Supplemental Digital Content is available in the text.
Key Words: hypoglycemia, type II diabetes, social determinants of health, food insecurity, emergency room visits, hospitalization
Abstract
Background:
Multipayer initiatives have sought to address social determinants of health, such as food insecurity, by linking primary care patients to social services. It remains unclear whether such social determinants contribute to avoidable short-term health care costs.
Objectives:
We sought to quantify costs and mitigating factors for the increased risk of hypoglycemia at the end of each month among low-income Americans, a phenomenon related to exhaustion of food budgets.
Research Design:
We used claims data on 595,770 commercially insured American adults aged 19 through 64 years old from 2004 through 2015 to estimate the risks and costs of emergency room visits and inpatient hospitalizations for hypoglycemia during the last week of each month versus prior weeks.
Results:
Although persons with household incomes greater than the national median did not experience a monthly cycle of hypoglycemia, those with incomes less than the national median had an odds ratio of 1.07 (95% confidence interval, 1.02–1.12; P=0.005) for emergency room visits or inpatient hospitalizations for hypoglycemia during the last week of each month, compared with earlier weeks. The risk of end-of-the-month hypoglycemia was mitigated to statistical insignificance during a period of increased federal nutrition program benefits from 2009 through 2013. Eliminating the monthly cycle of hypoglycemia among commercially insured nonelderly adults would be expected to avert $54.1 million per year (95% confidence interval, $0.8–$204.0) in emergency department and inpatient hospitalization costs.
Conclusions:
Addressing the end-of-the-month increase in hypoglycemia risk among lower-income populations may avert substantial costs from emergency department visits and inpatient hospitalizations.
Recent health care payment reform initiatives have focused on strategies to address social determinants of health—such as food, housing, and income insecurity—as a routine part of primary care. For example, addressing social determinants of health is a major focus of the State Innovation Models and Accountable Health Communities programs, in which insurers (including Medicare, Medicaid, and private payers) fund primary care practices to link lower-income populations to social services.1,2 Addressing inadequate income to pay for food has been the focus of some recent health care–based interventions, such as programs to “prescribe” food to lower-income populations by referring patients from primary care practices to food pantries, or providing onsite support for enrollment in federal nutrition programs.3,4 Although social determinants of health, such as having inadequate income for food clearly contribute to morbidity and mortality, the introduction of payer initiatives to address social determinants remains heavily debated.5–10 It remains particularly unclear whether such social determinants contribute to avoidable short-term health care costs, such that payers should expect to reduce short-term health care expenditures through such initiatives.11
The social determinant of food insecurity—the state of being without reliable access to a sufficient quantity of affordable, nutritious food12—is associated with worsened outcomes for chronic diseases such as type 2 diabetes.5,7–10 A major source of concern is whether food insecurity may contribute to hypoglycemia, which is increasingly recognized as a major adverse event and safety indicator in diabetes care.13,14 Hypoglycemia may be a risk among people with inadequate food access who continue taking hypoglycemic medications such as those used to treat type II diabetes. Numerous studies conducted in clinical populations of low-income patients have demonstrated increased hypoglycemia risk among food insecure patients compared with food secure patients.7,15 Adults with diabetes queuing for food at food pantries are also more likely to report experiencing hypoglycemia if they are food insecure.
A heightened risk of hypoglycemia among low-income populations was also observed in a study using aggregate data from the state of California from 2000 through 2008, in which hospitalizations for hypoglycemia were found to be 29% higher among people living in lowern–median-income ZIP codes compared with higher–median-income ZIP codes.16 The source of the increase in hospitalizations remains unclear. Social factors associated with living in a lower-income ZIP code, besides food insecurity (such as having inadequate access to primary care services that could avert emergency room visits), could explain this finding; many lower-income populations receive Medicaid, which is accepted at fewer primary care practices such that recipients have higher emergency department utilization for avoidable disease complications like hypoglycemia.17 However, the California study also reported an elevated risk of hypoglycemia admission in the last week of the month in low-income ZIP codes, suggesting that food insecurity may be directly related to an elevated risk of hypoglycemia. Exhaustion of income to pay for food at the end of each month is part of a “pay cycle” that develops among poor households as paychecks, disability funds, welfare funds, and nutritional program funds are generally distributed at the beginning of each month and are exhausted by month’s end.18 If exhaustion of food budgets is truly a contributor to increased end-of-month hypoglycemia among lower-income populations, then increased food aid to such populations should reduce the risk of end-of-the-month hypoglycemia.
