Abstract
Introduction
Due to advances in critical care medicine, more patients survive their critical illness. However, intensive care unit (ICU) survivors often experience long-term physical, cognitive and mental problems, summarised as post-intensive care syndrome (PICS), impacting their health-related quality of life (HRQoL). In what frequency PICS occurs, and to what extent this influences ICU survivors’ HRQoL, is mostly unknown. The aims of this study are therefore to study the: (1) 5-year patient outcomes, (2) predictors for PICS, (3) ratio between HRQoL of ICU survivors and healthcare-related costs, and (4) care and support needs.
Methods
The MONITOR-IC study is a multicentre prospective controlled cohort study, carried out in ICUs in four Dutch hospitals. Patients will be included between July 2016 and July 2021 and followed for 5 years. We estimated to include 12000 ICU patients. Outcomes are the HRQoL, physical, cognitive and mental symptoms, ICU survivors’ care and support needs, healthcare use and related costs. A control cohort of otherwise seriously ill patients will be assembled to compare long-term patient-reported outcomes. We will use a mixed methods design, including questionnaires, medical data from patient records, cost data from health insurance companies and interviews with patients and family members.
Ethics and dissemination
Insights from this study will be used to inform ICU patients and their family members about long-term consequences of ICU care, and to develop prediction and screening instruments to detect patients at risk for PICS. Subsequently, tailored interventions can be developed and implemented to prevent and mitigate long-term consequences. Additionally, insights into the ratio between HRQoL of ICU patients and related healthcare costs during 5 years after ICU admission can be used to discuss the added value of ICU care from a community perspective. The study has been approved by the research ethics committee of the Radboud University Medical Center (2016-2724).
Clinical trial registration
Keywords: critical care, intensive care units, long-term items, postintensive care syndrome, Quality of life
Strengths and limitations of this study.
The strength of the MONITOR-IC study is the thorough and comprehensive methodological approach, inclusion of thousands of intensive care unit (ICU) patients, 5-year follow-up, use of mixed methods and the combination of data regarding patients’ health-related quality of life (HRQoL), healthcare use and patients’ needs.
The baseline questionnaire includes questions relating to the patient’s situation before the ICU admission. Therefore, we are able to compare the experienced post-ICU symptoms and related HRQoL with the situation before the admission.
We aimed to include more than 12 000 patients. However, patients have to fill in eight questionnaires during 5 years. High loss to follow-up rates are likely due to high mortality rates.
The symptoms and consequences are based on the reported outcomes by patients themselves. This could lead to bias due to over or underestimation of their own symptoms, for example, their cognitive functioning.
Moreover, post-intensive care syndrome (PICS) occurs among ICU survivors and their family members and relatives, also called PICS-Family (PICS-F). At the time of writing this protocol, we decided to focus on ICU survivors, and not their family members.
Introduction
The number of patients admitted to the intensive care unit (ICU) is increasing every year.1 Meanwhile, advances in medical technologies allow more patients to survive their critical illness.2 With this growing number of ICU survivors, there is an urgent need to shift our focus from short-term mortality to long-term outcomes of ICU survivors.1 3
In 2002, the members of the international surviving intensive care Roundtable already discussed whether ICU survivors have optimal long-term outcomes, and whether decisions regarding ICU care would change with increasing knowledge of outcomes4 and the associated costs.3 Costs of ICU care are high; 20% of the total hospital budget, with cost per day between threefold and fivefold greater in ICU departments than in general wards.5 These high costs are due to the need for highly trained staff, expensive modern equipment, and intensive use of diagnostic tests, pharmaceuticals and interventions.6 Although economic evaluation of care in the ICU is often ethically difficult,6 understanding of the costs and consequences associated with technologies, services and programmes aimed at reducing mortality and morbidity of patients with critical illness is important.6 7
Over the last two decades, it has become more and more clear how devastating and long-lasting the post-discharge consequences can be, and what the impact is on ICU survivors and their family.8 These long-term consequences are called post-intensive care syndrome (PICS), defined as ‘new or worsening impairment in physical, cognitive, or mental health status arising and persisting after hospitalisation for critical illness’.2 Examples of these physical impairments are pain, breathing difficulties, fatigue and loss of bodyweight resulting in physical weakness and problems in daily functioning and activities.1 8–11 A total of 10%–75% of the ICU survivors are still suffering from these difficulties 1 year later.12 Cognitive problems, such as problems with memory, processing, planning and problem solving, are seen in 30%–80% of the ICU survivors.2 8 Although these impairments can improve over several months, they can persist for many years as well.10 In addition, mental impairment, such as depression,13 anxiety14 and sleep disturbances, is common.1 2 In 25% of the ICU survivors, post-traumatic stress disorder (PTSD) symptoms occur at 1-year follow-up.15 These PTSD symptoms can persist for 8 years.2 Moreover, ICU survivors experience a significant socioeconomic burden because of long-term sick leave, early retirement and need for assistance at home which is primarily given by informal caregivers, impacting on family income.16 17 Furthermore, ICU survivors experience a lower quality of life,18 leading to high utilisation of healthcare services and related costs.16 19
