Summary
Background
The Boston Area Travel Medicine Network surveyed travelers on travel-related health problems.
Methods
Travelers were recruited 2009–2011 during pre-travel consultation at three clinics. The investigation included pre-travel data, weekly during-travel diaries, and a post-travel questionnaire. We analyzed demographics, trip characteristics, health problems experienced, and assessed the relationship between influenza vaccination, influenza prevention advice, and respiratory symptoms.
Results
Of 987 enrolled travelers, 628 (64%) completed all surveys, of which 400 (64%) reported health problems during and/or after travel; median trip duration was 12 days. Diarrhea affected the most people during travel (172) while runny/stuffy nose affected the most people after travel (95). Of those with health problems during travel, 25% stopped or altered plans; 1% were hospitalized. After travel, 21% stopped planned activities, 23% sought physician or other health advice; one traveler was hospitalized. Travelers who received influenza vaccination and influenza prevention advice had lower rates of respiratory symptoms than those that received influenza prevention advice alone (18% vs 28%, P = 0.03).
Conclusions
A large proportion of Boston-area travelers reported health problems despite pre-travel consultation, resulting in inconveniences. The combination of influenza prevention advice and influenza immunization was associated with fewer respiratory symptoms than those who received influenza prevention advice alone.
Keywords: Travel, Influenza, Travel-associated health problems, Survey, Knowledge-attitudes-practices
1. Introduction
Global travel continues to grow, with international tourist arrivals reaching 1.1 billion in 2014 [1]. With increasing international travel, the number of travelers becoming ill during or after travel could also increase.
Over the past three decades, several studies have evaluated health issues encountered during and after travel. These include a survey of Swiss travelers and one of American travelers whose trips were up to 3 months, and analyses from GeoSentinel, a worldwide network of specialized tropical and travel medicine clinics that collect data on travel-related illnesses [2–5]. Health problems occurred during 15% of journeys undertaken by 10,524 Swiss short-term travelers surveyed from 1981 to 1984; 8% consulted a doctor and 3% were unable to work for an average of 15 days [2]. A survey of U.S. travelers found that 64% of 784 reported a health problem, particularly those who undertook longer trips; 8% needed medical evaluations and 26% were ill after return [3]. Two GeoSentinel analyses that examined 17,353 ill returned travelers seen from 1996 to 2004 and 42,173 ill returned travelers seen from 2007 to 2011 found the most commonly reported disorders were gastrointestinal, systemic febrile illness, dermatologic, and respiratory problems [4,5]. In the latter study, 41% of travelers sought pre-travel medical consultations [5].
Pre-travel medical consultations are recommended by the medical community, national agencies such as the U.S. Centers for Disease Control and Prevention (CDC), and professional organizations such as the International Society of Travel Medicine to prepare travelers on how to prevent or manage health problems associated with travel. However, airport-based surveys of outbound U.S. travelers conducted in 2003 and 2009 found that only about 36–54% of travelers to low- or low-middle-income countries had sought health information [6,7].
1.1. Study objectives
Given increased international travel, changes in traveling populations, the evolving risk of disease, and ubiquitous infections like influenza, there is a need to re-evaluate the occurrence of illness associated with travel and to use the results to inform health recommendations. In international travelers attending pre-travel health consultations in three Boston-area travel medicine clinics, we sought to: 1) describe the types, frequency, and impact of health problems occurring during and after travel; 2) assess possible associations of underlying health conditions and trip characteristics with travel-related health problems; and 3) assess the association of influenza vaccination and pre-travel health advice with respect to travel-associated respiratory symptoms, because respiratory infections are among the most common health problems that travelers encounter [2–5] and influenza is the most common vaccine-preventable disease in travelers [8].
2. Materials and methods
2.1. Sample description
We recruited participants aged ≥18 years attending a pre-travel health consultation at three clinics: two in urban, academic hospitals and one in a suburban hospital in the Boston-Area Travel Medicine Network (BATMN) from 2009 through 2011. Written consent was obtained from all participants and Institutional Review Board (IRB) approvals obtained at all clinic sites.
2.2. Measures
At the pre-travel health consultation, travelers were invited to participate and were encouraged to complete a during-travel weekly diary for each week of travel and a post-travel survey upon return. Information collected at baseline (pre-travel) included demographic and trip characteristics, underlying health conditions and medications, immunizations administered, medications prescribed pre-travel, and information received during the pre-travel health consultation. Underlying health conditions included diabetes mellitus, asthma, heart disease, HIV/AIDS, solid organ or bone marrow transplantation, cancer, autoimmune disease, pregnancy, and unspecified chronic medical conditions (including chronic kidney disease on dialysis, cirrhosis, and other diagnoses that did not fit into one of the above-mentioned categories). Specific immune suppressive or immune modulating medications, including prednisone or other steroids, ≥20 mg daily, methotrexate, cancer chemotherapy, and other immunosuppressive drugs were recorded. The during-travel weekly diary queried travel behaviors (including drinking tap water, eating salads, using insect repellent), illnesses experienced, and impact of illness (including needed medical evaluation, stopped activities, hospitalizations). The post-travel survey included questions about adherence to certain prevention practices, illnesses since return, and impact of those illnesses. Participants were included in the analysis if they completed the pre-travel baseline questionnaire, at least one during-travel weekly diary, and a post-travel survey 2–4 weeks after return. A unique numeric identifier was used to link the pre-travel baseline data to the during-travel and post-travel surveys.
