Abstract
BACKGROUND
Intermittent administration of teriparatide, a drug composed of the first 34 amino acids of parathyroid hormone, has anabolic effects on bone. Although teriparatide has been evaluated for the treatment of osteoporosis and for the healing of fractures, clinical trials evaluating it for the treatment of osseous conditions of the oral cavity in humans are lacking.
METHODS
A total of 40 patients with severe, chronic periodontitis underwent periodontal surgery and received daily injections of teriparatide (20 μg) or placebo, along with oral calcium (1000 mg) and vitamin D (800 IU) supplementation, for 6 weeks. The patients were followed for 1 year. The primary outcome was a radiographic linear measurement of alveolar bone level. Secondary outcomes included clinical variables, bone turnover markers in serum and oral fluid, systemic bone mineral density, and quality of life.
RESULTS
Radiographic linear resolution of osseous defects was significantly greater after teriparatide therapy than after placebo beginning at 6 months, with a mean linear gain in bone at 1 year of 29% as compared with 3% (P<0.001). Clinical improvement was greater in patients taking teriparatide than in those taking placebo, with a reduction in periodontal probing depth of 33% versus 20% (2.42 mm vs. 1.32 mm) and a gain in clinical attachment level of 22% versus 7% (1.58 mm vs. 0.42 mm) in target lesions at 1 year (P = 0.02 for both comparisons). No serious adverse events were reported; however, the number of patients in the study was small. No significant differences were noted with respect to the other variables that were assessed.
CONCLUSIONS
Teriparatide, as compared with placebo, was associated with improved clinical outcomes, greater resolution of alveolar bone defects, and accelerated osseous wound healing in the oral cavity. Teriparatide may offer therapeutic potential for localized bone defects in the jaw. (Funded by the National Institutes of Health and others; ClinicalTrials.gov number, NCT00277706.)
Periodontitis affects more than one in five American adults, is a major cause of tooth loss, and is associated with systemic disorders such as diabetes mellitus, preterm low birth weight, and cardiovascular disease.1–5 Therefore, the development of predictable procedures to regenerate oral bone that is lost owing to developmental defects, trauma, or disease is desirable. A systemic anabolic agent to promote oral bone regeneration would be useful. Teriparatide, which consists of the first 34 amino acids of parathyroid hormone, is an anabolic agent approved by the Food and Drug Administration for the treatment of osteoporosis. Multiple clinical trials have shown that teriparatide is associated with increased bone mineral density and a reduced risk of fractures in patients with osteoporosis6–8; however, studies that assess the effects of teriparatide on osseous conditions of the oral cavity in humans are lacking. Preclinical studies suggest that lesions in the oral cavity, especially osseous wounds, may be a receptive target for the anabolic actions of teriparatide.9–11 We evaluated the effect of daily administration of teriparatide, in conjunction with an oral surgical procedure, on periodontal regeneration in men and women with severe periodontal disease.
METHODS
STUDY DESIGN
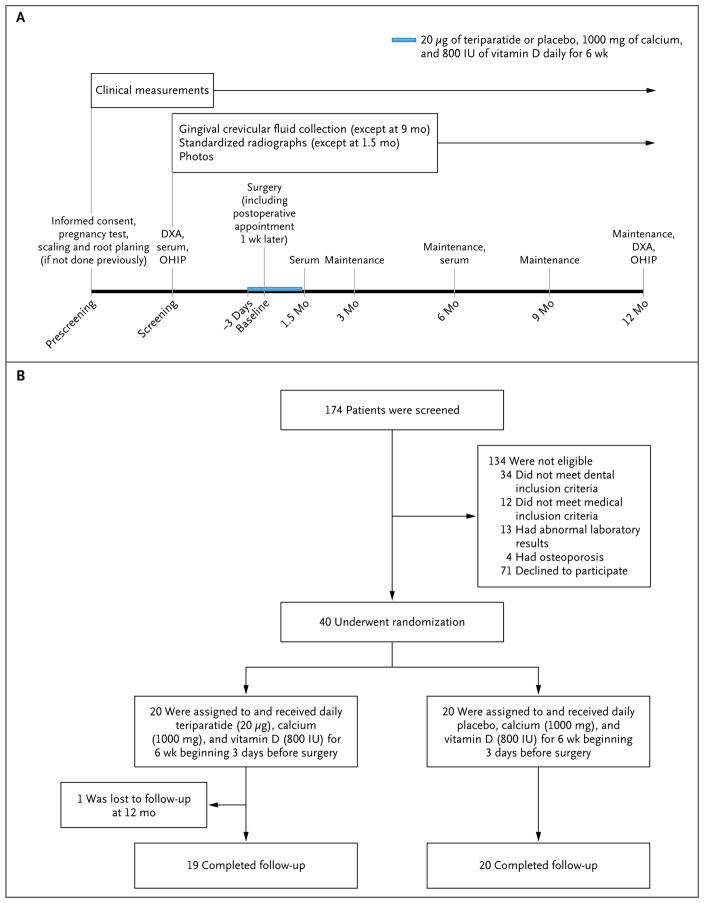
We conducted this single-center, randomized, placebo-controlled, double-blind, parallel-design clinical trial between January 20, 2005, and June 25, 2009 (Fig. 1). A total of 40 patients with severe periodontal disease underwent periodontal surgery in one sextant of the mouth and concurrently received either 20 μg of teriparatide or placebo daily, along with 1000 mg of calcium and 800 IU of vitamin D, for a 6-week period. The patients were followed for 1 year after surgery.
