Abstract
Objective
The aim of this study was to evaluate our long-term results with the Zweymüller hochgezogen and SL total hip arthroplasty system. This is the first study to provide a 30-year follow-up.
Methods
We reviewed 186 Alloclassic stem systems (Zweymüller hochgezogen (112) and SL (74), implanted in 179 patients from 1986 to 1987.
Two different types of cementless acetabular components were used.
143 patients had died over the last 30 years, so thirty out of 36 patients being still alive, with a mean follow-up of 29,48 years (SD 0,51), were contacted by telephone and evaluated radiologically and clinically. Our loss-to-follow up was 16,7%. The mean age at follow-up was 83,57 years (72,4–95,2; SD 6,77).
Results
If the endpoint is defined as the removal of the stem for aseptic loosening (3 cases), the overall survival rate is 98,38%. If the endpoint is revision for any reason (27 cases), the survival rate is 85,48%. Eleven patients needed an exchange of head and liner. The mean time from implantation until change of head and liner was 21,44 years (SD 5,92).
Most of the radiolucent lines and osteolytic zones were found in the proximal Gruen-zones 1 and 7 (69,7 and 21,2%).
Conclusion
After 30 years of monitoring we can state that the evaluated system is very reliable in primary and secondary THA.
Keywords: Total hip arthroplasty, Long term follow up, SL, Alloclassic, Stem
1. Background
Numerous studies deal with short and midterm results of the cementless implanted Alloclassic Zweymüller total hip arthroplasty stem system, which was implanted for the first time on the 5th of October in 1979, and the direct successor, the SL-stem.
Some studies describe long-term results up to 20 years.
Since the first publication of the results of our cohort,1 14 years have passed and we have been able to obtain reliable long-term results.
Up to now, there is no publication dealing with results after 30 years and the events causing a revision of the prosthesis during this long timelapse. The aim was to evaluate the results after 30 years.
2. Patients and methods
From 1986 on, our institution has been implanting the Alloclassic Zweymüller and the SL-total hip arthroplasty system.
All of the 186 Alloclassic stem systems (Zweymüller hochgezogen (112) and SL (74); AlloPro/Sulzer Medica, Winterthur, Switzerland and Centerpulse, Winterthur, Switzerland), implanted in 179 patients from 1986 to 1987, were included in this study.
The cups used were cementless too and concisted of 181 (97,3%) Alloclassic CSF (AlloPro/Sulzer Medica, Winterthur, Switzerland and Centerpulse, Winterthur, Switzerland) and 5 (2,7%) Endler (AlloPro/Sulzer Medica, Winterthur, Switzerland).
The group consisted of 102 women and 77 men.
The mean age at surgery was 62,76 years (33,2–83,1; standard-deviation 9,34).
The indication (Table 1) for total hip arthroplasty was pimary osteoarthritis in 139 cases (74,73%) and secondary osteoarthritis in 32 cases (17,2%. Others were revision surgeries in 15 cases (8,07%).
Table 1.
Indications for implantation of the cementless Alloclassic THA-system.
| Indication | Absolute number | Percentage |
|---|---|---|
| Primary osteoarthritis | 139 | 74,73% |
| Necrosis of the femoral head | 19 | 10,21% |
| Dysplasia | 8 | 4,30% |
| Trauma | 4 | 2,15% |
| Perthes | 1 | 0,54% |
| St.p. Girdlestone procedure | 5 | 2,69% |
| St.p. loosening of stem | 10 | 5,38% |
Over the last 30 years, 143 patients had died. Out of 36 patients being still alive, 30 could be contacted by telephone. Due to bad general medical condition and distant relocation in many cases, we did not expect to get the chance to clinically evaluate a majority of the shrinking cohort. Those patients and their relevants were interviewed by telephone if the prostheses were still in situ and if there occurred any problems over the past years, concerning the prostheses. In nine cases we were able to perform a full clinical and radiological examination.
Our total loss-to-follow up was 16,7%. The mean age at follow-up was 83,57 years (72,4–95,2; SD 6,77).
We assessed the survival rate of the implant, the adverse events caused by the implant over the last 30 years, the occurrence of radiolucent lines and osteolytic zones in the recent weight bearing x-rays according to the classification of Gruen on the a-p view and the patients’ satisfaction with the result after 30 years.
Survival curves were calculated for all implanted stems for aseptic loosening as well as revision for any reason.
