Abstract
Background
Tuberculous infection of the lumbar spine may be associated with psoas abscess. The aim of this clinical study was to compare the outcome of posterior lumbar debridement and spinal fusion, combined with either a one-stage anteroposterior (AP) or posterior (P) approach to percutaneous catheter drainage (PCD) for the treatment of lumbar tuberculosis with psoas abscess.
Material/Methods
From January 2008 to June 2012, 74 patients were diagnosed at our hospital with lumbar tuberculosis with unilateral or bilateral psoas abscess. Forty-three patients underwent P-PCD (group A), and 31 patients underwent AP-PCD (group B). Operative duration, blood loss, the length of hospital stay, spinal correction, clinical cure rate, and other clinical outcomes in the two groups were compared.
Results
Comparison of the outcome for the P-PCD and AP-PCD patients showed that there was no significant difference in outcome for spinal bone fusion, correction of spinal deformity, or cure rate from tuberculosis infection (P>0.05). Blood loss, operative time, and the length of hospital stay for patients in group A, the P-PCD group, were significantly less than for group B, the AP-PCD group (P<0.05). Also, group B, the AP-PCD group, had an increased incidence of complications than group A, the P-PCD group, leading to increased hospital stay (OR 3.04, CI 0.52–17.75).
Conclusions
For the treatment of tuberculous psoas abscess using PCD, the posterior approach may achieve the same clinical efficacy as the anteroposterior approach, but is associated with reduced length of hospital stay, and lower risk of complications.
MeSH Keywords: Psoas Abscess; Skin Absorption; Tuberculosis, Spinal
Background
Tuberculosis (TB) is an infectious disease that has affected human populations for centuries [1]. TB remains an important cause of morbidity and mortality worldwide. During the past few decades, rates of new pulmonary TB cases have been falling slowly, but there has been a recent increase in the incidence of extrapulmonary TB [2].
Osteoarticular tuberculosis accounts for approximately 3–5% of cases of extrapulmonary TB, and up to 50% of these cases are spinal TB [3]. Patients with spinal TB may suffer from paraspinal abscess or psoas abscess, which are observed in approximately 75–83% of cases [4,5]. Because of the close anatomical relationship between the psoas and the vertebrae, lumbar spinal TB is often associated with psoas abscess [6].
The approach to the treatment of lumbar spinal TB and psoas abscess may include percutaneous catheter drainage (PCD) via the posterior (P) approach, with an anteroposterior (AP) approach having been recently described [7]. However, the anteroposterior PCD procedure results in greater blood loss, longer operating time and an increased risk of complications, with an anterior-alone approach now thought not to be suitable for the treatment of lumbar TB [8].
During the past ten years, PCD has been used in the treatment of abscess due to TB [9–11], but there are few reports on the treatment of lumbar tuberculosis with psoas abscess by posterior PCD (P-PCD). Furthermore, there have been no clinical studies to compare the clinical outcome following anteroposterior PCD (AP-PCD) and P-PCD.
The aim of this clinical study was to compare the outcome of posterior lumbar debridement and spinal fusion, combined with either a one-stage anteroposterior (AP) or posterior (P) approach to PCD for the treatment of lumbar TB with psoas abscess.
Material and Methods
Patients studied: posterior percutaneous catheter drainage (P-PCD) (group A); anteroposterior percutaneous catheter drainage (AP-PCD) (group B)
From January 2008 to June 2012, 74 patients with lumbar tuberculosis (TB) with unilateral or bilateral psoas abscess received surgery at our spinal center and were recruited into this study. Patients had undergone posterior lumbar debridement and spinal fusion, combined with either a one-stage anteroposterior (AP) or posterior (P) approach to percutaneous catheter drainage (PCD) for the treatment of lumbar tuberculosis with psoas abscess.
There were 43 patients who received posterior PCD (P-PCD) (group A) including 25 men and 18 women, aged from 20 to 63 years, with an average age of 38.5±8.7 years. The average follow-up time was 18.9±3.4 months. There were 36 cases in group A with P-PCD who had unilateral psoas abscess, and seven cases had bilateral psoas abscess. There were eight patients who suffered from neurological deficit, according to the American Spinal Injury (ASIA) grading system: one case was grade C; seven cases were grade D.