Figure 1. Study Design.
The timeline of events for the study is shown in Panel A. All patients received nonsurgical therapy (scaling and root planing) at least 4 weeks before surgery. Teriparatide or placebo was administered daily, along with 1000 mg of calcium and 800 IU of vitamin D daily, for 6 weeks beginning 3 days before surgery. Patients were evaluated over the course of 12 months after surgery. Serum refers to the collection of serum for assay; maintenance refers to a periodontal maintenance procedure that included supragingival and subgingival scaling and polishing. Screening, randomization, and follow-up of patients through the end of the study period are shown in Panel B. Only one patient (in the teriparatide group) was lost to follow-up at 12 months. In addition, another patient in the teriparatide group missed the 9-month visit, although she completed the study. DXA denotes dual-energy x-ray absorptiometry, and OHIP Oral Health Impact Profile quality-of-life survey.
PATIENTS
Men and women between 30 and 75 years of age with severe localized or generalized periodontal disease were eligible to participate in the study. Dental inclusion criteria were the presence of a vertical osseous defect adjacent to a tooth, accompanied by a periodontal probing depth of 6 mm or more and loss of a clinical attachment level of 6 mm or more. One periodontal osseous defect in each patient was selected for surgical treatment. At the time of surgery, the periodontal defects in the treated area were further classified on the basis of the number of remaining surfaces of supporting bone (one, two, or three bony walls). Bone fill in areas that had pathologic resorption in the area where roots diverge in a multirooted tooth (furcations) were not specifically included as outcome measures of the study. Additional inclusion criteria were normal serum calcium and parathyroid hormone levels, as well as 25-hydroxy-vitamin D levels of at least 16 ng per milliliter. Serum samples were analyzed independently at the Mayo Clinic. Dual-energy x-ray absorptiometry (DXA) was performed to evaluate the patient’s bone mineral density at the hip and spine. Patients were excluded from the study if they received a diagnosis of osteoporosis (bone mineral density T score of −2.5 or less). Additional exclusion criteria were metabolic bone disease, previous radiation treatment, cancer, growth hormone deficiency, conditions affecting calcium absorption, kidney disease, heavy smoking (>1 pack per day), pregnancy, and the use of medications that affect bone metabolism.
A total of 174 patients were screened, of whom 134 were not eligible: 34 did not meet the pre-specified dental inclusion criteria, 12 did not meet the medical inclusion criteria, 13 had abnormal serum test results, 4 had osteoporosis, and 71 declined to participate (Fig. 1).
STUDY OVERSIGHT
The institutional review board at the University of Michigan approved the study, which was designed by all the authors. Eli Lilly provided teriparatide for this study but had no role in the design of the study, the accrual or analysis of the data, or the preparation of the manuscript. The protocol, including the statistical analysis plan, is available with the full text of this article at NEJM.org. All the authors vouch for the accuracy and completeness of the data reported and for adherence to the protocol and to the statistical analysis plan. All patients provided written informed consent before enrollment.
PROTOCOL
The patients were randomly assigned to receive either teriparatide (20 μg) or placebo beginning 3 days before surgery and continuing for 6 weeks. Randomization was performed with the use of a computer-generated schedule in the pharmacy; teriparatide and placebo were dispensed in identical delivery devices. The study drugs were self-administered daily through subcutaneous injection in the thigh or abdomen. Patients also received 1000 mg of calcium and 800 IU of vitamin D daily as oral supplements.
Periodontal surgery consisted of a traditional open-flap débridement procedure in the oral region that was chosen for study (for a detailed description of the periodontal therapeutic procedures, see the Supplementary Appendix, available at NEJM.org). Under local anesthesia, gingival margin incisions were made on the lateral (facial) and medial (lingual) sides, and the gingival tissues, including periostea, were fully elevated to expose the underlying bone and the roots of the involved teeth. Meticulous débridement of root surfaces and granulomatous tissues was accomplished with the use of surgical curettes and ultrasonic scalers to remove bacterial deposits and inflamed soft tissues. After irrigation with saline, simple interrupted sutures (Gore-Tex suture CV-5, W.L. Gore and Associates) were used to re-approximate and secure the surgical flaps. No bone-replacement grafts or cell-occlusive membranes were used. A 0.12% chlorhexidine antimicrobial rinse was prescribed, along with 600 mg of ibuprofen or 5 mg of hydrocodone plus 500 mg of acetaminophen (or both ibuprofen and hydrocodone–acetaminophen), as needed for analgesia. Patients were instructed to refrain from brushing in the surgical area for 1 week and from flossing for 3 weeks. The sutures were removed at 1 week. Every 3 months after surgery, a periodontal maintenance procedure (including supragingival and subgingival scaling and polishing) was performed, and patients were given instruction in oral hygiene.