Here, we test whether emergency room visits and hospital admissions for hypoglycemia are in fact heightened among lower-income populations nationwide toward the end of each month, using data from a large, commercially insured cohort to reduce the possibility of confounding by differential access to primary care among persons with Medicaid. We test the hypothesis that the end-of-the-month hypoglycemia would be mitigated by the American Recovery and Reinvestment Act (ARRA) of 2009, which increased food budget support for low-income populations through the Supplemental Nutrition Assistance Program (SNAP).19 We also calculate the costs of care for hypoglycemic emergency room visits and hospital admissions attributable to the end-of-the-month “pay cycle” effect, incorporating comprehensive data on both patient and payer cost burdens.
METHODS
Study Sample
Data were obtained from the Optum Clinformatics Data Mart, which collects administrative health claims for members of a large national managed care company. Claims data are verified, adjudicated, adjusted with a standard pricing methodology to account for differences in pricing across health plans and provider contracts, and deidentified before inclusion in the Data Mart dataset. For this analysis, data were comprised of health plan claims from all 50 states for commercially insured individuals over the period January 2004 through September 2015. The data include demographics (age, sex, race/ethnicity, and income from enrollment applications) and all medical claims data (outpatient and inpatient visits, International Classification of Disease series 9 diagnostic codes, laboratory results, pharmaceutical prescriptions, charges, copayments, deductibles, coinsurance fees, and insurance payments). Income data were available in 5 general categories to reduce the risk of identifiability (<$40,800, $40,800–<$51,000, $51,000–<$61,200, $61,200–<$76,500, $76,500–<$102,000, and ≥$102,000 in household size-adjusted and inflation-adjusted 2016 real US$). The study was restricted to exclusively commercially insured adults aged 19 through 64 years old, to reduce the influence of differential primary care access among Children’s Health Insurance Program and Medicare-eligible participants. The study sample is considered typical of the commercially insured population in the United States.20
Primary and Secondary Outcomes
The primary outcome was defined as an emergency room visit or inpatient hospital admission for a principal diagnosis of hypoglycemia present at the time of visit or admission. Hypoglycemia was identified using an algorithm (validated against both chart review and laboratory values) that included a primary visit diagnosis for hypoglycemia by ICD-9 code and a secondary diagnosis of type 2 diabetes, but excluded cases for which secondary hypoglycemia could be induced by infection or other comorbid condition, or occurred during hospitalization rather than being the cause of hospitalization (eg, due to medication error).21 Note that a diagnostic code-based algorithm validated against both chart review and laboratory assessment was used, instead of laboratory values alone, because routine guidelines for clinical practice by paramedics and emergency department physicians often call for immediate treatment of suspected hypoglycemia with dextrose, even before glucometer or venous blood draws have been conducted.22 Secondary outcomes included the cost of emergency room visits and of inpatient hospital admissions for hypoglycemia, and the estimated total cost savings if the elevated risk of hypoglycemia among lower-income persons during the last 7 days of the month were eliminated (ie, equaled the average risk during the previous days of the month). Costs were defined as total standardized gross payments (not charges) to all providers and facilities associated with an emergency room visit or inpatient hospitalization for a primary visit diagnosis of hypoglycemia, including both commercial insurance payments as well as patient copayments, deductibles, and coinsurance fees, following current costing guidelines.23 We calculated the total cost savings to the commercial insurance market per year if the monthly cycle among lower-income persons were eliminated, by multiplying independent estimates of the size of the commercially insured lower-income nonelderly adult