There were 31 patients who received anteroposterior PCD (AP-PCD) (group B) including 17 men and 14 women, aged from 22 to 61 years, with an average age of 39.9±9.5 years. The average follow-up time was 19.6±3.5 months. There were 27 cases in group B with unilateral psoas abscess, and four cases had bilateral psoas abscess. There were six patients who suffered from neurological deficit, according to the ASIA grading system: two cases were grade C; four cases were grade D.
All patients included in the study had a definitive diagnosis of TB that included bacterial culture, acid-fast staining, polymerase chain reaction (PCR), or tissue histology from samples removed during surgery.
The diagnostic criteria that provided an indication for surgical intervention included [12]: 1) severe or progressive neurological deficit; 2) severe kyphosis or kyphosis likely to progress; 3) failed conservative treatment that included 1) and 2), or severe pain due to abscess or spinal instability.
The characteristics and location of the psoas abscess were confirmed by computed tomography (CT) scan or magnetic resonance imaging (MRI). Patients with polycystic psoas abscess, necrotic tissue sequestered in the abscess, multi-site psoas abscess, and dense pus mixed with caseous necrosis according to CT or MRI imaging were all excluded. All the abscesses included in this study were larger than 3 cm [10]. Two senior surgeons reviewed the surgical indications and performed the procedures.
Written informed consent was obtained from all patients. The Ethics Committee of The Affiliated Hospital of Southwest Medical University, Luzhou, Sichuan, China approved the study protocol. The clinical data of the patients with tuberculous psoas abscess in group A and group B are shown in Table 1.
Table 1.
Patients data of two groups.
| Group | No. cases | Sex | Age (years) | Follow-up time (months) | Pathologic vertebrae segments(n) | Psoas abscess | ||
|---|---|---|---|---|---|---|---|---|
| M | F | Unilateral | Bilateral | |||||
| A | 43 | 25 | 18 | 38.6±8.7 | 18.9±3.4 | 1.16 | 36 | 7 |
| B | 31 | 17 | 14 | 40±9.5 | 19.6±3.5 | 1.18 | 27 | 4 |
| Total | 74 | 42 | 32 | 39.1±9 | 19.2±3.4 | 1.17 | 63 | 11 |
Preoperative management
All patients in group A and group B underwent standard four-drug TB therapy that included isoniazid (5 mg/kg), rifampicin (10 mg/kg), ethambutol hydrochloride(15 mg/kg) and pyrazinamide (25 mg/kg) as first-line treatment, lasting four or five weeks.
The patients in Group A underwent PCD before surgery (Figure 1): the skin markers were confirmed by ultrasound guidance. Under local anesthesia, a 0.5 cm skin incision was performed. There were 50 large-lumen (from 10-F to 14-F) drainage catheters that were used in 43 patients. All drainage catheters were inserted into abscess cavities with the Seldinger technique by an anterior or posterior extraperitoneal approach (Figures 1, 2). During the period of catheter drainage, 5% sodium bicarbonate solution was used to irrigate the psoas abscess cavities once or twice. Catheters in the abscess were removed when there was no pus flowing out, and ultrasound examination proved that there was no residual pus.
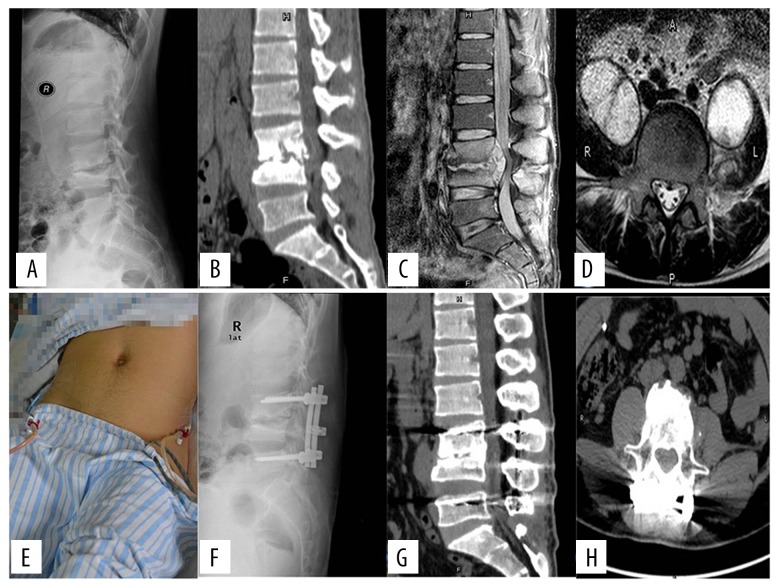
Figure 1.
