Abstract
A 47-year-old man with HIV infection presented 10 years after initial secondary syphilis diagnosis and treatment for routine follow-up. His HIV was well controlled on antiretroviral therapy. Rapid plasma reagin was 1:1, and TP-PA was reactive. Physical examination revealed a wide pulse pressure, a systolic murmur, and an early diastolic decrescendo murmur. Echocardiogram revealed moderate to severe aortic regurgitation, and subsequent computed tomography angiogram showed a 6.8-cm fusiform aneurysm of the proximal ascending aorta. Aortic valve and ascending hemiarch replacement were performed. Pathology showed adventitial inflammation with plasma cells, gumma-like amorphous areas surrounded by histiocytes, and giant cells with calcified plaques. Cardiovascular syphilis, while rare, remains a relevant cause of aortic aneurysm, even in previously treated patients. The physical exam can be critical in identifying this potentially fatal complication.
Keywords: aortic aneurysm, aortic regurgitation, cardiovascular syphilis, HIV
CASE
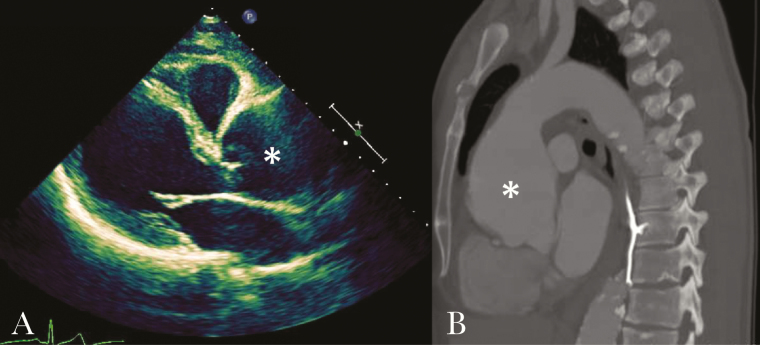
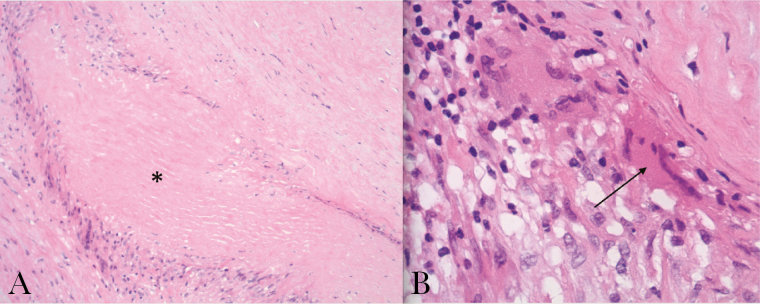
A 47-year old male with well-controlled HIV on antiretroviral therapy (CD4 498 cells/mm3, viral load undetectable) presented for a routine clinic appointment in 2015 without complaints. Ten years prior, he presented with a diffuse rash, had a rapid plasma reagin (RPR) titer of 1:512, and was diagnosed with secondary syphilis. After treatment with 2.4 million units of benzathine penicillin, his RPR decreased appropriately to 1:8 at six months post-treatment, and remained at low titer thereafter. There was no repeat infection, and his most recent RPR titer was 1:1 with a reactive Treponema pallidum particle agglutination test. He had a lumbar puncture in 2009 with normal CSF cell count, protein, and negative venereal disease research laboratory test (VDRL). He had no personal or family history of hypertension, dyslipidemia, heart disease, or autoimmune disease. Physical examination revealed a wide pulse pressure (blood pressure 132/53), an early diastolic decrescendo murmur at the left lower sternal border, and a systolic murmur at the right upper sternal border. Neurologic, musculoskeletal, and skin exam were normal, and there were no abdominal bruits. An electrocardiogram identified no abnormalities. An echocardiogram found moderate to severe aortic regurgitation. Computed tomography angiogram revealed a 6.8-cm fusiform aneurysm of the proximal ascending aorta [Figure 1], and coronary angiography found a lack of coronary artery disease. Surgery was performed with placement of a bioprosthetic aortic valve and ascending hemiarch replacement with graft; no significant atherosclerosis was noted intraoperatively. Bacterial, fungal, and AFB stains and cultures were negative. Histopathology examination was notable for the presence of adventitial inflammation with plasma cells, gumma-like amorphous areas surrounded by histiocytes, and giant cells with calcified plaques [Figure 2]. Treponemal polymerase chain reaction and immunohistochemistry on the tissue were negative. The patient recovered fully.
Figure 1.
(A) Still image of an echocardiogram showing severe aortic root dilatation (asterisk). (B) Computerized tomography angiogram demonstrating fusiform aneurysm (asterisk) of the proximal ascending aorta with diameter up to 6.8 cm.
Figure 2.
(A) Hematoxylin and eosin stain of aortic tissue with gumma-like amorphous area (asterisk) surrounded by histiocytes and giant cells. (B) Higher magnification demonstrating giant cells (arrow).