population in the United States (19,907,300 adults aged 19 through 64 as of November 201624) by the annualized per capita difference in emergency room visit and inpatient hospitalization probabilities for hypoglycemia during the last 7 days of the month versus all previous days of the month, multiplied by the costs of those emergency room visits and inpatient hospitalizations among the lower-income persons in our dataset. Lower/higher income was defined by the cutoff of $51,000 for a family of 4, the closest available cut-point in our dataset to the median household size-adjusted and inflation-adjusted US household income of $53,895/year (in 2016 real US$).25 The reasons for choosing this cut-point were that it includes not only the low-income cutoff for SNAP participation, but also accounts for the fact that most states (covering 91% of SNAP recipients) use a system of broad-based categorical eligibility (which increases the threshold to 200% of the federal poverty guideline in several states); accounts for substantial deductions before considering SNAP eligibility; and includes marginal lower-income Americans with substantial food insecurity who do not qualify for SNAP.26,27
Statistical Analyses
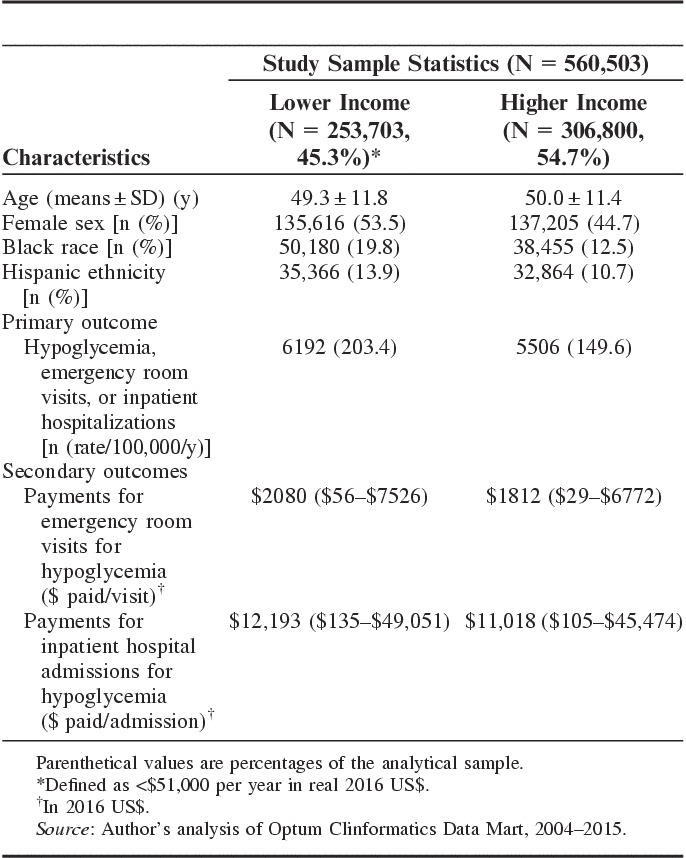
Multivariate logistic regression analyses were performed. Covariates (age, sex, race, and ethnicity) are defined in Table 1.
TABLE 1.
Demographics and Frequency of Primary and Secondary Outcomes Among the Study Sample
First, we regressed the primary outcome against the covariates of age, age-squared, sex, black race, Hispanic ethnicity, income category, year of visit, and a dummy variable designating the last week (last 7 d) of the month, among the lower-income population subset, and again among the higher-income population subset. We additionally tested a form of the regression model in which we explicitly tested for heterogenous treatment effects by income level,28 by running the regression with the above covariates among the entire population, and testing the interaction term between whether the visit/admission for hypoglycemia was in the last week of the month and whether a person was lower income by the above criteria.
Second, we assessed whether the association between the week of the month and the risk of emergency room visits or inpatient hospitalizations for hypoglycemia was consistent among lower-income populations during the ARRA stimulus (May 2009 to October 2013) and during nonstimulus periods. ARRA increased the monthly benefit for participants of the SNAP from $115 to $135 on an average (a 17% increase).19 We tested for effect modification by creating a dummy variable for the period of the stimulus and estimating the odds ratio (OR) of the primary outcome during the last week of the month by income level during the stimulus period and during nonstimulus periods (ie, the individual-level equivalent to aggregate-level interrupted time series analysis).29
Third, we computed the average cost for emergency room visits and hospital admissions per person for hypoglycemia (in 2016 real US$), winsorizing at the 5th and 95th percentiles to omit outliers.
Finally, we repeated our analysis with a falsification test to help ensure that any observed association between per-person rate of emergency room visits or inpatient hospital admissions for hypoglycemia was due to pathophysiologically plausible pay cycle effects rather than residual confounding. We repeated the analysis with the per-person rate of emergency room visits or inpatient hospital admissions for appendicitis (as identified by ICD-9 codes 540–541), which should not be affected by a pay cycle. We tested whether we could reject the hypothesis that there would be no within-month variation in appendicitis visit rates; rejecting such a hypothesis by finding a significant within-month variation in appendicitis visits would suggest spurious associations between week of the month and visit rate, due to residual confounding.
No missing data were imputed, as complete claims data were obtained. Analyses were performed in Stata version 14 (StataCorp, Austin, TX). The analysis was approved by the Stanford University Institutional Review Board (e-protocol #39274). A comprehensive STROBE checklist for observational data analysis is provided in the Appendix (Supplemental Digital Content, http://links.lww.com/MLR/B370).