Because the study was conducted during the H1N1 outbreak, we assessed influenza advice and vaccination in the pre-travel setting. Respiratory symptoms assessed included cough, runny/stuffy nose, and sore throat. Influenza-like illness was defined according to the WHO definition of cough with fever; however, exact temperature data for travelers experiencing fever were not collected systematically.
2.3. Analysis
Data were entered into two separate password-protected databases (CS Pro, U.S. Census Bureau, Washington, DC), one for the pre-travel baseline data and a second for the during-travel/post-travel surveys. Those who reported experiencing ≥1 symptom during or after travel were compared with those who did not report any symptoms. Travelers who reported a health problem both during and after travel were counted both in the analysis of health problems during travel as well as after travel. Travel destinations were grouped by the 2011 UN human development index (if a traveler went to ≥1 country, the lowest ranked country was used) [9]. Demographic and travel characteristics were evaluated by chi-square test for categorical and Wilcoxon rank sum test for continuous variables. Results from bivariate analyses were expressed as prevalence rate ratios (PRR) with 95% confidence intervals. All two-tailed p-values <0.05 were considered statistically significant. SAS 9.2 (SAS Institute, Cary, NC) was used for all analyses.
3. Results
3.1. Sample description
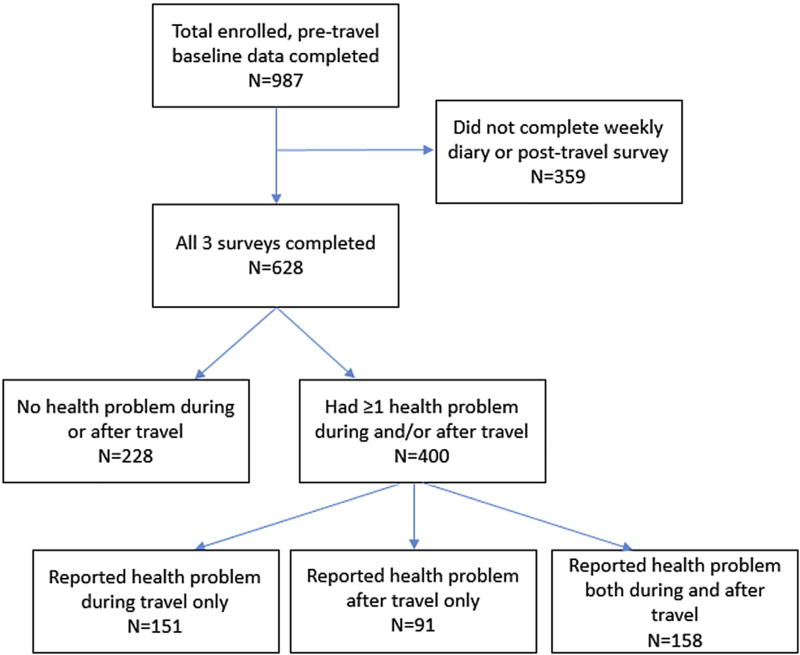
We enrolled 987 travelers. Of those, 628 (64%) completed all three data collection instruments, including at least one during-travel weekly diary and a post-travel survey 2–4 weeks after return (Fig. 1); sites differed in their travelers’ completion rates (39%–75%). Comparison of the 628 to the 359 who did not complete all three parts (non-completers) revealed no differences, except that white travelers had a higher rate of completion than all other racial/ethnic groups (P < 0.001) and completion rates were higher in older travelers (median age 47 years vs. 32 years in non-completers, P < 0.001).
Figure 1.
Study enrollment, those who completed all three data collection surveys, and those who reported health problems during and/or after travel.
3.2. Demographic and trip characteristics
Of the 628 travelers included in the analysis, 59% were female, with a median age of 47 years (range 19–83 years). The median duration of travel was 12 days (range 3–65 days). Most of the 628 participants were U.S.-born, white, traveled for tourism/vacation, and stayed in hotels (Table 1). Non-whites were less likely to report health problems than whites (PRR = 0.83; 95% CI (0.68–1.01), P = 0.04).
Table 1.
Demographics of participants (N = 628) and comparison between those reporting health problems during or after travel and those who did not experience health problems.