Outcome of posterior lumbar debridement and spinal fusion, combined with a one-stage posterior (P) approach to percutaneous catheter drainage (PCD) for the treatment of lumbar tuberculosis with psoas abscess. A 42-year-old man underwent posterior percutaneous catheter drainage (P-PCD). Preoperative lateral X-radiograph (A) and sagittal computed tomography (CT) (B) showed spinal tuberculosis at L3–4. Preoperative sagittal magnetic resonance image (MRI) (C) and axial MRI (D) showed epidural abscess and bilateral psoas abscess: (E) PCD of bilateral abscess; (F) postoperative lateral X-radiograph; 18-month follow-up sagittal CT-can (G) and axial CT scan (H) showed that as bone fusion was achieved, the bilateral psoas abscess disappeared.
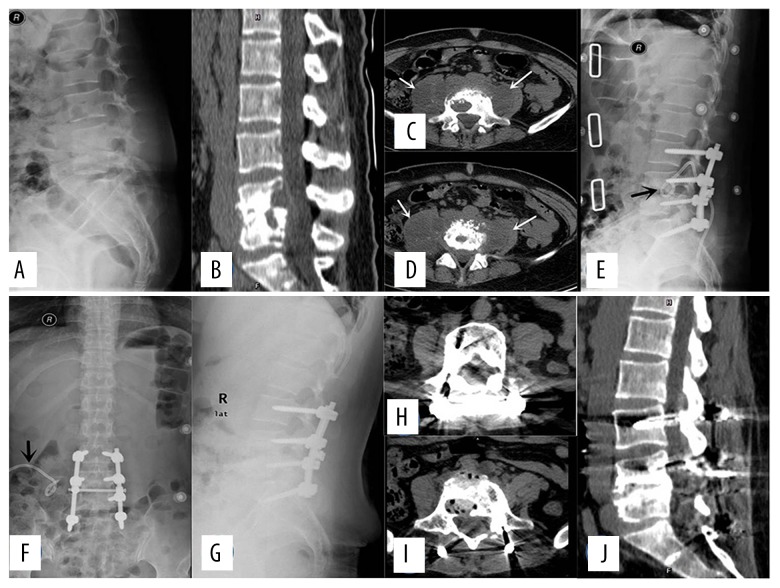
Figure 2.
Outcome of posterior lumbar debridement and spinal fusion, combined with a one-stage posterior (P) approach to percutaneous catheter drainage (PCD) for the treatment of lumbar tuberculosis with psoas abscess. A 36-year-old female underwent posterior percutaneous catheter drainage (P-PCD). Preoperative lateral X-radiograph (A) and sagittal computed tomography (CT) scan (B) showed spinal tuberculosis at L4–5; (C, D) different levels of the axial CT scan showed bilateral abscesses (white arrows); postoperative lateral X-radiograph (E) and anteroposterior X-radiograph (F), the left catheter had been removed and the right catheter was still in place (black arrows); (G) lateral radiograph three months after surgery; 24-month follow-up shows different levels of the axial CT scan (H, I) and a sagittal CT scan (J).