RESULTS
Descriptive Statistics on the Study Sample
Descriptive statistics on the study sample are provided in Table 1. The sample included 560,503 unique individuals who had at least 1 medical encounter (emergency room visit and/or inpatient hospitalization for any diagnosis) during the study period. This sample of participants had a mean age of 49.7 years old; 48.7% were female, 15.8% were of black race, 12.2% were of Hispanic ethnicity, and 45.3% lived in lower-income households (less than the national median household income). The individuals experienced a total of 1,332,738 unique emergency department visits and/or inpatient hospitalizations, of which the primary outcome of an emergency department visit or inpatient hospitalization for hypoglycemia occurred among 6192 lower-income and 5506 higher-income persons, for a hypoglycemia visit/admission rate 203.4 per 100,000 persons per year among the lower-income population, and 149.6 per 100,000 persons per year among the higher-income population.
Risk of Primary and Secondary Outcomes
Results of the main statistical analysis are illustrated in Figure 1 and Appendix Table 1 (Supplemental Digital Content, http://links.lww.com/MLR/B370). Among the lower-income population (less than the national median household income), the OR of the primary outcome of an emergency room visit or inpatient hospitalization for hypoglycemia during the last week of each month was 1.07 [95% confidence interval (CI), 1.02–1.12; P=0.005] versus the other weeks of the month, after controlling for age, age-squared, sex, race, ethnicity, year, and income group. The effect was more pronounced among the lowest-income category (OR=1.09, among persons with income <$40,800) than the second lowest-income group (OR=1.06, among persons with income $40,800–<$51,000), and scaled further down with higher income (OR=1.02, among persons with income $51,000–<$61,200; OR=0.99, for those with income $61,200–<$76,500; OR=0.96 for those with income $76,500–<$102,000; and OR=0.92, for those with income ≥$102,000). Among the higher-income population, the OR of the primary outcome of an emergency room visit or inpatient hospitalization for hypoglycemia during the last week of each month was 0.98 (95% CI, 0.93–1.03; P=0.457) versus the other weeks of the month, after including the control variables.
FIGURE 1.
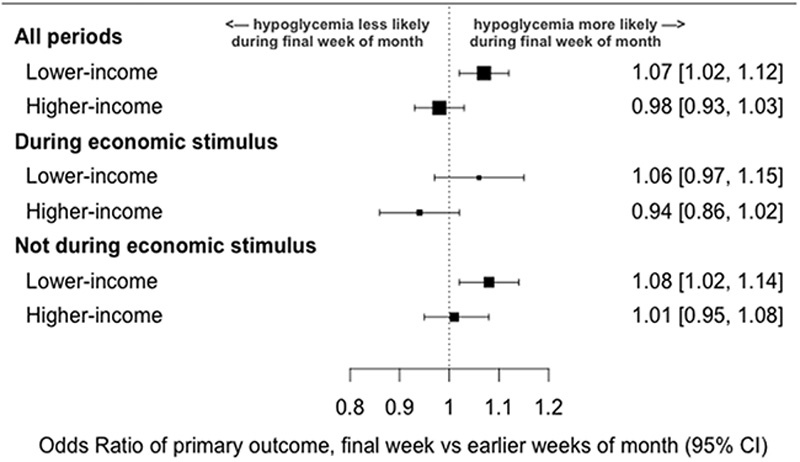
Risk of emergency room visits or inpatient hospitalizations for hypoglycemia among a commercially insured sample of nonelderly US adults (N=560,503)*. *Lower income is defined as lower than the US national household median income (<$51,000) in 2016 real US$. The primary outcome is emergency room visits or inpatient hospital admissions for hypoglycemia. All odds ratios were estimated after controlling for age, age-squared, sex, race, ethnicity, year, and categorical income level as defined in the main text. The economic stimulus period refers to the American Recovery and Reinvestment Act (ARRA) stimulus from May 2009 through October 2013. CI indicates confidence interval. Source: Author’s analysis of Optum Clinformatics Data Mart, 2004–2015.
In the regression model testing the 2 main effects (being in the last week of the month and having a household income lower than the national median), and the interaction term between the 2 main effects among the full study sample, the OR of the primary outcome during the last week of the month versus the other weeks was 0.98 (95% CI, 0.93–1.03; P=0.464), whereas the OR of the primary outcome if having an income less than the national median versus higher was 1.10 (95% CI, 1.03–1.17; P=0.007), and the OR of the interaction term between being in the last week of the month and having an income lower than the national median was 1.09 (95% CI, 1.02–1.17; P=0.014), after including the other control variables.