| Total N = 628 |
Reported experiencing health problem during and/or after travel N = 400 |
Did not experience any health problems during or after travel N = 228 |
|
|---|---|---|---|
| Median age, years (range) | 47 (19–83) | 47 (19–83) | 48 (19–81) |
| Gender | n (row %) | ||
| Male | 255 (41) | 155 (61) | 100 (39) |
| Female | 373 (59) | 245 (66) | 128 (34) |
| Duration of travel | |||
| ≥14 days | 238 (38) | 163 (68) | 75 (32) |
| <14 days | 383 (62) | 233 (61) | 150 (39) |
| Racea | |||
| White | 528 (85) | 344 (65) | 184 (35) |
| Black | 32 (5) | 12 (38) | 20 (63) |
| Asian: Far East | 28 (5) | 18 (64) | 10 (36) |
| Asian: Indian Subcontinent | 13 (2) | 10 (77) | 3 (23) |
| Hispanic/Latino | 10 (2) | 5 (50) | 5 (50) |
| Bi/Multi-Racial | 9 (2) | 5 (56) | 4 (44) |
| Middle Eastern | 2 (< 1) | 1 (50) | 1 (50) |
| Birth country | |||
| U.S.-born | 517 (82) | 337 (65) | 180 (35) |
| Foreign-born | 110 (18) | 62 (56) | 48 (44) |
| Travel reasonb | |||
| Visiting friends and relatives (VFRs) | 87 (14) | 57 (66) | 30 (34) |
| Tourism/Vacation | 419 (67) | 269 (64) | 150 (36) |
| Business | 115 (18) | 75 (65) | 40 (35) |
| Educational/Research | 24 (4) | 18 (75) | 6 (25) |
| Volunteer/Missionary/Aid Work | 97 (15) | 58 (60) | 39 (40) |
| Seeking medical/dental care outside of the U.S. | 1 (< 1) | 0 (0) | 1 (100) |
| Other | 14 (2) | 10 (71) | 4 (29) |
| Accommodationsb | |||
| Hotel | 412 (66) | 269 (65) | 143 (35) |
| Home/Local Residence | 127 (20) | 85 (67) | 42 (33) |
| Hostel/Budget Hotel/Guest House | 81 (13) | 54 (67) | 27 (33) |
| Dormitory | 28 (4) | 15 (54) | 13 (46) |
| Tent | 84 (13) | 55 (65) | 29 (35) |
| Ship/Yacht/Boat | 59 (9) | 38 (64) | 21 (36) |
| Otherd | 92 (15) | 49 (53) | 43 (47) |
| Top 5 destinationsb | |||
| India | 107 (12) | 70 (65) | 37 (35) |
| South Africa | 46 (5) | 20 (43) | 26 (57) |
| Tanzania | 44 (5) | 29 (66) | 15 (34) |
| Kenya | 39 (4) | 22 (56) | 17 (44) |
| Haiti | 36 (4) | 21 (58) | 15 (42) |
| Destination grouping by UN Human Development Indexc | |||
| Low human development | 165 (26) | 104 (63) | 61 (37) |
| Medium human development | 320 (51) | 209 (65) | 111 (35) |
| High human development | 143 (23) | 87 (61) | 56 (39) |
Nonwhites/whites PRR = 0.83, P = 0.04.
Respondents could have ≥1 choice.
Based on UN human development ranking (high + very high are combined); if traveler went to ≥1 country, the lowest ranked country was used.
No text specified.
The 10 most common destinations were India, South Africa, Tanzania, Kenya, Haiti, Peru, Thailand, Egypt, China, and Costa Rica; more travelers reported experiencing health problems in India, Tanzania, Peru, and Thailand (68% of travelers reporting health problems) compared to travelers to the other six countries (54% of travelers reporting health problems). A higher proportion of U.S.-born travelers reported a health problem than foreign-born travelers, although this was not statistically significant (P = 0.08).
Nearly all (99%) of the 628 travelers reported receiving advice on food and water precautions and diarrhea management, and 333 (53%) reported receiving advice on influenza prevention. Among those with information regarding specific immunizations, 384 (84%) of 412 with information about hepatitis A vaccine received the vaccine, 281 (78%) of 361 with typhoid vaccine information received the vaccine (oral or injection), and 145 (46%) of 315 with influenza vaccine information received the vaccine.
3.3. Types, frequency, and impact of health problems occurring during and after travel
Of the 628 participants, 400 (64%) reported health problems during and/or after travel; 151 (38%) of 400 reported health problems during travel only, 91 (23%) of 400 reported health problems after travel only, and 158 (39%) of 400 reported health problems both during and after travel. In total, 309 (77%) of 400 travelers reported health problems during travel and 249 (62%) of 400 reported health problems after travel. The most common type of health problem was diarrhea, affecting 208 (52%) of 400 travelers (Table 2). One hundred thirty-one travelers reported diarrhea during travel only (33% of those who reported health problems), 36 travelers reported diarrhea after travel only (9% of 400 travelers), and 41 travelers reported diarrhea during and after travel (10% of 400 travelers). While diarrhea was the most commonly reported symptom during travel, runny/stuffy nose was the most common symptom reported after travel, followed by cough. Other frequently reported specific symptoms overall include headache, fatigue, nausea/vomiting, shaking chills, fever, constipation, myalgia, and rash (Table 2).
