Abstract
Background
Adaptive behaviors are essential for optimal outcomes and independence in individuals with developmental disabilities. This study examined longitudinal trajectories of adaptive behavior in infants with fragile X syndrome (FXS), compared to typical development (TD) and infant siblings of children diagnosed with autism (ASIBs).
Method
Participants included 76 male infants (FXS =25, ASIBs=27, TD = 24) assessed up to 4 times between 6 and 24 months of age for a total of 215 assessments of adaptive behavior. A sample of 12 females with FXS was included for a comparative sex analysis.
Results
Results indicate that infant males with FXS displayed lower initial adaptive behavior across all domains that emerged by 9 months-of-age with slower growth rates than both comparison groups. A flat profile across the domains at 24 months was evident. Increased severity of autism symptoms was related to reduced adaptive skills at 24 months-of-age. Females with FXS displayed higher scores than males on the Socialization and Motor domains and equivalent scores on the Communication and Daily Living domains at 9 months-of-age with different rates of growth across domains.
Conclusions
This is the first study to provide evidence of etiological specificity in adaptive behavior profiles during infancy across two populations at high risk for ASD. These findings support targeted adaptive behavior interventions in young children with FXS beginning as early at 9 months of age to reduce identified deficits and the cascading impacts of these early impairments.
Keywords: adaptive behavior, fragile x syndrome, infancy, autism infant siblings
Introduction
Optimal outcomes for everyday functioning are highly reliant on adaptive behavior skills for both typical and clinical populations, with adaptive skills touted as more salient than intellectual ability (Kanne et al., 2011). In fact, deficits in adaptive behavior have been associated with increased risk of psychopathology (Tremblay, Richer, Lachance, & Côté, 2010), impaired health and lower quality of life (Ebrahim et al., 2013), and poor social functioning (Farley et al., 2009). Adaptive behavior impairments are common in children with intellectual disabilities; however, the emergence and profile of adaptive behavior impairments differs across genetic syndromes and disorders.
Fragile X syndrome (FXS) is a single gene disorder caused by a CGG repeat expansion on the FMR1 gene that occurs in approximately 1 in 5000 in males (Coffee et al., 2009). FXS results in almost universal intellectual disability in males and is the leading known heritable cause of intellectual disability. Likewise, FXS is highly associated with autism spectrum disorder (ASD) with approximately 60% of males meeting DSM criteria (Harris et al., 2008). As such, FXS is an ideal model to study the emergence and trajectory of adaptive behavior skills in infants at high risk for both intellectual disabilities and ASD.
Despite the importance of characterizing early development in FXS, only a handful of studies on the infant behavioral phenotype in FXS exist with no prospective research on adaptive behavior in the first two years of life. Adaptive behaviors are the strongest predictor of independence in individuals with FXS (Hartley et al., 2011), therefore understanding the early development of adaptive behavior, upon which more complex and mature behaviors are built, can facilitate treatment planning and refine prognostic indicators. Improved characterization of adaptive behavior trajectories in young children with FXS is critical given evidence that early intervention can result in improved adaptive behavior skills that may generalize to other domains including socialization skills and core autism symptoms (Estes et al., 2015).
Adaptive behavior impairments have been documented in individuals with FXS; however, clear strengths and weaknesses in adaptive skills have not been established. Some research suggests a relative strength in Daily Living skills (Dykens et al., 1996; Hatton et al., 2003), while others report strengths in Socialization (Frolli, Piscopo, & Conson, 2014; Klaiman et al., 2014). However, in direct contrast, Daily Living skills (Frolli et al., 2014) and Socialization have been identified as weaknesses in other reports (Hahn et al., 2015), with some differences in strengths and weaknesses being attributed to the presence or absence of autism symptomatology (Hatton et al., 2003). The most consistent finding is a relative weakness in the area of adaptive Communication (Dykens et al., 1996; Frolli et al., 2014; Klaiman et al., 2014; Rogers, Wehner, & Hagerman, 2001). These contrasting findings may reflect the varying age groups with which these studies were conducted, suggesting that patterns of strengths and weaknesses may change across development. Little is known about the domain of adaptive Motor development in FXS, given that it has been excluded from many previous analyses at the domain level due to the norm scores being limited to children under the age of 6 years. However in the one study that compared adaptive Motor skills to other domains, Motor was identified as a strength, but only in those with co-occurring autism symptomatology (Hatton et al., 2003).