Although some risk factors for PICS are known (such as immobility, pre-existing impairments, age, sedation, duration of mechanical ventilation, delirium and sepsis),3 10 20 continued investigation of risk factors and underlying mechanisms is essential to understand which subgroups of patients are prone to develop PICS.3 10 Interventions and strategies to prevent or mitigate PICS, such as ICU diaries, early mobilisation, postdischarge rehabilitations and follow-up consultations with specialised nurses for ICU survivors, were recently described.1 21–25 However, conclusive evidence for these interventions is lacking or limited.24 26–29 Moreover, the majority of the healthcare professionals are still not aware of PICS, and interventions available for ICU survivors are therefore often not provided.1 3
More insight is necessary to better define the scope of long-term ICU symptoms and associated healthcare costs.3 Incidence rates of PICS differ largely in studies, which is due to differences in study patient populations, comorbidities, measurement tools and time frames.2 Additionally, previous studies addressing PICS often have limited focus or methodological limitations such as small sample sizes, low response rates, short follow-up, use of non-validated or unreliable instruments, no control group and absence of a preadmission (baseline) measurement.30–35
For this reason, we set up a controlled cohort study called the MONITOR-IC. In this study, with a 5-year follow-up, we aim to study the ICU survivors’ long-term outcomes, their health-related quality of life (HRQoL) and their needs, in order to identify specific types of patients who are at risk for specific impairments, factors affecting their recovery and to target effective interventions both in the ICU and later during the fragile recovery period.3 8 36 Additionally, we aim to get more insight into the ratio between the HRQoL and related healthcare costs to discuss the added value of ICU care from a community perspective.
Objectives
Overarching objective
To quantify and describe the extent of the physical, mental and cognitive long-term outcomes and HRQoL of ICU survivors during 5 years following ICU admission, in order to ultimately improve care for ICU patients.
Specific research questions
What are the post-intensive care symptoms that patients experience during 5 years after ICU admissions and what is their HRQoL?
What are important predictors for the various physical, cognitive and mental long-term outcomes?
What is the ratio between HRQoL and healthcare-related costs?
What are the care and support needs of ICU survivors during 5 years after ICU admission?
Methods/Design
Study design and setting
The MONITOR-IC study is a multicentre prospective controlled cohort study in which long-term outcomes of ICU patients are studied for a period of 5 years.
The study will be carried out in ICUs of four hospitals in the Netherlands; one academic hospital, one teaching hospital and two non-teaching hospitals. ICU patients will be recruited between July 2016 and July 2021 with a subsequent follow-up for 5 years. Mixed methods will be used to collect data, including questionnaires, medical data from patient records, cost data from health insurance companies and interviews with ICU survivors and their family members.
To compare the outcomes, such as the quality of life and experienced symptoms of ICU patients with non-ICU patients, we will set up a control group as well.
Study population and eligible criteria
ICU patients are eligible to participate when they are 16 years or older; admitted at least 12 hours to a trauma, medical, neurosurgery or cardiac surgery ICU; and gave written informed consent (or by their legal representative).
Patients are eligible for the control cohort when they are 16 years or older and admitted either to the ICU for less than 12 hours, or to the post anaesthesia care unit, the medium care or high dependency unit, for instance, for monitoring during short interventions, such as bronchoalveolar lavage or insertion of a central venous catheter.
Patients are not eligible for the study when they have a life expectance of <48 hours; receive palliative care; are admitted for a donor procedure; cannot read and speak the Dutch language; or are not able to fill in the questionnaire and do not have family members/legal representatives either.
For the MONITOR-IC study, we estimated to include 12 000 patients. This estimation is based on: (1) the initial ICU admissions in the academic hospital and the three other participating hospitals together (2500 and 2200 respectively per year), and (2) an estimated response rate of 60%, which is based on previous conducted ICU studies.37 38
In the control cohort, we will include approximately 3000 patients during the next 4 years.
Patient recruitment
Patients scheduled for ICU admission after elective surgery will be recruited at the outpatient clinic (anaesthesiology or cardiac surgery) (figure 1). Patients with a non-scheduled admission will be recruited at the ICU. Patients will receive information from ICU nurses and intensivists regarding the aim, content and relevance of the study, and will be asked for participation. Informed consent is asked for the questionnaires, data from the patients’ individual medical records (MR) and data from their health insurance company. In case patients are unable to give consent, their legal representative will be asked.
Figure 1.
