] and in An. coluzzi [22] from different parts of Africa. In Gadchiroli, pyrethroids are used in indoor residual spraying (IRS) from 1998 since today [6]. An. culicifacies was fully susceptible to deltameherine (mortality-100%) till 2002 but tolerant (verification required) to malathion (mortality – 92.9%) and resistant to DDT 4% (mortality – 51%) (6). In 2010, the species was reported resistant to DDT 4% (mortality – 23.2%), tolerant (verification required) to Malathion 5% (mortality – 96%) and susceptible to Deltametherin [7] 0.05% which changed to tolerant (mortality-94%) in the present study. In, the current study, the An. culicifacies found in Gadchiroli are resistant not only to above three -insecticides but also to Lambda cyhalothrin 0.05%, Cyfluthrin 0.15%, and tolerant to Permethrin 0.75% . Deltametherin has been continuously used in malaria program in Gadchiroli since last many years either in IRS or ITN or LLIN. These above studies explain how resistance in An. culicifacies has developed against pyrethroid (Deltamethrin 0.05%) gradually over time due to selection pressure. The resistance development in Malathion over the time can be explained by its large scale use in agriculture. The corrected mortality for Permethrin 0.75% was 91.6% that needs repeat test for its confirmation. Though permethrin is also a pyrethroid but never been used in Gadchiroli ever before. In the beginning of 2016, LLIN containing Permethrin (Olyset brand) have been distributed. Probably exposure to these LLIN may explain above findings.
The current study shows pyrethroid resistance, is a major threat for the malaria control program, as it is being extensively used for IRS and nets (ITN/LLIN) in India. The country has targeted to eliminate malaria by 2030, in view of this -the finding of this study is significant. Rational and judicious use of insecticides with rotation is key to avoid or dilute resistance and control vectors in malaria. Periodic monitoring of the susceptibility status to guide insecticide for vector control measures is essential. There is an urgent need to find out alternate insecticides for IRS. In this local context, the susceptibility needs to be tested against other insecticides of synthetic pyrethroid (Bifenithron & Alpha-Cypermethrin) which is approved by National Vector Borne Disease Control Program, India for IRS. Bifenithron (synthetic pyrethroid) which not used before in Gadchiroli may be useful option after ruling out cross-resistance.
Conclusion
An. culicifacies found in Gadchiroli are resistance to three major groups of insecticides i.e. organochlorine (DDT 4%), organphosphorous (Malathion 5%) and pyrethroids (Deltametherin 0.05%, Cyfluthrin 0.15% and Lambda cyhalothrin0.05%). This is an adverse finding for the elimination of malaria, explaining the recent increase in malaria incidence in Gadchiroli. Therefore, the selection of insecticides for spraying (IRS) needs to be chosen with caution and effort should be taken to develop and apply effective insecticide resistance management strategies. The phenomenon needs to be further studied in different locations and the susceptibility needs to be tested against other insecticides. The findings may have significant implications to the choice of insecticides in the malaria control program in tribal areas.
Disclosure statement
No potential conflict of interest was reported by the authors.
Funding
This work was supported by the Indian Council of Medical Research, New Delhi and the Tata Trusts Mumbai.
Acknowledgment
We specially thank Dr Kanchan Jagtap (Joint director, Govt. of Maharashtra), Dr. Mahendra Jagtap (State Entomologist, Govt. of Maharashtra) and Dr S. J. Pande (District malaria officer, Gadchiroli) and Mr Rajesh Karlekar (VBD consultant, Gadchiroli) for their sincere co-operation in the study. We would like to thank Sh. Dhan Singh, Sh. S.B. Dubey, Sh. S.R. Mishra, Sh. B.S. Patel (NIRTH field staff) and Mr Mahadhev Satpute, Mr Haridas Sakere, Mr Najuk Jade, Mrs. Deola and Mr Anandrao Dudhabale (SEARCH field staff) for their support in the field. We thank Dr Anand Bang of the Tata Trusts for facilitating the support.
References
- [1].WHO World Malaria Report 2015 [Internet]. WHO; [cited 2017 Jun 13]]. Available from: https://www.who.int/malaria/publications/world-malaria-report-2015/report/en/ [Google Scholar]
- [2].Registrar General and Census Commissioner of India, Census of India 2011 Available from: https://www.censusindia.gov.in.
