Abstract
A 61-year-old man attended an outpatient colorectal clinic for a chronic, non-specific abdominal pain, associated with rectal bleeding. He underwent a number of investigations including a CT pneumocolon, which revealed an incidental finding of 20 cm of additional sigmoid colon. This case is interesting because tubular sigmoid duplication is an extremely unusual condition, rarely diagnosed in adults; only a few cases have been reported of this condition in the adult population. Our team chose to treat this patient conservatively, in order to avoid putting the patient at risk of an unnecessary surgery.
Keywords: congenital disorders, gastrointestinal system
Background
Gastrointestinal (GI) duplications are very rare congenital anomalies of the GI tract and have mostly been described in the paediatric population, as they are normally diagnosed in early childhood.1 Colonic duplications are the least common type of GI duplications, and their diagnosis is challenging.2 Tubular sigmoid duplication, such as the one found in our patient, is an even more rare subtype, with only a few cases reported in the literature.
Case presentation
A 61-year-old man was referred to a colorectal outpatient clinic by his general practitioner for investigation for a possible colonic malignancy. He had a 4-month history of intermittent, vague, non-specific abdominal pain, altered bowel habit and intermittent rectal bleeding.
The patient’s medical history included severe sleep apnoea, Barrett’s oesophagus, bilateral cataracts, anal fissure and anxiety. He also had a tonsillectomy and total knee replacement in the past. His medication list included a proton pump inhibitor (omeprazole 20 mg tablet once per day) and a selective serotonin uptake inhibitor (citalopram 20 mg tablet once per day), and he was on night continuous positive airway pressure. He is an ex-smoker and social drinker, with no known allergies.
On examination, the patient was noted to be obese (body mass index (BMI)=35.3 kg/m2). On palpation, his abdomen was soft, with minimal tenderness mainly on the right side, and there were no discernible masses. A digital rectal examination performed was normal.
Investigations
His laboratory results were within normal defined limits. On account of the patient’s history of change in bowel habit and rectal bleeding, he initially had a CT scan of his abdomen and pelvis with intravenous contrast, which was found to be normal. This was followed by a colonoscopy, which was limited to the ascending colon as a result of excessive scope looping. In this first colonoscopy, his sigmoid duplication was not noticed.
As the initial colonoscopy was incomplete, a CT pneumocolon was arranged in order to visualise the remainder of his large bowel. This study demonstrated a tubular structure in the pelvis arising from the distal sigmoid, raising the possibility of sigmoid duplication. To further investigate the possibility of this sigmoid duplication, a water-soluble contrast enema was arranged. This enema demonstrated a length of redundant sigmoid bowel (figure 1).
Figure 1.
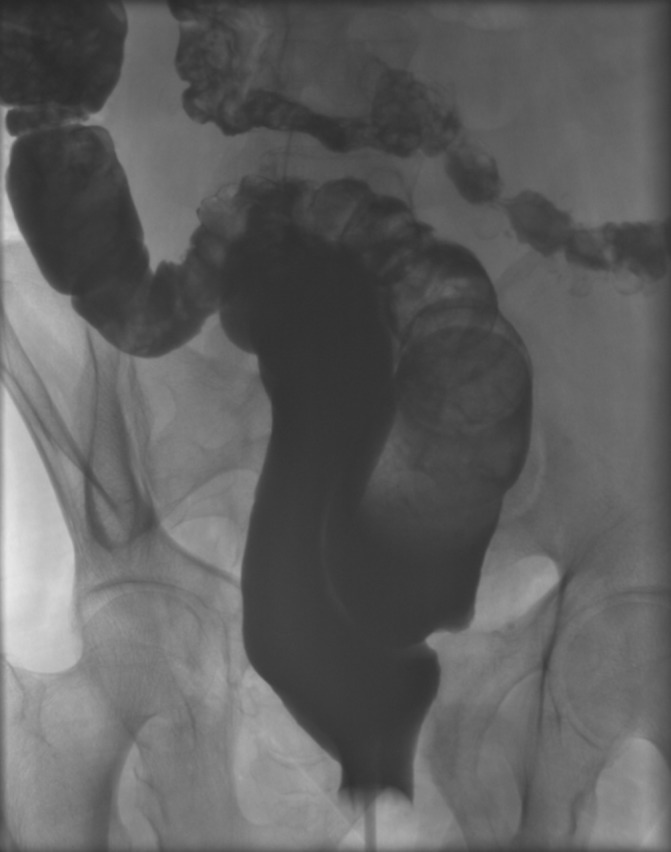
Water-soluble contrast enema showing duplication and adjoining segment of sigmoid.
