Abstract
Osteoporosis is a common condition with serious consequences because of fractures. Despite availability of treatments to reduce fracture risk, there is a large osteoporosis treatment gap that has reached crisis proportions. There are too few specialists to provide services for patients who need them. Bone Health Extension for Community Health Care Outcomes (TeleECHO) is a strategy using real-time ongoing videoconferencing technology to mentor health care professionals in rural and underserved communities to achieve an advanced level of knowledge for the care of patients with skeletal diseases. Over the first 21 months of weekly Bone Health TeleECHO programs, there were 263 registered health care professionals in the United States and several other countries, with 221 attending at least 1 online clinic and typically 35 to 40 attendees at each session at the end of the reported period. Assessment of self-confidence in 20 domains of osteoporosis care showed substantial improvement with the ECHO intervention (P = 0.005). Bone Health TeleECHO can contribute to mitigating the crisis in osteoporosis care by leveraging scarce resources, providing motivated practitioners with skills to provide better skeletal health care, closer to home, with greater convenience, and lower cost than referral to a specialty center. Bone Health TeleECHO can be replicated in any location worldwide to reach anyone with Internet access, allowing access in local time zones and languages. The ECHO model of learning can be applied to other aspects of bone care, including the education of fracture liaison service coordinators, residents and fellows, and physicians with an interest in rare bone diseases.
Keywords: ECHO Act, Project ECHO, osteoporosis, treatment gap, telehealth, telemedicine
Bone Health TeleECHO is a strategy to reduce the osteoporosis treatment gap through ongoing interactive sharing of knowledge using videoconferencing technology.
Osteoporosis is a major public health concern with serious consequences resulting from fractures. There are about 200 million individuals with this disease worldwide and 9 million osteoporotic fractures each year, accounting for one fracture every three seconds somewhere in the world [1]. The National Osteoporosis Foundation reports a lifetime risk of osteoporotic fracture for one of every two women and one of every four men in the United States [2]. Fractures may be followed by pain, disability, death, loss of independence, and high health care costs. Despite the availability of excellent diagnostic tools and medications proven to reduce fracture risk, most patients at high risk of fracture are not being treated. The osteoporosis treatment gap is large and appears to be getting worse; only 10% to 20% of women with a hip fracture being treated with a pharmacologic agent to reduce fracture risk [3, 4]. In this setting, there is alarming evidence that hip fracture rates in the United States are now higher than projected [5]. The lack of needed care for so many patients with osteoporosis has recently been labeled a crisis [6], leading to an international call to action to improve osteoporosis care [7]. The prevailing paradigm for managing patients with osteoporosis is failing. New approaches to preventing fractures and reducing the personal and economic burden of fractures are needed. One component of addressing the crisis is better education of health care professionals.
Bone Health Extension for Community Health Care Outcomes (TeleECHO) uses videoconferencing technology to expand health care workforce capacity, increase access to specialty level care, and reduce health disparities in rural and underserved communities for patients with osteoporosis. This is a progress report of the first 21 months of Bone Health TeleECHO.
1. Project ECHO
Project ECHO (http://echo.unm.edu/) links an expert specialist team (“hub”) with health care professionals (“spokes”) located anywhere. Ongoing real-time videoconferences provide interactive collaborative learning through discussion of deidentified patient cases presented by the learners, combined with brief didactic presentations by faculty experts. The ECHO model of learning and care management was developed at the University of New Mexico Health Sciences Center (UNM HSC) to address the treatment gap for chronic hepatitis C in rural New Mexico. In a proof-of-concept study, primary care providers in underserved areas supported by the ECHO intervention achieved treatment outcomes that were as good as specialists at the university clinic [8]. Project ECHO has since expanded to include more than 130 hubs in 23 countries for 65 diseases and conditions. There are now TeleECHO clinics devoted to opioid addiction, palliative care, behavioral health disorders, tuberculosis, HIV, reproductive care, endocrinology, rheumatology, and much more [9]. The ECHO model is not telemedicine, which typically consists of one physician treating one patient at a remote location, and is not a webinar, which is usually an online lecture with limited opportunity for interactive discussions.
The potential of the ECHO model to improve health care has been recognized in a rare accomplishment of bipartisan cooperation by the US Congress and Senate. The Expanding Capacity for Health Outcomes Act (ECHO Act) [10], signed by President Obama in December 2016, requires the Department of Health and Human Services to evaluate and report on technology-enabled collaborative learning and capacity building models to include recommendations to reduce barriers to adoption of such models.