Developmental trajectories in adaptive skills have been an important area of research in FXS. Studies to-date have varied in methodology, metrics, and varying age distributions which has resulted in what may appear to be contradictory findings (Table 1 presents study summaries). In general, studies analyzing raw or age equivalent scores have reported overall growth in adaptive skills from toddlerhood (i.e., 1-2 years old) through middle childhood (i.e., 10-11 years old) in males with FXS (Hahn et al., 2015; Hatton et al., 2003; McCary, Machlin, & Roberts, 2013). These findings are consistent with a cross-sectional study of males between the ages of 1 and 10 suggesting increasing skill acquisition with age (Dykens et al., 1996). These studies have also reported a slowing, plateau or slight loss of adaptive skills for individuals with FXS beginning around the age of 10 (Dykens et al., 1996; Hahn et al., 2015).
Table 1. Summary of literature examining adaptive behavior in fragile X syndrome across development.
| First Author | Year | FXS n | Sex | Metric | Sample | Age | Analysis | Primary Conclusions |
|---|---|---|---|---|---|---|---|---|
| Dykens | 1996 | 132 Group 1 = 44 Group 2 = 42 Group 3 = 28 Group 4 = 16 |
Males | Age equivalent scores | Cross-sectional | Group 1: 1-5 (M = 3.8) Group 2: 6-10 (M = 8.18) Group 3: 11-15, (M =13.71) Group 4: 16-20 (M = 18.63) |
Correlation | Age and scores are positively correlated between 1-5 years, and 6-10 years. No correlation between age and scores were found between 11-20 years. |
| Hatton | 2003 | 70 | 60 Males 10 females |
Age equivalent scores | Longitudinal (2-8 time points m = 4.4) | l-11, mean = 6.3 years | HLM | Positive growth in overall adaptive skill acquisition over time. |
| Hahn | 2015 | 55 | 44 Males 11 Females |
Raw Scores | Longitudinal, 3 to 5 time points (M = 4.87) | 2-10 years | HLM | Positive growth through middle childhood, with some evidence of minor declines. |
| Klaiman | 2014 | 275 | 186 Males 89 Females |
Standard scores | Longitudinal (1-4 times points) | Time 1: 9.12 years | HLM | Standard scores decreased over time. This decrease was greater in males than females. |
| Frolli | 2014 | 47 | Males | Standard scores | Longitudinal, 3 time points | Time 1: 9-11 years (M = 10.25 years) Time 2: 11-13 years Time 3: 13-15 years |
Repeated Measures ANOVA | Domains of Communication and Socialization increased over time, Daily Living skills remained stable. |
| Fisch | 2002 | 18 Group 1= 8 Group 2 = 10 |
Males | Standard Scores | Longitudinal (2 time points, 2 cohorts) | Group 1: M = 5 years Group 2: M = 8 years |
Repeated Measures MANOVA | Declines in adaptive behavior composite over time in both age cohorts. |
In contrast to these studies reporting growth using raw or age equivalent scores, research using standard scores reports mixed findings. Declines across all domains of adaptive behavior have been reported in a small sample of children between 5 and 11 years (Fisch et al., 2002) and confirmed in the largest sample with the most extensive age range to date spanning 2 through 18 years (Klaiman et al., 2014). Yet, increases in the Communication and Socialization domains and no change in Daily Living skills between the ages of 9 and 15 have also been reported (Frolli et al., 2014). These contradictory findings may be partly attributed to contrasting analytical methods with Frolli's work examining discrete changes between two time points, while Klaiman's (2015) study utilized growth models which intentionally smooth small changes between time points to identify an average growth trajectory.