Further colonoscopy confirmed the diagnosis of a 20 cm duplex sigmoid colon, where two separate lumina of the sigmoid colon were seen (figure 2). The additional bowel was scoped, and it was found to be normal. The patient did not have any further associated duplication of the GI tract at a different level. During the colonoscopy, two polyps (one at 45 cm and one in the midrectum) were also detected, and on biopsy, these were confirmed as tubular adenomas with low-grade dysplasia. The patient’s case was discussed at the colorectal multidisciplinary team meeting, and the plan was for polypectomy with follow-up colonoscopy and for conservative treatment of the sigmoid duplication.
Figure 2.
Colonoscopy showing two adjacent lumina in the bowel.
Treatment
The patient was seen in the outpatient clinic following his investigations, and the findings of his rare sigmoid duplication were explained to him. In particular, the consultant in charge of his care explained that the sigmoid duplication was not likely the main cause of his chronic pain, as discussed below. The patient was advised to take simple analgesia, lose weight, and minimise his stress levels. He was also informed that he would have regular follow-up and further colonoscopy.
The rationale behind this plan was that the patient was not experiencing any of the complications associated with his condition. Furthermore, the risks associated with an operative intervention and subsequent hospital stay were considered to be higher than the risk of a possible future complication related to his sigmoid duplication. The patient will be nevertheless regularly reviewed in the outpatient colorectal department.
Discussion
GI duplication is a congenital mass lesion attached to the GI tract that varies in site, morphology or embryological origin and can occur at any level from mouth to anus.1–3 Intra-abdominal duplications comprise 80% of all GI malformations and most commonly occur in the ileum (over 50%), whereas colonic duplication is very rare (6%–13%).2 4
Duplex colon can be a cystic (80%) or tubular lesion (20%) that can share the same blood supply with the parent bowel.2 5 Unlike cystic duplications, tubular duplications can communicate with the true bowel, and the rareness of this communication explains the lack of symptoms and the difficulty in diagnosing this condition in earlier life.2 3 6
GI duplications are generally diagnosed in early childhood.2 As such, journal articles and case reports published on the topic mainly discuss GI malformations in the context of the paediatric population. The exact incidence is unknown; however, an incidence of 1 per 100 000 deliveries has been reported.2 7 8 Moreover, about 20% of the patients have multiple congenital duplications including, in some cases, multiple organ duplication.2
In general, there is no pathognomonic clinical presentation of intra-abdominal colonic duplication. Symptoms vary from vague chronic features such as colicky abdominal pain or a change in bowel habit, to acute symptoms of bowel obstruction, which are the most common.2 6 9 Obstructive symptoms can occur either because the duplication can cause pressure on adjacent loops or because of volvulus, intussusception or perforation.6 9 The risk of malignancy is very rare.10
Examination may reveal tenderness at the site of the malformation, and a palpable mass can sometimes be present. A palpable mass could not be found on examination of our patient’s abdomen; however, his BMI of 35.3 kg/m2 would also have made this finding difficult. Tubular duplications also communicate with the true bowel, and this also explains the general lack of symptoms associated with our patient’s duplication in our case.6
Only few isolated reports of tubular sigmoid duplications in adults are found in the literature. Roberts et al6 highlighted the difficulty of making the diagnosis of colonic duplications, when they described two cases of patients with sigmoid duplications, who both underwent a bowel resection for a suspected carcinoma. In both cases, histology confirmed the presence of a colonic duplication, but no cancer.6 In 2010, Mourra et al4 reviewed seven cases of colorectal duplication, but only one of them was a case of sigmoid duplication that had a preoperative diagnosis of colonic duplication. In 2014, Al-Jaroof et al9 reported a case of sigmoid tubular duplication in a 33-year-old woman who underwent an exploratory laparotomy that confirmed the diagnosis.9 In this particular case, the diagnosis of colonic duplication was in the differential diagnosis, along with a giant diverticulum, volvulus and duplication cyst. Finally, in 2015, Sobhani et al11 reported a case of a 27-year-old man who was diagnosed with a tubular sigmoid duplication intraoperatively after he had an exploratory laparotomy for an acute abdomen.