2. Bone Health TeleECHO
Bone Health TeleECHO was developed through collaboration of UNM HSC with the Osteoporosis Foundation of New Mexico [11]. It aims to improve the care of osteoporosis and serve as a model for replication (development of other Bone Health TeleECHO programs) in other states and countries [12]. Bone Health TeleECHO comprises a multidisciplinary faculty team engaging learning partners in a weekly 75-minute videoconference. The team approach is based on the experience of ECHO clinics for other diseases and conditions, as adapted for skeletal heath. The Bone Health TeleECHO faculty team has included an endocrinologist, rheumatologist, orthopedist, internist, and psychiatrist. The clinic started as a 60-minute teleconference but was later expanded to 75 minutes to accommodate more discussion with a larger number of participants.
All TeleECHO case presentations are compliant with US Health Insurance Portability and Accountability regulations. Participants are encouraged to ask questions and make comments regarding any clinical issues that arise in the discussion. Each TeleECHO session also includes a short didactic presentation, typically lasting about 10 to 15 minutes. Learners may participate in as many TeleECHO sessions as possible for as long as desired. Funding for Bone Health TeleECHO support staff is provided by the ECHO Institute. Faculty members receive no direct compensation. No-cost continuing medical education credits are provided by UNM.
3. Materials and Methods
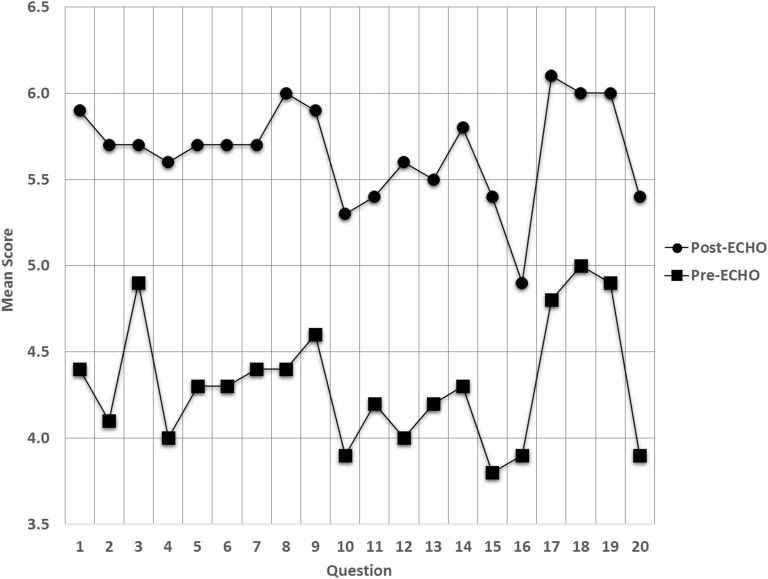
Demographic data for ECHO participants were obtained with online registration. ECHO staff collected attendance data with each weekly ECHO clinic. Outcomes were assessed by means of a blinded self-efficacy questionnaire administered online after 10 months of Bone Health TeleECHO clinics. This included collection of demographic information and asked for a rating on a scale of 0 to 7 (7 is highest) on self-confidence for 20 domains of osteoporosis care (Table 1) before and after the ECHO intervention. Effect size was classified according to the method of Cohen [13] and Sawilowsky [14] (0.2 = small, 0.5 = medium, 0.8 = large, 1.20 = very large effect size), commonly used in the behavioral sciences.
Table 1.
