Abstract
Objective
Traumatic events, particularly those interpersonal in nature, are associated with increased risk for co-occurring sequelae, including sleep disturbances, posttraumatic stress disorder (PTSD), and alcohol use disorder (AUD). However, the associations between these phenotypes have not been explored among college students.
Methods
We examined relationships between type of potentially traumatic event (PTE) exposure (pre-college) and sleep disturbances, as well as mediating effects of lifetime PTSD and AUD symptoms on these relationships, in a large undergraduate sample (N=1599, 64.7% female). Hierarchical linear regressions were conducted, beginning with demographics and adding interpersonal and accidental PTEs in a stepwise regression. Following, mediation analyses were run.
Results
Within the sample, 33.7% endorsed at least one interpersonal PTE, while 64.4% endorsed at least one accidental PTE. Hierarchical regressions demonstrated that interpersonal (β =0.202, p=0.000), but not accidental, PTE exposure significantly predicted disturbed sleep. Both PTSD and AUD symptoms significantly mediated (p values <0.001) the relationship between interpersonal PTE exposure and sleep, with indirect effects accounting for 61% and 17% of total effects, respectively. In the correlated mediation model, both disorders remained significant mediators (p < 0.001), with indirect effects accounting for 56% (PTSD symptoms) and 14% (AUD symptoms) of total effects on sleep.
Conclusions
Results suggest that interpersonal PTEs are more potent predictors of sleep problems than accidental PTEs. Further, trauma exposure psychiatric symptom sequelae (PTSD, AUD) account for part of the relationship between interpersonal PTE exposure and disturbed sleep, both independently and jointly, suggesting that treating PTSD and AUD symptoms in college students may also improve sleep.
Keywords: potentially traumatic events, sleep disturbances, posttraumatic stress disorder, alcohol use disorder, college students
1. Introduction1
College represents a period of increased vulnerability for poor quality and insufficient sleep, issues that are both pervasive and debilitating. College students sleep on average 6.5 hours per night (compared to the recommended 8.5–9.25 hours) [1]. Further, poor sleep quality in this population is common: ~38% of college students report poor sleep [1], with females in particular endorsing more sleep problems [2], and inadequate sleep is regularly cited as a top concern among college students [3]. Given the high prevalence of sleep problems in this population and associations between poor sleep and negative outcomes (e.g., related to mental health, school performance) [4], identification of factors associated with disturbed sleep in students is critical to inform prevention and intervention efforts.
One potential contributor to sleep disturbances is exposure to traumatic events, which are often associated with poor sleep, even years following the trauma [e.g., 5, 6, 7]. Young adulthood is the highest risk period for potentially traumatic event (PTE) exposure across the lifespan, putting college students at increased risk [8–11]. Traumatic events can be categorized as interpersonal (e.g., physical assault, sexual assault) or accidental (e.g., natural disasters, motor vehicle accidents), with interpersonal trauma experienced more frequently by women [12] and associated with greater risk for internalizing psychiatric disorders [e.g., 13]. However, few studies have explored sleep differences (e.g., disturbed sleep, insomnia) across sub-types of trauma exposure [14], and there is a lack of research examining the general relationships between trauma and sleep among college students specifically [15], despite college being a time of increased risk for both trauma exposure and sleep problems.
Although trauma exposure may have a direct effect on disturbed sleep, it could also be that common psychiatric sequelae of trauma, such as PTSD and alcohol use disorder [AUD] [e.g., 13], which have a high incidence of comorbidity [16] drive the association between trauma exposure and poor sleep. PTSD rates are high in college populations, ranging from 6% to 17% [17–20] and women are twice as likely as men to meet criteria for PTSD following a traumatic event [12]. Sleep disturbances (i.e., poor and/or insufficient sleep) are widely recognized as a “hallmark symptom” of PTSD [21–23], reflected in multiple symptom clusters of the disorder [24]. In fact, difficulties falling or staying asleep are reported by the majority of individuals with PTSD [25]. College students may also be at increased risk to misuse alcohol following a trauma exposure [e.g., 26, 27], a behavioral pattern that is also associated with poor sleep [e.g., 28, 29]. Alcohol use is common in this population and approximately half of college students binge drink [30], which per the National Institute on Alcohol Abuse and Alcoholism is defined as a “pattern of drinking that brings blood alcohol concentration (BAC) levels to 0.08 g/dL” and “typically occurs after 4 drinks for women and 5 drinks for men—in about 2 hours,” [31]. Binge drinking is associated with risk of development of AUD [32]. Alcohol use itself disrupts sleep cycles and is associated with worse sleep quality and shorter duration, despite being commonly used to cope [33]. Further adolescents with AUDs endorse poor sleep [34]. In college students, heavy alcohol use is correlated with insufficient sleep and sleep disorders, such as insomnia and parasomnias, as well as sleep timing [15, 28, 29, 35].