Operative techniques used for (P-PCD) (group A)
If the patients had no fever, abdomen pain, or other symptoms correlated to the PCD procedure after 5–7 days, posterior lumbar debridement, fusion and instrumentation were performed. Under general anesthesia, patients were placed in the prone position. Pedicle screws were inserted into the cephalic and caudal adjacent lumbar spine vertebral segments. If the residual height of the non-infected lumbar vertebrae was more than half a vertebral length, the pedicle screws were inserted into it. A single titanium rod was implanted for the temporary fixation at one side. Lumbar vertebral laminectomy was performed at the decompression level to expose the intervertebral lesion. The caseous tissue and sequestrum were thoroughly cleaned. A preformed titanium rod was used to correct the spinal kyphosis. The autogenous iliac bone was implanted for a large bone defect at intervertebral space. If the bone defect was small, autogenous bone was selected for posterior fusion of the same segments.
Operative techniques used for (AP-PCD) (group B)
Under general anesthesia, pedicle screws were inserted in two normal vertebral bodies around the lesion. If the residual height of the non-infected lumbar vertebrae was more than half a vertebral length, the pedicle screws were inserted into it. A preformed titanium rod was used to correct the spinal kyphosis. The patient was moved to the right or left lateral position, depending on the site of the psoas abscess. An anterolateral extraperitoneal approach was used to expose the tuberculous lesion. Abscess, sequestrum and intervertebral disc were radically eradicated until the margin of the bleeding vertebra was obtained. After sufficient spinal cord decompression, autogenous tricortical iliac bone or rib was implanted to reconstruct the anterior vertebral column (Figure 3).
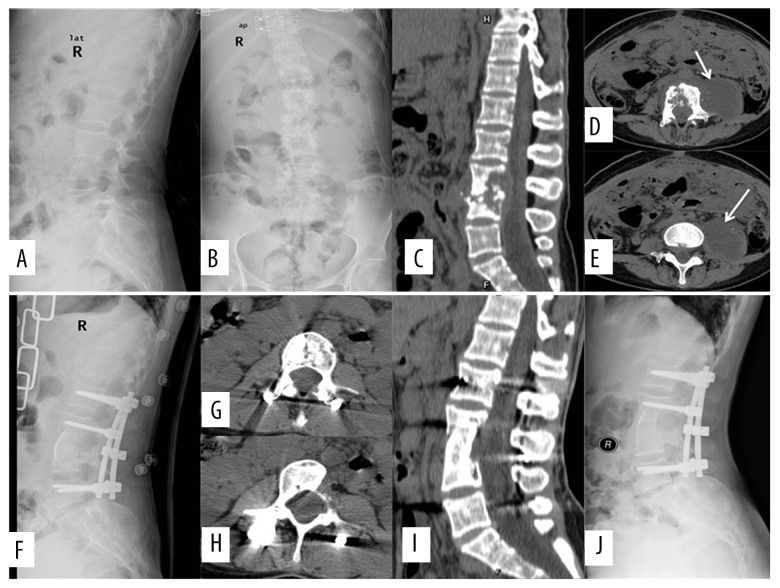
Figure 3.
Outcome of posterior lumbar debridement and spinal fusion, combined with a one-stage anteroposterior (AP) approach to percutaneous catheter drainage (PCD) for the treatment of lumbar tuberculosis with psoas abscess. A 51-year-old man underwent anteroposterior percutaneous catheter drainage (AP-PCD). Preoperative lateral X-radiograph (A) and anteroposterior X-radiograph (B), spinal tuberculosis at L3–4; preoperative sagittal computed tomography (CT) scan (C) showed epidural abscess; different levels of axial CT scan (D, E) showed a left abscess (white arrows); postoperative lateral X-radiograph (F); a 6-month follow-up sagittal CT scan (I) and axial CT scan (G, H); a 24-month follow-up lateral X-radiograph (J).
Postoperative management
The resected tissue and pus were sent for PCR analysis, bacterial culture, and pathological diagnosis. All patients were treated with anti-TB drugs sequentially, with four first-line drugs that were continued for three months and followed by a three-drug anti-TB treatment (Rifampicin/INH/Ethambutol) for at least nine months. If the drug sensitivity test (DST) suggested that any first-line drug resistance, individualized chemotherapy was specially designed for these patients based on their chemotherapy history and TB drug susceptibility profiles.