Taken together, existing work suggests that rates of growth in adaptive behavior in FXS are nearly half that expected of typically developing (TD) peers resulting in delays across all domains that become more severe over time. Consistent across studies is the negative impact of autism symptomology on adaptive behavior skill development in children with FXS with autism symptoms exerting an increasingly negative impact over time (Cohen, 1995; Hahn et al., 2015; Hatton et al., 2003; Hustyi et al., 2014; Rogers et al., 2001). Likewise, consistency in the effect of sex is present across multiple studies with girls with FXS exhibiting less severe impairments in their adaptive behavior development and a faster rate of growth than their chronologically age matched, but not mental age matched, male counterparts (Hahn et al., 2015; Hatton et al., 2003; Klaiman et al., 2015). The milder impairment in females with FXS is likely due to the presence of their second X chromosome, which is unaffected by the FMR1 mutation (Hagerman, Rivera, & Hagerman, 2008; Huddletson, Visootsak, & Sherman, 2014).
The correspondence between mental age/intellectual level and adaptive behavior is inconsistent across multiple levels. The defining features of adaptive behavior and its measurement are still emerging (Tassé et al., 2012), with some studies indicating poor correspondence between adaptive behavior and intellectual skills seen in young children with ASD (Estes, Zwaigenbaum et al., 2015). In FXS, nonverbal intellectual skills and adaptive behavior appear related but not always equal, with some reports of nonverbal cognitive levels exceeding adaptive skills before 10 years-of-age with convergence over time (Hatton et al., 2003) while others report adaptive skills commensurate with or exceeding cognitive levels in a sample of 2-24 year olds (Dykens et al., 1996). In more recent longitudinal work in 2 to 10 year olds with FXS, lower cognitive functioning was found to negatively impact adaptive behavior growth over time (Hahn et al., 2015).
Etiologically distinct profiles of adaptive behavior have not been well studied with the majority of studies focused on FXS exclusively without a comparison group. In the only published study to contrast adaptive behavior in FXS to other genetic disorders, results indicate partial specificity (Dykens & Hodapp, 2001) in that the adaptive behavior profiles displayed some etiological specificity, yet, there was a moderate degree of overlap attributed to the presence of intellectual impairments within and across the groups (DiNuovo & Buono, 2011). Males with FXS displayed adaptive behavior impairments that were not distinct from chronological and mental age matched groups with Prader-Willi, Down and Williams syndromes, yet, their adaptive skills were higher compared to Angelman syndrome (DiNuovo & Buono, 2011). In the only study that contrasted adaptive behavior skills in FXS to ASD, results indicate that the adaptive skills of young children (18 to 83 months-of-age) with FXS are more impaired and earlier emerging than a chronologically age matched group with non-syndromic ASD (McCary et al., 2013).
Given the elevated risk of ASD diagnoses in FXS and the presence of autism symptoms in 53% of 12 month-old infants with FXS (Roberts, Tonnsen, McCary, Caravella, & Shinkareva, 2016) contrasting the developmental trajectory of adaptive skills in infants with FXS to high risk infants with an older sibling with ASD (ASIBs) would contribute to the specificity of adaptive behavior profiles for both populations. However, research examining adaptive behavior in infant ASIBs is also limited as it is in FXS. To date, two studies exist that reported analysis of adaptive behavior in ASIBs less than 2 years old (Estes, Zwaigenbaum, et al., 2015; Toth, Dawson, Meltzoff, Greenson, & Fein, 2007). One compared 20-month-old ASIBs without ASD to an age matched low risk control group, and identified lower mean scores on all adaptive behavior domains, with the exception of Communication in the high risk group, when compared to the control group. These findings suggest that even when autism does not develop, ASIBs evidence lower adaptive functioning than low risk children. In contrast, Estes and colleagues (2015) did not find differences between unaffected ASIBs and low risk controls on adaptive behavior scores between 6 and 24 months of age. However, they did report that ASIBs presenting with high levels of ASD symptomatology, had lower adaptive skills than typical controls that emerged by 6 months-of-age and became progressively more discrepant through 24 months-of-age (Estes, Zwaigenbaum et al., 2015). These contrasting findings likely represent the inherent phenotypic heterogeneity in ASIB samples (Landa, Gross, Stuart, & Bauman, 2012; Ozonoff et al., 2014).