Given established associations between trauma and sleep [e.g., 5, 6, 7], trauma and psychiatric outcomes [e.g., 13], and psychiatric outcomes and poor sleep [e.g., 21, 36], it is critical to understand the relationships among these phenotypes. The association between trauma and sleep, although robust, may be significantly driven by PTSD and AUD symptoms, since these phenotypes are associated with exposure to trauma and poor sleep. However, there is a paucity of research on these relationships, particularly in college students, as stated above. Thus, the present study was conducted to examine relationships between exposure to PTEs, disturbed sleep, and common post-traumatic sequelae (PTSD and AUD symptoms) in a large undergraduate sample. Aims included: 1) examining trauma-related correlates of sleep disturbances, 2) using hierarchical regressions to determine the relative contribution of PTE type (interpersonal, accidental) on disturbed sleep, and 3) conducting analyses to determine whether or not the relationship between interpersonal PTE exposure and sleep disturbances is mediated by PTSD symptoms, AUD symptoms, or symptoms of both disorders.
2. Methods
2.1. Participants
The present study includes data from the fourth cohort (the only cohort where sleep items were fully assessed) of the Spit for Science study (S4S; N=1,854) in which incoming first year students in 2014 age 18 or older were invited to participate in a university-wide research study on college behavioral health. First year students who did not participate in the fall were sent additional e-mail invitations in the spring, thereby providing another opportunity to complete the survey. The survey given to participants enrolled in the spring asked participants to retrospectively report on the items from the fall survey. For Cohort 4, invitations were sent to 3519 individuals, with a 66% response rate. Participants were representative of the broader student population in terms of both gender and race/ethnicity.
2.2. Procedures
The University Institutional Review Board approved all study procedures and informed consent was obtained from all study participants. Study data were collected and managed using REDCap (Research Electronic Data Capture), a web-based application hosted at the University [37]. Participants received $10 and a t-shirt for their involvement. Additional detailed information concerning recruitment and study details can be found in Dick et al. [38], which reviews the Spit for Science study.
2.3. Measures
2.3.1 Potentially traumatic events (PTEs)
PTE exposure was assessed via an abbreviated version of the Life Events Checklist [39], which asked participants to report on the occurrence of five different stressful events: natural disasters, physical assaults, sexual assaults, other unwanted or uncomfortable sexual experiences, and transportation accidents. Participants completing the survey in the fall or retrospectively in the spring of their first year were given the response options of “yes” or “no” to items regarding whether each stressful event occurred “before the past 12 months”, “during the past 12 months”, “before starting college”, or “never happened to me”. Categories were further clustered by interpersonal (i.e., physical assaults, sexual assaults, other unwanted or uncomfortable sexual experiences) and accidental (i.e., natural disasters and transportation accidents) PTEs.
2.3.2. Probable PTSD symptoms
The PC-PTSD screener [40] was utilized to assess probable PTSD and each participant endorsing at least one lifetime PTE was asked “Have any of these experiences resulted in any of the following symptoms:” a) “Have had nightmares about it or thought about it when you did not want to?”, b) “Tried hard not to think about it or went out of your way to avoid situations that reminded you of it?”, c) “Were constantly on guard, watchful, or easily startled?”, d) “Felt numb or detached from others, activities, or your surroundings?”. A positive endorsement of an item was coded as a “1” and a sum score of the four items was used to index of PTSD symptoms. The items were found to possess good internal consistency (α = .93).
2.3.3. Alcohol Use Disorder (AUD) Symptoms
Lifetime AUD symptoms were assessed via 16 items derived from DSM criteria for AUD [24]. Example items include, “Has drinking ever interfered with your school, work, or household duties?”; “Have you been in a dangerous situation while drinking or drunk?”; “In situations where you couldn’t drink, did you ever have such a strong desire for it that you couldn’t think of anything else?”. Each item was answered using a three-point scale with the following answer options 1 = “never”, 2 = “1–2 times”, 3 = “3 or more times”. Participants endorsing a “3” were coded as positive for the symptom, and a sum of the 16 symptoms was calculated. Individuals who did not report drinking alcohol or ever having been drunk were coded as 0 for all AUD symptoms. AUD symptom sum scores ranged from 0–13. Due to the distribution of this variable with few students having a high number of symptoms, we collapsed the sum scores into an ordinal scale, with a new range of 0–3: 0 [0]; 1 [1]; 2 [2,3]; 3 [4+]. The items were found to possess good internal consistency (α = 0.94).
2.3.4. Sleep disturbances
Sleep disturbances were assessed via a modified 4-item version of the Pittsburgh Sleep Quality Index (PSQI) [41]. Items included those reflecting typical sleep duration, sleep latency (in minutes; past month), daytime dysfunction (past month), and self-reported sleep quality. Responses on each of the 4 items were recoded into a 0–3 scale, as is done in the full PSQI. Following, all 4 variables were summed to create a total sleep disturbance score, with a possible range of 0–12. This score was used whenever sleep is mentioned in all main analyses. Cronbach’s α for the sleep items was 0.63.
2.3.5. Demographics
Standard demographic variables, such as age, gender, and ethnicity, were assessed and used as covariates. We did not include age as a covariate, since there is a limited range within this student sample.