Clinical follow-up and statistical analysis
Patients in group A and group B were reviewed clinically every month for the first three months and at three monthly intervals, with X-rays, erythrocyte sedimentation rate (ESR), liver and renal function tests. Bone fusion was assessed monthly based on CT scans after the first three months.
A diagnosis of clinical cure of TB was made when the following were present for at least six months: 1) there was no fever or other symptoms; 2) the ESR returned to normal; 3) the imaging results showed bone fusion, and there was no abnormality. During the period anti-TB drug treatment, if the ESR fell for several weeks, this indicated that the anti-TB drugs were effective.
The kyphosis angle was calculated on the lateral X-ray, using two lines drawn, one parallel to the superior surface of the cephalic vertebra of the diseased segments and the other parallel to the inferior surface of the caudal vertebra of the diseased segments, with the kyphosis angle at their intersection. The kyphosis angle value was positive for lumbar lordosis and negative for lumbar kyphosis. Neurological function was assessed using the ASIA classification. The operative time, the amount of blood loss, the length of hospital stay, the clinical cure rate, and other clinical results for the two patient groups, A and B, were analyzed and compared.
The Student’s t-test was used to analyze the statistical significance between groups and the chi-squared test was used for noncontinuous variables. P<0.05 was considered to be statistically significant.
Results
All patients with tuberculosis (TB) in both groups were cured of infection at the final clinical follow-up. The patients with neurological dysfunction improved after surgery (Table 2). All cases achieved bone fusion.
Table 2.
Patients with neurological deficit in both groups before surgery and at final follow-up.
| Preoperative ASIA grade | No (Group A/B) | ASIA grade at final follow-up (Group A/B) | ||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | ||
| C | 1/2 | 0/1 | 1/1 | |||
| D | 7/4 | 7/4 | ||||
For patients in group A, who had undergone the posterior (P) approach to percutaneous catheter drainage (PCD) (P-PCD), the time of use of 50 drainage catheters in the psoas abscess ranged from six to 14 days with an average of 9.6±1.9 days. There was no sinus formation at the PCD puncture location. There were 40 (93%) cases that were primarily cured, three (7%) cases relapsed, one case with a posterior abscess, one case with a sinus at the surgical site, one case with a recurrent psoas abscess. Cerebrospinal fluid leak (CSFL) occurred in one case during the surgery, wound dehiscence occurred in one case.
For patients in group B, who had undergone the anteroposterior (AP) approach to PCD (AP-PCD), 29 (93.5%) cases were primarily cured of TB infection. There were 2 (6.5%) cases that relapsed, one case with a sinus at the anterior surgical site, and one case with a recurrent psoas abscess. There were other complications that occurred in four cases (Table 3).
Table 3.
The clinical results of both groups.
| Group A | Group B | P value | |
|---|---|---|---|
| Case (n) | 43 | 31 | |
| Pre-operative ESR (mm/h) | 46.72±10.18 | 47.39±8.12 | P>0.05 |
| Post-operative ESR (mm/h) | Normal | Normal | – |
| Bone fusion time (months) | 5.12±1.4 | 4.58±1.09 | P>0.05 |
| Preoperative kyphosis angle (°) | −0.77±8.98 | −0.06±9.87 | P>0.05 |
| Postoperative kyphosis angle (°) | 9.81±5.9# | 8.9±7.76# | P>0.05 |
| The final follow-up kyphosis angle (°) | 8.35±6.19* | 7.32±8.06* | P>0.05 |
| Average correction of kyphosis angle (°) | 10.19±4.58 | 8.87±2.81 | P>0.05 |
| Average loss of the correction (°) | 1.41 | 1.06 | P>0.05 |
| Surgical time (min) | 178.49±30.01 | 242.26±27.65 | P<0.01 |
| Loss of blood (ml) | 479.53±107.72 | 798.71±129.56 | P<0.01 |
| Hospital stay (day) | 18.67±2.52 | 20.55±2.96 | P<0.01 |
| Relapse (n) | 3 | 2 | P>0.05 |
| Complications (n) | 2 | 4 | P>0.05 |
| Ileus | 0 | 1 | – |
| Wound dehiscence | 1 | 2 | – |
| Mixed infection | 0 | 0 | – |
| Leakage of cerebrospinal fluid | 1 | 0 | – |
| Vascular injury | 0 | 0 | – |
| Erectile dysfunction | 0 | 0 | – |
| Pneumonia | 0 | 1 | – |
There is significant statistical different between preoperative and postoperative kyphosis angle (Student’s t-test P<0.05);
there is significant statistical different between preoperative and final follow-up kyphosis angle (Student’s t-test P<0.05).