The risk of end-of-the-month hypoglycemia among the lower-income population was nonsignificant during the ARRA stimulus period but significant during nonstimulus periods. Among the lower-income population, the OR of the primary outcome during the last week of the month versus the previous weeks was 1.06 (95% CI, 0.97–1.15; P=0.208) during the ARRA stimulus, versus 1.08 (95% CI, 1.02–1.14; P=0.011; both 1.08 before and 1.08 after) during the nonstimulus period, after controlling for age, age-squared, sex, race, ethnicity, year, and income group. Among the higher-income population, the OR of the primary outcome during the last week of the month versus the previous weeks was 0.94 (95% CI, 0.86–1.02; P=0.124) during the ARRA stimulus, versus 1.01 (95% CI, 0.95–1.08; P=0.785) during the nonstimulus period, after including the control variables.
The emergency room visit costs for hypoglycemia were $1965 per person on an average (median, $861; 95% CI, $34–$7020). The inpatient admission costs for hypoglycemia were $11,632 per person on an average (median, $3609; 95% CI, $133–$47,632). Costs were higher, but not significantly so, between the last 7 days of each month and the previous 3 weeks of each month. During the last 7 days of each month, emergency room visits for hypoglycemia cost $3040 on an average (95% CI, $58–$11,298) versus $1356 on an average (95% CI, $29–$4899) during the earlier days; inpatient hospitalizations during the last 7 days cost $17,098 on an average (95% CI, $231–$61,507) versus $5278 on an average (95% CI, $87–$24,434) during the earlier days. A breakdown of costs for which the patient was responsible, versus the insurer, for emergency room visits and hospitalizations for hypoglycemia is provided in Table 2. The hypoglycemia visits were typically costlier than admissions for other reasons among people with type II diabetes; the emergency room costs for any diagnosis with a secondary diagnosis of type II diabetes were $1979 per person on an average (median, $815; 95% CI, $29–$7683), and the inpatient admissions costs were $13,474 per person on an average (median, $8330; 95% CI, $189–$45,792).
TABLE 2.
Per Capita Costs Attributable to Emergency Room Visits and Inpatient Hospitalizations for Hypoglycemia (N=560,503)*
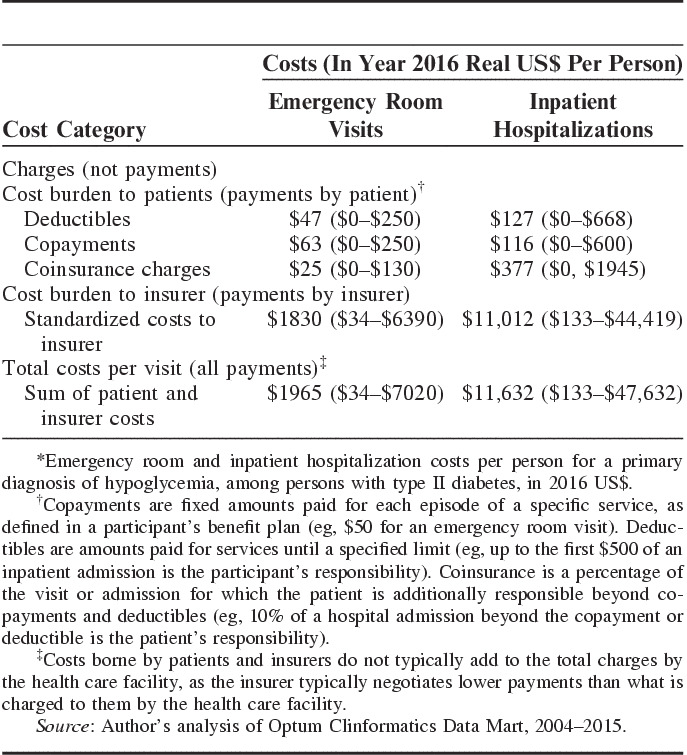
The average cost of hypoglycemic emergency room visits and inpatient hospitalizations associated with the increased risk of final-week hypoglycemia during the nonstimulus versus stimulus period was $271,667 (95% CI, $3876–$1,024,721) per year per 100,000 people. This estimate was the additional cost during nonstimulus than stimulus periods of emergency room visits in week 4 than in earlier weeks among the lower-income population (the difference in emergency room visit rate for hypoglycemia during week 4 minus the rate during earlier weeks, multiplied by the average cost of each emergency department visit), plus the additional cost during nonstimulus than stimulus periods of inpatient hospital admissions for hypoglycemia in week 4 than in earlier weeks among the lower-income population (the difference in inpatient admission rate for hypoglycemia during week 4 minus the rate during earlier weeks, multiplied by the average cost of each admission). Projecting this cost estimate to the 19.9 million nonelderly commercially insured lower-income US population, we estimated that eliminating the monthly cycle of hypoglycemia among lower-income nonelderly Americans would be expected to avert up to $54.1 million per year (95% CI, $0.8–$204.0) in commercial health care costs from emergency room visits and inpatient hospitalizations.