2.4. Data Analytic Plan
Descriptive statistics were run in SPSS Version 23. We restricted our analyses to individuals from Cohort 4 who completed their assessment in the first semester of their freshman year and who answered (were not missing on) trauma and alcohol items (84% of the initial Cohort 4 sample). There were no meaningful differences between individuals included and excluded. Thus, our subset of Cohort 4 included 1,599 participants (64.7% female; Mage=18.49, SD=0.39 at enrollment). Race was dummy coded and separated into three categories with Caucasian set as the reference group (52.6% of participants); 16.6% of participants were African American, 16.1 % were Asian, and 14.7% were grouped into the ‘Other’ category (comprised of American Indian/Native Alaskan, Hispanic/Latino, Native Hawaiian/Other Pacific Islander, more than one race, and unknown). The endorsement of individual sleep items was as follows: 16.3% (N=260) of the sample endorsed “fairly bad” or “very bad” sleep quality, while 18.9% (N=299) endorsed having trouble staying awake during daytime activities at least 1–2 times a week. For 24.8% (N=383) of individuals, it took over 30 minutes to fall asleep in the last month. Only 2.9% (N=46) reported less than 6 hours of sleep per night. Individuals endorsing at least one interpersonal PTE differed significantly from those who did not endorse any interpersonal PTEs across all four individual sleep items (X2 ranged from 30.5–47.5).
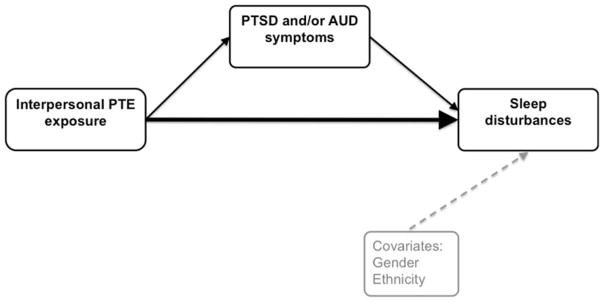
We began by examining correlations using R between key variables (trauma, total sleep disturbance score, PTSD symptoms, AUD symptoms). Following, a hierarchical regression analysis in SPSS was run to examine the potential unique effects of each PTE type on total sleep disturbance score, with independent variables entered step-wise, beginning with demographics (gender, race; Step 1), followed by interpersonal PTE (Step 2) and accidental PTE (Step 3). Next, mediation models (see Figure 1 for a theoretical path diagram) were conducted using MPlus 7.31. Three separate mediation models were run to examine potential indirect effects on the relationship between interpersonal PTE exposure and sleep disturbances. The first used PTSD symptoms as the mediator, the second used AUD symptoms as the mediator, and the third used both PTSD and AUD symptoms together as correlated mediators. Mplus uses the product of coefficients strategy to calculate indirect effects [42, 43]. In the simple case, partial mediation by a single variable (i.e., a partial indirect effect) is evaluated in relation to the Z-distribution, with the ratio of the product of the a and b path coefficients over the normal-theory SE for that product. When assessing the total indirect effect operating through multiple mediators, the sum of the products of coefficients taken over the square root of the asymptotic variance of the sum of those products provides a ratio to be evaluated in relation to the Z-distribution.
Figure 1.
Theoretical mediation model for interpersonal PTE exposure and sleep disturbances, with PTSD and/or AUD symptoms as the mediator(s).
3. Results
3.1. Demographic information and correlations
Demographic information and correlations for key variables are shown in Table 1. Interpersonal and accidental PTEs were strongly correlated. Interpersonal PTE exposure had robust, positive correlations with disturbed sleep (measured via total score), PTSD symptoms, and AUD symptoms, while accidental PTE exposure was negatively correlated with PTSD, and only weakly positively correlated with sleep and AUD symptoms. Sleep was moderately correlated with both PTSD and AUD symptoms, and AUD and PTSD symptoms also had a modest correlation. With regard to endorsement of PTEs, 426 (27.0%) individuals reported exposure to both interpersonal and accidental PTEs. The prevalence across specific accidental PTEs differed, as 826 (51.9%) individuals endorsed natural disaster and 607 (38.2%) endorsed transportation accident (X2 = 95.85, p = 0.000). For interpersonal PTEs, more individuals endorsed sexual assault or other sexual experience (N=357, 22.6%) than physical assault (N=315, 19.9%) (X2 = 109.37, p=0.000).
Table 1.
Demographic information and correlations across key variables used in analysis
| Mean (SD) | 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|---|
| 1. Interpersonal PTE (possible range: 0–1) | 535 (33.7) | 1.00 | -- | -- | -- | -- |
| 2. Accidental PTE (possible range: 0–1)1 | 1025 (64.4) | 0.42 | 1.00 | -- | -- | -- |
| 3. Sleep | 2.79 (1.86) | 0.29 | 0.09 | 1.00 | -- | -- |
| 4. PTSD symptoms | 1.27 (1.51) | 0.62 | −0.24 | 0.33 | 1.00 | -- |
| 5. AUD symptoms | 0.49 (0.88) | 0.30 | 0.06 | 0.20 | 0.21 | 1.00 |
Abbreviations: AUD = Alcohol use disorder, PTE = potentially traumatic event, PTSD=Posttraumatic stress disorder.
Note that when accidental PTE is separated into natural disaster and transportation accident, natural disaster has a negative correlation with PTSD, while transportation accident has a modest but positive correlation.