Bone Health TeleECHO Outcomes Data
| Domain No. | Domain of Knowledge | Pre-ECHO Mean | Post-ECHO Mean | Difference Mean | SD |
|---|---|---|---|---|---|
| 1 | Identify patients who would benefit from pharmacological treatment to reduce fracture risk | 4.40 | 5.90 | 1.50 | 0.97 |
| 2 | Evaluate patients for secondary causes of osteoporosis | 4.10 | 5.70 | 1.60 | 1.51 |
| 3 | Assess patients for risk of falling | 4.90 | 5.70 | 0.80 | 0.92 |
| 4 | Understand potential side effects of pharmacological medications used for treatment of osteoporosis | 4.00 | 5.60 | 1.60 | 1.26 |
| 5 | Educate my clinic staff about the management of osteoporosis patients | 4.30 | 5.70 | 1.40 | 1.26 |
| 6 | Understand the balance of benefits and risks with osteoporosis medications | 4.30 | 5.70 | 1.40 | 1.07 |
| 7 | Effectively communicate the balance of benefits and risks with osteoporosis medications | 4.40 | 5.70 | 1.30 | 1.34 |
| 8 | Serve as a consultant in my clinic and in my community for osteoporosis care | 4.40 | 6.00 | 1.60 | 1.26 |
| 9 | Understand the pathophysiology of osteoporosis | 4.60 | 5.90 | 1.30 | 1.25 |
| 10 | Use the WHO FRAX to help with clinical decisions | 3.90 | 5.30 | 1.40 | 1.43 |
| 11 | Use the National Osteoporosis Foundation treatment guidelines | 4.20 | 5.40 | 1.20 | 1.14 |
| 12 | Distinguish good quality from poor quality acquisition, analysis, and reporting of bone density testing by DXA | 4.00 | 5.60 | 1.60 | 1.78 |
| 13 | Use DXA effectively in managing patients with osteoporosis | 4.20 | 5.50 | 1.30 | 1.57 |
| 14 | Individualize osteoporosis treatment decisions | 4.30 | 5.80 | 1.50 | 1.35 |
| 15 | Identify, evaluate, and treat patients with suboptimal response to osteoporosis treatment | 3.80 | 5.40 | 1.60 | 1.17 |
| 16 | Explain the benefits of secondary fracture prevention with a hospital-based FLS | 3.90 | 4.90 | 1.00 | 1.41 |
| 17 | Use the WHO criteria for classifying patients as having osteopenia, osteoporosis, or severe osteoporosis | 4.80 | 6.10 | 1.30 | 1.49 |
| 18 | Recommend interventions to reduce fall risk | 5.00 | 6.00 | 1.00 | 1.25 |
| 19 | Discuss the benefits and risks of nonpharmacological therapy for osteoporosis | 4.90 | 6.00 | 1.10 | 1.29 |
| 20 | Diagnose and treat men with osteoporosis | 3.90 | 5.40 | 1.50 | 1.51 |
After 10 months of weekly online clinics (October 2015 through July 2016), learners were asked to rate confidence in skills for 20 domains of osteoporosis care before and after the ECHO intervention. Results are for those who participated in at least 10 clinics and had direct patient care responsibilities (n = 10). Overall rating was 4.32 before ECHO and 5.67 after ECHO (P = 0.005 for difference). Rating scale: 0 = not applicable; 1 = none or no skill; 2 = vague knowledge, skills, or competence; 3 = slight knowledge, sills, or competence; 4 = average among my peers; 5 = competent; 6 = very competent; 7 = expert, teach others.
Abbreviations: DXA, dual-energy X-ray absorptiometry; FRAX, fracture risk assessment tool; WHO, World Health Organization.
4. Results
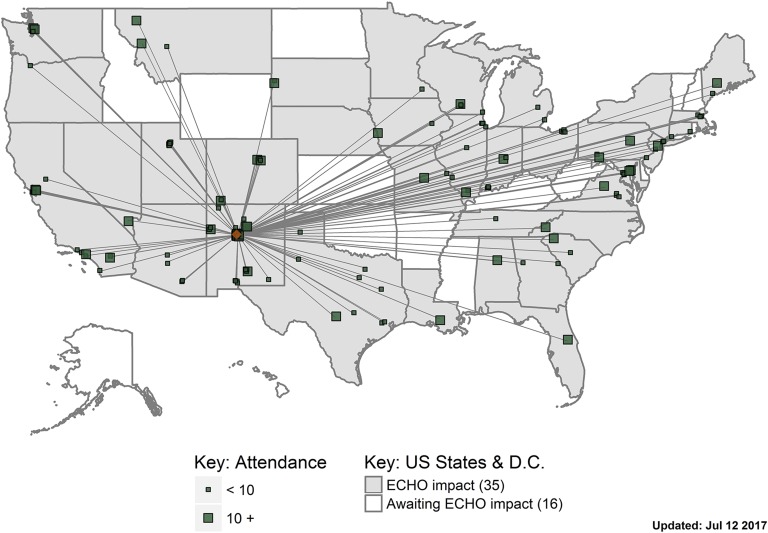
During the first 21 months of Bone Health TeleECHO, beginning 6 October 2015, 263 learners from throughout the United States and other countries (Canada, Mexico, United Kingdom, Ireland, Spain, Chile, and Trinidad and Tobago) registered to participate, with 221 participating in at least 1 TeleECHO session (Fig. 1). Participation at each TeleECHO clinic at the end of the reported period typically included 35 to 40 learners online and several more at the Project ECHO hub at UNM HSC. Learners represented many medical specialties (e.g., internal medicine, family practice, endocrinology, rheumatology, orthopedics), advanced practice providers (e.g., nurse practitioners, physician assistants), and other medical disciplines (e.g., physical therapists, nutritionists).
Figure 1.