3. Results
3.1. Survival rate
If the endpoint ist the removal of the stem for aseptic loosening (3 cases), the overall survival rate is 98,38% (Fig. 1). If the endpoint is revision for any reason (27 cases), the survival rate is 85,48% (Fig. 2). Eleven patients needed an exchange of head and liner, one of them was operated twice on one hip. The mean time from implantation until change of head and liner was 21,44 years (SD 5,92). Those patients, who died over the last 30 years, have lived with the arthroplasty system for an average of 18,38 years (2,02–30,34; SD 6,9).
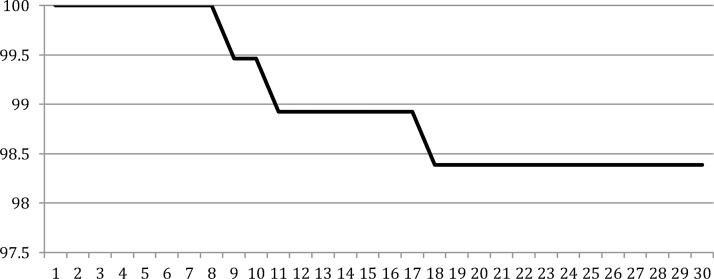
Fig. 1.
Survival curve for the endpoint‚ aseptic loosening of the stem’.
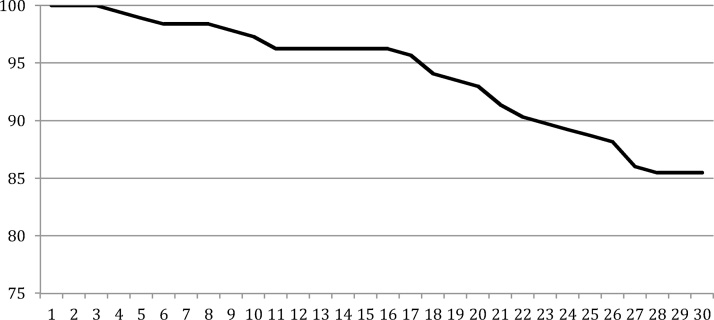
Fig. 2.
Survival curve for the endpoint‚ revision for any reason’.
3.2. Radiological
Most of the radiolucent lines and osteolytic zones (Fig. 3) were found in the proximal Gruen-zones 1 and 7 (69,7 and 21,2%). None of the implanted stems was considered to be at risk.
Fig. 3.
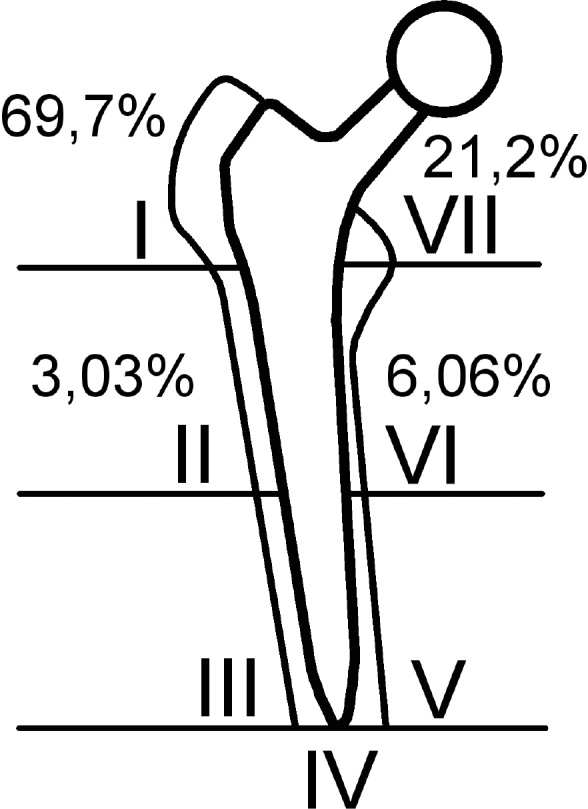
Osteolytic zones and radiolucent lines according to the zones of Gruen; n = 33.