3.2. Hierarchical regression
Table 2 presents results of the hierarchical linear regression. In Step 1, female gender was associated with increased sleep disturbances (measured via total score). In Step 2, interpersonal PTE exposure was associated with increased sleep disturbance, and female gender from Step 1 was nominally significant. When accidental PTE exposure was added in Step 3, interpersonal PTE exposure remained significant and female gender was significant. However, accidental PTE exposure did not account for independent variance in disturbed sleep. Based on these results, mediation models were conducted using the interpersonal variable only.
Table 2.
Hierarchical regression models examining the joint effects of PTE type (interpersonal vs. accidental) on sleep
| Beta | t | Sig. | Adjusted R Square | F Change | Sig. F Change? | |
|---|---|---|---|---|---|---|
|
| ||||||
| Step 1: | 0.005 | 2.970 | 0.019* | |||
|
| ||||||
| Female gender | 0.081 | 3.123 | 0.002* | |||
|
|
||||||
| Ethnicity | ||||||
| AA | 0.022 | 0.800 | 0.424 | |||
| Asian | 0.029 | 1.085 | 0.278 | |||
| Other | 0.027 | 0.981 | 0.327 | |||
|
| ||||||
| Step 2: | 0.047 | 64.937 | 0.000* | |||
|
| ||||||
| Interpersonal PTE | 0.207 | 8.058 | 0.000* | |||
|
|
||||||
| Female gender | 0.050 | 1.922 | 0.055 | |||
|
|
||||||
| Ethnicity: | ||||||
| AA | 0.028 | 1.040 | 0.298 | |||
| Asian | 0.037 | 1.405 | 0.160 | |||
| Other | 0.022 | 0.824 | 0.410 | |||
|
| ||||||
| Step 3: | 0.046 | 0.509 | 0.476 | |||
|
| ||||||
| Interpersonal PTE | 0.202 | 7.589 | 0.000* | |||
|
|
||||||
| Accidental PTE | 0.019 | 0.713 | 0.476 | |||
|
|
||||||
| Female gender | 0.051 | 1.960 | 0.050* | |||
|
|
||||||
| Ethnicity: | ||||||
| AA | 0.028 | 1.046 | 0.296 | |||
| Asian | 0.038 | 1.420 | 0.156 | |||
| Other | 0.023 | 0.866 | 0.387 | |||
Abbreviations: AA = African American; PTE = potentially traumatic event; Sig. = significant.
indicates that this regression coefficient or change is significant.
3.3. Mediation models
Given the correlations between interpersonal PTE exposure, sleep, PTSD symptoms, and AUD symptoms, we chose to run three mediation models, shown in Table 3. PTSD symptoms were a significant mediator of the relationship between interpersonal PTE exposure and disturbed sleep, with 61.1% of the total effect being accounted for by PTSD symptoms (p < 0.001). AUD symptom count was also a significant mediator, with 16.8% of the effect indirectly coming from this variable (p < 0.001). Given that PTSD and AUD symptoms were correlated in our sample (r = 0.21), a combined mediation model was conducted that included their correlation, and the indirect effect of symptoms of both disorders was significant (p < 0.001), accounting for 69.3% of the total effect of interpersonal PTE exposure on sleep. PTSD symptoms accounted for the majority of this effect (55.6%) and AUD symptoms (13.8%) continued to have a significant indirect effect (both p values < 0.001) on the relationship between interpersonal PTE exposure and disturbed sleep.
Table 3.
Mediation models for PTSD and AUD symptoms
| Mediator | Model R2 | Total direct effect | Total indirect effect (mediation) | Total effect (indirect + direct) | Mediated proportion of total effect | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| β | SE | Ratio | β | SE | Ratio | β | SE | Ratio | |||
| Interpersonal PTE | |||||||||||
| PTSD symptoms | 0.120 | 0.344 | 0.114 | 3.02 | 0.540 | 0.071 | 7.61 | 0.884 | 0.105 | 8.43 | 0.611 |
| AUD symptoms | 0.075 | 0.709 | 0.102 | 6.92 | 0.143 | 0.035 | 4.11 | 0.852 | 0.100 | 8.50 | 0.168 |
| Correlated mediation | 0.130 | 0.261 | 0.114 | 2.30 | 0.590 | 0.070 | 8.38 | 0.851 | 0.100 | 8.50 | 0.693 |
| PTSD symptoms | - | - | - | - | 0.473 | 0.066 | 7.16 | - | - | - | 0.556 |
| AUD symptoms | - | - | - | - | 0.117 | 0.033 | 3.51 | - | - | - | 0.138 |
Abbreviations: AUD = Alcohol use disorder, PTE = potentially traumatic event, PTSD=Posttraumatic stress disorder, n.s.=non-significant. The following p-values correspond to the ratio column (Z-score) of the table: 1.96 (p=0.05); 2.58 (p=0.01); 3.29 (p=0.001).