There was no significant statistical difference between groups regarding cure rate, with the chi-squared test (P>0.05). There was no statistical difference in the rate of complications between groups (P>0.05) and the overall response rate (ORR)=3.04 (CI=0.52–17.75). The correction of the kyphosis deformity, the loss of correction angle, and the bone fusion time between groups had no statistically significant difference (P>0.05). The amount of blood loss, operative time, and the length of hospital stay were statistically significant between the groups (P<0.05). The comparative statistical data of both groups are shown in Table 3.
Discussion
Tuberculous psoas abscess is associated with paravertebral abscess arising from lumbar tuberculosis (TB). Because psoas abscess can progress to the inguinal region, early diagnosis and effective treatment are important. Spinal TB can also mimic other diseases, including malignancy, and this reason also supports the need for early diagnosis and appropriate treatment [13–15]. Although cases of psoas abscess due to TB can present with a range of symptoms, this study has shown that most cases presented with few symptoms and required diagnosis using computed tomographic (CT) or magnetic resonance imaging (MRI). Recent studies have highlighted the infectious complications of psoas abscess, but also the possibility of complete resolution [16]. Imaging studies have now contributed to the development of treatment protocols for abscesses due to TB [17,18]. Small abscesses due to TB may be treated with anti-tuberculous drugs, but large abscesses are more likely to develop leaking fistula or sinus tracts and require surgical intervention [17,18].
Although open surgery via the extraperitoneal approach combined with drug treatment has traditionally been the mainstay of therapy, retroperitoneal or laparoscopic drainage has recently been used [17,18]. However, because general anesthesia is required, open surgery is associated with more clinical complications. In the early 1970s, image-guided percutaneous drainage (PCD) began to be used in the treatment of psoas abscess [19]. PCD has the advantage of less trauma, the use of local anesthesia, and rapid alleviation of the symptoms of psoas abscess. The pus can be obtained via PCD at an early stage for microbial diagnosis including polymerase chain reaction (PCR), bacterial culture, and drug sensitivity testing (DST).
Previous reports on the use of PCD using a posteroanterior (PA) approach have combined this with conservative anti-TB therapy [9–11]. However, when lumbar vertebral TB requires surgery, if there is unilateral or bilateral psoas abscess, the anterior approach alone can eradicate the infection focus, but anterior instrumentation may be more challenging at the level of lower lumbar vertebral disease (L4–5, L5–S1) and for multi-level lesions [20]. Also, anterior instrumentation cannot achieve the same biomechanical stability as posterior instrumentation. Therefore, the anteroposterior (AP) approach would seem to be the most suitable [21]. In 2014, Li and colleagues described an improved single-stage posterior surgical approach for spinal TB with psoas abscess [22]. However, in this technique, the skin incision has to be extended to the level of the psoas abscess, and this aggressive posterior approach may prolong the surgical time and result in trauma [22]. Also, in 2013, Pang and colleagues reported a one-stage posterior approach with postural drainage for the treatment of thoracolumbar spinal TB with psoas abscess [23]. However, the drainage procedure used prolongs the time of general anesthesia, and postural drainage may not be sufficient for psoas abscess [23].