CLINICAL AND RADIOGRAPHIC ASSESSMENTS
Clinical variables, including periodontal probing depth, clinical attachment level, and bleeding on probing, were evaluated at baseline, 6 weeks, and 3, 6, 9, and 12 months. Full-mouth radiographs were obtained at baseline and 12 months. Peri-apical and bitewing radiographs of the surgical site were obtained at baseline and at 3, 6, 9, and 12 months. Radiographs were standardized with the use of bite registration material and an aluminum stepwedge of known density12,13 and were then analyzed with the use of Emago software (Oral Diagnostic Systems). We evaluated the bone gain in defects by measuring the linear distance from the deepest point of the defect to the first point at which complete bone fill was detected, beginning from the coronal aspect of the initial defect. Changes in the density of the defect were assessed after the defect was divided horizontally into apical, middle, and coronal thirds. The radiologist and periodontist conducted independent analyses of the radiographs; we determined interexaminer agreement and intraexaminer reproducibility by having the radiologist and periodontist independently analyze a separate set of radiographs and compare the results for accuracy. Radiographic measurements were completed in duplicate at least 1 week apart, and the results from the two clinicians were averaged.
OTHER ASSESSMENTS
Venous blood specimens were obtained at baseline, 6 weeks after surgery, and 6 months after surgery for measurements of levels of calcium, bone-specific alkaline phosphatase, and 25-hydroxyvitamin D. Samples of gingival crevicular fluid were obtained from the surgical site and five other randomly selected sites at baseline, 6 weeks, and 3, 6, and 12 months, according to standard protocols.14 Levels of bone biomarkers, including procollagen type 1 N-propeptide (P1NP), osteocalcin, and pyridinoline cross-linked carboxy-terminal propeptide of type 1 procollagen (ICTP), were determined. Systemic bone mineral density, measured with the use of DXA, was assessed at baseline and 12 months. The Oral Health Impact Profile (OHIP), a standardized oral-health quality-of-life survey, was administered at baseline and at 12 months.15
STATISTICAL ANALYSIS
A detailed calculation of sample size was difficult, since few studies have evaluated medications intended to augment local osseous repair in periodontal therapy. However, in one study of a selective cyclooxygenase-2 inhibitor in periodontal therapy, a sample of 22 patients per group was sufficient for the study to have 70% power to detect a 1-mm difference between the groups in the gain in clinical attachment level and reduction in probing depth,16 with a type I error rate of 5%.
The single surgical site in each patient was the unit of comparison. Therefore, the mesial and buccal periodontal measures corresponding to each surgical site were averaged before analysis by the two statisticians. Between-group differences in patient characteristics were assessed with the use of a Wilcoxon rank-sum test for continuous variables and a chi-square test of association for categorical variables. The significance of changes over time within the teriparatide and placebo groups was assessed with the use of a paired t-test, whereas between-group differences at each time point were assessed with the use of a two-sample t-test. In addition, generalized estimating equations were used to simultaneously examine the between-group differences at all time points, but they led to the same conclusions as those that resulted from the use of the two-sample t-tests. No patients dropped out of the study, and any intermittent missing data owing to missed appointments were assumed to be missing completely at random and were not imputed. P values of less than 0.05 were considered to indicate statistical significance; no adjustments have been made for multiple comparisons.
RESULTS
PATIENTS
The baseline demographic characteristics of the patients are shown in Table 1 (with additional information provided in Table 1 in the Supplementary Appendix). There were no significant differences between patients in the teriparatide group and those in the placebo group with respect to these characteristics. All the patients completed the drug-administration phase of the study. One patient in the teriparatide group was lost to follow-up at 12 months, and another patient in that group missed the 9-month visit but returned for the 12-month visit. We assessed adherence to the drug regimen by collecting all unused medication and monitoring serum bone-specific alkaline phosphatase levels, which were significantly elevated from baseline in patients in the teriparatide group at the 6-week assessment (P = 0.003), coinciding with the end of the period in which the study drug was administered (Fig. 2). Patients in both groups practiced acceptable oral hygiene throughout the study, as assessed at evaluation and maintenance visits.
Table 1.
