Abstract
Introduction
Psoriasis vulgaris is a common skin disease that is characterised by persistent localised erythematous scaly plaques. Yinxieling is a Chinese herbal formula for psoriasis that has been used for more than 20 years in China. To facilitate application, PSORI-CM01 was developed based on the optimisation and simplification of Yinxieling tablets performed in a previous study and in clinical practice. However, the scientific evidence regarding whether PSORI-CM01 is more effective for psoriasis than the original Yinxieling remains insufficient. Therefore, we designed a randomised clinical trial to investigate the effect, safety and cost-effectiveness of PSORI-CM01 granules compared with those of Yinxieling tablets for the treatment of patients with psoriasis.
Methods and analysis
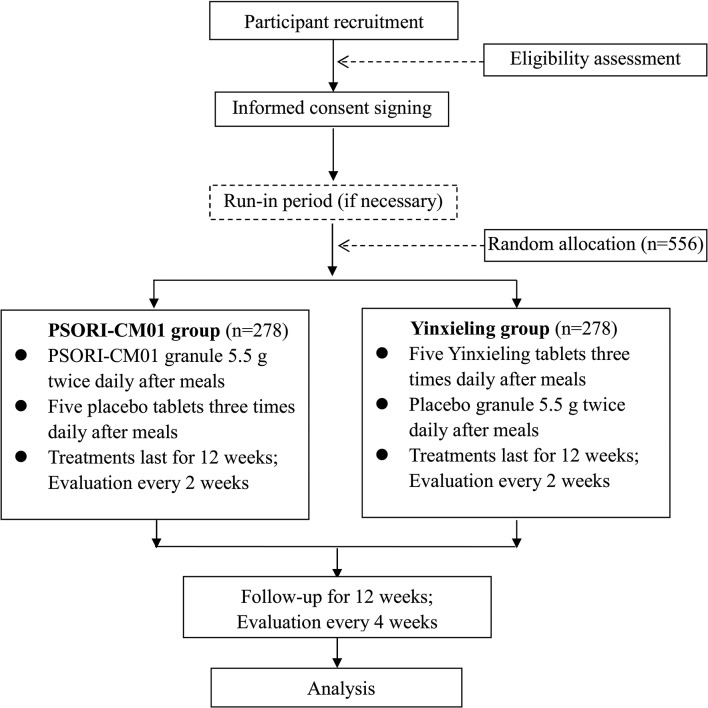
This ongoing study is a two-arm parallel, randomised, double-blind, double-dummy clinical trial. Five hundred and fifty-six participants with psoriasis will be recruited and then randomly allocated into two groups in a 1:1 ratio. Participants in PSORI-CM01 group will receive a 5.5 g granule of PSORI-CM01 two times daily and five placebo tablets three times daily for 12 weeks. The participants in the Yinxieling group will receive five Yinxieling tablets three times daily and a placebo granule two times daily for 12 weeks. The primary outcome is the reduction of the Psoriasis Area and Severity Index. The secondary outcomes include relapse rate, Visual Analogue Scale scores, body surface area and the Dermatology Life Quality Index. Cost-effectiveness analysis will be performed from a health and community care provider perspective.
Ethics and dissemination
This research protocol had been reviewed and approved by the institutional review boards of three trial centres (Guangdong Provincial Hospital of Chinese Medicine (B2014-026-01), Affiliated Hospital of Tianjin Chinese Medicine Academy (2014-KY-001) and Third Hospital of Hangzhou (B2014-026-01)). The findings will be disseminated to the public through conference presentations and open-access journals.
Trial registration number
Chinese Clinical Trial Registry (ChiCTR-TRC-14005185); Pre-results.
Keywords: psoriasis, chinese herbal medicine, clinical trial, protocol
Strengths and limitations of this study.
We are performing a trial to provide evidence regarding the clinical effectiveness of a Chinese medicine treatment for psoriasis before and after optimisation and simplification.
There is no absolute placebo control, which means that this trial will be unable to assess the absolute efficacy and will assess only the relative efficacy.
For broad use of the herbal formula, we designed PSORI-CM01 based on the rule ‘treated from the blood’, which is related to the core pathogenesis of psoriasis in traditional Chinese medicine (TCM) theory.
There is no stratification based on TCM syndromes in the design of the trial because PSORI-CM01 can be applied to the blood heat, blood stasis and blood dryness syndromes of psoriasis.