United States map of Bone Health TeleECHO “hub and spoke” network (21 months’ data). The ECHO hub in Albuquerque links to faculty to learners and learners to other learners through collaborative, ongoing, real-time case-based medical education. Participants were located in 34 states and the District of Columbia. Participants in other countries are not shown on this map.
There were 16 responders to self-efficacy questionnaire, with 10 responders having attended more than 10 clinics and having patient care responsibilities. In this group, there was a statistically significant overall improvement in confidence of caring for osteoporosis patients (Fig. 2), with an effect size of 1.18 (P = 0.005).
Figure 2.
Bone Health TeleECHO outcomes. Learners with direct patient care responsibilities who attended more than 10 TeleECHO clinics (n = 10) were evaluated for self-confidence in managing osteoporosis patients in 20 different domains of care. There was a very large effect size [13] (P = 0.005) after the ECHO intervention compared with before the intervention.
5. Discussion
Bone Health TeleECHO has attracted participation of learners from a wide range of specialties and medical disciplines with broad geographic distribution. The self-efficacy data reported here show that regular participation in Bone Health TeleECHO improves self-confidence in caring for patients with osteoporosis. The ECHO model of learning has been demonstrated to improve clinical outcomes and be cost-effective for the care of patients with chronic hepatitis C [15] and other conditions [16], providing reassurance that Bone Health TeleECHO can improve the care of their osteoporosis patients and contribute to reducing the osteoporosis treatment gap. Health care providers who attain an advanced level of knowledge can take better care of their own patients and patients of other providers in the community, providing better care, closer to home, at lower cost than referral to a specialty center that may be located far from the patient who needs care. The ECHO model aims to move knowledge, not patients. Bone Health TeleECHO can be scaled to any level through replication, with the goal of having many Bone Health TeleECHO programs at hubs in many locations. A second Bone Health TeleECHO program has been launched with a hub in Michigan. A third program, based in Washington, DC, has been developed for fracture liaison service (FLS) coordinators. Other replications are expected in the near future.
There are limitations in interpreting the data presented here. The number of study subjects was small. Improvement of self-confidence in managing patients with osteoporosis does not guarantee improved clinical outcomes. Although the ECHO model of learning has improved outcomes for other disease states, osteoporosis may be different. The ultimate measure of osteoporosis treatment success is reduced fracture risk. However, it is unlikely that a study can be designed and conducted to show fracture risk reduction with any educational intervention. It could be expected that with better clinical skills in managing patients with osteoporosis, the patient mix will evolve to include higher risk patients, confounding the ability to assess changes in fracture rates. Surrogates of fracture risk can be measured; analysis of insurance health care claims data for bone density tests, patients diagnosed with osteoporosis, and osteoporosis prescriptions filled can provide an indirect assessment of improved clinical care and projected fracture risk reduction. Comparison could be made between Bone Health TeleECHO participants before and after the ECHO intervention or between Bone Health TeleECHO participants and similar health care professionals in similar practice settings who have not participated with ECHO. The feasibility of conducting such studies is being investigated.
The ECHO model of learning has potential applications for skeletal diseases other than osteoporosis. It could become an essential learning tool for FLS coordinators worldwide. It could be used as an effective and efficient means of linking clinicians with an interest in rare bone diseases. It could also be a useful way of teaching medical students, residents, and fellows in teaching programs at institutions lacking expertise in skeletal diseases, preparing them for specialty board examinations and, more important, for managing patients in clinical practice. This offers hope that replication of Bone Health TeleECHO in other locations may serve as a force multiplier that could play a role in reducing the osteoporosis treatment gap.
The ECHO Institute at UNM HSC provides helpful services and resources at no cost to assist in the replication of TeleECHO clinics. Individuals and teams from universities, hospitals, health care systems, and governmental agencies have participated in ECHO introductory videoconferences and on-site orientation and training. There is open sharing of TeleECHO curricula, best practices, and archived presentations. Development of a new TeleECHO clinic often begins with a local “champion” who is passionate about sharing knowledge and willing to assemble a committed team of experts. Faculty may be recruited from a single institution and assemble in one location or may be located elsewhere and linked online. Compensation for university faculty may be included with teaching responsibilities. Most TeleECHO clinics attract learners in the same or nearby time zones who speak the same language; however, technologies are now available to conduct bilingual TeleECHO clinics with simultaneous verbal or written translations.
Funding of TeleECHO clinics is typically from grants (federal, state, and private sources) or institutional support by universities and hospitals. As a TeleECHO clinic becomes more successful, it may be more attractive to other funders. Long-term sustainability of funding may be enhanced when payers recognize the economic benefit of supporting ECHO to avoid preventable consequences, such as fractures and fracture-related medical expenses.