Baseline Characteristics of the Patients.*
| Characteristic | Placebo (N = 20) | Teriparatide (N = 20) |
|---|---|---|
| Age — yr | ||
|
| ||
| Median | 57 | 48 |
|
| ||
| Range | 31–65 | 30–61 |
|
| ||
| Sex — no. (%) | ||
|
| ||
| Male | 6 (30) | 9 (45) |
|
| ||
| Female | 14 (70) | 11 (55) |
|
| ||
| Race or ethnic group — no. (%)† | ||
|
| ||
| White | 15 (75) | 15 (75) |
|
| ||
| Black | 4 (20) | 2 (10) |
|
| ||
| Asian | 1 (5) | 1 (5) |
|
| ||
| Hispanic | 0 | 1 (5) |
|
| ||
| Arabic | 0 | 1 (5) |
|
| ||
| Smoking status — no. (%) | ||
|
| ||
| Current smoker | 6 (30) | 9 (45) |
|
| ||
| Former smoker | 7 (35) | 5 (25) |
|
| ||
| Never smoked | 7 (35) | 6 (30) |
|
| ||
| Clinical measurements — mm | ||
|
| ||
| Clinical attachment level | 6.39±1.44 | 7.05±2.07 |
|
| ||
| Probing depth | 6.47±1.45 | 7.32±1.47 |
|
| ||
| Recession | 0.05±0.80 | 0.03±1.44 |
|
| ||
| Radiographic defect depth | 5.73±1.40 | 6.5±2.61 |
|
| ||
| Serum biomarkers‡ | ||
|
| ||
| Bone-specific alkaline phosphatase — μg/liter | 17.32±17.89 | 16.68±10.64 |
|
| ||
| 25-Hydroxyvitamin D — ng/ml | 28.10±11.37 | 28.9±7.92 |
|
| ||
| Calcium — mg/dl | 9.42±0.29 | 9.44±0.32 |
|
| ||
| Bone-density T score | ||
|
| ||
| Spine | −0.09±1.32 | −0.02±1.39 |
|
| ||
| Femur | −0.19±1.13 | −0.30±1.25 |
|
| ||
| Bone mineral density — g/cm3 | ||
|
| ||
| Spine | 1.20±0.17 | 1.21±0.18 |
|
| ||
| Femur | 1.02±0.15 | 1.01±0.17 |
Plus–minus values are means ±SD. No significant differences were noted between the groups at baseline.
Race or ethnic group was self-reported.
Normal values for bone-specific alkaline phosphatase are less than 22 μg per liter, the normal range for 25-hydroxyvitamin D is 25 to 80 ng per milliliter, and the normal range for calcium is 8.6 to 10.2 mg per deciliter. To convert the values for calcium to millimoles per liter, multiply by 0.25.
Figure 2. Changes in Serum Biomarkers over Time.
Mean levels of serum calcium (Panel A), 25-hydroxyvitamin D (Panel B), and bone-specific alkaline phosphatase (Panel C) are shown for the teriparatide and placebo groups at baseline, 6 weeks, and 6 months. All patients received vitamin D and calcium supplementation for a 6-week period, beginning 3 days before periodontal surgery. Levels of 25-hydroxyvitamin D were significantly higher than baseline levels in the placebo group at 6 weeks (P = 0.02). At 6 weeks, patients in the teriparatide group had a significantly greater increase from baseline in serum alkaline phosphatase levels than patients in the placebo group (P = 0.003). I bars indicate standard errors.
RADIOGRAPHIC FINDINGS
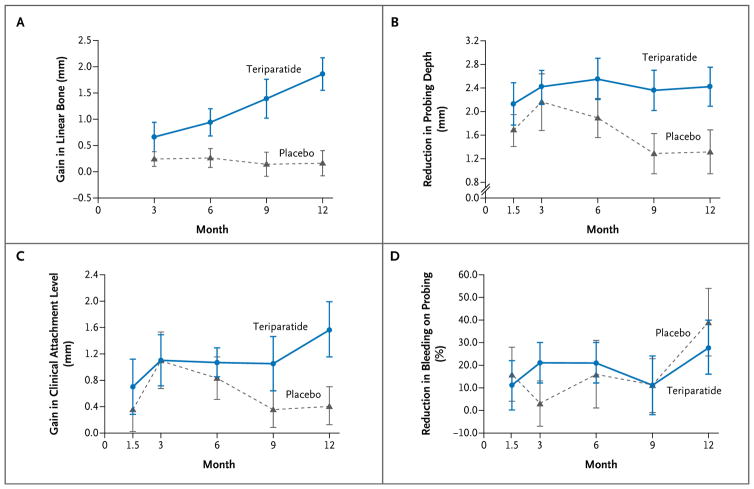
Periodontal surgery resulted in significant linear resolution of periodontal bone defects in the teriparatide group at 6, 9, and 12 months (P = 0.03, P = 0.004, and P<0.001 at the three time points, respectively) (Fig. 3). At 12 months, there was a mean linear gain in bone of 1.86 mm in patients in the teriparatide group, as compared with 0.16 mm in patients in the placebo group (P<0.001). In the teriparatide group, there was a trend toward increased bone density in the apical and middle portions of the defect (data not shown).
Figure 3. Changes in Radiographic and Clinical Variables over Time.
Mean gains in linear bone, as measured radiographically with the use of standardized bitewing radiographs, are shown in Panel A. Patients in the teriparatide group had significantly greater resolution of defects than did patients in the placebo group beginning at 6 months, with maximum resolution of defects at 12 months (P = 0.03, P = 0.004, and P<0.001 for the comparisons at 6, 9, and 12 months, respectively). Panel B shows the mean reductions from baseline in probing depth; Panel C, the mean gains in clinical attachment level; and Panel D, the mean reductions in bleeding on probing. Reductions in probing depth were significantly greater in patients in the teriparatide group than in patients in the placebo group at 9 and 12 months (P = 0.02). Gains in the clinical attachment level were significantly greater in patients in the teriparatide group at 12 months (P = 0.02). There were no significant between-group differences with respect to bleeding on probing. I bars indicate standard errors.