Background
Psoriasis is a chronic, immune-mediated, inflammatory skin disease characterised by erythema, scale and redness, and thickening and scaling of the skin. The main histopathological change of psoriasis is accelerated keratinocyte cell proliferation.1 2 However, the cause of this disease remains unknown. Although an early concept of the pathogenesis of psoriasis focused on the proliferation and differentiation of keratinocytes, recent studies have recognised that dysregulation of the immune system plays a critical role in the development of psoriasis. The interactions between dendritic cells, T cells, keratinocytes, neutrophils and the cytokines released from immune cells are the core mechanism of the development of psoriasis.3 Genetic, environmental and behavioural factors are thought to be triggers that contribute to the onset of psoriasis.4 The prevalence of psoriasis in adults is estimated to range from 0.91% to 8.5% worldwide.5 Clinically, psoriasis vulgaris (PV) is the most common subtype of psoriasis and affects approximately 90% of patients.6
The most common treatments for psoriasis include topical medication, ultraviolet light, systematic drugs and biologics. Topical medications, such as corticosteroids, retinoid and vitamin D analogues, are considered to be first-line therapies for PV. Systematic drugs are for severe psoriasis, while ultraviolet light and biologics are used when applicable and necessary.7
A series of systematic reviews have demonstrated that Chinese medicine contains an effective therapy for psoriasis.8–16 Yinxieling tablets, which are a Chinese herbal medicine compound preparation with 10 ingredients (ie, Angelica sinensis, radix paeoniae rubra, Chloranthus spicatus, smoked plum, radix rehmanniae recen, Ligusticum wallichii, radices lithospermi, Curcuma zedoaria, rhizome smilacis glabrae and liquorice), that is used for the treatment of psoriasis was developed by the National Medical Master Xuan Guowei, who is a well-known Chinese medicine doctor. These tablets were formulated according to traditional Chinese medicine (TCM) theory and are theoretically effective and safe. In TCM theory, three syndromes of psoriasis are generally acknowledged: blood stasis, blood heat and blood dryness type. In the acute stage, the pathogenesis of PV is mostly blood heat that is obstructed on the surface of the skin. In the chronic stage, the pathogenesis of PV is blood deficiency that develops into dryness that prohibits the nourishing of the skin or blood stasis that obstructs blood flow in skin collaterals. Therefore, activating blood circulation and removing blood stasis should be the focus of curing of psoriasis. Yinxieling tablets play the role of activating blood circulation and removing blood stasis in the treatment of psoriasis.17
In the recent 20 years of clinical practice, Yinxieling tablets have been extensively used for the treatment of psoriasis and have exhibited a promising clinical efficacy in terms of relieving the symptoms of psoriasis and reducing the relapsing rate. Molecular biological technologies have been used to analyse the pharmacological mechanisms of multiple ingredients in Yinxieling tablets.18 19 These studies have demonstrated that Yinxieling tablets are involved in the regulation of immune-mediated cells and the interaction of cellular cytokines, which has revealed the potential mechanism of Yinxieling tablets in the treatment of psoriasis. In the exploration of the molecular and pharmacological mechanisms of Yinxieling tablets, two clinical trials have been performed to confirm their clinical effectiveness. In Wang et al’s study, 24 patients with psoriasis were equally randomised into the following two groups: a treatment group that received Yinxieling tablets for 8 weeks and a control group that received acitretin capsules for 8 weeks. The therapeutic effect of the Yinxieling tablets in the treatment of psoriasis was similar to that of the acitretin capsules, but fewer side effects appeared in the Yinxieling tablet group.20 In Dai et al’s study, 90 patients in observation groups were treated with Yinxieling, and 30 patients in a control group were treated with placebo for 8 weeks. The result revealed that the Yinxieling decoction had a therapeutic effect on PV.21 However, there are limitations to the further development of Yinxieling because of its complex compounds.
To expand the application of Yinxieling, an optimised formula, that is, PSORI-CM01 (former name YXBCM01), was developed. This formula is composed of only seven ingredients (ie, radix paeoniae rubra, smoked plum, C. spicatus, radices lithospermi, C. zedoaria, rhizome smilacis glabrae and liquorice) of the Yinxieling tablet that were found to have positive correlations with pharmacodynamic indicators based on a computerised systematic pharmacological method and orthogonal experiments.22 23 An observational study revealed that 2 months of treatment with PSORI-CM01 for PV reduced the Psoriasis Area and Severity Index (PASI) and Dermatology Life Quality Index (DLQI) scores with no adverse events.24 Another 12-week observational study revealed that the PASIs of patients with psoriasis were reduced after PSORI-CM01 treatment, and the metabolic variations were observed in patients with psoriasis before and after PSORI-CM01 treatment.25 Our previous study demonstrated that PSORI-CM01 can reduce keratinocyte proliferation in vitro and inhibit epidermal hyperplasia in an imiquimod-induced psoriasis-form mouse model.26 The PSORI-CM01 formula can also affect the Th-17/IL-23 axis and inhibit the expression of cytokines and chemokines and thus improve inflammatory conditions in the dermic microenvironment.27
However, the previous studies of PSORI-CM01 are all based on preliminary clinical observations and animal experiments. Whether the clinical efficacy and safety of PSORI-CM01 granules are better than those of its prototype, that is, the Yinxieling tablet, remains uncertain. Therefore, a rigorously designed randomised controlled trial to determine whether PSORI-CM01 is more effective than the Yinxieling tablet and to investigate the efficacy and safety of this new formula is warranted.