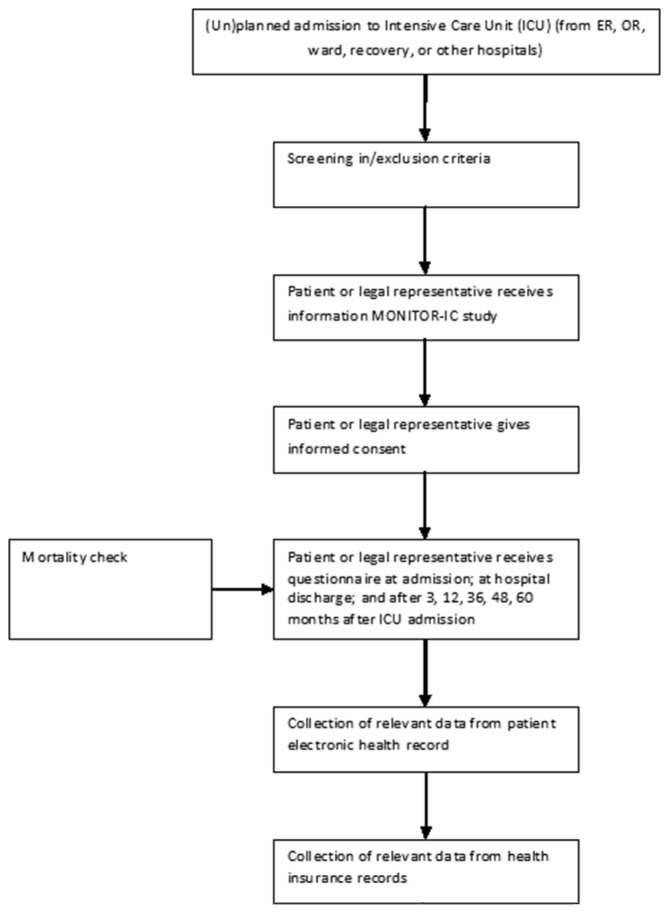
Flow chart of patient inclusion and data collection. ER, emergency room; OR, operating room.
Outcomes measures
The outcomes of the MONITOR-IC study are the HRQoL among ICU survivors and their physical (fatigue, vulnerability and frailty), cognitive and mental (anxiety, depression and stress) impairments. Additional outcomes are the patients’ care and support needs, their healthcare use and related costs.
Data collection
Different methods will be used to collect data among ICU patients, including questionnaires, patients’ MR, database of healthcare cost data of Dutch health insurance companies and interviews with patients and their family members (table 1).
Table 1.
Research questions and methods
| Research question | Methods |
| 1. What are the post-intensive care symptoms that patients experience during 5 years after ICU admission and what is their HRQoL? | Questionnaires MR |
| 2. What are important predictors for the various physical, cognitive and mental long-term outcomes? | Questionnaires MR |
| 3. What is the ratio between HRQoL and healthcare-related costs? | Questionnaires Health insurance database |
| 4. What are the care and support needs of ICU survivors during 5 years after ICU admission? | Questionnaires Interviews with ICU survivors and their family members |
HRQoL, health-related quality of life; ICU, intensive care unit; MR, medical records.
Questionnaires
All patients, or their relatives in case patients are not able to fill in the questionnaire themselves, will be approached to fill in the self-administered paper-based or online questionnaire (depending on their preferences) eight times: at ICU admission (T0), at hospital discharge (T1), after 3 months (T2), 12 months (T3), 24 months (T4), 36 months (T5), 48 months (T6) and 60 months after ICU admission (T7). To get insight into the situation before the ICU admission, the baseline questionnaire (T0) is provided when the patients are asked for informed consent. This could be preoperatively for the planned admissions or after admission at the ICU. Then, patients are asked to rate their situation before the ICU admission.
The investigators keep track on when patients should receive the next questionnaire or the postal or telephone reminders after 4 and 6 weeks.
The questionnaire is established in close collaboration with worldwide experts in the fields of ICU long-term outcomes and the FCIC (Family and Patient-Centered Intensive Care); the Dutch foundation for ICU survivors and their family members.
The components in the questionnaire vary at different measurement points (see table 2, and for more information regarding the domains and items see online supplementary file 1) but contain the following:
Patients’ health status and HRQoL will be assessed using the 36-Item Short Form Survey (SF-36)39 and the 5-level EQ-5D version (EQ-5D-5L).40 Both questionnaires are validated instruments and applicable in different countries and languages. The SF-36 is a comprehensive instrument, measuring the general health status and quality of life, consisting of eight different health domains. The EQ-5D-5L is a simple instrument to measure the HRQoL.4 Although the SF-36 is the most often used questionnaire measuring quality of life in intensive care patients,41 the EQ-5D-5L is added since this questionnaire can be best used for the calculation of quality adjusted survival, a key measure of health effects for cost-effectiveness assessments.4
-
Patients’ level of frailty and vulnerability will be assed using the Clinical Frailty Score (CFS).42 Frailty is common in patients with critical illness and is associated with poorer outcomes in terms of ICU and hospital mortality, impairment in HRQoL and functional dependence.43 The CFS is simple, short and reliably measures frailty. Using the CFS it is possible to predict outcomes more effectively.44
The level of fatigue, which is not well covered by the other included questionnaires, will be measured using the CIS-8, a subscale of the Checklist Individual Strength (CIS-20),45 and is used by ICU patients before.37
Critical illness and ICU treatment are associated with long-term cognitive impairment,46 which will be measured using the validated abbreviated 14-item Cognitive Failure Questionnaire (CFQ-14).47 The original CFQ-2548 is often used to screen ICU survivors for cognitive problems; however, the number of questions and missing values is a limitation.47 Therefore, we have chosen the shorter version which is highly correlated with the original questionnaire.48
-
The mental impairments will be assed using the Hospital Anxiety and Depression Scale (HADS) to determine the levels of anxiety and depression.49 The HADS is the most often used questionnaire to measure symptoms of anxiety and depression in ICU survivors.41
Subjective distress, caused by traumatic events, will be measured using the IES-R (Impact of Event Scale Revised),50 a standardised measure of PTSD symptoms.