CLINICAL FINDINGS
Periodontal treatment was associated with improvement in clinical variables at the surgical site in both study groups (Fig. 3). At 12 months, the average reduction in probing depth was 2.42 mm in the teriparatide group, as compared with 1.32 mm in the placebo group (P = 0.02), and mean gains in the clinical attachment level were 1.58 mm as compared with 0.42 mm (P = 0.02). Bleeding on probing was reduced by 28% in the teriparatide group and by 39% in the placebo group at 12 months (P = 0.52). There was no significant difference between the groups in bleeding on probing at any time point.
At the outset of the study, many patients had localized severe, chronic periodontitis. Probing depths in nonsurgical sites were an average of 2.4 mm in patients in the placebo group and 2.8 mm in patients in the teriparatide group. No significant changes in probing depth were noted in nonsurgical sites in either the teriparatide group or the placebo group during the course of the study (data not shown).
SERUM BIOMARKERS
At 6 weeks, there was a transient increase in the bone-specific alkaline phosphatase level over the baseline level in patients taking teriparatide (mean increase, 1.9 μg per liter), whereas there was a decrease from the baseline level in patients taking placebo (mean decrease, 0.9 μg per liter) (P=0.003 for the change from baseline with teriparatide vs. placebo) (Fig. 2). Mean serum calcium levels remained stable in both groups throughout the study. Levels of 25-hydroxyvitamin D were significantly elevated at 6 weeks in patients taking placebo but returned to baseline levels by 6 months (P = 0.02).
ORAL-FLUID BIOMARKERS, BONE MINERAL DENSITY, AND QUALITY OF LIFE
No significant between-group differences were noted in the levels of bone biomarkers measured in oral-fluid samples (gingival crevicular fluid); however, in both groups, there was a trend toward an increase in P1NP (a marker of bone formation) at 6 weeks (data not shown). Systemic bone mineral density was calculated from DXA scans of the spine and femur areas. Five patients in the teriparatide group and nine in the placebo group had osteopenia as assessed by DXA, with no significant difference between the groups (Table 1). Changes from baseline to 12 months in bone mineral density and in the scores on the OHIP quality-of-life survey, as well as the difference in changes between the two groups at 12 months, were not significant (data not shown).
ADVERSE EVENTS
Adverse events occurred in 17.5% of the patients in the study (Table 2). There were no significant between-group differences in the incidence or type of adverse events reported. No elevated serum calcium levels were detected during the study. Clinical assessment revealed no deviation from the normal course of postsurgical healing in any patient.
Table 2.
Clinical Adverse Events.*
| Clinical Adverse Event | Placebo (N = 20) | Teriparatide (N = 20) |
|---|---|---|
| number of events | ||
| Injection-related | ||
|
| ||
| Dizziness | 1 | 2 |
|
| ||
| Nausea | 3 | 0 |
|
| ||
| Dyspnea | 0 | 1 |
|
| ||
| Bruising or redness at injection site | 2 | 0 |
|
| ||
| Headache | 0 | 2 |
|
| ||
| Tooth-related | ||
|
| ||
| Caries | 2 | 0 |
|
| ||
| Thermal sensitivity | 1 | 1 |
|
| ||
| Sensitive gingiva | 1 | 0 |
|
| ||
| Bruising at surgical site | 2 | 0 |
|
| ||
| Swelling at surgical site | 2 | 0 |
|
| ||
| Foreign body in surgical site | 1 | 0 |
|
| ||
| Thought to be unrelated to study or drug | 6 | 2 |
|
| ||
| Total | 21 | 8 |
For patients who had multiple adverse events, each event was reported separately. None of the adverse events were considered to be serious (as defined according to the Food and Drug Administration Safety Information and Adverse Event Reporting Program [www.fda.gov/Safety/MedWatch/HowToReport/ucm053087.htm]).
DISCUSSION
Administration of teriparatide in conjunction with periodontal surgery, as compared with periodontal surgery alone, was associated with improved clinical and radiographic outcomes. Previous studies of periodontal surgery have shown that gains in clinical attachment level of 0.2 to 1.5 mm and reductions in probing depth of 1.5 to 2.7 mm can be expected 1 year after surgery.17–20 The maximum healing response can occur in as short a period as 3 to 6 months, with a modest regression from maximum healing at 1 year.21 In our study, patients who received placebo had mean gains in clinical attachment level of 0.42 mm and mean reductions in probing depth of 1.32 mm at 12 months; these findings suggest that the overall improvement was consistent with that seen in previous studies.17–20
Patients in the teriparatide group, as compared with patients in the placebo group, had significant reductions in probing depth at 9 and 12 months, suggesting that a short dosing regimen may have long-lasting effects. Similarly, gains in clinical attachment levels continued to be seen throughout the course of the study in the teriparatide group, whereas the maximum gain occurred at 3 months in the placebo group. No patient had any regenerative space-maintaining material (such as a bone graft or cell-occlusive barrier) placed in the area of the defect. This lack of a space provision for a vertical lesion suggests that there was a different mechanism for the neogenesis of new periodontal tissues.