Methods
Design
This is a double-dummy, double-blind, randomised, controlled trial to investigate the efficacy and safety of the new formula PSORI-CM01 granule compared with its prototype, the Yinxieling tablet. This study will be performed in three centres in China: the Guangdong Provincial Hospital of Chinese Medicine (GPHCM), the Affiliated Hospital of Tianjin Chinese Medicine Academy and the Third Hospital of Hangzhou. Because Yinxieling tablets and PSORI-CM01 granules have different preparation forms, a double-dummy, double-blind trial design was selected to guarantee rigorous blinding.
The study procedure consists of three components, that is, an initial screening, a treatment period and a follow-up period. In the initial screening, patients with psoriasis will be recruited via a dermatology clinic for physical examination and inclusion assessment. A 2-week run-in period may be requested depending on the results of the assessments. If eligible, written informed consent will be requested of the participants. Additional consent provisions for collection and use of participant data and biological specimens will be requested as well. All details of the informed consent will be clearly explained to the participant to assure their understanding. Once informed consent is obtained, a participant will be given a random sequence number. All participants will be allocated into two groups at a ratio of 1:1. One group will receive PSORI-CM01 granules with Yinxieling placebo tablets, and the other group will receive Yinxieling tablets with PSORI-CM01 placebo granules (figure 1). We will collect patients’ information about TCM syndromes before and after the treatment. Target lesions will be recorded with digital photographs taken with single-lens reflex cameras at every visit.
Figure 1.
Flow chart of the study.
The trial protocol was approved by the GPHCM ethics committee and registered with the Chinese Clinical Trial Registry (ChiCTR-TRC-14005185).
Eligibility criteria
Inclusion criteria
The patients must meet all of the following criteria at the time of randomisation to be eligible for recruitment:
The patients must meet the criteria for the diagnosis of PV referred to in the Clinical Guidelines of Psoriasis 2008 reported by the Chinese Medical Association.28
Male and female patients must be between 18 and 65 years old.
A PASI of more than 3 and less than 30, and a body surface area (BSA) of less than 30% are required.
Informed consent must be obtained.
Exclusion criteria
The trial exclusion criteria include any of the following:
Psoriatic lesions can only be seen on the face, scalp, nails, anus, mucus and palmar-plantar areas.
Acute progressive psoriasis, an erythroderma tendency and psoriatic arthritis (PsA) are present.
Patients who are pregnant, lactating and those who plan to become pregnant within a year will be excluded.
Those with a Self-rating Anxiety Scale more than 50 or an Self-rating Depression Scale more than 53, and those with other psychiatric disorders will be excluded.
Those with a history of primary cardiovascular, respiratory, digestive, urinary, endocrinological and haematological diseases that cannot be controlled with ordinary treatments will be excluded. Those with malignant diseases, infections, electrolyte imbalances and acid-base disturbances will be excluded. Patients with the following clinical test results will be excluded: an aspartate transaminase or alanine transaminase three times greater than the normal upper limit, creatinine 1.5 times greater than the normal upper limit; haemoglobin elevated by 20 g/dLabove the normal upper limit; a platelet count less than 75.0×109/L; a white cell count less than 3.0×109/L and other abnormal laboratory test results, as assessed by the investigators, which are not suitable for this clinical study.
Patients who are allergic to any medicine or ingredients used in this study will be excluded.
Those participating other clinical trials and those who have participated in trials within 1 month will be excluded.
Patients who have used corticosteroids or retinoic acid acting on the skin over the previous 2 weeks, those on systemic therapy or phototherapy (ultraviolet light B and psoralen and ultraviolet A) with the previous 4 weeks and those on biological therapy over the previous 12 weeks will be excluded.
Interventions
PSORI-CM01 group
Participants in PSORI-CM01 group will receive 5.5 PSORI-CM01 granules two times daily after meals and five placebo tablets three times daily after meals for 12 weeks.
Yinxieling group
Participants in Yinxieling group will receive five Yinxieling tablets three times daily after meals and placebo granules 5.5 g two times daily after meals for 12 weeks.
Outcome measures
Primary outcome
The primary outcome is the reduction in the PASI score, which will be calculated as follows:
Reduction of the PASI=PASI at baseline−PASI at week 12.
The PASI scores of the patients will be assessed every 2 weeks during the treatment period and every 4 weeks during the follow-up period. The PASI reduction calculated at week 12 will be considered the primary outcome.
Secondary outcomes
The secondary outcome measures include relapse rate, BSA, Visual Analogue Scale (VAS) and DLQI. The VAS and BSA will be assessed every 2 weeks during the treatment period and every 4 weeks in the follow-up period. The DLQI will be assessed by the patients every 4 weeks during the treatment period. In the follow-up period, the DLQI will only be assessed at the last week (week 24). Laboratory reports were also be monitored until the last visit (table 1).