-
Care needs and support from professionals and informal caregivers will be measured using questions created by our research team, former ICU patients and members of the FCIC, and by previous studies among chronic patients.51
Social consequences will be measured using the novel question set designed by Griffiths et al,16 to determine changes in family circumstances, socioeconomic stability and care requirements.
Table 2.
Overview of used scales in the questionnaire and time frame
| Methods | Outcome | Used scales | T0 | T1 | T2 | T3 | T4 | T5 | T6 | T7 |
| (ICU) admission | Discharge hospital | 3 months | 12 months | 24 months | 36 months | 48 months | 60 months | |||
| Questionnaire | Demographic data | X | ||||||||
| Health status and HRQoL | SF-36 | X | X | X | X | X | X | X | ||
| EQ-5D | X | X | X | X | X | X | X | |||
| Physical impairments | CFS | X | X | X | X | X | X | X | X | |
| CIS-8 | X | X | X | X | ||||||
| Cognitive impairments | CFQ-14 | X | X | X | X | X | ||||
| Mental impairments | HADS | X | X | X | X | X | ||||
| IES-R | X | X | X | X | ||||||
| New symptoms after ICU admission | X | X | X | X | X | X | ||||
| Care needs and professional support/informal caregivers | X | X | X | X | ||||||
| Social consequences | X | X | X |
CFQ-14, 14-item Cognitive Failure Questionnaire; CFS, Clinical Frailty Score; CIS-8, Checklist Individual Strength Questionnaire; EQ-5D, EuroQol Five-Dimensional Questionnaire; HADS, Hospital Anxiety and Depression Scale; HRQoL, health-related quality of life; ICU, intensive care unit; IES-R, Impact of Event Scale Revised; SF-36, 36-Item Short Form Survey.
bmjopen-2017-018006supp001.pdf (141.3KB, pdf)
Although we are aware of the overlap between the used questionnaires, it will allow us to check the reliability. For more information regarding the questionnaires, domains and scores, see online supplementary file 1.
Medical data
Patients’ demographics and information regarding their diagnosis and treatment, such as primary conditions, pre-existing comorbidity, disease severity, sepsis, (re)admission, length of mechanical ventilation, length of ICU stay, delirium, pain and expected mortality, will be extracted from their MR and the NICE (Dutch National Intensive Care Evaluation) registry.52
Health insurance data
Healthcare use and related costs, covered by the Dutch healthcare insurance, will be retrieved from Vektis, a Dutch organisation which collects and manages health insurance claimed data of all health insurance companies in the Netherlands.53 These data are collected based on the diagnosis treatment combination; a total set of activities carried out by the hospital and medical specialists. Additionally, data are collected regarding nursing days, visits at the outpatient clinic and emergency department, nursing homes, ambulance transport, consultation with general practitioner, paramedical care (including physiotherapist, occupational therapist, dietitian and speech therapist), prescribed medication, mental healthcare and revalidation. The Vektis database contains data from all healthcare insured citizens and covers 99% of the total Dutch population. Using patient’s unique insurance number, we are able to merge patient’s insurance data with the questionnaire data and medical data from the MR at patient level.
Care delivered by community nurses and informal caregivers is not included in the Vektis database and will be studied via the questionnaire.
Interviews
To get insight into the experiences of ICU survivors during 5 years after ICU admission and their need for support, face-to-face semistructured interviews will be conducted with ICU survivors and their family members. Interviews will take place at the participants’ preferred location (home or clinic). Interviews will be conducted until data saturation is reached.
Patients will be purposively sampled based on various experienced outcomes, such as the quality of life, daily functioning, anxiety, depression and their experienced needs for more information or emotional support. Experienced and trained researchers will conduct the interviews using a topic guide. This guide will be developed using the current literature and experience of the research team and will cover the following subjects: experiences with the ICU admission and follow-up, experienced problems and needs for support. All interviews will be audio recorded and transcribed verbatim.