In this study, anteroposterior (AP) and posterior (P) PCD were undertaken before surgery was performed to treat the vertebral lesion. PCD could be performed easily, resulting in negligible loss of blood, less pain, and under local anesthesia and avoiding the complications of anterior surgery [8]. During the surgery, the patients who underwent posterior PCD (P-PCD) (group A) did not have to change the operative position, unlike the patients who underwent anteroposterior PCD (AP-PCD) (group B). This study has shown that posterior PCD (P-PCD) minimized surgical time, reduced surgical trauma, and facilitated more rapid recovery for patients. Furthermore, posterior PCD (P-PCD) (group A) had a lower risk of causing complications (OR 3.04, CI 0.52–17.75), while achieving favorable correction of kyphosis angle and bone fusion (P>0.05). Posterior PCD (P-PCD) (group A) did not lead to secondary bacterial infection, injury to abdominal organs or blood vessels, or other complications. Ultrasound guidance is very safe and is free from the radiation associated with CT scan guidance. During the catheter drainage, anti-TB drugs and alkaline sodium bicarbonate injection were used to irrigate the cavities; these procedures can promote the local concentration of anti-TB drugs and inhibit mycobacterial growth, reducing the risk of recurrence of psoas abscess.
In this study, there was only one recurrence of psoas abscess, seen in group A. However, we cannot conclude whether the reason for the recurrence of psoas abscess was from the vertebral lesion or not. Following the findings of this study, we recommend that individualized treatment for lumbar TB with psoas abscess should be implemented, and recommend against the use of PCD if the psoas abscess has the following characteristics: multiple abscess sites within the psoas; caseous necrosis sequestered within the pus of the abscess; polycystic psoas abscess; small psoas abscess size of less than 3 cm.
Conclusions
Because the anteroposterior approach to PCD is not necessarily suitable for all patients with lumbar tuberculosis with psoas abscess, the posterior approach should be considered, as it results in a good clinical outcome and is less invasive. The findings of this small clinical study at a single center have shown that, for the treatment of tuberculous psoas abscess using PCD, the posterior approach may achieve the same clinical efficacy as the anteroposterior approach, but is associated with reduced length of hospital stay, and lower risk of complications.
Footnotes
Conflict of interest
None.
Source of support: Departmental sources
References
- 1.Tuli SM. Historical aspects of Pott’s disease (spinal tuberculosis) management. Eur Spine J. 2013;22(Suppl 4):529–38. doi: 10.1007/s00586-012-2388-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) Global Tuberculosis Report 2013. Euro Surveill. 2013;18(43) pii: 20615. [PubMed] [Google Scholar]
- 3.Rajasekaran S, Khandelwal G. Drug therapy in spinal tuberculosis. Eur Spine J. 2013;22(Suppl 4):587–93. doi: 10.1007/s00586-012-2337-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jain AK, Sreenivasan R, Saini NS, et al. Magnetic resonance evaluation of tubercular lesion in spine. Int Orthop. 2012;36(2):261–69. doi: 10.1007/s00264-011-1380-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindahl S, Nyman RS, Brismar J, et al. Imaging of tuberculosis. IV. Spinal manifestations in 63 patients. Acta Radiol. 1996;37(4):506–11. doi: 10.1177/02841851960373P215. [DOI] [PubMed] [Google Scholar]
- 6.Millar TM, McGrath P, McConnachie CC. Tuberculosis of the spine presenting with a cold abscess through the lumbar triangle of Petit. Clin Anat. 2007;20(3):329–31. doi: 10.1002/ca.20354. [DOI] [PubMed] [Google Scholar]