6. Summary
Bone Health TeleECHO is an innovative strategy for expanding capacity for managing patients with osteoporosis by elevating the knowledge level of health care professionals in rural and underserved communities. Real-time ongoing teleconferencing technology links learners with a team of faculty experts for interactive discussions of best practice osteoporosis care with case-based learning and brief didactic presentations. The force multiplication effect of Bone Health TeleECHO is enhanced by replication in many locations.
Acknowledgments
Acknowledgments
Disclosure Summary: E.M.L. reported research grant support from Amgen; consulting fees from Amgen, Radius, Shire, Alexion, and Ultragenyx; speaking fees from Radius, Shire, and Alexion; and board membership with the National Osteoporosis Foundation, International Society for Clinical Densitometry, and the Osteoporosis Foundation of New Mexico. T.P.O. is a consultant and speaker for Amgen. The remaining authors have nothing to disclose.
Footnotes
- FLS
- fracture liaison service
- TeleECHO
- Extension for Community Health Care Outcomes
- UNM HSC
- University of New Mexico Health Sciences Center.
References and Notes
- 1.International Osteoporosis Foundation Facts and statistics. Available at: https://www.iofbonehealth.org/facts-statistics. Accessed 29 May 2017.
- 2.Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R; National Osteoporosis Foundation . Clinician’s guide to prevention and treatment of osteoporosis [published correction appears in Osteoporos Int. 2015;26(7):2045–2047]. Osteoporos Int. 2014;25(10):2359–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Solomon DH, Johnston SS, Boytsov NN, McMorrow D, Lane JM, Krohn KD. Osteoporosis medication use after hip fracture in U.S. patients between 2002 and 2011. J Bone Miner Res. 2014;29(9):1929–1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gillespie CW, Morin PE. Osteoporosis-related health services utilization following first hip fracture among a cohort of privately-insured women in the United States, 2008-2014: an observational study. J Bone Miner Res. 2017;32(5):1052–1061. [DOI] [PubMed] [Google Scholar]
- 5.Lewiecki EM, Adler RA, Curtis JR, Gagel R, Saag KG, Singer AJ, Siris E, Wright NC, Yun H, Steven PM. Hip fractures and declining DXA testing: at a breaking point? [abstract] J Bone Miner Res. 2016;31(Suppl):S26 [Abstract 1077]. [Google Scholar]
- 6.Khosla S, Shane E. A crisis in the treatment of osteoporosis. J Bone Miner Res. 2016;31(8):1485–1487. [DOI] [PubMed] [Google Scholar]
- 7.American Society for Bone and Mineral Research Call to action to address the crisis in the treatment of osteoporosis. Available at: https://www.asbmr.org/call-to-action.aspx. Accessed 11 January 2017.
- 8.Arora S, Thornton K, Murata G, Deming P, Kalishman S, Dion D, Parish B, Burke T, Pak W, Dunkelberg J, Kistin M, Brown J, Jenkusky S, Komaromy M, Qualls C. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364(23):2199–2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.University of New Mexico School of Medicine. Project ECHO. About ECHO. Available at: https://echo.unm.edu/about-echo/. Accessed 3 August 2017.
- 10.www.GovTrack.us. S. 2873 (114th): ECHO Act. Available at: https://www.govtrack.us/congress/bills/114/s2873. Accessed 3 August 2017.
- 11.University of New Mexico School of Medicine Bone Health ECHO. Available at: http://echo.unm.edu/bone-health/. Accessed 3 August 2017.
- 12.Lewiecki EM, Boyle JF, Arora S, Bouchonville MF II, Chafey DH. Telementoring: a novel approach to reducing the osteoporosis treatment gap. Osteoporos Int. 2017;28(1):407–411. [DOI] [PubMed] [Google Scholar]
- 13.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: L. Erlbaum Associates; 1988:xxi. [Google Scholar]
- 14.Sawilowsky S. New effect size rules of thumb. J Mod Appl Stat Methods. 2009;8(2):467–474. [Google Scholar]
- 15.Wong JB, Thornton KA, Carroll C, Arora S. Cost-effectiveness of hepatitis C treatment by primary care providers supported by the extension for community healthcare outcomes (ECHO) model [abstract]. Hepatology. 2013;58(S1):33A. Abstract 245. [Google Scholar]
- 16.Moore AB, Krupp JE, Dufour AB, Sircar M, Travison TG, Abrams A, Farris G, Mattison MLP, Lipsitz LA. Improving transitions to post-acute care for elderly patients using a novel video-conferencing program: ECHO-care transitions. Am J Med. 2017;130(1):1119–1204. [DOI] [PubMed] [Google Scholar]