3.3. Clinical
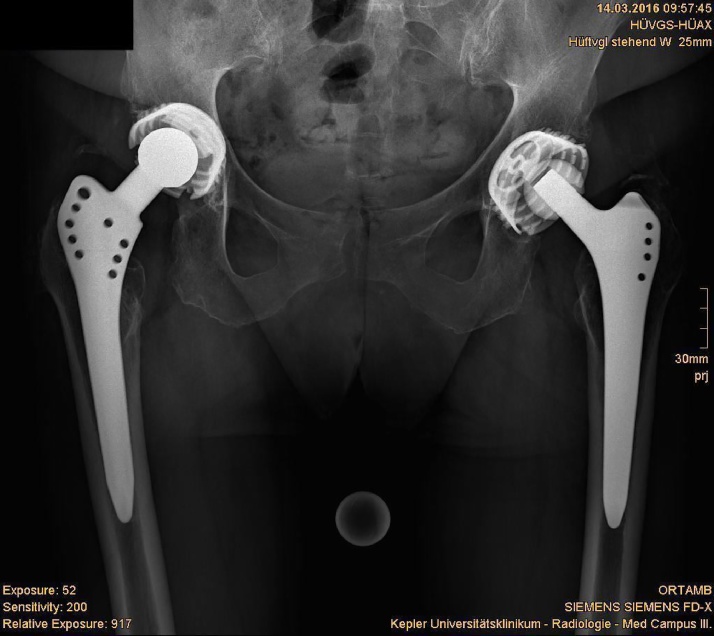
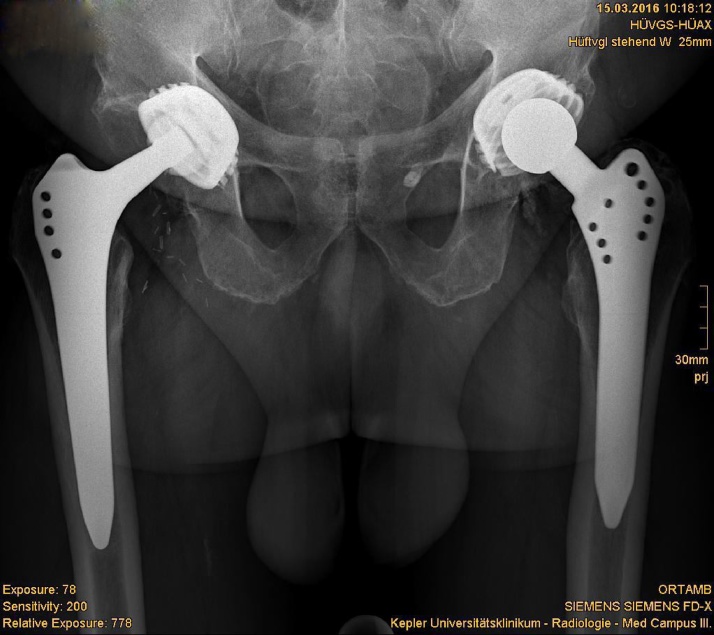
Overall satisfaction of our patients with the implanted Alloclassic stem system was very good (Fig. 4, Fig. 5). None of the 30 patients described pain. Only one patient was not satisfied due to leg length inequality caused by high congenital hip dysplasia of the contralateral side.
Fig. 4.
Radiograph showing excellent results after 30 years in a highly active 84-year old female (r).
Fig. 5.
Radiograph showing excellent results after 30 years in a highly active 84-year old female (r).
3.4. Adverse events resulting in further surgery
We had three cases of aseptic loosening as well as three cases of septic loosening. Aseptic loosening of the acetabular component was found three times, whereof two were seen in cases of a loose stem and one as a result of a totally worn-out liner. Five patients had to be revised because of a periprosthetic fracture. Major calcification occurred in three cases (Table 2).
Table 2.
Reasons for revision surgery.
| Type of failure | Absolute number | Relative risk |
|---|---|---|
| Asepic loosening of stem | 3 | 1,61% |
| Septic loosening | 3 | 1,61% |
| Periprosthetic fracture | 5 | 2,69% |
| Major calcification | 3 | 1,61% |
| Implant fracture | 1 | 0,54% |
| Aseptic loosening of cup | 2, all of them with loose stem | 1,07% |
| Totally worn-out liner | 1 | 0,54% |
| Wear | 11 | 5,91% |
| Overall cases needing revision surgery | 27 | 14,51% |
We had one case of implant-fracture (Fig. 6), which lead to revision-surgery of the femoral component. One totally worn-out liner leaded to revision surgery of the acetabular compunent (Fig. 7).
Fig. 6.
Radigraph showing implant fracture after 20 years.
Fig. 7.
Radiograph showing totally worn-out liner after 25 years.
One case of periprosthetic joint infection and one periprosthetic fracture resulted in a Girdlestone-procedure.