In summary, adaptive behaviors in children with FXS appear to be delayed with deficits emerging in toddlerhood. Adaptive skill growth peaks by middle childhood with overall adaptive functioning reaching maximum age equivalents between 5 to 7 years of age (Dykens et al., 1996; Hatton et al., 2006). Additionally, autism symptomatology leads to more severe impairment in adaptive functioning in individuals with FXS. Sex also impacts adaptive skill development, with girls with FXS gaining skills at a faster rate than males resulting in overall higher skill acquisition. However, research has not yet investigated adaptive skills in infancy to determine when these deficits first appear, how adaptive skills develop across the first two years of life, what their relationship is with autism symptomology, and whether growth trajectories differ between males and females.
The current study aims to address gaps in the literature by examining adaptive behavior development in infants with FXS at 6, 9, 12 and 24 months-of-age contrasted to age matched TD controls and ASIBs, who are at high risk for ASD and other developmental impairments. This project was guided by the following 3 research questions and hypotheses:
Do adaptive behavior trajectories differ between infants with FXS, ASIBs and a TD control group over the first two years of life? We hypothesize that infants with FXS will evidence lower levels of adaptive functioning beginning at 9 months and exhibit slower growth rates than both comparison groups.
Do infants with FXS and ASIBs show specific strengths or weaknesses across adaptive behavior domains at 24 months of age? We hypothesize that infants with FXS will show strengths in the domains of Socialization and Motor skills, and weaknesses in the areas Communication and Daily Living.
How do autism symptom severity and sex impact growth in adaptive behavior skills across the first two years of life in infants with FXS syndrome? We hypothesize that higher rates of autism symptomatology will be related to slower rates of adaptive skill acquisition over time and lower adaptive behavior scores at 24 months of age, and female infants with FXS will evidence higher initial adaptive skills and faster growth rates than males with FXS.
Methods
Participants
Participants included 76 male infants who are part of an ongoing longitudinal study aimed to detect behavioral and biomarkers of autistic features in infants at high risk for developing ASD, which included three groups; infants with FXS (n= 25), ASIBs (n=27), and low risk controls (TD) (n= 24). FXS was confirmed by a genetic report. Inclusion into the ASIB group was based on a community diagnosis of ASD in the older sibling with known causes (e.g., syndrome) ruled out. Genetic testing for FXS was not conducted on the ASIB group, however a family history of any known syndromes or intellectual disability was ruled out. The ASIB group was included as an etiologically distinct group at elevated risk for ASD. For the low risk TD group, there was no family history of ASD and typical development was confirmed at 24 months through our study. Typical development was defined as no developmental delay (Mullen Early Learning Composite > 85) and an absence of elevated autism features (ADOS-2 severity score < 4) at 24 months. Exclusion criteria for all participants included diagnosis of any medical condition (other than FXS), premature birth before 37 weeks or birth weight less than 2000 grams, families whose predominant language in the home was not English, and infants who were adopted. TD participants were most commonly recruited through letters and pamphlets distributed through community settings, such a pediatricians' offices and parent groups. To target the FXS and ASIB cohorts, recruitment materials were sent through listservs, parent support groups, social media groups, and service provision centers exclusive to these two populations.