- [3]. Available from: https://www.who.int/features/2015/india-programme-end-malaria/en/
- [4].Malaria-situation-April17.pdf [Internet]; [cited 2017 Jun 14]. Available from: https://nvbdcp.gov.in/Doc/malaria-situation-April17.pdf
- [5].Office of District Malaria Office , Gadchiroli, Maharshtra. [Google Scholar]
- [6].Dhiman RC, Shahi B, Sharma SN, et al. Persistence of malaria transmission in a tribal area in Maharashtra, India. Curr Sci. 2005; 88(3):475–478. [Google Scholar]
- [7].Singh RK, Mittal PK, Gourshettiwar MP, et al. Susceptibility of malaria vectors to insecticides in Gadchiroli district (Maharashtra), India. J Vector Borne Dis. 2012;49(1):42–44. [PubMed] [Google Scholar]
- [8].District collectorate Gadchiroli - information about district [Internet]; 2017 Jun 14]. Available from: https://gadchiroli.nic.in/enmabtgad1.htm
- [9]. 9789241511575-eng.pdf [Internet]; [cited 2017 Jun 12]. Available from: https://apps.who.int/iris/bitstream/10665/250677/1/9789241511575-eng.pdf.
- [10].Manual on practical entomology in malaria part II. Methods and techniques. Geneva: World Health organization; 1975; p. 191. [Google Scholar]
- [11].Sharma AK, Tyagi V, Singh S, et al. Distribution of Anopheles culicifacies and detection of its sibling species E from Madhya Pradesh: central India. J Arthropod-Borne Dis. 2014;8:186–196. [PMC free article] [PubMed] [Google Scholar]
- [12].Sharma VP, Dev V. Biology & control of Anopheles culicifacies Giles 1901. Indian J Med Res. 2015;141(5):525–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Rahman J, Roy ML, Singh K. Development of increased tolerance to DDT in Anopheles culicifacies Giles, in the Panch Mahal district of Bombay state. India Indian J Malariol. 1959;12:125–130. [Google Scholar]
- [14].Rajagopal R. Malathion resistance in Anopheles culicifacies in Gujarat. Indian J Med Res. 1977;66:27–28. [PubMed] [Google Scholar]
- [15].Singh OP, Raghavendra K, Nanda N, et al. Pyrethroid resistance in An. culicifacies in Surat district, Gujarat, west India. Curr Sci. 2002;82:547–550. [Google Scholar]
- [16].Mishra AK, Chand SK, Barik TK, et al. Insecticide resistance status in Anopheles culicifacies in Madhya Pradesh, central India. J Vector Borne Dis. 2012;49(1):39–41. [PubMed] [Google Scholar]
- [17].Sahu SS, Gunasekaran K, Vijayakumar T, et al. Triple insecticide resistance in Anopheles culicifacies: a practical impediment for malaria control in Odisha State. Indian J Med Res. 2015. Dec; 142(Suppl 1):S59–S63. 10.4103/0971-5916.176621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Koekemoer LL, Spillings BL, Christian RN, et al. Multiple insecticide resistance in Anopheles gambiae (Diptera: Culicidae) from Pointe Noire, Republic of the Congo. Vector Borne Zoonotic Dis Larchmt N. 2011;11:1193–1200. 10.1089/vbz.2010.0192 [DOI] [PubMed] [Google Scholar]
- [19].Dabiré KR, Diabaté A, Djogbenou L, et al. Dynamics of multiple insecticide resistance in the malaria vector Anopheles gambiae in a rice growing area in South-Western Burkina Faso. Malar J. 2008;7(1):188. 10.1186/1475-2875-7-188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Djouaka RJ, Atoyebi SM, Tchigossou GM, et al. Evidence of a multiple insecticide resistance in the malaria vector Anopheles funestus in South West Nigeria. Malar J. 2016;15(1):565. 10.1186/s12936-016-1615-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Nardini L, Christian RN, Coetzer N, et al. DDT and pyrethroid resistance in Anopheles arabiensis from South Africa. Parasit Vectors. 2013;6(1):229. 10.1186/1756-3305-6-229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Toé KH, N’Falé S, Dabiré RK, et al. The recent escalation in strength of pyrethroid resistance in Anopheles coluzzi in West Africa is linked to increased expression of multiple gene families. BMC Genomics. 2015;16:146. 10.1186/s12864-015-1342-6 [DOI] [PMC free article] [PubMed] [Google Scholar]