Table 2.
| Symptom | During travel only: n (row %) |
After travel only: n (row %) |
During and after travel: n (row %) |
Proportion affected among those who reported any health problems (n = 400) |
Proportion of cohort affected (n = 628)b |
|---|---|---|---|---|---|
| Diarrhea | 131 (63) | 36 (17) | 41 (20) | 208 (52) | 208 (33) |
| Nausea or vomiting | 33 (61) | 18 (33) | 3 (6) | 54 (14) | 54 (9) |
| Constipation | 32 (65) | 11 (22) | 6 (12) | 49 (13) | 49 (8) |
| Abdominal pain | 8 (24) | 24 (73) | 1 (3) | 33 (8) | 33 (5) |
| Fever | 33 (67) | 16 (33) | 0 (0) | 49 (13) | 49 (8) |
| Shaking or chills | 33 (66) | 13 (26) | 4 (8) | 50 (13) | 50 (8) |
| Fatigue | 68 (67) | 23 (23) | 10 (10) | 101 (25) | 101 (16) |
| Body/muscle aches and pain | 25 (43) | 28 (48) | 5 (9) | 58 (15) | 58 (9) |
| Headache | 58 (57) | 28 (27) | 16 (16) | 102 (26) | 102 (16) |
| Lightheadedness or vertigo | 23 (88) | 3 (12) | 0 (0) | 26 (7) | 26 (4) |
| Cough | 31 (32) | 40 (41) | 26 (27) | 97 (24) | 97 (15) |
| Runny/stuffy nose | 2 (2) | 92 (95) | 3 (3) | 97 (24) | 97 (15) |
| Sore throat | 1 (3) | 31 (94) | 1 (3) | 33 (8) | 33 (5) |
| Rash or other skin problems | 27 (60) | 9 (20) | 9 (20) | 45 (11) | 45 (7) |
| Other symptoms | 165 (81) | 17 (8) | 21 (10) | 203 (51) | 203 (32) |
151 travelers reported symptoms during travel only, 91 reported symptoms after travel only, and 158 reported symptoms during and after travel.
The proportion is out of the entire cohort of 628 travelers.
≥1 symptom possible for each traveler.
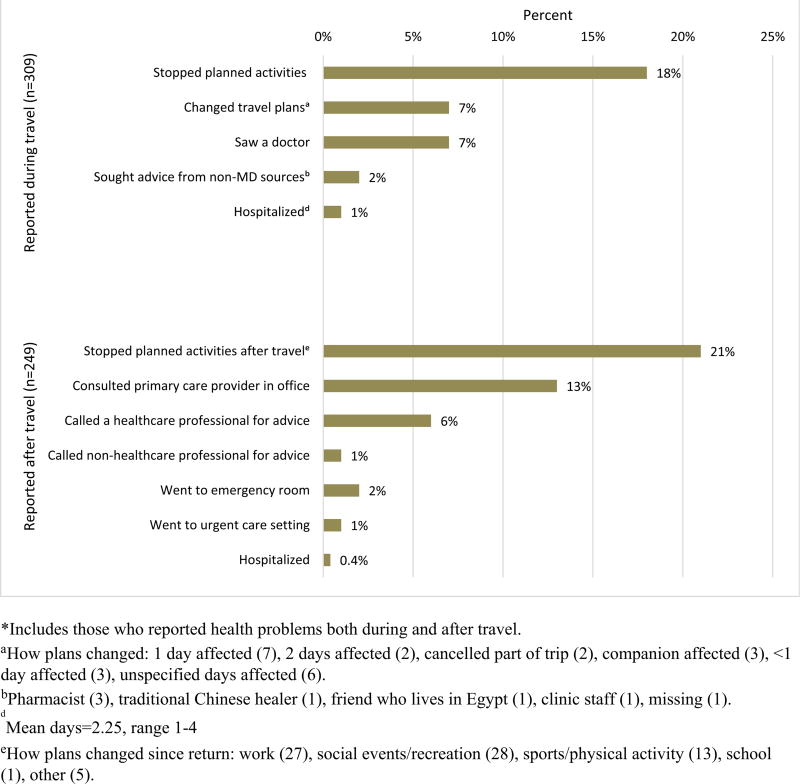
Of the 309 travelers who experienced illness during travel, 56 (18%) stopped planned activities and 23 (7%) had to change plans due to health problems (Fig. 2). Four travelers were hospitalized during travel, for a mean of 2.25 days (range 1–4 days); one reported having heart disease and was hospitalized for pulmonary embolism, while two others reported unspecified chronic medical conditions. Travelers who saw a doctor or sought medical advice from sources other than doctors (pharmacist/clinic staff/healer/friend) because of health problems during travel reported final diagnoses of infections, injury, allergic reaction, and drug reaction (Table 3).
Figure 2.
Impact of health problems experienced among those who reported health problems during (n =309) and after travel (n = 249).*
Table 3.
Specific diagnoses and treatments received during travel or after travel.