To check for spurious associations between week of the month and visits for hypoglycemia, we repeated our regressions with the outcome of appendicitis, which would not be expected to vary with week of the month. The OR for an emergency room visit or inpatient hospitalization for appendicitis was not significantly elevated during the last week of the month versus other weeks, among either the lower-income or higher-income populations. The odds of appendicitis visit or admission during the last week of the month was 1.01 among the lower-income population (95% CI, 0.98–1.04; P=0.880), and 1.01 among the higher-income population (95% CI, 0.99–1.03; P=0.174).
DISCUSSION
We observed that while higher-income persons did not experience a monthly cycle of hypoglycemia, lower-income persons had an increased risk of emergency room visits or inpatient hospitalizations for hypoglycemia during the last 7 days of each month. The increased risk was mitigated during the period of a recent economic stimulus that increased nutritional support to lower-income populations, suggesting that such support can mitigate health care costs attributable to food insecurity even over a short time-horizon. Eliminating the monthly cycle of hypoglycemia among commercially insured nonelderly adults would be expected to avert $54.1 million per year in emergency room and inpatient hospitalization costs.
Our findings lend support to the theory that a monthly “pay cycle,” associated with exhaustion of food budgets among lower-income adults, may be associated with increased risk of emergency room visits and hospital admissions for hypoglycemia. To reduce the chance that these associations were due to confounding, we tested and observed that appendicitis rates did not experience the same monthly cycle, as would be expected given the random nature of appendicitis. Further strengthening our analysis was our utilization of longitudinal, large-scale data from commercially insured patients who are not generally subject to as substantial barriers to primary care access as Medicaid patients, and for whom we knew household income rather than ZIP-code-level median income. The estimated costs of each emergency room visit and inpatient admission from our studied cohort is similar to the estimates from an independent analysis of alternative data sources ($1600 and $19,700, respectively, in 2016 real US$), which were studied to estimate hypoglycemia emergency room visit costs and hospitalizations from 2004 to 2008.30
Although hypoglycemia is not the only health outcome thought to be tightly linked to food insecurity, it is helpful as a model to study the acute impacts of social determinants of health. Although the incidence of hypoglycemia is low, the cost per event is high. Hypoglycemia is also a major preventable adverse event that contributes significantly to decreased quality of life in patients with diabetes,31 and may be associated with important long-term health consequences.32 Although newer agents to treat type II diabetes present a lower risk of hypoglycemia than older agents, currently over one third of patients with type II diabetes are treated with insulins and sulfonylureas that present considerable risk.27 Diabetes agents remain one of the most commonly implicated drug classes responsible for emergency department visits and hospitalizations, with 38.5% of all ED visits for adverse drug events resulting in hospitalization due to diabetes agents.14
Our findings suggest the critical need to directly examine the health impact of increasing food assistance on hypoglycemia. Our findings that a recent period of increased SNAP benefits was associated with less risk of end-of-the-month hypoglycemia among lower-income populations. In addition to SNAP and other federally financed nutrition programs, increased support for the charitable food system (food banks and food pantries) may reduce the need to rely on the health care system to address the health impacts of food insecurity. Facilitating collaboration between health care systems and the charitable food system may also assist lower-income populations, if such programs successfully reduce food insecurity and associated health care costs. Some multipayer initiatives are attempting to address social determinants of health in the clinical setting through ongoing pilot programs. Although results of such programs remain pending, physicians should consider modifying their diabetes treatment plans to avert hypoglycemia among persons with food insecurity, as recommended in the recently updated American Diabetes Association’s standards of care.33
Our study has notable limitations. The effect size of our ORs were modest, but consistent with other clinically or policy-relevant determinants of health outcomes such as the effect sizes of treating hypertension on cardiovascular outcomes,34 or the impact of sugar-sweetened beverage consumption on type II diabetes incidence.35 We lacked data on Medicare and Medicaid participants, for whom the effects of monthly pay cycles may be larger or smaller (as they may qualify for further supports not available to marginally fail to qualify). Notably, due to recent health reforms, large portions of low-income Americans are now privately insured, but privately insured patients are often less likely than Medicaid participants to be recognized as being at risk for food insecurity,36,37 and thus clinicians may not recognize the need to adjust treatment strategies for periods of limited food access. Indeed, recent literature suggests that extramarginal populations who barely miss the Medicaid or SNAP cut-points would be of most concern because they spend the most money on essential expenditures like rent and food, and face food insecurity without assistance that can mitigate the risks of hypoglycemia.38
We also lacked data on actual food consumption and on which participants in our sample participate in the SNAP or other food security initiatives and the actual food budgets or food spending of these persons. Our effect size estimates may also be conservative, lower-bound estimates because we included a comprehensive definition of low-income that may diminish the effect of week 4 versus week 1 differences among the lowest-income group.