4. Discussion
This is the first study in the literature to examine the relationships between trauma type, trauma-related psychopathology, and disturbed sleep in an under-studied, high-risk population. Thus, we extend the trauma and sleep literature to encompass a large undergraduate sample. There are two main results that warrant discussion. First, hierarchical regression analyses showed that interpersonal, but not accidental, PTE exposure was a significant predictor of disturbed sleep. Second, mediation analyses demonstrated that both PTSD and AUD symptoms were significant mediators of the relationship between interpersonal PTE exposure and sleep, both independently and jointly. However, the magnitude of PTSD symptoms’ indirect effect was much larger than that of AUD symptoms’ in all models.
4.1. Impact of PTE type
When combined with interpersonal PTE exposure, accidental PTE exposure was not a significant predictor of disturbed sleep. This suggests that when examining trauma types, interpersonal PTE exposure has a substantial impact on disturbed sleep in college students, above and beyond the effects of PTEs that are accidental in nature. Note that interpersonal and accidental PTEs were moderately correlated with one another (see Table 1). Note that the prevalence of accidental traumas, particularly natural disasters, was high in our sample, which could be due to natural disasters (i.e., earthquake, hurricane) that occurred in the area in the time period surrounding data collection (many students are local). These results are consistent with prior literature on trauma type and psychopathology, where interpersonal trauma has been shown to be a more potent predictor of internalizing disorders [12, 13]. However, this study is one of the first to date to extend this trauma type pattern of findings in the context of sleep outcomes. Our results are consistent with complimentary lines of evidence in that disturbed sleep and internalizing disorders are highly comorbid and related, in that sleep is not only a symptom of common disorders [24] but is also a predictor of future psychiatric outcomes following trauma exposure [e.g., 44]. Many studies have examined sleep following specific traumatic events (e.g., hurricanes, earthquakes, combat), but few have looked at multiple trauma types within the same sample [14]. A recent study that examined various traumatic events in an urban young adult sample found that interpersonal traumas were potent predictors of insomnia [14], which, taken with our results, shows that findings across trauma and sleep are robust.
4.2. Mediations
Since interpersonal PTE exposure was correlated with all outcome variables, we sought to determine if the relationship between interpersonal PTE exposure and sleep disturbances was accounted for by common psychiatric sequelae that were also associated with sleep and trauma in our sample. PTSD was a significant mediator, with a large indirect effect accounting for over half (61%) of the total effect of interpersonal PTE exposure on disturbed sleep. This is consistent with additional results from Hall Brown and colleagues [14], who found that the odds ratios for interpersonal traumas predicting endorsement of moderate to severe insomnia significantly decreased following the inclusion of PTSD and nocturnal fears into the model. We also found that AUD symptoms were a significant mediator of the relationship between interpersonal PTE exposure and sleep, although the magnitude of the indirect effect was not as high as for PTSD: AUD symptoms accounted for ~17% of the total relationship. Alcohol use negatively impacts sleep [36] and many individuals use alcohol to cope with both trauma and disturbed sleep [45].
Given that AUD and PTSD often co-occur and we see their moderate correlation in our sample, we analyzed these phenotypes simultaneously in a correlated mediation model. Results of this correlated mediation suggest that both PTSD and AUD symptoms have significant independent indirect effects on the relationship between interpersonal PTE exposure and sleep. The total indirect effect increased from what was seen in individual models, but the relationship was not additive (i.e., the new indirect effect was not the sum of each effect from individual mediations). This indicates that AUD symptoms may contribute uniquely to the trauma and sleep relationship, despite the smaller magnitude of the effect. This is particularly striking, given that the average age of onset for AUD diagnosis is 30 [46] and we have a young college sample. Based on these results, both AUD and PTSD symptoms should be considered when addressing post-trauma sleep disturbances in college students.
4.3. Clinical implications
The present study has several important clinical implications for the provision of both broad, population-based prevention efforts as well for crafting more targeted clinical interventions for at-risk students. First, our results demonstrating endorsement of disturbed sleep in this sample and its significant relation to trauma and mental health conditions (e.g., AUD, PTSD) underscore the importance of incorporating sleep screening into student health clinics and providing college students with basic sleep hygiene tips as well as psychoeducation about the relationship between sleep, mood, risk behaviors, and trauma exposure. Further, given the significant effect of interpersonal traumas on sleep (e.g., endorsing interpersonal PTE exposure is associated with greater sleep symptoms; shown here) that has also been demonstrated for other internalizing psychiatric disorders within our study sample as well as in previous research [12, 13], it may be beneficial to allocate additional resources to students who have experienced interpersonal trauma. This is especially relevant given the high rates of revictimization among college students [e.g., 47].
For students currently experiencing disturbed sleep symptoms, a more targeted intervention may be warranted. Cognitive Behavioral Therapy for Insomnia (CBT-I; a behavioral treatment that addresses the cognitive, physiological, and behavioral maintaining factors of insomnia) is the recommended first line of treatment for sleep issues [48] and has been demonstrated to be effective in college students [49], as well as in populations with co-morbid psychiatric and medical conditions [50]. CBT-I improves sleep-related symptoms in individuals with PTSD and may also have a positive influence on other PTSD symptoms [51]. While CBT-I appears to be effective for individuals with comorbid AUDs [52], there are few studies examining its effects on alcohol symptoms. Further, sleep issues often linger in studies that treat PTSD symptoms or alcohol symptoms alone, without a more targeted sleep-intervention [45]. A recent study examining sleep symptoms following psychosocial treatment for co-morbid PTSD and substance use disorders (SUDs) did find improvement in insomnia, but residual sleep disturbances remained for many participants and there was evidence that improved sleep had a positive influence on PTSD, but not SUD, outcomes [53]. Thus, a more holistic treatment plan that incorporates the triad of related issues established in this paper (i.e., sleep issues, AUD symptoms, and PTSD symptoms) may more effectively address these concerns. However, further research is needed, as to date, studies exploring such an integrative treatment program are scarce and none have used college populations.