| Final diagnoses of those who saw a doctor because of health problems during travel (n = 21) | n |
|
| |
| Infectious = 7 | |
| Amoebiasis | 1 |
| Bacterial infection | 1 |
| Cellulitis (left foot) | 1 |
| Diarrhea | 1 |
| Infection, influenza virus | 1 |
| Streptococcal pharyngitis | 1 |
| Upper respiratory infection | 1 |
| Injury = 3 | |
| Broken toe, allergic reaction | 1 |
| Fractured tibia (below knee) | 1 |
| Laceration/sutures | 1 |
| Drug reaction = 2 | |
| Reaction to transdermal scopolamine patch | 2 |
| Dermatologic = 2 | |
| Frostbite 2+ degree | 1 |
| Allergic reaction | 1 |
| No diagnosis specified = 7 | |
|
| |
| Diagnoses given by physician or healthcare professional after travel – only for those who sought medical care from professionals (n = 52) | n |
|
| |
| Infectious = 26 | |
| Sinusitis | 5 |
| Cold/upper respiratory infection | 4 |
| Virus | 3 |
| Diarrhea | 3 |
| Bronchitis | 2 |
| Campylobacter | 2 |
| Urinary tract infection | 2 |
| Aseptic meningitis | 1 |
| Bacteria | 1 |
| Cellulitis | 1 |
| Giardia | 1 |
| Infected/fractured tooth | 1 |
| Fever | 1 |
| Ringworm | 1 |
| Injury = 2 | |
| Fractured tooth | 1 |
| X-ray ruled out fracture | 1 |
| Dermatologic = 4 | |
| Bites | 2 |
| Allergic reaction | 3 |
| Rash | 1 |
| Non-infectious respiratory problem = 2 | |
| Pulmonary embolism | 1 |
| Asthma attack | 1 |
| Ectopic pregnancy = 1 | |
| Other/unknown/missing (information included fever, bacteria, ruled out for malaria, ruled out for dengue, stool sample negative) = 17 | |
| Treatment prescribed or recommended reported after travel (n = 33) | |
| Over-the-counter medications | 15 |
| Medications administered in-hospitala | 6 |
| Herbal or holistic treatments | 1 |
Of six travelers who were given a medication while in a hospital, only one was hospitalized and reported a diagnosis of aseptic meningitis (given doxycycline). The other five travelers who received a medication in a hospital reported diagnoses and mediations as follows: (stomach virus, IV saline, 1 person); asthma attack, albuterol, 1); (ectopic pregnancy, methotrexate, 1); (sinusitis, ceftriaxone IV, 1); (cellulitis, IV antibiotics, 1).
Of 249 travelers who experienced illness after travel, 53 (21%) stopped planned activities, 40 (16%) saw a doctor, 17 (7%) sought other medical advice because of travel-related health problems, and one traveler was hospitalized. Travelers who sought medical care by a healthcare professional after travel reported diagnoses that included infections, pulmonary embolism, asthma exacerbation, ectopic pregnancy, and dermatologic problems (Table 3).
3.4. Association of travel-related health problems with underlying health conditions or trip characteristics
Travelers experienced health problems whether they went to very high, high, medium, or low UN human development index (HDI) destinations (Table 1).
Less than half (41%) of 628 travelers reported either having pre-existing health conditions or taking medications on a regular basis. There was no difference in reported health problems in those with and without specific underlying health conditions (such as diabetes mellitus, asthma, heart disease, cancer, and autoimmune disorders). Also, there was no difference in reported health problems in those who were taking medications prior to travel and those who were not (including prednisone, methotrexate, cancer chemotherapy, other immunosuppressive drugs) (P = 0.74). However, a higher proportion of travelers with an “unspecified chronic medical condition” reported health problems (31% vs 23% no problem; P = 0.03).
Median trip duration was 12–16 days for travelers with specific symptoms reported, except rash or other skin problems, for which median trip duration was 26 days (range 5–41 days). Median trip durations were 19–20 days for the symptoms of runny/stuffy nose and sore throat.
3.5. Respiratory illness and influenza vaccination
Respiratory symptoms, including cough, sore throat, or runny nose, were reported by 143 (23%) of 628 travelers, affecting 36% of those who reported health problems. Twenty-three (16%) of the 143 with respiratory symptoms had cough and fever suggestive of influenza-like illness (ILI). There was a progressive increase in proportions reporting respiratory symptoms with declining UN HDI (17% for high HDI, 31% for medium, 51% for low).
There were 204 travelers who received influenza vaccine before travel and influenza prevention advice at the pre-travel appointment. Of these, 36 (18%) reported at least one respiratory symptom during or after travel; 4 (2%) had cough and fever suggestive of ILI. Of 129 travelers who received influenza prevention advice but did not receive influenza vaccination at the pre-travel appointment nor had previous vaccination for the current season, 36 (28%) experienced respiratory symptoms during and/or after travel; 10 (8%) experienced cough and fever suggestive of ILI. Of 41 travelers who did not receive influenza prevention advice, did not receive influenza vaccination at the pre-travel appointment, and did not have previous vaccination for the current season, 7 (17%) experienced respiratory symptoms during and/or after travel; none experienced cough and fever suggestive of ILI. Those who were vaccinated for influenza before travel and who received influenza prevention advice at the travel clinic visit had a lower rate of any respiratory symptoms during and/or after travel than those who received influenza prevention advice alone (18% vs 28%, P = 0.03).
Age was the only characteristic that differed between travelers who were immunized and whose who were not immunized (Supplemental Table 4). Those who were immunized were older than those who were not immunized (median age 49 vs. 42 years; P = 0.0009). Travelers visiting friends and relatives (VFR) were vaccinated at a rate similar to non-VFR travelers (Supplemental Table 4). Among those who were vaccinated for influenza prior to travel, VFR travelers experienced any respiratory symptoms during or after travel at a rate similar to non-VFRs.