Despite these limitations, our findings reveal an increased risk of hypoglycemia at the end of each month, thought to be related to exhaustion of food budgets in food insecure households. Breaking the monthly cycle of hypoglycemia, emergency room visits and inpatient hospital admissions in lower-income individuals, whether through nutrition program stimulus or other initiatives to support food security, should be investigated as strategies to improve health and reduce health care costs among lower-income populations.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website, www.lww-medicalcare.com.
Footnotes
Data for this project were accessed using the Stanford Center for Population Health Sciences Data Core. The PHS Data Core is supported by a National Institutes of Health National Center for Advancing Translational Science Award (UL1 TR001085) and from internal Stanford funding. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Supported by the National Institute On Minority Health And Health Disparities of the National Institutes of Health under Award Number DP2MD010478 and the National Institute Of Diabetes And Digestive And Kidney Diseases of the National Institutes of Health under Award Number K23DK109200. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors declare no conflict of interest.
REFERENCES
- 1.Centers for Medicare and Medicaid Services. State Innovation Models Initiative: General Information. Washington, DC: Centers for Medicare and Medicaid Services; 2015. [Google Scholar]
- 2.Alley DE, Asomugha CN, Conway PH, et al. Accountable health communities—addressing social needs through Medicare and Medicaid. N Engl J Med. 2016;374:8–11. [DOI] [PubMed] [Google Scholar]
- 3.Peek ME, Wilkes AE, Roberson TS, et al. Early lessons from an initiative on Chicago’s South Side to reduce disparities in diabetes care and outcomes. Health Aff (Millwood). 2012;31:177–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goddu AP, Roberson TS, Raffel KE, et al. Food Rx: a community-university partnership to prescribe healthy eating on the south side of Chicago. J Prev Interv Community. 2015;43:148–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.S eligman HK, Jacobs EA, López A, et al. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012;35:233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vijayaraghavan M, Jacobs EA, Seligman H, et al. The association between housing instability, food insecurity, and diabetes self-efficacy in low-income adults. J Health Care Poor Underserved. 2011;22:1279–1291. [DOI] [PubMed] [Google Scholar]
- 7.Seligman HK, Davis TC, Schillinger D, et al. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved. 2010;21:1227–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140:304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seligman HK, Bindman AB, Vittinghoff E, et al. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999-2002. J Gen Intern Med. 2007;22:1018–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff (Millwood). 2015;34:1830–1839. [DOI] [PubMed] [Google Scholar]
- 11.Solberg LI. Theory vs practice: should primary care practice take on social determinants of health now? No. Ann Fam Med. 2016;14:102–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.United States Department of Agriculture Economic Research Service. Definitions of food security. 2006. Available at: www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security.aspx. Accessed November 21, 2016.