Table 1.
Schedule for treatment and outcome measurements
| Period | Enrolment | Allocation | Treatment period | Follow-up period | ||||||||
| Time points | −1 week | 0 week | 2 weeks | 4 weeks | 6 weeks | 8 weeks | 10 weeks | 12 weeks | 16 weeks | 20 weeks | 24 weeks | |
| Enrolment | Eligibility screening | ● | ||||||||||
| Informed consent | ● | |||||||||||
| Characteristic | ● | |||||||||||
| Medical history | ● | |||||||||||
| Laboratory examination | ● | ● | ||||||||||
| Biological specimens | ● | ● | ||||||||||
| Random allocation | ● | |||||||||||
| Intervention | PSORI-CM01 granules and placebo tablets |
|
||||||||||
| Yinxieling tablets and placebo granules |

|
|||||||||||
| Assessment | TCM syndrome | ● | ● | ● | ||||||||
| PASI | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | |
| BSA | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | |
| VAS | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | |
| DLQI | ● | ● | ● | |||||||||
| SAS | ● | |||||||||||
| SDS | ● | |||||||||||
| Safety assessment | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | |
✩For PSORI-CM01 group.
★For Yinxieling group.
BSA, body surface area; DLQI, Dermatology Life Quality Index; PASI, Psoriasis Area and Severity Index; SAS, Self-rating Anxiety Scale; SDS, Self-rating Depression Scale; TCM, traditional Chinese medicine; VAS, Visual Analogue Scale.
Health economics
An economic evaluation will be performed from the perspective of the Health Department of Guangdong Province and will occur in the form of cost–utility analysis and will be conducted using utility values obtained from the DLQI preference-based quality of life measure. The DLQI is a dermatology-specific quality of life instrument for routine clinical use. This instrument is a validated questionnaire with a simple 10-question format. At present, the DLQI is the most frequently used instrument for evaluating the effects of skin disease and related treatments on patients’ lives. The DLQI will be measured at baseline and at 4 and 16 weeks for utility-based quality-of-life evaluation in this study. Resource use will include intervention costs, healthcare costs and community service costs, which will be calculated for each trial participant. We will analyse an incremental cost-effectiveness ratio of the cost per patient by calculating the incremental mean difference in costs between the two trial arms and the incremental difference in patient outcome after the follow-up.
Sample size
Due to the lack of studies evaluating the effects of PSORI-CM01 granule and Yinxieling tablets on psoriasis that are available for sample size calculation, we performed the sample calculation based on our previous study’s results and experts’ opinions.29 The superiority test for two means was used for the sample size calculation. We assumed that the superiority margin of the PASI was 1.5, and the SD were 1.1 and 2.5 for the PSORI-CM01 granules and Yinxieling tablets, respectively. The significance level (alpha) of the test was 0.025, and statistical power was 80%. A sample size of 236 was deemed necessary for the each arm after the calculations. Considering a 15% loss to follow-up, 278 patients are needed in each arm for a total of 556 patients. The PASW Statistics software (V.18.0) was used for the calculations.
Randomisation and allocation
Eligible patients will be randomly assigned, in a 1:1 ratio, to one of the two treatment groups (PSORI-CM01 group or Yinxieling group) at the second visit through central randomisation. Equal randomisation will be conducted using a computer-generated random allocation sequence through the stratified block randomisation method of the SAS software (V.9.12) by the Key Unit of Methodology in Clinical Research (KUMCR) of GPHCM. Allocation concealment will be ensured, as the randomisation code will be released by the Interactive Web Response System for Chinese Medicine Trials, which was a verified online randomisation facility established by the KUMCR (http://www.gztcmgcp.net/sjxt/login.asp). After that, the participants will be randomly allocated to two different treating groups.
Test drugs and blinding
After preliminary clinical observations, we changed the form of the PSORI-CM01 formula to granules because the preparation of oral granules normally involves smooth, quick water absorption and swelling properties that allow for easy swallowing.
The PSORI-CM01 granules and the matching placebo granules used in the trial were prepared by Tianjiang Pharmaceutical (Jiangyin, Jiangsu Province, China). The Yinxieling tablets and the matching placebo tablets were prepared by Kangyuan Pharmaceutical (Guangzhou, Guangdong Province, China). All of the above drugs met the requirements of Good Manufacturing Practice. The main ingredients of the placebo granules and the placebo tablets are maltodextrin, lactose and a natural edible pigment, and these ingredients are similar to those of the PSORI-CM01 granules and Yinxieling tablets in appearance, weight and taste.
The practitioners will be blind to the allocation arm, and the arms will have similar medical procedures. Moreover, the evaluations of the participants and the analysis of the results will be performed by physician assessors and statisticians who are blinded to the group allocation.