The diagnosis of colonic duplications is challenging. The literature on GI duplications highlights the importance of considering GI duplications as a potential differential diagnosis in patients with gastrointestinal symptoms ranging from abdominal pain and chronic constipation to bowel obstruction, intussusception or perforation.12–15 In order to reach a correct and accurate diagnosis of gastrointestinal duplication, modalities such as CT or MRI with barium enema or colonoscopy are recommended as investigative options.13 15 A water-soluble contrast enema examination is considered potentially diagnostic.15 16 In this study, the diagnosis of the tubular colonic duplication was made through a combination of CT pneumocolon, water-soluble contrast enema along with a second, repeat colonoscopy.
In our case, we consider that the GI anomaly was found incidentally, and the patient’s symptoms were not likely associated for a number of reasons. First of all, the history of pain was recent and localised to the right side of the abdomen. Second, long-standing constipation is the most common change in bowel habit associated with colonic duplications, whereas our patient noticed increased frequency of bowel motion, up to eight times per day with loose stools.4 In addition to this, his colonoscopy showed a normal duplex sigmoid with no abnormal changes. Moreover, the patient’s high BMI and severe stress were more likely the cause of his symptoms rather than the duplex colon.
Therapeutic or preventive surgical excision is very common in GI duplications in paediatric population. In 1989, Holcomb et al1 presented 96 paediatric cases of GI duplications, out of which 94 underwent surgery, and only one case was asymptomatic and did not require surgery. Holcomb et al1 highlight the importance of an appropriate surgical approach that should be as radical as necessary to eliminate symptoms. In 2015, Sharma et al17 reported six paediatric cases of symptomatic enteric duplications that all underwent surgery underlining that enteric duplications often need urgent surgical intervention as massive bleeding or bowel perforation may occur, whereas surgical treatment in asymptomatic cases is controversial despite the risk of malignancy.
Although the literature recommends surgical intervention, via either an open or laparoscopic approach, especially in the paediatric population, there are no established guidelines for asymptomatic colonic duplications in adults. Owing to the rarity of the GI duplications, the risk of malignancy has not been quantified, and malignant change has been reported as ‘rare’ in literature,1 10 but it remains an indication for surgical resection in children indeed. However, in our opinion, when it comes to an uncomplicated incidental finding in an asymptomatic adult, the decision making regarding either to operate or not requires much consideration especially due to the lack of same cases.
The vast majority of reported colonic duplications in adults who underwent surgery suffered from life-threatening complications such as bowel obstruction. On the contrary, our patient has been living with his congenital abnormality for more than 60 years, and he has never suffered from any complication related to his anomaly. Even if there is a possibility that his abdominal pain is caused by his sigmoid duplication, surgical intervention in his case carries risks that outweigh the benefits. The main benefit from a surgical intervention would be the prevention of future possible complications associated with colonic duplications, as discussed above. However, the patient’s comorbidities, his high BMI and his age increase significantly the mortality and morbidity risk associated with undergoing a major abdominal operation and subsequent hospital stay.
Learning points.
Sigmoid tubular duplication is an extremely rare gastrointestinal (GI) abnormality.
Most duplications in adults are incidentally diagnosed.