Bone gain in the osseous defects, as assessed radiographically, began early in the patients receiving teriparatide, and these patients continued to have improvement over the course of 12 months, resulting in greater — and highly significant — overall linear bone gain than that which occurred in patients receiving placebo. These results suggest that teriparatide may play an important role in improving and sustaining alveolar bone gain. The radiographic results are consistent with observed changes in clinical variables in this study. Linear bone gain after traditional periodontal surgery without regenerative space-maintaining material is minimal, with improvement beginning as early as 6 months and reported gains ranging from 0.3 to 1.1 mm at 12 months, an outcome that is consistent with the radiographic results of the patients in the placebo group in our study.17–20,22–24
Few clinical studies have evaluated the effect of local and systemic biologic modifiers, such as platelet-derived growth factor (PDGF), fibroblast growth factor 2, low-dose doxycycline, and enamel matrix derivative, on periodontal regeneration in the oral cavity.21,25–28 A multicenter study evaluated local delivery of PDGF to stimulate bone fill and promote improvement in the clinical attachment level in persons with periodontal defects.28 PDGF in a carrier, as compared with the carrier alone, was associated with significantly more gain in the clinical attachment level at 3 months, but not at 6 months, and greater gain in linear bone at 6 months. Similarly, a randomized, controlled study showed that local application of enamel matrix derivative, as compared with traditional periodontal flap surgery, resulted in a greater reduction in radiographic linear defects and a greater gain in clinical attachment levels.26 Two studies showed that there were significantly greater reductions in probing depth and gains in clinical attachment levels with low-dose doxycycline in conjunction with periodontal surgery, as compared with surgery alone, but the effect was not sustained after the doxycycline was withdrawn.21,25 A recent randomized, controlled trial compared periodontal surgery with and without local application of fibroblast growth factor 2.27 At 36 weeks, the application of fibroblast growth factor 2 was associated with a trend toward increased gain in alveolar bone height, as assessed radiographically. In the present study, a 6-week regimen of teriparatide appeared to have sustained positive clinical results up to 12 months after surgery, suggesting that teriparatide also had a positive effect on newly formed bone in the wound site. The positive time-dependent results may be due to accelerated early events, such as an increase in the activity or number of osteoblasts that is manifested as increased bone production months after the drug is administered.29
Systemic administration of antiresorptive agents such as bisphosphonates has been suggested as a means to enhance nonsurgical periodontal therapy.30–35 There have been conflicting findings, with some studies showing improved clinical outcomes with bisphosphonate therapy33–35 and others showing no additional benefit.30,31 However, clinical trials evaluating bisphosphonate therapy to improve surgical outcomes are lacking. Furthermore, osteonecrosis of the jaw is considered to be a potential side effect of bisphosphonate therapy and has been associated with surgical trauma to the jaw.36 Several reports have suggested that teriparatide might be an alternative treatment for patients with osteoporosis in whom periodontal surgery is planned.37,38
A study of fracture repair suggested that teriparatide preferentially enhances bone remodeling and wound healing in areas of high bone turnover, such as fractures and surgical sites.6,39 Thus, the oral cavity may be an ideal therapeutic target for teriparatide, especially when it is administered in conjunction with periodontal surgery. Future clinical applications of this approach might incorporate a local delivery system, as has been used in preclinical animal models,11,40 to concentrate the drug within the oral cavity.
Our study has several limitations. Because the study sample was small, the results should be interpreted with caution. In addition, adverse events that do not occur at high frequency could not be detected.
In summary, our trial showed that teriparatide administration for 6 weeks, as compared with placebo, in conjunction with periodontal surgery, was associated with greater resolution of osseous defects in patients with severe periodontal disease and with significantly better clinical outcomes during the year of observation after surgery.
Supplementary Material
Acknowledgments
Supported in part by Eli Lilly, the American Academy of Periodontology Foundation Tarrson Regeneration Scholarship, and a grant (UL1RR024986) from the National Center for Research Resources, National Institutes of Health, to the University of Michigan Clinical Research Unit.