Statistical analysis
All analyses will be performed with PASW Statistics and SAS V.9.2 software by a statistician who is blinded to the random allocation of groups. Intent-to-treat (ITT)-based statistical analyses with 95% CIs will be performed. The ITT analyses will include all of the patients who are randomised.30 Safety analysis will be undertaken by analysing the frequency of adverse events that are suspected to be related to the treatment. The various parameters observed will be compared using the χ2 test for non-continuous variables (ie, the primary outcome and relapse rate), and t-tests and analyses of variance (ANOVAs) will be used for the continuous variables. Rank or skewed (not follow normality) data in these analyses will be examined using Wilcoxon signed-rank test. To distinguish the treatment effect and the time effect, repeated measures analysis of variance of the change from baseline will be performed for the different time point assessments. A subgroup analyses will be performed based on the severity of the disease and the TCM syndromes. Statistical significance will be established at p<0.05.
Adverse events
Before the beginning of, and after 12 weeks of treatment, medical histories will be recorded for each patient, and standard laboratory examinations and specific laboratory investigations will also be performed. The standard laboratory examinations will include the following: haematological parameter assessment (haemoglobin and red blood cell, platelet and white cell counts); urinalysis (proteins and red blood cell and white cell biochemical assessments (serum electrolytes), indices of renal function (creatinine and urea) and hepatic function (alkaline phosphatase, aspartate aminotransferase, alanine aminotransferase, and g-glutamyl-transpeptidase); and ECG. The specific laboratory investigations mainly include the serum cytokine levels.
All adverse events will be collected and graded for severity and potential relation to the treatments by assessors at every visit. The safety evaluations include the incidence of treatment-induced or serious adverse events, dropout due to adverse events and laboratory parameter changes. In cases of severe adverse effects, all drugs in this trial will be immediately discontinued.
Data management
All physicians, assessors and research assistants will attend training workshops before the conduction of trial. Investigators in different centre will all be required to follow the standard operating procedures. The quality controllers from the contract research organisation Guangdong International Clinical Research Center of Chinese Medicine (Guangzhou, China) will perform regular monitoring in each centre throughout the trial. All study data will be managed as detailed in the full trial protocol and in accordance with the data management plan, which was developed by the data monitoring committee of the GPHCM. The data collection will include all information in the case report forms. The data will be entered using the double entry method. To ensure data quality and data consistency between the source data and the data entered into the database, two research assistants will independently input the data from the CRFs into database using a prespecified database software that was developed by the data monitoring committee. The data monitoring committee will assess the safety data and the critical efficacy outcomes after the trial is finished.
Discussion
Psoriasis is a disease of immune abnormality that progresses slowly over a long period with frequent symptom recurrences. Psoriasis causes detrimental effects on the quality of life of both adults and children. Elevated rates of various psychopathologies, including poor self-esteem, sexual dysfunction, anxiety, depression and suicidal ideation, have been reported in patients with psoriasis.31–35 Psoriasis is not a disease that only affects the skin. Increasing evidence supports the recognition of psoriasis as a chronic multisystem inflammation disorder with multiple associated comorbid conditions. Comorbidities linked to psoriasis include (PsA), cardiovascular diseases, obesity, metabolic syndrome, malignancy, hypertension and inflammatory bowel disease.25 PsA is an erosive and deforming joint disease that is associated with psoriasis and affects 7%–42% of the psoriasis population.36 PsA-induced joint damaging complications lead to lower articular function and higher mortality and affect patients’ abilities to work and their social relationships.37 Inpatients with severe psoriasis, the life expectancy is reduced by 5 years primarily due to cardiovascular disease.37 Additionally, psoriasis has a strong connection with metabolic syndrome, which makes it a marker for increased risks of the morbidities and mortalities associated with these diseases.38 Psoriasis can also cause substantial economic loss. According to a systematic literature review conducted by the American Academy of Dermatology, the total direct and indirect burden of psoriasis is estimated to be US$35.2 billion in the USA per annum.39
The treatments used for moderate to severe psoriasis (ie, phototherapy and oral systemic and biological therapies) were received by 27.3% of the total psoriasis sample, of whom 37.2% used biologics.40 Orally administered Chinese herbal medicine has been used for the clinical management of psoriasis for years. However, a number of high-quality clinical trials are needed before Chinese herbal medicine can be recommended for psoriasis. We conducted a series of systematic reviews to evaluate the effects of Chinese herbal medicine alone and in combination with pharmacotherapy for psoriasis.8–16 The results revealed that there is promising evidence of positive effects from a number of studies of multiherb formulations.
We changed the form of the PSORI-CM01 formula to granules in this study. Considering too many blood-activating and stasis-dissolving drugs would cause consumption of Qi, we removed A. sinensis, radix rehmanniae recen, Ligusticum wallichii from Yinxieling. The remain seven herbs turned to be PSORI-CM01. Tablets containing micronised Chinese herbal medicine are not suitable for immediate release. Granules are solid when stored and will swell and gel via water absorption. Additionally, granules from simplified formulations offer great opportunities to improve continuous processes, present performances comparable to more complicated formulations and are able to correspond to the requirements of the authorities. In this study, the microstructure and tensile strength of the granules resembled those of the tablets formed from the original ungranulated powder.