The risk of malignancy in GI duplication is very low and cannot be quantified.
There is no established treatment for asymptomatic colonic duplication in adults, hence these patients may require frequent follow-up.
Follow-up and long-term studies of asymptomatic cases of duplex colon in adults would contribute to establishing a definitive treatment plan.
Footnotes
Contributors: The role of all authors was crucial for completing the case report and eventually submitting it for publication. AA took the initiative for writing the case report and submitting it. AA and H-KK did online research for literature, wrote and revised the case report. SA and CH did the overall supervision and enhanced the text with important comments.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Holcomb GW, Gheissari A, O’Neill JA, et al. Surgical management of alimentary tract duplications. Ann Surg 1989;209:167–74. 10.1097/00000658-198902000-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mukharjee I. Alimentary tract duplications. Medscape 2016. [Google Scholar]
- 3.Gross RE, Holcomb GW, Farber S. Duplications of the alimentary tract. Pediatrics 1952;9:448–68. [PubMed] [Google Scholar]
- 4.Mourra N, Chafai N, Bessoud B, et al. Colorectal duplication in adults: report of seven cases and review of the literature. J Clin Pathol 2010;63:1080–3. 10.1136/jcp.2010.083238 [DOI] [PubMed] [Google Scholar]
- 5.Smith JR. Accessory enteric formations: a classification and nomenclature. Arch Dis Child 1960;35:87–9. 10.1136/adc.35.179.87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts M, Rabinovitch J, Felton M, et al. Duplication of the sigmoid colon. Ann Surg 1959;150:904–8. 10.1097/00000658-195911000-00015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Harake A, Bassal A, Ramadan M, et al. Duodenal duplication cyst in a 52-year-old man: a challenging diagnosis and management. Int J Surg Case Rep 2013;4:296–8. 10.1016/j.ijscr.2013.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cochran WJ. Intestinal duplication MSD manual. 2016. http://www.msdmanuals.com/professional/pediatrics/congenital-gastrointestinal-anomalies/intestinal-duplication.
- 9.Al-Jaroof AH, Al-Zayer F, Meshikhes AW. A case of sigmoid colon duplication in an adult woman. BMJ Case Rep 2014;bcr2014203874 10.1136/bcr-2014-203874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Domajnko B. Case report duplication cyst of the sigmoid colon. Gastroenterology research and practice. Hindawi https://www.hindawi.com/journals/grp/2009/918401/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sobhani R, Fatemi MJ, Ayoubi Yazdi N, et al. Tubular duplication of the sigmoid colon with acute abdomen: an adult case report. Indian J Surg 2015;77:1005–7. 10.1007/s12262-014-1110-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kyo K, Azuma M, Okamoto K, et al. Laparoscopic resection of adult colon duplication causing intussusception. World J Gastroenterol 2016;22:2398–402. 10.3748/wjg.v22.i7.2398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang H-C. Y-Shaped Colonic Duplication: Report of A Case and Literature Review Chang Gung. Med J 2011;34:43–7. [PubMed] [Google Scholar]
- 14.Fenelon C, Boland MR, Kenny B, et al. A colonic duplication cyst causing bowel ischaemia in a 74-year-old lady. J Surg Case Rep 2016;2016:rjw147–3. 10.1093/jscr/rjw147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Banchini F, Delfanti R, Begnini E, et al. Duplication of the transverse colon in an adult: case report and review. World J Gastroenterol 2013;19:586–9. 10.3748/wjg.v19.i4.586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blank G, Königsrainer A, Sipos B, et al. Adenocarcinoma arising in a cystic duplication of the small bowel: case report and review of literature. World J Surg Oncol 2012;1010:5555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sharma S, Yadav AK, Mandal AK, et al. Enteric duplication cysts in children: a clinicopathological dilemma. J Clin Diagn Res 2015;9 10.7860/JCDR/2015/12929.6381 [DOI] [PMC free article] [PubMed] [Google Scholar]