DISCUSSION
Rates of primary, secondary, and late syphilis are rising in many parts of the United States, particularly in the South and among men who have sex with men [1]. However, cardiovascular manifestations are rarely reported. Historical studies of untreated syphilis suggest that cardiovascular syphilis occurrs in up to 70% of patients, and aortic aneurysm specifically in 8–45% of patients [2–4]. More recently, a single center resected 23 syphilitic aortic aneurysms from 2009 to 2014 [5]. In a series of 90 cases of syphilitic aortitis diagnosed at necropsy from 1966 to 1990, 13% had died from aortic rupture [4]. Given the increasing rate of syphilis, clinicians must remain aware of these potentially fatal sequelae.
It is challenging to make a definitive diagnosis of cardiovascular syphilis due to the long latency of years to decades from initial infection to development of clinical complications and the rare identification of organisms in tissue [6, 7]. A history of previous clinical infection or reactive treponemal tests is needed to support the diagnosis. Pertinent exam findings, such as the murmur of aortic regurgitation, may be helpful, particularly when the patient is asymptomatic, as in this case [8]. When associated with syphilitic aortitis, aortic regurgitation is due to dilation of the vessel, not pathological involvement of the aortic valve cusp and, as in our case, may be the only clinical clue to a diagnosis of cardiovascular syphilis [5]. Massive aortic root dilatation with thinning of the vessel wall is typically due to syphilis, and together with clinical evaluation helps to distinguish from differential diagnoses including giant cell or Takayasu arteritis and ankylosing spondylitis [9]. The history of syphilis, histopathology findings, and lack of evidence for these alternative diagnoses all support the diagnosis of cardiovascular syphilis in this patient.
Cardiovascular syphilis typically manifests as thoracic aortitis. Endarteritis obliterans of the vasa vasorum leads to disruption of the tunica media and, together with intimal fibrosis and calcification, leads to weakening of the vessel wall and subsequent dilation [6]. The thoracic aorta is primarily involved as the vascular and lymphatic supply does not extend to the abdominal portion, but abdominal aortic aneurysms attributed to syphilis have been documented. Histology demonstrates a lymphoplasmacytic infiltrate with occasional giant cells. Later lesions may include gummas with central necrosis and surrounding macrophages and plasma cells, as seen in this case [9].
Cardiovascular syphilis should be treated with penicillin 2.4 million units intramuscularly every 7 days for 3 doses [7]. The risk of dissection or rupture of thoracic aortic aneurysms is 4.4 times greater for aneurysms 6.0–6.9 cm than those 4.0–4.9 cm; surgical evaluation should be pursued for ascending aortic or aortic sinus diameter >5.5 cm or associated symptoms [10, 11]. In this case, given the low RPR and lack of evidence of active infection in the resected tissue, no further treatment was given.
CONCLUSION
Although cardiovascular syphilis is rare, clinicians must maintain awareness of this potentially fatal form of disease as syphilis cases are on the rise in many parts of the United States. Our case also highlights that cardiovascular syphilis must be considered even in patients with a history of previously treated syphilis and, importantly, that cardiovascular syphilis may be asymptomatic; thus, the physical exam remains an essential tool in diagnosing this complication.
Acknowledgements
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2015. Atlanta: US Department of Health and Human Services; 2016. [Google Scholar]
- 2. Gjestland T. The Oslo study of untreated syphilis; an epidemiologic investigation of the natural course of the syphilitic infection based upon a re-study of the Boeck-Bruusgaard material. Acta Derm Venereol Suppl (Stockh) 1955; 35:3–368; Annex I–LVI. [DOI] [PubMed] [Google Scholar]
- 3. Jackman JD Jr, Radolf JD. Cardiovascular syphilis. Am J Med 1989; 87:425–33. [DOI] [PubMed] [Google Scholar]
- 4. Roberts WC, Ko JM, Vowels TJ. Natural history of syphilitic aortitis. Am J Cardiol 2009; 104:1578–87. [DOI] [PubMed] [Google Scholar]
- 5. Roberts WC, Barbin CM, Weissenborn MR, et al. Syphilis as a cause of thoracic aortic aneurysm. Am J Cardiol 2015; 116:1298–303. [DOI] [PubMed] [Google Scholar]
- 6. Tomey MI, Murthy VL, Beckman JA. Giant syphilitic aortic aneurysm: a case report and review of the literature. Vasc Med 2011; 16:360–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hook EW., 3rd Syphilis. Lancet. 2016. [Google Scholar]
- 8. Elder A, Japp A, Verghese A. How valuable is physical examination of the cardiovascular system? BMJ 2016; 354:i3309. [DOI] [PubMed] [Google Scholar]
- 9. Silver MD, Gotlieb AI, Schoen FJ.. Cardiovascular Pathology. 3rd ed New York: Churchill Livingstone; 2001. [Google Scholar]
- 10. Hiratzka LF, Bakris GL, Beckman JA et al. ; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American College of Radiology; American Stroke Association; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society of Interventional Radiology; Society of Thoracic Surgeons; Society for Vascular Medicine 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. J Am Coll Cardiol 2010; 55:e27–e129. [DOI] [PubMed] [Google Scholar]
- 11. Coady MA, Rizzo JA, Hammond GL et al. Surgical intervention criteria for thoracic aortic aneurysms: a study of growth rates and complications. Ann Thorac Surg 1999; 67:1922–1926; discussion 1953–8. [DOI] [PubMed] [Google Scholar]