To our knowledge, this trial is the first study to compare the clinical effectiveness of Chinese medicine treatment for psoriasis before and after optimisation and simplification. Moreover, we aim to provide supporting data for the effectiveness of the PSORI-CM01 granule that resulted from the optimisation of Yinxieling tablet as determined in a previous study and clinical practice. This study is the third clinical trial that our research team has conducted on the effectiveness of the PSORI-CM01 granule for patients with psoriasis. The first study compared oral PSORI-CM01 granule plus topical sequential therapy for moderate to severe psoriasis and was a double-blind, randomised, placebo-controlled trial that evaluated the effectiveness of PSORI-CM01 combined with usual topical therapy compared with the usual topical therapy that is used in the clinical practice of Western medicine alone.29 41 The second study evaluated oral PSORI-CM01 granule plus topical calcipotriol for psoriasis relative to placebo plus topical calcipotriol over 12 weeks; this study was a pilot randomised, placebo-controlled, double-blinded trial.42 These two trials aimed to evaluate the benefits of the addition of PSORI-CM01 granules compared with conventional treatments of psoriasis. In contrast to the above two trials, the present clinical trial protocol acts as the foundation for evaluating the treatment of psoriasis with Chinese medicine.
For facilitating appropriate reference standards for scientific, ethical and safety issues before the trial begins, this protocol has been developed according to Standard Protocol Items: Recommendations for Interventional Trials 2013 and Consolidated Standards of Reporting Trials statement.43 44
Ethics and dissemination
This research protocol had been reviewed and approved by the institutional review boards of three trial centres (Guangdong Provincial Hospital of Chinese Medicine (B2014-026-01), Affiliated Hospital of Tianjin Chinese Medicine Academy (2014-KY-001) and Third Hospital of Hangzhou (B2014-026-01)).
The Biological Resource Centre of GPHCM approved the biobank procedure. Written informed consent will be given by participants. The informed consent forms for participation in clinical trial and the biobanking part are separated. The results will be disseminated to the public through conference presentations and open access journals.
Trial status
The recruitment phase began in November 2014. Thus far, 63 patients have been recruited. The estimated end date for this study is in October 2018.
Supplementary Material
Acknowledgments
We thank Professor Guo-Wei Xuan (Guangdong Provincial Hospital of Chinese Medicine, Guangzhou, China), Professor Ai-E Xu and Professor Jun-Jun Shan (The Third Hospital of Hangzhou, Hangzhou, China), Professor Jun-ling Zhang and Professor Hong-mei Wang (Affiliated Hospital of Tianjin Chinese Medicine Academy) for their suggestions. We also thank Wen-Wei Ouyang and Li-Ming Lu (Guangdong Provincial Hospital of Chinese Medicine) for comments and suggestions on data management and the statistical analysis plan.
Footnotes
Contributors: JD, DY and CL drafted the manuscript. CL and ZW participated in the design of the study, DY, YY, ZH, HW and HD coordinate the study. All authors participated in, read and approved the final manuscript.
Funding: This research was supported by grants of the National Key Technology R&D Program for the 12th Five-year Plan of Ministry of Science and Technology, China (no 2013BAI02B03), Provincial Science and Technology Project of Guangdong Province, China (no 2015B020211013) and Guangdong Provincial Bureau of traditional Chinese Medicine Research Project (no 20161110).