4. Discussion
A large proportion of our cohort of travelers experienced health problems during or after travel despite receiving pre-travel consultation, similar to a study of American travelers nearly two decades earlier [3]. Given the increase in U.S. annual outbound travel from 52 million to more than 68.2 million trips from 1995 to 2014 and the evidence from our study [10], morbidity from travel-related illness clearly affects a sizable population. Identifying health problems associated with travel and offering strategies to modify risks continue to be relevant. Despite providing travel advice through “traditional” travel clinic visits in the past three decades, travel-related illnesses remain prevalent and new approaches to prevent illness are needed.
The most common symptoms reported by our travelers (diarrhea, headache, cough/runny nose, myalgia/fatigue, fever/chills, and rash) were consistent with previous studies [2–5] as well as a recent survey of Finnish travelers [11]. Health problems led to changing or stopping travel plans in 25% of all travelers during travel and 21% after travel, which may have resulted in an adverse impact on their travel experience or work productivity. In addition, 7% of travelers reporting a health problem during travel saw a local doctor during travel and 1% were hospitalized, raising the concern for potential acquisition of nosocomial infections and colonization with multi-drug resistant (MDR) bacteria [12–17].
4.1. Potential improvements and interventions
We found that “unspecified chronic health conditions” were associated with health problems during travel, including hospitalization. Medical advances are enabling individuals with chronic and active medical problems opportunities to travel despite their health limitations [18,19]. Yet travelers with these problems may be more vulnerable to illness while traveling, possibly with increased susceptibility to infection, exposure to pathogens not present at home, and unfamiliar conditions or exertions due to travel, leading to exacerbation of their underlying conditions. This study underscores the need for more research into which chronic health conditions are actually associated with increased risk of encountering problems during travel, in addition to the need for individualized travel recommendations.
VFR travel has increased in proportion among U.S. travelers over time from 20% in 1995 up to 37% in 2014 [10], and some VFR travelers are at higher risk of certain travel-related illness such as hepatitis A, malaria, and typhoid fever [20–22]. Our analysis found similar rates of health problems between VFRs and tourist travelers, and no difference in influenza immunization rates between VFRs and non-VFRs. VFR travelers generally have been less likely to seek pre-travel advice than tourist travelers [22] and more likely to decline a recommended vaccine [23]. Our results suggest that VFR travelers who obtain pre-travel health consultation have similar rates of health problems as non-VFRs. Therefore, consistent messages from healthcare providers about travel-related health problems may encourage VFR travelers to obtain pre-travel health consultations.
Notably, travelers who received both influenza vaccination and influenza prevention advice reported lower rates of respiratory symptoms than those who received influenza prevention advice alone. This finding highlights the importance of tracking pre-travel consultation and intervention to health outcomes during and after travel, and systematic research regarding such a relationship is needed. As outlined in an Institute of Medicine report, international travel and commerce, human behavior, and demographics have been identified as major risk factors for the emergence of infectious diseases, including influenza [24]. Health professionals providing pre-travel consultation and interventions are well positioned to try to influence the behavior of travelers to minimize health risks to themselves and the larger community. Moreover, our finding of increased respiratory symptoms with declining UN HDI appears plausible, although not previously emphasized [25], since countries with low UN HDI typically have suboptimal public health infrastructure, air quality, infectious disease surveillance, sanitation and infection control, and may experience emergence of new pathogens. Nevertheless, the specific relationships should be evaluated further. The potential for international travelers to disseminate microbes and resistance genes and contribute to the spread of emerging and re-emerging diseases are compelling reasons to promote pre-travel health consultations to advise travelers of this risk. Primary care and specialty providers are also positioned to educate patients about travel-related risk of influenza and antibiotic resistant organisms, especially for patients with chronic medical conditions.
4.2. Limitations
This study has the advantage over previous airport surveys and post-travel surveys in that a population was followed before, during, and after travel, but it has several limitations. BATMN sites may not be representative of traveler populations seen in other institutions or other geographic regions. Also, travelers who seek pre-travel consultation may not be representative of all travelers, and the difference in completion rates between sites and ethnicities may reflect biases among different groups. We were unable to determine whether travelers who developed illness during or after travel were more likely to complete the survey than those who remained well. Similar to other traveler surveys, the reporting of symptoms has inherent subjective biases. The sample size was relatively small, and a substantial proportion of participants did not complete a diary during travel or did not respond to requests to be interviewed post-travel. The category of travelers with “unspecified chronic health conditions” included diagnoses that did not fall into specific categories. The inclusiveness of this category limited the analysis on the association of chronic health conditions with travel-related health problems. We were unable to obtain information on the temperature of each traveler who reported fever during and/or after travel; therefore, cough and fever may not be suggestive of ILI. Because the post-travel survey was conducted 2–4 weeks after travel, some reports of travel-associated ILI may have been overly inclusive. Also, symptoms such as fatigue and headache may be due to jet lag but we did not correlate these symptoms with time zones traveled. Education and advice given in different clinics may have varied in depth and quality. For example, details of the influenza prevention advice at different sites, such as hand-washing, were not captured and precluded assessment of whether such advice may be associated with reduced risk of respiratory and flu-like symptoms [26] as well as a reduced risk of gastrointestinal symptoms [27]. Of note, our study took place at the time of 2009 pandemic influenza A(H1N1) circulation. The discussion of influenza prevention, along with heightened awareness of influenza, may have led to beneficial behavior and outcomes.