5. Limitations
Results should be interpreted in light of eight main limitations, many of which are inherent to the study design. First, the dataset includes only subjective, self-report measures and would have benefited from corroborative objective measures (e.g., actigraphy for sleep). Second, many of the study measures are brief versions or abridged from their original form, including those for key variables such as PTSD and sleep difficulties, which may limit our ability to draw diagnostic conclusions from available data. Specifically for sleep, we do not have data on sleep timing, which would be relevant given associations between sleep timing and alcohol [28, 35]. Third, reliability for the sleep items was on the lower end (0.63), likely due to the use of an abbreviated scale. Fourth, college students are not yet in the highest risk age range for AUD onset [46], so there may be a floor effect. Fifth, freshmen college students may not be reflective of college students across the years, as some behaviors change across college (e.g., sleep quality/duration is worst freshmen year), while others (e.g., alcohol use) may remain relatively stable [1, 54]. Sixth, college students are a selected population, which may limit the generalizability of findings. However, Spit for Science is socioeconomically and racially diverse, with a higher survey response rate than most studies [38] and college is an important time period to study. Seventh, the temporal assessment of psychiatric phenotypes is also problematic, as we only have information on timing for sleep disturbances – PTSD and AUD were lifetime measures (note that pre-college traumatic events were assessed). This, combined with the cross-sectional study design, makes it impossible to ascertain directionality within our models. Finally, we do not have data on actual clinical diagnoses or treatment outcomes within this sample, which limits our conclusions to symptoms of these disorders, as opposed to clinical definitions, and does not permit us to examine how these relationships may be affected by treatment.
6. Conclusions and future directions
Our results provide evidence that interpersonal PTE exposure is a potent, enduring predictor of disturbed sleep in a large college population, and that this relationship between interpersonal PTE exposure and sleep may be partially explained by PTSD and AUD symptoms. As many epidemiologic studies of insomnia in college students do not specifically examine traumatic events [15], these results are novel and may have important clinical and treatment implications for an at-risk population. Important future research directions include examining the influence of new-onset interpersonal traumas, as well as revictimization, on these relationships, investigating how other predictors of poor sleep in college students may interact with trauma to influence sleep, and using longitudinal data to better understand temporal relationships. Further, examination of other factors that could be contributing to these relationships (e.g., personality) is also warranted.
Highlights.
Interpersonal, but not accidental, trauma significantly predicted disturbed sleep.
PTSD symptoms mediated the relationship between interpersonal trauma and sleep.
Alcohol use disorder symptoms had a significant, but lesser, mediation effect.
When analyzed together, both disorders continued to have indirect effects on sleep.
Addressing PTSD and AUD symptoms in college students may help improve sleep.
Acknowledgments
Spit for Science: The VCU Student Survey has been supported by Virginia Commonwealth University, P20 AA107828, R37AA011408, K02AA018755, and P50 AA022537 from the National Institute on Alcohol Abuse and Alcoholism, and UL1RR031990 from the National Center for Research Resources and National Institutes of Health Roadmap for Medical Research. Mackenzie Lind is supported by T32 MH020030. Dr. Amstadter’s time is partially funded by K02 AA023239. We would like to thank the VCU students for making this study a success, as well as the many VCU faculty, students, and staff who contributed to the design and implementation of the project.