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Institutional Ethics Committee of Guangdong Provincial Hospital of Traditional Chinese Medicine.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Sociedade Brasileira de Dermatologia. Consenso brasileiro de psoríase. Rio de Janeiro: Sociedade Brasileira de Dermatologia, 2009. [Google Scholar]
- 2. Perera GK, Di Meglio P, Nestle FO. Psoriasis. Annu Rev Pathol 2012;7:385–422. 10.1146/annurev-pathol-011811-132448 [DOI] [PubMed] [Google Scholar]
- 3. Ben Salem C, Hmouda H, Bouraoui K. Psoriasis. N Engl J Med 2009;361:1710 10.1056/NEJMc091749 [DOI] [PubMed] [Google Scholar]
- 4. Chandra A, Ray A, Senapati S, et al. . Genetic and epigenetic basis of psoriasis pathogenesis. Mol Immunol 2015;64:313–23. 10.1016/j.molimm.2014.12.014 [DOI] [PubMed] [Google Scholar]
- 5. Parisi R, Symmons DP, Griffiths CE, et al. . Global epidemiology of psoriasis: a systematic review of incidence and prevalence. J Invest Dermatol 2013;133:377–85. 10.1038/jid.2012.339 [DOI] [PubMed] [Google Scholar]
- 6. Griffiths CE, Barker JN. Pathogenesis and clinical features of psoriasis. Lancet 2007;370:263–71. 10.1016/S0140-6736(07)61128-3 [DOI] [PubMed] [Google Scholar]
- 7. Nast A, Boehncke WH, Mrowietz U, et al. . German S3-guidelines on the treatment of psoriasis vulgaris (short version). Arch Dermatol Res 2012;304:87–113. 10.1007/s00403-012-1214-8 [DOI] [PubMed] [Google Scholar]
- 8. Zhang CS, Yang L, Zhang AL, et al. . Is Oral Chinese Herbal Medicine Beneficial for Psoriasis Vulgaris? A Meta-Analysis of Comparisons with Acitretin. J Altern Complement Med 2016;22:174–88. 10.1089/acm.2014.0212 [DOI] [PubMed] [Google Scholar]
- 9. May BH, Zhang AL, Zhou W, et al. . Oral herbal medicines for psoriasis: a review of clinical studies. Chin J Integr Med 2012;18:172–8. 10.1007/s11655-012-1008-z [DOI] [PubMed] [Google Scholar]
- 10. Zhang CS, Yu JJ, Parker S, et al. . Oral Chinese herbal medicine combined with pharmacotherapy for psoriasis vulgaris: a systematic review. Int J Dermatol 2014;53:1305–18. 10.1111/ijd.12607 [DOI] [PubMed] [Google Scholar]
- 11. Deng S, May BH, Zhang AL, et al. . Plant extracts for the topical management of psoriasis: a systematic review and meta-analysis. Br J Dermatol 2013;169:769–82. 10.1111/bjd.12557 [DOI] [PubMed] [Google Scholar]
- 12. Deng S, May BH, Zhang AL, et al. . Topical herbal formulae in the management of psoriasis: systematic review with meta-analysis of clinical studies and investigation of the pharmacological actions of the main herbs. Phytother Res 2014;28:480–97. 10.1002/ptr.5028 [DOI] [PubMed] [Google Scholar]
- 13. Yang L, Zhang CS, May B, et al. . Efficacy of combining oral Chinese herbal medicine and NB-UVB in treating psoriasis vulgaris: a systematic review and meta-analysis. Chin Med 2015;10:27 10.1186/s13020-015-0060-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Deng S, May BH, Zhang AL, et al. . Phytotherapy in the management of psoriasis: a review of the efficacy and safety of oral interventions and the pharmacological actions of the main plants. Arch Dermatol Res 2014;306:211–29. 10.1007/s00403-013-1428-4 [DOI] [PubMed] [Google Scholar]
- 15. Yu JJ, Zhang CS, Zhang AL, et al. . Add-on effect of chinese herbal medicine bath to phototherapy for psoriasis vulgaris: a systematic review. Evid Based Complement Alternat Med 2013;2013:673078 10.1155/2013/673078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Deng S, May BH, Zhang AL, et al. . Topical herbal medicine combined with pharmacotherapy for psoriasis: a systematic review and meta-analysis. Arch Dermatol Res 2013;305:179–89. 10.1007/s00403-013-1316-y [DOI] [PubMed] [Google Scholar]
- 17. Lu CJ, Yu JJ, Deng JW. Disease-syndrome combination clinical study of psoriasis: present status, advantages, and prospects. Chin J Integr Med 2012;18:166–71. 10.1007/s11655-012-1006-1 [DOI] [PubMed] [Google Scholar]
- 18. Han L, Peng Y, Zhao RZ, et al. . Effect of yinxieling on proliferation of HaCaT. J Guanghou Univ TCM 2011;28:159–62. [Google Scholar]
- 19. Cz L, Xx W, Liu FN. Effect of Yinxieling on PCNA expressionand apoptosis of keratinocyte. Trad Chin Drug Res Clin Pharmacol 2006;17:329–31. [Google Scholar]
- 20. Wang L, Yongjing H, Wang M. Clinical observation of yinxieling tablets for the treatment of Psoriasis Vulgaris. J Tradit Chin Med 2009;26:520–5. [Google Scholar]
- 21. Dai YJ, Li YY, Zeng HM, et al. . Effect of Yinxieling decoction on PASI, TNF-α and IL-8 in patients with psoriasis vulgaris. Asian Pac J Trop Med 2014;7:668–70. 10.1016/S1995-7645(14)60113-9 [DOI] [PubMed] [Google Scholar]