- 13.Rodriguez-Gutierrez R, Ospina NS, McCoy RG, et al. Inclusion of hypoglycemia in clinical practice guidelines and performance measures in the care of patients with diabetes. JAMA Intern Med. 2016;176:1714–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shehab N, Lovegrove MC, Geller AI, et al. US Emergency Department visits for outpatient adverse drug events, 2013-2014. JAMA. 2016;316:2115–2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Seligman H, Jacobs E, Lopez A, et al. Food insecurity and hypoglycemia among safety net patients with diabetes. Arch Intern Med. 2011;171:1204–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seligman HK, Bolger AF, Guzman D, et al. Exhaustion of food budgets at month’s end and hospital admissions for hypoglycemia. Health Aff (Millwood). 2014;33:116–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Office of the Inspector General. Access to Care: Provider Availability in Medicaid Managed Care. Washington, DC: Department of Health and Human Services; 2014. [Google Scholar]
- 18.Abramsky S. The American Way of Poverty: How the Other Half Still Lives. New York: Nation Books; 2013. Available at: http://books.google.com/books?hl=en&lr=&id=7cwPAAAAQBAJ&oi=fnd&pg=PT7&dq=the+american+way+of+poverty+abramsky&ots=aaQVLEPoqz&sig=ZWCnhRE6pzvthPTzhAa5OxPavus. Accessed October 24, 2014. [Google Scholar]
- 19.Nord M, Prell MA. Food Security Improved Following the 2009 ARRA Increase in SNAP Benefits. Washington, DC: US Department of Agriculture, Economic Research Service; 2011. [Google Scholar]
- 20.Rice JB, Desai U, Cummings AKG, et al. Burden of diabetic foot ulcers for medicare and private insurers. Diabetes Care. 2014;37:651–658. [DOI] [PubMed] [Google Scholar]
- 21.Ginde AA, Blanc PG, Lieberman RM, et al. Validation of ICD-9-CM coding algorithm for improved identification of hypoglycemia visits. BMC Endocr Disord. 2008;8:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and The Endocrine Society. Diabetes Care. 2013;36:1384–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sanders GD, Neumann PJ, Basu A, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016;316:1093–1103. [DOI] [PubMed] [Google Scholar]
- 24.US Census Bureau. Current Population Survey: Annual Social and Economic Supplements. Washington, DC: US Census Bureau; 2013. [Google Scholar]
- 25.US Bureau of the Census. Real median household income in the United States. FRED, Federal Reserve Bank of St. Louis. 1984. Available at: https://fred.stlouisfed.org/series/MEHOINUSA672N. Accessed November 21, 2016.
- 26.Gray KF. Characteristics of supplemental nutrition assistance program households: fiscal year 2013. Mathematica Policy Research. 2014. Available at: https://ideas.repec.org/p/mpr/mprres/76ece7a812824260ae395b64da09dbdd.html. Accessed February 9, 2017.
- 27.Centers for Disease Control and Prevention. NHANES 2013-2014 Questionnaire Data—Prescription Medications. Atlanta: CDC; 2016. [Google Scholar]
- 28.Burke JF, Hayward RA, Nelson JP, et al. Using internally developed risk models to assess heterogeneity in treatment effects in clinical trials. Circ Cardiovasc Qual Outcomes. 2014;7:163–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kontopantelis E, Doran T, Springate DA, et al. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ. 2015;350:h2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Quilliamp BJ, Simeonep JC, Ozbayp AB, et al. The incidence and costs of hypoglycemia in type 2 diabetes. Am J Manag Care. 2011;10:673–680. Available at: www.ajmc.com/journals/issue/2011/2011-10-vol17-n10/ajmc_11oct_quilliam_673to680. Accessed December 4, 2016. [PubMed] [Google Scholar]
- 31.Laiteerapong N, Karter AJ, Liu JY, et al. Correlates of quality of life in older adults with diabetes: the diabetes & aging study. Diabetes Care. 2011;34:1749–1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Whitmer RA, Karter AJ, Yaffe K, et al. Hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. JAMA. 2009;301:1565–1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Herman WH, Donner TW, Dudl RJ, et al. Standards of Medical Care in Diabetes. Diabetes Care. 2016;39(suppl 1):S107–S108. [DOI] [PubMed] [Google Scholar]
- 34.Goff DC, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk. Circulation. 2014;129(suppl 2):S49–S73. [DOI] [PubMed] [Google Scholar]
- 35.Paynter NP, Yeh H-C, Voutilainen S, et al. Coffee and sweetened beverage consumption and the risk of type 2 diabetes mellitus: the atherosclerosis risk in communities study. Am J Epidemiol. 2006;164:1075–1084. [DOI] [PubMed] [Google Scholar]
- 36.Berkowitz SA, Hulberg AC, Standish S, et al. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med. 2017;177:244–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berkowitz SA, Baggett TP, Wexler DJ, et al. Food insecurity and metabolic control among US adults with diabetes. Diabetes Care. 2013;36:3093–3099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Heflin C, Hodges L, Mueser P. Supplemental Nutrition Assistance Program benefits and emergency room visits for hypoglycaemia. Public Health Nutr. 2016;19:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website, www.lww-medicalcare.com.