Analysis
Questionnaires, MR and health insurance data
During the data collection, data are checked on a regular basis to identify out-of-range answers, inconsistent responses and missing data. Data from the questionnaires, MR and healthcare insurance will be merged at patient level. Descriptive statistics will be used to describe baseline characteristics and the incidence of long-term outcomes. Regression analysis will be used to determine associations between patient characteristics, treatment and long-term outcomes. Subgroups will be identified based on their illness and condition (eg, sepsis, delirium, comorbidities, acute respiratory distress syndrome (ARDS)), treatment (eg, length of ICU stay, duration of mechanical ventilation, dialysis) and social demographics (age, gender, education, family setting, and so on).
In order to predict the various physical, cognitive and mental long-term outcomes, multiple prediction models will be developed. Multivariable linear (for continuous outcome variables) and logistic (for dichotomous outcome variables) regression analysis will be performed. Linear and logistic multilevel models will be used to compare long-term outcomes between the study population (cohort) and control cohort group.
To determine the ratio between HRQoL and patient outcomes and the health-related costs, quality-adjusted life years (QALYs) will be calculated. QALYs are a measure of the state of health of a person or group in which the benefits, in terms of length of life, are adjusted to reflect the quality of life. QALYs are calculated by estimating the years of life remaining for particular treatment and weighting each year with a quality of life score.54 SPSS 22 (Software Package for the Social Sciences) will be used for data analysis.
Interviews
For the analysis of the interview data, the constant comparative method55 will be used. Relevant data will be identified and structured by open, axial and selective coding.
Two researchers will independently code the transcripts to minimise subjectivity in findings. The differences and similarities between the codes will be discussed together, and in case of disagreement, a third researcher will be involved. In the meetings with the team, the codebook will be refined and emerging categories and themes will be discussed.
Data analysis will be supported with the use of Atlas.ti, a qualitative data analysis program.
Ethics
The MONITOR-IC study will be conducted complying with the Dutch Personal Data Protection Act.
The study has been approved by the research ethics committee of the Radboud University Medical Center, CMO region Arnhem-Nijmegen (2016-2724). The study is registered in the ClinicalTrials.gov database (NCT03246334).
Relevance of findings
The results of the MONITOR-IC study will be disseminated through international and national publications and presentations. We will quantify and describe the extent of the physical, cognitive and mental long-term outcomes of ICU survivors, their healthcare use and their needs (box).
Box. Relevance of study.
Information about long-term outcomes for patients and their family members
Support for treatment choices for multiple medical specialties, in particular intensive care
Coordination of care by personalised follow-up care for post-ICU (intensive care unit) patients
Adjustments in healthcare policy for post-ICU patients
Screening instrument for early signs and symptoms
Establishing and implementing interventions to prevent or mitigate long-term consequences
Information for health insurance companies for purchasing care and professional associations for guideline development
Detecting unnecessary ICU care
Evaluation of changes in ICU healthcare policy on long-term effects
This knowledge is of importance for patients, healthcare professionals, managers and health insurers to develop and evaluate the (after)care for ICU patients taking their health status and needs into account. Patients and their family members could be better informed about the possible long-term physical, cognitive, mental and social consequences after ICU discharge. Moreover, the inclusion of thousands of ICU patients in this study allows us to study several patient subgroups; for example, the quality of life and specific care needs of patients after sepsis, ARDS or delirium. Using these disease-specific insights, prediction and screening instruments can be developed to determine patients at risk for long-term consequences. Subsequently, interventions, such as diaries, early mobilisation and follow-up consultations for patients and their family members, could be adjusted, established and implemented to prevent or mitigate long-term consequences. Furthermore, long-term effects of important changes in health policy will be visible, where evaluation of effectiveness and efficacy of (changes in) policy on micro, meso and macrolevels is possible. Healthcare professionals will be better able to weigh up the options in the decision-making process concerning ICU admission, treatment options and the added value for individual patients, which will improve shared decision-making with patients and their families as well.
Finally, this study gives more perspectives into the ratio between the patients’ HRQoL and healthcare costs. Over the last decades, the ICU care is overwhelmed with new and also costly technologies and therapies, resulting in increasing costs, but without actual insight in the added value for patient and their health outcomes. Consequently, an open ethical dialogue, based on this ratio and what this ratio might be, is then possible.
The strengths of the MONITOR-IC study are the thorough and comprehensive methodological approach, inclusion of thousands of ICU patients, 5-year follow-up, use of mixed methods and the combination of data regarding patients’ HRQoL, healthcare use and patients’ needs. Moreover, the baseline questionnaire includes questions relating to the patient’s situation before the ICU admission. Therefore, we are able to compare the experienced post-ICU symptoms and related HRQoL with the situation before the admission.
There are also some limitations that need to be addressed. We aimed to include more than 12 000 patients. However, patients have to fill in eight questionnaires during 5 years. High loss to follow-up rates are likely due to high mortality rates.56 Furthermore, the post-ICU symptoms and consequences are based on the reported outcomes by patients themselves. This could lead to bias due to overestimation or underestimation of their own symptoms, for example, their cognitive functioning. Using the data of the health insurance companies regarding, for example, patients’ visits to the general practitioner or medical specialist, we try to overcome this. Moreover, PICS occurs among ICU survivors and their family members and relatives, also called PICS-Family (PICS-F).57 These long-term consequences in families of survivors and non-survivors consist of psychological, physical and social consequences as well.58–60 Although it is important to increase awareness of these possible long-term consequences on family members,2 we decided to focus only on the ICU survivors. In the future extension of this study, family members might be included as well.