We thank Lea Franco, Mallory Mitchell, Jim Sugai, and Kemal Ustun for assistance with the gingival crevicular fluid assays; Jonathan Ee, Henry Mallett, and JooHyung Choi for help with data entry; and Lindsay Rayburn for advice regarding radiographic analysis.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Curtis JW., Jr Infections associated with diabetes mellitus. N Engl J Med. 2000;342:895–6. [PubMed] [Google Scholar]
- 2.Michalowicz BS, Hodges JS, DiAngelis AJ, et al. Treatment of periodontal disease and the risk of preterm birth. N Engl J Med. 2006;355:1885–94. doi: 10.1056/NEJMoa062249. [DOI] [PubMed] [Google Scholar]
- 3.Tonetti MS, D’Aiuto F, Nibali L, et al. Treatment of periodontitis and endothelial function. N Engl J Med. 2007;356:911–20. doi: 10.1056/NEJMoa063186. [DOI] [PubMed] [Google Scholar]
- 4.Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366:1809–20. doi: 10.1016/S0140-6736(05)67728-8. [DOI] [PubMed] [Google Scholar]
- 5.Offenbacher S, Beck JD, Moss K, et al. Results from the Periodontitis and Vascular Events (PAVE) Study: a pilot multi-centered, randomized, controlled trial to study effects of periodontal therapy in a secondary prevention model of cardiovascular disease. J Periodontol. 2009;80:190–201. doi: 10.1902/jop.2009.080007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aspenberg P, Genant HK, Johansson T, et al. Teriparatide for acceleration of fracture repair in humans: a prospective, randomized, double-blind study of 102 post-menopausal women with distal radial fractures. J Bone Miner Res. 2010;25:404–14. doi: 10.1359/jbmr.090731. [DOI] [PubMed] [Google Scholar]
- 7.Dempster DW, Cosman F, Kurland ES, et al. Effects of daily treatment with parathyroid hormone on bone microarchitecture and turnover in patients with osteoporosis: a paired biopsy study. J Bone Miner Res. 2001;16:1846–53. doi: 10.1359/jbmr.2001.16.10.1846. [DOI] [PubMed] [Google Scholar]
- 8.Neer RM, Arnaud CD, Zanchetta JR, et al. Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344:1434–41. doi: 10.1056/NEJM200105103441904. [DOI] [PubMed] [Google Scholar]
- 9.Barros SP, Silva MA, Somerman MJ, Nociti FH., Jr Parathyroid hormone protects against periodontitis-associated bone loss. J Dent Res. 2003;82:791–5. doi: 10.1177/154405910308201006. [DOI] [PubMed] [Google Scholar]
- 10.Schneider A, Taboas JM, McCauley LK, Krebsbach PH. Skeletal homeostasis in tissue-engineered bone. J Orthop Res. 2003;21:859–64. doi: 10.1016/S0736-0266(03)00042-1. [DOI] [PubMed] [Google Scholar]
- 11.Jung RE, Cochran DL, Domken O, et al. The effect of matrix bound parathyroid hormone on bone regeneration. Clin Oral Implants Res. 2007;18:319–25. doi: 10.1111/j.1600-0501.2007.01342.x. [DOI] [PubMed] [Google Scholar]
- 12.Duckworth JE, Judy PF, Goodson JM, Socransky SS. A method for the geometric and densitometric standardization of intraoral radiographs. J Periodontol. 1983;54:435–40. doi: 10.1902/jop.1983.54.7.435. [DOI] [PubMed] [Google Scholar]
- 13.Reddy MS, Jeffcoat MK. Digital subtraction radiography. Dent Clin North Am. 1993;37:553–65. [PubMed] [Google Scholar]
- 14.Giannobile WV, Lynch SE, Denmark RG, Paquette DW, Fiorellini JP, Williams RC. Crevicular fluid osteocalcin and pyridinoline cross-linked carboxyterminal telopeptide of type I collagen (ICTP) as markers of rapid bone turnover in periodontitis: a pilot study in beagle dogs. J Clin Periodontol. 1995;22:903–10. doi: 10.1111/j.1600-051x.1995.tb01793.x. [DOI] [PubMed] [Google Scholar]
- 15.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 16.Sculean A, Berakdar M, Donos N, Auschill TM, Arweiler NB. The effect of postsurgical administration of a selective cyclo-oxygenase-2 inhibitor on the healing of intrabony defects following treatment with enamel matrix proteins. Clin Oral Investig. 2003;7:108–12. doi: 10.1007/s00784-003-0200-0. [DOI] [PubMed] [Google Scholar]
- 17.Pihlstrom BL, Oliphant TH, McHugh RB. Molar and nonmolar teeth compared over 6 1/2 years following two methods of periodontal therapy. J Periodontol. 1984;55:499–504. doi: 10.1902/jop.1984.55.9.499. [DOI] [PubMed] [Google Scholar]
- 18.Isidor F, Karring T. Long-term effect of surgical and non-surgical periodontal treatment: a 5-year clinical study. J Periodontal Res. 1986;21:462–72. doi: 10.1111/j.1600-0765.1986.tb01482.x. [DOI] [PubMed] [Google Scholar]
- 19.Heitz-Mayfield LJ, Trombelli L, Heitz F, Needleman I, Moles D. A systematic review of the effect of surgical debridement vs non-surgical debridement for the treatment of chronic periodontitis. J Clin Periodontol. 2002;29(Suppl 3):92–102. 160–2. doi: 10.1034/j.1600-051x.29.s3.5.x. [DOI] [PubMed] [Google Scholar]
- 20.Bhongade ML, Tiwari IR. A comparative evaluation of the effectiveness of an anorganic bone matrix/cell binding peptide with an open flap debridement in human infrabony defects: a clinical and radiographic study. J Contemp Dent Pract. 2007;8:25–34. [PubMed] [Google Scholar]