Finally, this study did not explore the level of morbidity in those who do not seek pre-travel preparation, and cannot project morbidity for those travelers. Given the persistent travel-related morbidity in those who received pre-travel preparation, new and more effective approaches are clearly needed to prevent travel-associated morbidity.
5. Conclusions
Health problems during and after travel affected about two-thirds of international travelers who had received pre-travel consultation. Travelers primarily reported gastrointestinal, respiratory, and dermatologic symptoms and febrile illness. Disruption of travel plans results in inconvenience, stress, and a less enjoyable experience. Possible mitigation of respiratory illness by advice on influenza prevention and immunization would be a welcome benefit, but additional studies are needed to identify essential elements of the intervention. Preparing travelers to anticipate post-travel health problems is sensible. Behaviors such as hand washing could prevent other illnesses besides influenza or other respiratory infections. Future focus in travel medicine should address travelers with chronic illness by engaging their subspecialists and primary care doctors. Finally, immunizations must be combined with education about disease prevention due to a lack of vaccines to prevent some infections acquired by travelers, as well as incomplete protection provided by some vaccines, such as influenza.
Supplementary Material
Acknowledgments
We thank Allison Kay and Deborah Gannon for their assistance with conducting the surveys and entering data. This research was funded by a cooperative agreement (1 U19CI000508-01) between the Centers for Disease Control and Prevention and Boston Medical Center. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Christine Benoit was formerly at Maxwell Finland Laboratory for Infectious Diseases, Boston Medical Center, Boston, MA, USA.
LHC and RJS had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
LHC is an advisor for Shoreland, Inc. and has received speaker travel support and honorarium from GSK. EDB reports clinical trials funding from Intercell (now Valneva) for JE vaccine Ixiaro in children. DHH is a member of the iJet advisory board and has served as a consultant to Glaxo Smith Kline’s vaccine division.
Footnotes
Conflict of interest
The authors report no financial disclosures relevant to this work.
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.tmaid.2016.09.009.
References
- 1.UNWTO World Tourism Barometer January 2015 Edition. [Accessed 4 August 2015]; Available at: http://mkt.unwto.org/barometer/january-2015-volume-13.
- 2.Steffen R, Rickenbach M, Wilhelm U, Helminger A, Schär M. Health problems after travel to developing countries. J Infect Dis. 1987;156:84–91. doi: 10.1093/infdis/156.1.84. [DOI] [PubMed] [Google Scholar]
- 3.Hill DR. Health problems in a large cohort of Americans traveling to developing countries. J Travel Med. 2000;7:259–66. doi: 10.2310/7060.2000.00075. [DOI] [PubMed] [Google Scholar]
- 4.Freedman DO, Weld LH, Kozarsky PE, Fisk T, Robins R, von Sonnenburg F, et al. Spectrum of disease and relation to place of exposure among ill returned travelers. N Engl J Med. 2006;354(2):119–30. doi: 10.1056/NEJMoa051331. [DOI] [PubMed] [Google Scholar]
- 5.Leder K, Torresi J, Libman MD, Cramer JP, Castelli F, Schlagenhauf P, et al. GeoSentinel surveillance of illness in returned travelers, 2007–2011. Ann Intern Med. 2013;158(6):456–68. doi: 10.7326/0003-4819-158-6-201303190-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamer DH, Connor BA. Travel health knowledge, attitudes and practices among United States travelers. J Travel Med. 2004;11:23–6. doi: 10.2310/7060.2004.13577. [DOI] [PubMed] [Google Scholar]
- 7.LaRocque RC, Rao SR, Tsibris A, Lawton T, Barry MA, Marano N, et al. Pre-travel health advice-seeking behavior among US international travelers departing from Boston Logan International Airport. J Travel Med. 2010;17(6):387–91. doi: 10.1111/j.1708-8305.2010.00457.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steffen R, Behrens RH, Hill DR, Greenaway C, Leder K. Vaccine-preventable travel health risks: what is the evidence — what are the gaps? Travel Med. 2015;22:1–12. doi: 10.1111/jtm.12171. [DOI] [PubMed] [Google Scholar]
- 9.United Nations Development Programme. Human development index. [Accessed 1 November 2015]; Available at: http://hdr.undp.org/en/content/human-development-index-hdi.
- 10.US Department of Commerce, International Trade Administration, Office of Travel and Tourism Industries. US Travel and Tourism Statistics (US Resident Outbound) [Accessed 4 August 2015]; Available at: http://travel.trade.gov/outreachpages/outbound.general_information.outbound_overview.html.