Supplementary Material
Acknowledgments
We gratefully acknowledge the Family and Patient Centered Intensive Care (FCIC), the national foundation for ICU survivors and their family members, for their close cooperation. We are also grateful to Cees Zimmerman and Grietje Marten-van Stijn, respectively intensivists and ICU nurse of the ICU follow-up outpatient clinic in the Radboud university medical center, as co-designers of this study.
Footnotes
Contributors: JvdH, MvdB, MZ, HV and WG contributed to the design of the study. WG drafted the manuscript. JvdH, MvdB, MZ and HV were involved in the editing of the manuscript. All authors read and approved the final manuscript.
Funding: This work was supported by the Radboud University Medical Center, Nijmegen, The Netherlands.
Competing interests: None declared.
Ethics approval: The Radboud University Medical Center, CMO region Arnhem-Nijmegen.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Svenningsen H, Langhorn L, Agard AS, et al. Post-ICU symptoms, consequences, and follow-up: an integrative review. Nurs Crit Care 2017;22:212–20. 10.1111/nicc.12165 [DOI] [PubMed] [Google Scholar]
- 2.Harvey MA, Davidson JE. Postintensive Care Syndrome:right care and right now and later.Crit Care Med 2016;44:381–5. 10.1097/CCM.0000000000001531 [DOI] [PubMed] [Google Scholar]
- 3.Needham DM, Davidson J, Cohen H, et al. Improving long-term outcomes after discharge from intensive care unit: Report from a stakeholders conference. Crit Care Med 2012;40:502–9. 10.1097/CCM.0b013e318232da75 [DOI] [PubMed] [Google Scholar]
- 4.Angus DC, Carlet J. 2002 Brussels Roundtable Participants. Surviving intensive care: a report from the 2002 Brussels Roundtable. Intensive Care Med 2003;29:368–77. 10.1007/s00134-002-1624-8 [DOI] [PubMed] [Google Scholar]
- 5.Tan SS, Bakker J, Hoogendoorn ME, et al. Direct cost analysis of intensive care unit stay in four European countries: applying a standardized costing methodology. Value Health 2012;15:81–6. 10.1016/j.jval.2011.09.007 [DOI] [PubMed] [Google Scholar]
- 6.Talmor D, Shapiro N, Greenberg D, et al. When is critical care medicine cost-effective? A systematic review of the cost-effectiveness literature. Crit Care Med 2006;34:2738–47. 10.1097/01.CCM.0000241159.18620.AB [DOI] [PubMed] [Google Scholar]
- 7.Conti M, Merlani P, Ricou B. Prognosis and quality of life of elderly patients after intensive care. Swiss Med Wkly 2012;142:w13671 10.4414/smw.2012.13671 [DOI] [PubMed] [Google Scholar]
- 8.Jutte JE, Erb CT, Jackson JC. Physical, Cognitive, and Psychological Disability Following Critical Illness: What Is the Risk? Semin Respir Crit Care Med 2015;36:943–58. 10.1055/s-0035-1566002 [DOI] [PubMed] [Google Scholar]
- 9.van der Schaaf M, Beelen A, Dongelmans DA, et al. Functional status after intensive care: a challenge for rehabilitation professionals to improve outcome. J Rehabil Med 2009;41:360–6. 10.2340/16501977-0333 [DOI] [PubMed] [Google Scholar]
- 10.Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med 2011;39:371–9. 10.1097/CCM.0b013e3181fd66e5 [DOI] [PubMed] [Google Scholar]
- 11.Granja C, Amaro A, Dias C, et al. Outcome of ICU survivors: a comprehensive review. The role of patient-reported outcome studies. Acta Anaesthesiol Scand 2012;56:1092–103. 10.1111/j.1399-6576.2012.02686.x [DOI] [PubMed] [Google Scholar]
- 12.Harvey MA. Mitigating PICS, 2016: http://www.sccm.org/Communications/Critical-Connections/Archives/Pages/Mitigating-PICS.aspx
- 13.Rabiee A, Nikayin S, Hashem MD, et al. Depressive Symptoms After Critical Illness: A Systematic Review and Meta-Analysis. Crit Care Med 2016;44:1744–53. 10.1097/CCM.0000000000001811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nikayin S, Rabiee A, Hashem MD, et al. Anxiety symptoms in survivors of critical illness: a systematic review and meta-analysis. Gen Hosp Psychiatry 2016;43:23–9. 10.1016/j.genhosppsych.2016.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parker AM, Sricharoenchai T, Raparla S, et al. Posttraumatic stress disorder in critical illness survivors: a metaanalysis. Crit Care Med 2015;43:1121–9. 10.1097/CCM.0000000000000882 [DOI] [PubMed] [Google Scholar]