- 22. Yan YH, Zhao RZ, Cj L. Optimization of Yinxieling Capsule with orthogonal design. 25: Lishizhen medicine and materia medica research, 2014:2763–5. [Google Scholar]
- 23. Zhu W, Songmin H, Xiaohong Y, et al. . Computerized systematic pharmacological research of Yinxieling formula. Trad Chin Drug Res Clin Pharmacol 2011;22:379–82. [Google Scholar]
- 24. Yan YH, Cj L. Effect of modified Yinxieling on pustularpsoriasis. Trad Chin Drug Res Clin Pharmacol 2011;22:691–3. [Google Scholar]
- 25. Lu C, Deng J, Li L, et al. . Application of metabolomics on diagnosis and treatment of patients with psoriasis in traditional Chinese medicine. Biochim Biophys Acta 2014;1844:280–8. 10.1016/j.bbapap.2013.05.019 [DOI] [PubMed] [Google Scholar]
- 26. Wei JA, Han L, Lu CJ, et al. . Formula PSORI-CM01 eliminates psoriasis by inhibiting the expression of keratinocyte cyclin B2. BMC Complement Altern Med 2016;16:255 10.1186/s12906-016-1234-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Han L, Sun J, Lu CJ, et al. . Formula PSORI-CM01 inhibits the inflammatory cytokine and chemokine release in keratinocytes via NF-κB expression. Int Immunopharmacol 2017;44:226–33. 10.1016/j.intimp.2017.01.023 [DOI] [PubMed] [Google Scholar]
- 28. Psoriasis Group of Dermatology and Venereology: Chinese Medical Association. Clinical guidelines of psoriasis 2008. Chin J Dermatol 2009;42:213–4. [Google Scholar]
- 29. Yao DN, Lu CJ, Wen ZH, et al. . Oral PSORI-CM01, a Chinese herbal formula, plus topical sequential therapy for moderate-to-severe psoriasis vulgaris: pilot study for a double-blind, randomized, placebo-controlled trial. Trials 2016;17:140 10.1186/s13063-016-1272-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sedgwick P. What is intention to treat analysis? BMJ 2013;346:f3662 10.1136/bmj.f3662 [DOI] [Google Scholar]
- 31. Kimball AB, Jacobson C, Weiss S, et al. . The psychosocial burden of psoriasis. Am J Clin Dermatol 2005;6:383–92. 10.2165/00128071-200506060-00005 [DOI] [PubMed] [Google Scholar]
- 32. Kimball AB, Wu EQ, Guérin A, et al. . Risks of developing psychiatric disorders in pediatric patients with psoriasis. J Am Acad Dermatol 2012;67:651–7. 10.1016/j.jaad.2011.11.948 [DOI] [PubMed] [Google Scholar]
- 33. Russo PA, Ilchef R, Cooper AJ. Psychiatric morbidity in psoriasis: a review. Australas J Dermatol 2004;45:155–61. 10.1111/j.1440-0960.2004.00078.x [DOI] [PubMed] [Google Scholar]
- 34. Yang YW, Kang JH, Lin HC. Increased risk of psoriasis following obstructive sleep apnea: a longitudinal population-based study. Sleep Med 2012;13:285–9. 10.1016/j.sleep.2011.07.018 [DOI] [PubMed] [Google Scholar]
- 35. Farley E, Menter A. Psoriasis: comorbidities and associations. G Ital Dermatol Venereol 2011;146:9–15. [PubMed] [Google Scholar]
- 36. Slobodin G, Rosner I, Rozenbaum M, et al. . Psoriatic arthropathy: where now? Isr Med Assoc J 2009;11:430–4. [PubMed] [Google Scholar]
- 37. Abuabara K, Azfar RS, Shin DB, et al. . Cause-specific mortality in patients with severe psoriasis: a population-based cohort study in the U.K. Br J Dermatol 2010;163:586–92. 10.1111/j.1365-2133.2010.09941.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Voiculescu VM, Lupu M, Papagheorghe L, et al. . Psoriasis and metabolic Syndrome–scientific evidence and therapeutic implications. J Med Life 2014;7:468–71. [PMC free article] [PubMed] [Google Scholar]
- 39. Vanderpuye-Orgle J, Zhao Y, Lu J, et al. . Evaluating the economic burden of psoriasis in the United States. J Am Acad Dermatol 2015;72:961–7. 10.1016/j.jaad.2015.02.1099 [DOI] [PubMed] [Google Scholar]
- 40. Takeshita J, Gelfand JM, Li P, et al. . Psoriasis in the US medicare population: prevalence, treatment, and factors associated with biologic use. J Invest Dermatol 2015;135:2955–63. 10.1038/jid.2015.296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wen ZH, Xuan ML, Yan YH, et al. . Chinese medicine combined with calcipotriol betamethasone and calcipotriol ointment for Psoriasis vulgaris (CMCBCOP): study protocol for a randomized controlled trial. Trials 2014;15:294 10.1186/1745-6215-15-294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Parker S, Zhang AL, Zhang CS, et al. . Oral granulated Chinese herbal medicine (YXBCM01) plus topical calcipotriol for psoriasis vulgaris: study protocol for a double-blind, randomized placebo controlled trial. Trials 2014;15:495 10.1186/1745-6215-15-495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Chan AW, Tetzlaff JM, Altman DG, et al. . SPIRIT: statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;2013:200–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel group randomized trials. BMC Med Res Methodol 2001;1:2 10.1186/1471-2288-1-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.