In three patients a fissure of the proximal femur was seen intraoperatively, so no second surgical procedure was needed.
4. Discussion
Our evaluation of the cementless implanted Alloclassic-stem-system ist the first ultra-longterm-study with a mean follow up of 29,48 years. During this timespan, a broad variety of complications occurred in our cohort. Nevertheless, for a big majority of 85,48%, the implantation of the evaluated THA-system was the last surgery needed involving the replaced joint.
14,52% needed revision surgery for any cause. It has to be considered, that in those cases, which needed an exchange of head and liner, a regular PE-liner had been used in the initial surgery. Since the introduction of ultra-high cross-linked UHMWPE in 1998, revision surgery was performed under usage of this material, which promises less wear and as a result, a far smaller revision rate due to wear. 2,3,4
Having good data for the cost-effectiveness of THA, this effect gets stronger when the revision rate decreases.5,6
The fear of creating a life-long patient when performing a THA in a younger individual, does not seem to be justified, regarding the small wear rates of modern materials.
As expected and shown in previous studies of the Alloclassic-stem, most of the radiolucent lines and osteolytic zones werde found proximally, bone apposition more distally.7, 8, 9 Shown by the authors in a previous study, there may be a positive effect on the reduction of osteolytic zones caused by wear when changing head and liner.10 Nevertheless none of the evaluated stems was at risk.
Our findings are comparable to previous results shown by Pospischill and Knahr in 2005 with a survival rate of 100% for aseptic loosening for the stem after 15 years.11
Pieringer et al. showed in 2006 100% survival rate (aseptic loosening) for the stem after 157 months.12 Busch et al. showed in 2012 89% survival rate (any reason) for cup and stem after 17 years.13 Kolb et al. reported a survival rate of 96% percent for the stem after 20 years.14 With 4337 evaluated stems, the czech register published a survival rate of 99,88% after 1–11 years.15
It has to be stated, that the criteria, revision for any reason’ increases with the years and usage because of progressive wear and the need for replacing head and liner.16
Knowing the excellent results for aseptic loosening of the discussed system, we have to note that the growing popularity of short stemmed types needs further benchmarks to prove superiority. Criteria such as bone loss in revision surgery and soft tissue trauma with the known resulting problems are arguments to pursue the development and evaluation of bone sparing, and more anatomically shaped arthroplasty systems.17, 18, 19
Our evaluation is limited by the small number of patients being alive after 30 years. Furthermore, most of the surviving patients are in a bad general medical condition or have moved far away from our institution, which leads to a very small number of clinical evaluations. Nevertheless, our primary aim was not the collection of clinical scores, but the survival rate of the implant and the resulting complications during a 30-year-timespan. This objective was achieved satisfactorily.
The evaluated system is very reliable in primary and secondary THA, as shown in previous studies as well as in this one. In our institution, it is the basic implant and first one for younger colleagues to get in contact with. It is our backup-system in cases of failure of short-stemmed total hip arthroplasty systems.
Conflict of interest
All authors declare that they have no conflicts of interest concerning this article.
Contributor Information
Lorenz Pisecky, Email: lorenz.pisecky@kepleruniklinikum.at.
Günter Hipmair, Email: guenter.hipmair@kepleruniklinikum.at.
Bernhard Schauer, Email: bernhard.schauer@kepleruniklinikum.at.
Nikolaus Böhler, Email: nikolaus.boehler@kepleruniklinikum.at.