- 16.Griffiths J, Hatch RA, Bishop J, et al. An exploration of social and economic outcome and associated health-related quality of life after critical illness in general intensive care unit survivors: a 12-month follow-up study. Crit Care 2013;17:R100 10.1186/cc12745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Norman BC, Jackson JC, Graves JA, et al. Employment Outcomes After Critical Illness: An Analysis of the Bringing to Light the Risk Factors and Incidence of Neuropsychological Dysfunction in ICU Survivors Cohort. Crit Care Med 2016;44:2003–9. 10.1097/CCM.0000000000001849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oeyen SG, Vandijck DM, Benoit DD, et al. Quality of life after intensive care: a systematic review of the literature. Crit Care Med 2010;38:2386–400. 10.1097/CCM.0b013e3181f3dec5 [DOI] [PubMed] [Google Scholar]
- 19.Hill AD, Fowler RA, Pinto R, et al. Long-term outcomes and healthcare utilization following critical illness–a population-based study. Crit Care 2016;20:76 10.1186/s13054-016-1248-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Latronico N, Herridge M, Hopkins RO, et al. The ICM research agenda on intensive care unit-acquired weakness. Intensive Care Med 2017:1270–81. 10.1007/s00134-017-4757-5 [DOI] [PubMed] [Google Scholar]
- 21.Cuthbertson BH, Rattray J, Campbell MK, et al. The PRaCTICaL study of nurse led, intensive care follow-up programmes for improving long term outcomes from critical illness: a pragmatic randomised controlled trial. BMJ 2009;339:b3723 10.1136/bmj.b3723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jensen JF, Egerod I, Bestle MH, et al. A recovery program to improve quality of life, sense of coherence and psychological health in ICU survivors: a multicenter randomized controlled trial, the RAPIT study. Intensive Care Med 2016;42:1733–43. 10.1007/s00134-016-4522-1 [DOI] [PubMed] [Google Scholar]
- 23.Jones C, Bäckman C, Capuzzo M, et al. Intensive care diaries reduce new onset post traumatic stress disorder following critical illness: a randomised, controlled trial. Crit Care 2010;14:R168 10.1186/cc9260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehlhorn J, Freytag A, Schmidt K, et al. Rehabilitation interventions for postintensive care syndrome: a systematic review. Crit Care Med 2014;42:1263–71. 10.1097/CCM.0000000000000148 [DOI] [PubMed] [Google Scholar]
- 25.Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 2009;373:1874–82. 10.1016/S0140-6736(09)60658-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aitken LM, Rattray J, Hull A, et al. The use of diaries in psychological recovery from intensive care. Crit Care 2013;17:253 10.1186/cc13164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jensen JF, Thomsen T, Overgaard D, et al. Impact of follow-up consultations for ICU survivors on post-ICU syndrome: a systematic review and meta-analysis. Intensive Care Med 2015;41:763–75. 10.1007/s00134-015-3689-1 [DOI] [PubMed] [Google Scholar]
- 28.Ullman AJ, Aitken LM, Rattray J, et al. Diaries for recovery from critical illness. Cochrane Database of Systematic Reviews 2014;12:CD010468 10.1002/14651858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tipping CJ, Harrold M, Holland A, et al. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med 2017;43 10.1007/s00134-016-4612-0 [DOI] [PubMed] [Google Scholar]
- 30.Cuthbertson BH, Roughton S, Jenkinson D, et al. Quality of life in the five years after intensive care: a cohort study. Crit Care 2010;14:R6 10.1186/cc8848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Rooij SE, Govers AC, Korevaar JC, et al. Cognitive, functional, and quality-of-life outcomes of patients aged 80 and older who survived at least 1 year after planned or unplanned surgery or medical intensive care treatment. J Am Geriatr Soc 2008;56:816–22. 10.1111/j.1532-5415.2008.01671.x [DOI] [PubMed] [Google Scholar]
- 32.Hofhuis JG, Spronk PE, van Stel HF, et al. The impact of critical illness on perceived health-related quality of life during ICU treatment, hospital stay, and after hospital discharge: a long-term follow-up study. Chest 2008;133:377–85. 10.1378/chest.07-1217 [DOI] [PubMed] [Google Scholar]
- 33.Kaarlola A, Pettilä V, Kekki P. Quality of life six years after intensive care. Intensive Care Med 2003;29:1294–9. 10.1007/s00134-003-1849-1 [DOI] [PubMed] [Google Scholar]
- 34.Orwelius L, Nordlund A, Nordlund P, et al. Pre-existing disease: the most important factor for health related quality of life long-term after critical illness: a prospective, longitudinal, multicentre trial. Crit Care 2010;14:R67 10.1186/cc8967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu A, Gao F. Long-term outcomes in survivors from critical illness. Anaesthesia 2004;59:1049–52. 10.1111/j.1365-2044.2004.04011.x [DOI] [PubMed] [Google Scholar]