Footnotes
Abbreviations: AUD (alcohol use disorder); PTE (potentially traumatic event); PTSD (posttraumatic stress disorder)
Conflicts of interest: None
References
- 1.Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolesc Health. 2010;46:124–32. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 2.Krishnan V, Collop NA. Gender differences in sleep disorders. Curr Opin Pulm Med. 2006;12:383–9. doi: 10.1097/01.mcp.0000245705.69440.6a. [DOI] [PubMed] [Google Scholar]
- 3.American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2015. Hanover, MD: American College Health Association; 2015. [Google Scholar]
- 4.Hershner SD, Chervin RD. Causes and consequences of sleepiness among college students. Nat Sci Sleep. 2014;6:73–84. doi: 10.2147/NSS.S62907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McLay RN, Klam WP, Volkert SL. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from military deployments. Mil Med. 2010;175:759–62. doi: 10.7205/milmed-d-10-00193. [DOI] [PubMed] [Google Scholar]
- 6.Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and PTSD: a critical review of the empirical literature. J Anxiety Disord. 2010;24:1–15. doi: 10.1016/j.janxdis.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steine IM, Harvey AG, Krystal JH, Milde AM, Gronli J, Bjorvatn B, et al. Sleep disturbances in sexual abuse victims: a systematic review. Sleep Medicine Reviews. 2012;16:15–25. doi: 10.1016/j.smrv.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Breslau N. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma, Violence, & Abuse. 2009;10:198–210. doi: 10.1177/1524838009334448. [DOI] [PubMed] [Google Scholar]
- 9.Humphrey JA, White JW. Women’s vulnerability to sexual assault from adolescence to young adulthood. J Adolesc Health. 2000;27:419–24. doi: 10.1016/s1054-139x(00)00168-3. [DOI] [PubMed] [Google Scholar]
- 10.Bernat JA, Ronfeldt HM, Calhoun KS, Arias I. Prevalence of traumatic events and peritraumatic predictors of posttraumatic stress symptoms in a nonclinical sample of college students. J Trauma Stress. 1998;11:645–64. doi: 10.1023/A:1024485130934. [DOI] [PubMed] [Google Scholar]
- 11.Scarpa A, Fikretoglu D, Bowser F, Hurley JD, Pappert CA, Romero N, et al. Community Violence Exposure in University Students: A Replication and Extension. J Interpers Violence. 2002;17:253–72. doi: 10.1177/0886260502017003002. [DOI] [Google Scholar]
- 12.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord. 2011;25:456–65. doi: 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amstadter AB, Aggen SH, Knudsen GP, Reichborn-Kjennerud T, Kendler KS. Potentially traumatic event exposure, posttraumatic stress disorder, and Axis I and II comorbidity in a population-based study of Norwegian young adults. Soc Psychiatry Psychiatr Epidemiol. 2013;48:215–23. doi: 10.1007/s00127-012-0537-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hall Brown TS, Akeeb A, Mellman TA. The role of trauma type in the risk for insomnia. J Clin Sleep Med. 2015;11:735–9. doi: 10.5664/jcsm.4846. http://dx.doi.org/10.5664/jcsm.4846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor DJ, Bramoweth AD, Grieser EA, Tatum JI, Roane BM. Epidemiology of insomnia in college students: relationship with mental health, quality of life, and substance use difficulties. Behav Ther. 2013;44:339–48. doi: 10.1016/j.beth.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 17.Vrana S, Lauterbach D. Prevalence of traumatic events and post-traumatic psychological symptoms in a nonclinical sample of college students. J Trauma Stress. 1994;7:289–302. doi: 10.1007/BF02102949. doi. [DOI] [PubMed] [Google Scholar]
- 18.Marx BP, Sloan DM. The effects of trauma history, gender, and race on alcohol use and posttraumatic stress symptoms in a college student sample. Addict Behav. 2003;28:1631–47. doi: 10.1016/j.addbeh.2003.08.039. [DOI] [PubMed] [Google Scholar]
- 19.Smyth JM, Hockemeyer JR, Heron KE, Wonderlich SA, Pennebaker JW. Prevalence, type, disclosure, and severity of adverse life events in college students. J Am Coll Health. 2008;57:69–76. doi: 10.3200/JACH.57.1.69-76. [DOI] [PubMed] [Google Scholar]
- 20.Twamley EW, Hami S, Stein MB. Neuropsychological function in college students with and without posttraumatic stress disorder. Psychiatry Res. 2004;126:265–74. doi: 10.1016/j.psychres.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 21.Germain A. Sleep disturbances as the hallmark of PTSD: where are we now? Am J Psychiatry. 2013;170:372–82. doi: 10.1176/appi.ajp.2012.12040432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Liempt S. Sleep disturbances and PTSD: a perpetual circle? Eur J Psychotraumatol. 2012:3. doi: 10.3402/ejpt.v3i0.19142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ross RJ, Ball WA, Sullivan KA, Caroff SN. Sleep disturbance as the hallmark of posttraumatic stress disorder. Am J Psychiatry. 1989;146:697–707. doi: 10.1176/ajp.146.6.697. [DOI] [PubMed] [Google Scholar]
- 24.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- 25.Germain A, Shear MK, Hall M, Buysse DJ. Effects of a brief behavioral treatment for PTSD-related sleep disturbances: a pilot study. Behav Res Ther. 2007;45:627–32. doi: 10.1016/j.brat.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 26.Berenz EC, Cho SB, Overstreet C, Kendler K, Amstadter AB, Dick DM. Longitudinal investigation of interpersonal trauma exposure and alcohol use trajectories. Addict Behav. 2016;53:67–73. doi: 10.1016/j.addbeh.2015.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cho SB, Llaneza DC, Adkins AE, Cooke M, Kendler KS, Clark SL, et al. Patterns of Substance Use Across the First Year of College and Associated Risk Factors. Front Psychiatry. 2015;6:152. doi: 10.3389/fpsyt.2015.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Van Reen E, Roane BM, Barker DH, McGeary JE, Borsari B, Carskadon MA. Current Alcohol Use is Associated with Sleep Patterns in First-Year College Students. Sleep. 2016;39:1321–6. doi: 10.5665/sleep.5862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeMartini KS, Fucito LM. Variations in sleep characteristics and sleep-related impairment in at-risk college drinkers: a latent profile analysis. Health Psychol. 2014;33:1164–73. doi: 10.1037/hea0000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National Institute on Alcohol Abuse and Alcoholism. [Accessed 2 November 2016];College Fact Sheet. 2015 Dec; Available at: https://pubs.niaaa.nih.gov/publications/CollegeFactSheet/CollegeFactSheet.pdf.