References
- 1.Pieringer H., Auersperg V., Griessler W., Böhler N. Long-term results with the cementless Alloclassic brand hip arthroplasty system. J Arthroplasty. 2003;18(April (3)):321–328. doi: 10.1054/arth.2003.50045. [DOI] [PubMed] [Google Scholar]
- 2.Amstutz H.C., Takamura K.M., Ebramzadeh E., Le Duff M.J. Highly cross-linked polyethylene in hip resurfacing arthroplasty: long-term follow-up. Hip Int. 2015;25(January–Feburary (1)):39–43. doi: 10.5301/hipint.5000190. [DOI] [PubMed] [Google Scholar]
- 3.Nebergall A.K., Greene M.E., Rubash H., Malchau H., Troelsen A., Rolfson O. Thirteen-year evaluation of highly cross-linked polyethylene articulating with either 28-mm or 36-mm femoral heads using radiostereometric analysis and computerized tomography. J Arthroplasty. 2016;31(September Suppl. (9)):269–276. doi: 10.1016/j.arth.2016.02.076. [DOI] [PubMed] [Google Scholar]
- 4.Glyn-Jones S., Thomas G.E., Garfjeld-Roberts P. The John Charnley Award: highly crosslinked polyethylene in total hip arthroplasty decreases long-term wear: a double-blind randomized trial. Clin Orthop Relat Res. 2015;473(Feburary (2)):432–438. doi: 10.1007/s11999-014-3735-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elmallah R.K., Chughtai M., Khlopas A. Determining cost-effectiveness of total hip and knee arthroplasty using the short form-6D utility measure. J Arthroplasty. 2016;(August) doi: 10.1016/j.arth.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 6.Koenig L., Zhang Q., Austin M.S. Estimating the societal benefits of THA after accounting for work status and productivity: a markov model approach. Clin Orthop Relat Res. 2016;(October) doi: 10.1007/s11999-016-5084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pieringer H., Auersperg V., Griessler W., Böhler N. Long-term results with the cementless Alloclassic brand hip arthroplasty system. J Arthroplasty. 2003;18(April (3)):321–328. doi: 10.1054/arth.2003.50045. [DOI] [PubMed] [Google Scholar]
- 8.Gruen T.A., McNeice G.M., Amstutz H.C. Modes of failure of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;(141):17–27. [PubMed] [Google Scholar]
- 9.Wick M., Lester D.K. Radiological changes in second- and third-generation Zweymüller stems. J Bone Joint Surg Br. 2004;86(November (8)):1108–1114. doi: 10.1302/0301-620x.86b8.14732. [DOI] [PubMed] [Google Scholar]
- 10.Pisecky L., Hipmair G., Schauer B., Böhler N. ‘Osteolysis in THA after head and inlay revision surgery’. J Orthop. 2017;14(October (1)):192–194. doi: 10.1016/j.jor.2016.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pospischill M., Knahr K. Cementless total hip arthroplasty using a threaded cup and a rectangular tapered stem. Follow-up for ten to 17 years. J Bone Joint Surg Br. 2005;87(September (9)):1210–1215. doi: 10.1302/0301-620X.87B9.16107. [DOI] [PubMed] [Google Scholar]
- 12.Pieringer H., Auersperg V., Böhler N. Long-term results of the cementless ALLOCLASSIC hip arthroplasty system using a 28-mm ceramic head: with a retrospective comparison to a 32-mm head. J Arthroplasty. 2006;21(October (7)):967–974. doi: 10.1016/j.arth.2005.08.027. [DOI] [PubMed] [Google Scholar]
- 13.Busch V.J., Pouw M.H., Laumen A.M., van Susante J.L., Vervest A.M. Long-term outcome of 73 Zweymüller total hip prostheses with a screw cup in patients under 50 years of age. Hip Int. 2012;22(03):292–295. doi: 10.5301/HIP.2012.9239. [DOI] [PubMed] [Google Scholar]
- 14.Kolb A., Grübl A., Schneckener C.D. Cementless total hip arthroplasty with the rectangular titanium Zweymüller stem: a concise follow-up, at a minimum of twenty years, of previous reports. J Bone Joint Surg Am. 2012;94(September (18)):1681–1684. doi: 10.2106/JBJS.K.01574. [DOI] [PubMed] [Google Scholar]
- 15.Acta Chir orthop Traum čech. 2014;81(Suppl) [Google Scholar]
- 16.Schmalzried T.P., Shepherd E.F., Dorey F.J. The John Charnley Award. Wear is a function of use, not time. Clin Orthop Relat Res. 2008;(December (381)):36–46. doi: 10.1097/00003086-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Ries C., Schopf W., Dietrich F. Anatomic reconstruction of hip joint biomechanics: conventional vs. short-stem prosthesis. Z Orthop Unfall. 2015;153(Feburary (1)):46–50. doi: 10.1055/s-0034-1396230. [DOI] [PubMed] [Google Scholar]
- 18.Choi Y.W., Kim S.G. The short-term clinical outcome of total hip arthroplasty using short metaphyseal loading femoral stem. Hip Pelvis. 2016;28(June):82–89. doi: 10.5371/hp.2016.28.2.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rajakulendran K. Field RE. Neck-preserving femoral stems. HSS J. 2012;8(October (3)):295–303. doi: 10.1007/s11420-012-9302-z. [DOI] [PMC free article] [PubMed] [Google Scholar]