- 11.Vilkman K, Pakkanen SH, Lääveri T, Siikamäki H, Kantele A. Travelers’ health problems and behavior: prospective study with post-travel follow-up. BMC Infect Dis. 2016 Jul 13;16:328. doi: 10.1186/s12879-016-1682-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Angue M, Allou N, Belmonte O, Lefort Y, Lugagne N, Vandroux D, et al. Risk factors for colonization with multidrug-resistant bacteria among patients admitted to the intensive care unit after returning from abroad. J Travel Med. 2015;22(5):300–5. doi: 10.1111/jtm.12220. [DOI] [PubMed] [Google Scholar]
- 13.Epelboin L, Robert J, Tsyrina-Kouyoumdjian E, Laouira S, Meyssonnier V, Caumes E, et al. High rate of multidrug-resistant Gram-negative bacilli carriage and infection in hospitalized returning travelers: a cross-sectional cohort study. J Travel Med. 2015;22(5):292–9. doi: 10.1111/jtm.12211. [DOI] [PubMed] [Google Scholar]
- 14.Josseaume J, Verner L, Brady WJ, Duchateau FX. Multidrug-resistant bacteria among patients treated in foreign hospitals: management considerations during medical repatriation. J Travel Med. 2013;20(1):22–8. doi: 10.1111/j.1708-8305.2012.00668.x. [DOI] [PubMed] [Google Scholar]
- 15.Fournier S, Lepainteur M, Kassis-Chikhani N, Huang M, Brun-Buisson C, Jarlier V, et al. Link between carbapenemase-producing Enterobacteria carriage and cross-border exchanges: eight-year surveillance in a large French multihospitals institution. J Travel Med. 2012;19(5):320–3. doi: 10.1111/j.1708-8305.2012.00641.x. [DOI] [PubMed] [Google Scholar]
- 16.Hassing RJ, Alsma J, Arcilla MS, van Genderen PJ, Stricker BH, Verbon A. International travel and acquisition of multidrug-resistant Enterobacteriaceae: a systematic review. Euro Surveill. 2015 Nov 26;20(47) doi: 10.2807/1560-7917.ES.2015.20.47.30074. [DOI] [PubMed] [Google Scholar]
- 17.Lyman M, Walters M, Lonsway D, Rasheed K, Limbago B, Kallen A. Notes from the field: carbapenem-resistant Enterobacteriaceae producing OXA-48-like carbapenemases - United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2015 Dec 4;64(47):1315–6. doi: 10.15585/mmwr.mm6447a3. [DOI] [PubMed] [Google Scholar]
- 18.Hochberg NS, Barnett ED, Chen LH, Wilson ME, Iyer H, MacLeod WB, et al. International travel by persons with medical comorbidities: understanding risks and providing advice. Mayo Clin Proc. 2013;88(11):1231–40. doi: 10.1016/j.mayocp.2013.07.018. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz BS, Rosen J, Han PV, Hynes NA, Hagmann SH, Rao SR, et al. Immunocompromised travelers: demographic characteristics, travel destinations, and pretravel health care from the U.S. Global TravEpiNet Consortium. Am J Trop Med Hyg. 2015 Nov 4;93(5):1110–6. doi: 10.4269/ajtmh.15-0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Behrens RH, Collins M, Botto B, Heptonstall J. Risk of British travelers acquiring Hepatitis A (letter) BMJ. 1995;311:193. doi: 10.1136/bmj.311.6998.193a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mermin JH, Townes JM, Gerber M, Dolan N, Mintz ED, Tauxe RV. Typhoid fever in the United States, 1985–1994: change in risks of international travel and increasing antimicrobial resistance. Arch Intern Med. 1998;158:633–8. doi: 10.1001/archinte.158.6.633. [DOI] [PubMed] [Google Scholar]
- 22.Leder K, Tong S, Weld L, Kain KC, Wilder-Smith A, von Sonnenburg F, et al. Illness in travelers visiting friends and relatives: a review of the GeoSentinel Surveillance Network. Clin Infect Dis. 2006;43:1185–93. doi: 10.1086/507893. [DOI] [PubMed] [Google Scholar]
- 23.LaRocque RC, Deshpande BR, Rao SR, Brunette GW, Sotir MJ, Jentes ES, et al. Pre-travel health care of immigrants returning home to visit friends and relatives. Am J Trop Med Hyg. 2013;88(2):376–80. doi: 10.4269/ajtmh.2012.12-0460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamburg MA, Lederberg J, Smolinski MS. Microbial threats to health. National Academies Press; 2003. [PubMed] [Google Scholar]
- 25.Redman CA, MacLennan A, Wilson E, Walker E. Diarrhea and respiratory symptoms among travelers to Asia, Africa, and South and Central America from Scotland. J Travel Med. 2006;13:203–11. doi: 10.1111/j.1708-8305.2006.00046.x. [DOI] [PubMed] [Google Scholar]
- 26.Little P, Stuart B, Hobbs FD, Moore M, Barnett J, Popoola D, et al. An internet-delivered handwashing intervention to modify influenza-like illness and respiratory infection transmission (PRIMIT): a primary care randomised trial. Lancet. 2015 Oct 24;386(10004):1631–9. doi: 10.1016/S0140-6736(15)60127-1. [DOI] [PubMed] [Google Scholar]
- 27.Henriey D, Delmont J, Gautret P. Does the use of alcohol-based hand gel sanitizer reduce travellers’ diarrhea and gastrointestinal upset?: a preliminary survey. Travel Med Infect Dis. 2014 Sep-Oct;12(5):494–8. doi: 10.1016/j.tmaid.2014.07.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.