- 31.National Institute on Alcohol Abuse and Alcoholism. [Accessed 10 January 2017];Drinking Levels Defined. Available at: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking.
- 32.Chassin L, Pitts SC, Prost J. Binge drinking trajectories from adolescence to emerging adulthood in a high-risk sample: predictors and substance abuse outcomes. J Consult Clin Psychol. 2002;70:67–78. [PubMed] [Google Scholar]
- 33.Roehrs TA, Roth T. Sleep, sleepiness, sleep disorders and alcohol use and abuse. Sleep Med Rev. 2001;5:287–97. doi: 10.1053/smrv.2001.0162. [DOI] [PubMed] [Google Scholar]
- 34.Hasler BP, Martin CS, Wood DS, Rosario B, Clark DB. A longitudinal study of insomnia and other sleep complaints in adolescents with and without alcohol use disorders. Alcohol Clin Exp Res. 2014;38:2225–33. doi: 10.1111/acer.12474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Singleton RA, Jr, Wolfson AR. Alcohol consumption, sleep, and academic performance among college students. J Stud Alcohol Drugs. 2009;70:355–63. doi: 10.15288/jsad.2009.70.355. [DOI] [PubMed] [Google Scholar]
- 36.Roehrs TA, Roth T. Sleep Disturbance in Substance Use Disorders. Psychiatr Clin North Am. 2015;38:793–803. doi: 10.1016/j.psc.2015.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dick DM, Nasim A, Edwards AC, Salvatore JE, Cho SB, Adkins A, et al. Spit for Science: launching a longitudinal study of genetic and environmental influences on substance use and emotional health at a large US university. Front Genet. 2014;5:47. doi: 10.3389/fgene.2014.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gray M, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the Life Events Checklist. Assessment. 2004;11:330–41. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- 40.Prins A, Ouimette P, Kimerling R, Cameron RS, Hugleshofer D, Shaw-Hegwar J. The Primary Care PTSD Screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry. 2003;9:9–14. [Google Scholar]
- 41.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 42.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–31. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 44.Pigeon WR, Campbell CE, Possemato K, Ouimette P. Longitudinal relationships of insomnia, nightmares, and PTSD severity in recent combat veterans. J Psychosom Res. 2013;75:546–50. doi: 10.1016/j.jpsychores.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 45.Vandrey R, Babson KA, Herrmann ES, Bonn-Miller MO. Interactions between disordered sleep, post-traumatic stress disorder, and substance use disorders. Int Rev Psychiatry. 2014;26:237–47. doi: 10.3109/09540261.2014.901300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 47.Messman-Moore TL, Long PJ. Child sexual abuse and revictimization in the form of adult sexual abuse, adult physical abuse, and adult psychological maltreatment. J Interpers Violence. 2000;15:489–502. [Google Scholar]
- 48.Kaplan KA, Harvey AG. Treatment of sleep disturbance. In: Barlow DH, editor. Clinical handbook of psychological disorders: A step-by-step treatment manual. 5. New York, NY: The Guilford Press; 2014. pp. 640–99. [Google Scholar]
- 49.Taylor DJ, Zimmerman MR, Gardner CE, Williams JM, Grieser EA, Tatum JI, et al. A pilot randomized controlled trial of the effects of cognitive-behavioral therapy for insomnia on sleep and daytime functioning in college students. Behav Ther. 2014;45:376–89. doi: 10.1016/j.beth.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 50.Wu JQ, Appleman ER, Salazar RD, Ong JC. Cognitive Behavioral Therapy for Insomnia Comorbid With Psychiatric and Medical Conditions: A Meta-analysis. JAMA Intern Med. 2015;175:1461–72. doi: 10.1001/jamainternmed.2015.3006. [DOI] [PubMed] [Google Scholar]
- 51.Ho FY, Chan CS, Tang KN. Cognitive-behavioral therapy for sleep disturbances in treating posttraumatic stress disorder symptoms: A meta-analysis of randomized controlled trials. Clin Psychol Rev. 2016;43:90–102. doi: 10.1016/j.cpr.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 52.Brooks AT, Wallen GR. Sleep Disturbances in Individuals with Alcohol-Related Disorders: A Review of Cognitive-Behavioral Therapy for Insomnia (CBT-I) and Associated Non-Pharmacological Therapies. Subst Abuse. 2014;8:55–62. doi: 10.4137/SART.S18446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McHugh RK, Hu MC, Campbell AN, Hilario EY, Weiss RD, Hien DA. Changes in sleep disruption in the treatment of co-occurring posttraumatic stress disorder and substance use disorders. J Trauma Stress. 2014;27:82–9. doi: 10.1002/jts.21878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schulenberg JE, Maggs JL. A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. J Stud Alcohol Suppl. 2002:54–70. doi: 10.15288/jsas.2002.s14.54. [DOI] [PubMed] [Google Scholar]