- 36.Van Der Schaaf M, Bakhshi-Raiez F, Van Der Steen M, et al. Recommendations for intensive care follow-up clinics; report from a survey and conference of Dutch intensive cares. Minerva Anestesiol 2015;81:135–44. [PubMed] [Google Scholar]
- 37.van den Boogaard M, Schoonhoven L, Evers AW, et al. Delirium in critically ill patients: impact on long-term health-related quality of life and cognitive functioning. Crit Care Med 2012;40:112–8. 10.1097/CCM.0b013e31822e9fc9 [DOI] [PubMed] [Google Scholar]
- 38.Wolters AE, van Dijk D, Pasma W, et al. Long-term outcome of delirium during intensive care unit stay in survivors of critical illness: a prospective cohort study. Crit Care 2014;18:R125 10.1186/cc13929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 40.Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727–36. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Turnbull AE, Rabiee A, Davis WE, et al. Outcome Measurement in ICU Survivorship Research From 1970 to 2013: A Scoping Review of 425 Publications. Crit Care Med 2016;44:1267–77. 10.1097/CCM.0000000000001651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005;173:489–95. 10.1503/cmaj.050051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bagshaw SM, Stelfox HT, Johnson JA, et al. Long-term association between frailty and health-related quality of life among survivors of critical illness: a prospective multicenter cohort study. Crit Care Med 2015;43:973–82. 10.1097/CCM.0000000000000860 [DOI] [PubMed] [Google Scholar]
- 44.Le Maguet P, Roquilly A, Lasocki S, et al. Prevalence and impact of frailty on mortality in elderly ICU patients: a prospective, multicenter, observational study. Intensive Care Med 2014;40:674–82. 10.1007/s00134-014-3253-4 [DOI] [PubMed] [Google Scholar]
- 45.Vercoulen JH, Swanink CM, Fennis JF, et al. Dimensional assessment of chronic fatigue syndrome. J Psychosom Res 1994;38:383–92. 10.1016/0022-3999(94)90099-X [DOI] [PubMed] [Google Scholar]
- 46.Wolters AE, Slooter AJ, van der Kooi AW, et al. Cognitive impairment after intensive care unit admission: a systematic review. Intensive Care Med 2013;39:376–86. 10.1007/s00134-012-2784-9 [DOI] [PubMed] [Google Scholar]
- 47.Wassenaar A, de Reus J, Donders ART, et al. Development and validation of the abbreviated Cognitive Failure Questionnaire in Intensive Care Unit patients: a multicenter cohort study. Submitted 2017. [Google Scholar]
- 48.Broadbent DE, Cooper PF, FitzGerald P, et al. The Cognitive Failures Questionnaire (CFQ) and its correlates. Br J Clin Psychol 1982;21:1–16. 10.1111/j.2044-8260.1982.tb01421.x [DOI] [PubMed] [Google Scholar]
- 49.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 50.Weiss DS, Marmar CR. Chapter: The Impact of Event Scale-Revised. 1997. Assessing psychological trauma and PTSD New York, NY: Guilford Press; US 1997. [Google Scholar]
- 51.Nivel. National Panel Chronisch ieken en Gehandicapten. 2017. https://www.nivel.nl/nl/panels/nationaal-panel-chronisch-zieken-en-gehandicapten-0
- 52.Stichting NICE. Nationale Intensive care evaluatie. https://www.stichting-nice.nl/
- 53.Vektis. Informatiecentrum voor de zorg. https://www.vektis.nl/
- 54.NICE. National Institute for Health and Care Excellence London. 2017. https://www.nice.org.uk/glossary?letter=q
- 55.Boeije H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Quality and Quantity 2002;36:391–409. 10.1023/A:1020909529486 [DOI] [Google Scholar]
- 56.Williams TA, Leslie GD. Challenges and possible solutions for long-term follow-up of patients surviving critical illness. Australian Critical Care 2011;24:175–85. 10.1016/j.aucc.2011.03.001 [DOI] [PubMed] [Google Scholar]
- 57.Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: postintensive care syndrome-family. Critical care medicine 2012;40:618–24. 10.1097/CCM.0b013e318236ebf9 [DOI] [PubMed] [Google Scholar]
- 58.Cameron JI, Chu LM, Matte A, et al. One-Year Outcomes in Caregivers of Critically Ill Patients. N Engl J Med Overseas Ed 2016;374:1831–41. 10.1056/NEJMoa1511160 [DOI] [PubMed] [Google Scholar]
- 59.van Beusekom I, Bakhshi-Raiez F, de Keizer NF, et al. Reported burden on informal caregivers of ICU survivors: a literature review. Critical Care 2015;20:16 10.1186/s13054-016-1185-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wintermann G-B, Weidner K, Strauß B, et al. Predictors of posttraumatic stress and quality of life in family members of chronically critically ill patients after intensive care. Ann Intensive Care 2016;6:69 10.1186/s13613-016-0174-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-018006supp001.pdf (141.3KB, pdf)