- 7.Suh KT, Seong YJ, Lee JS. Simultaneous anterior and posterior surgery in the management of tuberculous spondylitis with psoas abscess in patients with neurological deficits. Asian Spine J. 2008;2(2):94–101. doi: 10.4184/asj.2008.2.2.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang HQ, Lin MZ, Li JS, et al. One-stage posterior debridement, transforaminal lumbar interbody fusion and instrumentation in treatment of lumbar spinal tuberculosis: A retrospective case series. Arch Orthop Trauma Surg. 2013;133(3):333–41. doi: 10.1007/s00402-012-1669-2. [DOI] [PubMed] [Google Scholar]
- 9.Matsumoto T, Yamagami T, Morishita H, et al. CT-guided percutaneous drainage within intervertebral space for pyogenic spondylodiscitis with psoas abscess. Acta Radiol. 2012;53(1):76–80. doi: 10.1258/ar.2011.110418. [DOI] [PubMed] [Google Scholar]
- 10.Dinc H, Ahmetoglu A, Baykal S, et al. Image-guided percutaneous drainage of tuberculousiliopsoas and spondylodiskitic abscesses: Midterm results. Radiology. 2002;225(2):353–58. doi: 10.1148/radiol.2252011443. [DOI] [PubMed] [Google Scholar]
- 11.Dave BR, Kurupati RB, Shah D, et al. Outcome of percutaneous continuous drainage of psoas abscess: A clinically guided technique. Indian J Orthop. 2014;48(1):67–73. doi: 10.4103/0019-5413.125506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mak KC, Cheung KM. Surgical treatment of acute TB spondylitis: Indications and outcomes. Eur Spine J. 2013;22(Suppl 4):603–11. doi: 10.1007/s00586-012-2455-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Osmanagic A, Emamifar A, Christian Bang J, Jensen Hansen IM. A rare case of Pott’s disease (spinal tuberculosis) mimicking metastatic disease in the southern region of Denmark. Am J Case Rep. 2016;17:384–88. doi: 10.12659/AJCR.897555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Isik A, Deniz Firat Y, Peker K, et al. How could such a wide piece of tree root pass through the narrow pyloric orifice? An extremely rare case. Am J Case Rep. 2014;15:284–87. doi: 10.12659/AJCR.890713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Isik A, Karavas E, Peker K, et al. Male Mondor’s disease is a rare entity. Breast J. 2016;22(6):700–1. doi: 10.1111/tbj.12657. [DOI] [PubMed] [Google Scholar]
- 16.Ijaz M, Sakam S, Ashraf U, Marquez JG. Unusual presentation of recurrent pyogenic bilateral psoas abscess causing bilateral pulmonary embolism by iliac vein compression. Am J Case Rep. 2015;16:606–10. doi: 10.12659/AJCR.894206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Atkin G, Qurashi K, Isla A. Laparoscopic drainage of bilateral tuberculous psoas abscesses. Surg Laparosc Endosc Percutan Tech. 2005;15(6):380–82. doi: 10.1097/01.sle.0000191590.92108.c4. [DOI] [PubMed] [Google Scholar]
- 18.Buyukbebeci O, Seckiner I, Karsli B, et al. Retroperitoneoscopic drainage of complicated psoas abscesses in patients with tuberculous lumbar spondylitis. Eur Spine J. 2012;21(3):470–73. doi: 10.1007/s00586-011-2049-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clark RA, Towbin R. Abscess drainage with CT and ultrasound guidance. RadiolClin North Am. 1983;21(3):445–59. [PubMed] [Google Scholar]
- 20.Rawall S, Mohan K, Nene A. Posterior approach in thoracolumbar tuberculosis: A clinical and radiological review of 67 operated cases. Musculoskelet Surg. 2013;97(1):67–75. doi: 10.1007/s12306-012-0235-y. [DOI] [PubMed] [Google Scholar]
- 21.Liu J, Wan L, Long X, et al. Efficacy and safety of posterior versus combined posterior and anterior approach for the treatment of spinal tuberculosis: A meta-analysis. World Neurosurg. 2015;83(6):1157–65. doi: 10.1016/j.wneu.2015.01.041. [DOI] [PubMed] [Google Scholar]
- 22.Li J, Li XL, Zhou XG, et al. Surgical treatment for spinal tuberculosis with bilateral paraspinal abscess or bilateral psoas abscess: One-stage surgery. J Spinal Disord Tech. 2014;27(8):E309–14. doi: 10.1097/BSD.0000000000000120. [DOI] [PubMed] [Google Scholar]
- 23.Pang X, Shen X, Wu P, et al. Thoracolumbar spinal tuberculosis with psoas abscesses treated by one-stage posterior transforaminal lumbar debridement, interbody fusion, posterior instrumentation, and postural drainage. Arch Orthop Trauma Surg. 2013;133(6):765–72. doi: 10.1007/s00402-013-1722-9. [DOI] [PubMed] [Google Scholar]