- 21.Gapski R, Hasturk H, Van Dyke TE, et al. Systemic MMP inhibition for periodontal wound repair: results of a multi-centre randomized-controlled clinical trial. J Clin Periodontol. 2009;36:149–56. doi: 10.1111/j.1600-051X.2008.01351.x. [DOI] [PubMed] [Google Scholar]
- 22.Dybvik T, Leknes KN, Bøe OE, Skavland RJ, Albandar JM. Bioactive ceramic filler in the treatment of severe osseous defects: 12-month results. J Periodontol. 2007;78:403–10. doi: 10.1902/jop.2007.060263. [DOI] [PubMed] [Google Scholar]
- 23.Laurell L, Gottlow J, Zybutz M, Persson R. Treatment of intrabony defects by different surgical procedures: a literature review. J Periodontol. 1998;69:303–13. doi: 10.1902/jop.1998.69.3.303. [DOI] [PubMed] [Google Scholar]
- 24.Shirakata Y, Setoguchi T, Machigashira M, et al. Comparison of injectable calcium phosphate bone cement grafting and open flap debridement in periodontal intrabony defects: a randomized clinical trial. J Periodontol. 2008;79:25–32. doi: 10.1902/jop.2008.070141. [DOI] [PubMed] [Google Scholar]
- 25.Gapski R, Barr JL, Sarment DP, Layher MG, Socransky SS, Giannobile WV. Effect of systemic matrix metalloproteinase inhibition on periodontal wound repair: a proof of concept trial. J Periodontol. 2004;75:441–52. doi: 10.1902/jop.2004.75.3.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heijl L, Heden G, Svärdström G, Ostgren A. Enamel matrix derivative (EMDOGAIN) in the treatment of intrabony periodontal defects. J Clin Periodontol. 1997;24:705–14. doi: 10.1111/j.1600-051x.1997.tb00253.x. [DOI] [PubMed] [Google Scholar]
- 27.Kitamura M, Nakashima K, Kowashi Y, et al. Periodontal tissue regeneration using fibroblast growth factor-2: randomized controlled phase II clinical trial. PLoS One. 2008;3(7):e2611. doi: 10.1371/journal.pone.0002611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nevins M, Giannobile WV, McGuire MK, et al. Platelet-derived growth factor stimulates bone fill and rate of attachment level gain: results of a large multi-center randomized controlled trial. J Periodontol. 2005;76:2205–15. doi: 10.1902/jop.2005.76.12.2205. [DOI] [PubMed] [Google Scholar]
- 29.Pettway GJ, Meganck JA, Koh AJ, Keller ET, Goldstein SA, McCauley LK. Parathyroid hormone mediates bone growth through the regulation of osteoblast proliferation and differentiation. Bone. 2008;42:806–18. doi: 10.1016/j.bone.2007.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.El-Shinnawi UM, El-Tantawy SI. The effect of alendronate sodium on alveolar bone loss in periodontitis (clinical trial) J Int Acad Periodontol. 2003;5:5–10. [PubMed] [Google Scholar]
- 31.Graziani F, Cei S, Guerrero A, et al. Lack of short-term adjunctive effect of systemic neridronate in non-surgical periodontal therapy of advanced generalized chronic periodontitis: an open label-randomized clinical trial. J Clin Periodontol. 2009;36:419–27. doi: 10.1111/j.1600-051X.2009.01388.x. [DOI] [PubMed] [Google Scholar]
- 32.Jeffcoat MK, Cizza G, Shih WJ, Genco R, Lombardi A. Efficacy of bisphosphonates for the control of alveolar bone loss in periodontitis. J Int Acad Periodontol. 2007;9:70–6. [PubMed] [Google Scholar]
- 33.Lane N, Armitage GC, Loomer P, et al. Bisphosphonate therapy improves the outcome of conventional periodontal treatment: results of a 12-month, randomized, placebo-controlled study. J Periodontol. 2005;76:1113–22. doi: 10.1902/jop.2005.76.7.1113. [DOI] [PubMed] [Google Scholar]
- 34.Rocha ML, Malacara JM, Sánchez-Marin FJ, Vazquez de la Torre CJ, Fajardo ME. Effect of alendronate on periodontal disease in postmenopausal women: a randomized placebo-controlled trial. J Periodontol. 2004;75:1579–85. doi: 10.1902/jop.2004.75.12.1579. [DOI] [PubMed] [Google Scholar]
- 35.Takaishi Y, Ikeo T, Miki T, Nishizawa Y, Morii H. Suppression of alveolar bone resorption by etidronate treatment for periodontal disease: 4- to 5-year follow-up of four patients. J Int Med Res. 2003;31:575–84. doi: 10.1177/147323000303100614. [DOI] [PubMed] [Google Scholar]
- 36.Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004;62:527–34. doi: 10.1016/j.joms.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 37.Lau AN, Adachi JD. Resolution of osteonecrosis of the jaw after teriparatide [recombinant human PTH-(1–34)] therapy. J Rheumatol. 2009;36:1835–7. doi: 10.3899/jrheum.081176. [DOI] [PubMed] [Google Scholar]
- 38.Harper RP, Fung E. Resolution of bisphosphonate-associated osteonecrosis of the mandible: possible application for intermittent low-dose parathyroid hormone [rhPTH (1–34)] J Oral Maxillofac Surg. 2007;65:573–80. doi: 10.1016/j.joms.2006.10.076. [DOI] [PubMed] [Google Scholar]
- 39.Tsiridis E, Morgan EF, Bancroft JM, et al. Effects of OP-1 and PTH in a new experimental model for the study of metaphyseal bone healing. J Orthop Res. 2007;25:1193–203. doi: 10.1002/jor.20420. [DOI] [PubMed] [Google Scholar]
- 40.Jung RE, Hämmerle CH, Kokovic V, Weber FE. Bone regeneration using a synthetic matrix containing a parathyroid hormone peptide combined with a grafting material. Int J Oral Maxillofac Implants. 2007;22:258–66. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.