A prospective longitudinal design was utilized. Infants were seen at 6 (M=6.43, SD =0.67), 9 (M=9.29, SD =0.56), 12 (M=12.61, SD =0.81) and 24 months (M = 24.75, SD = 0.92) In total, data from 215 assessments are included in the analyses (57 FXS, 86 ASIB and 72 TD). Characteristics of the sample are presented in Table 2. Variability in assessments by group and age was present given the design of the primary study focused on 9, 12 and 24 months across the three groups while a complementary study focused on the ASIB and TD groups extended these assessments to 6 months. Six-month assessments in the FXS group were conducted opportunistically. Infants with FXS were enrolled as young as possible; however, participants were enrolled up to 24 months. This is an essential practice in infant studies on FXS given the rarity of the disorder, and the reality of delayed diagnoses, given the average age of diagnosis of FXS is 36 months (Bailey, Raspa, Bishop, & Holiday, 2009). All infants included in the study had between 1 and 4 assessments, with 83% of participants having at least 2 assessments. A subset of 12 female infants with FXS seen at the same age intervals was added to the FXS sample to facilitate preliminary analysis of sex differences in adaptive skill trajectories.
Table 2. Sample Characteristics.
| Variable | FXS females n=12 | FXS males n=25 | TD n=24 | ASIB n=27 |
|---|---|---|---|---|
| Sample Size (n) | ||||
| 6 months | 2 | 6 | 17 | 15 |
| 9 months | 8 | 14 | 21 | 21 |
| 12 months | 7 | 17 | 16 | 27 |
| 24 months | 9 | 20 | 18 | 23 |
|
| ||||
| Age (months) | ||||
| 6 months | 7.27 (2.79) | 6.64 (1.05) | 6.28 (0.52) | 6.51 (0.65) |
| 9 months | 9.61 (1.09) | 9.45 (0.76) | 9.13 (0.37) | 9.35 (0.55) |
| 12 months | 12.57 (0.41) | 12.74 (0.92) | 12.29 (0.39) | 12.72 (0.89) |
| 24 months | 25.08 (2.26) | 25.02 (1.03) | 24.63 (0.93) | 24.62 (0.79) |
|
| ||||
| Vineland1 | ||||
| 6 months | 81 (5.66) | 74.83 (8.06) | 96.94 (8.13) | 88.60 (7.60) |
| 9 months | 93.50 (12.82) | 74.79 (13.01) | 96.43 (8.82) | 90.71 (9.04) |
| 12 months | 91.43 (14.50) | 73.94 (7.00) | 96.75 (8.53) | 97.58 (8.32) |
| 24 months | 87.89 (11.48) | 75.10 (9.48) | 97.50 (9.08) | 91.96 (8.27) |
|
| ||||
| Mullen2 | ||||
| 24 months | 78.29 (21.84) | 57.50 (9.81) | 105.93 (14.03) | 85.52 (17.28) |
|
| ||||
| AOSI3 | ||||
| 12 months | 5.83 (6.15) | 10.76 (5.52) | 4.88 (3.72) | 7.41 (4.57) |
|
| ||||
| ADOS4 | ||||
| 24 months | 3.25 (2.05) (n=8) | 6.16 (3.08) (n=19) | 1.53 (0.74) (n=15) | 4.09 (2.6) (n=22) |
|
| ||||
| Maternal Education | ||||
| Not Reported | 0 | 2 (8%) | 0 | 0 |
| < High School | 0 | 2 (8%) | 1 (4%) | 0 |
| High School | 2 (17%) | 2 (8%) | 1 (4%) | 4 (15%) |
| 1-4 years College | 4 (33%) | 8 (32%) | 12 (50%) | 12 (44%) |
| > Bachelors Degree | 6 (50%) | 11 (44%) | 10 (42%) | 11 (41%) |
|
| ||||
| Participant Race | ||||
| Not Reported | 0 | 1 (4%) | 0 | 0 |
| American Indian | 1 (8%) | 1 (4%) | 0 | 0 |
| Asian | 1 (8%) | 1 (4%) | 0 | 0 |
| Black | 1 (8%) | 3 (12%) | 4 (17%) | 2 (7%) |
| Hispanic | 1 (8%) | 1 (4%) | 0 | 0 |
| Mixed Race | 2 (17%) | 5 (20%) | 1 (4%) | 1 (4%) |
| White | 6 (50%) | 14 (56%) | 19 (79%) | 24 (89%) |
Adaptive Behavior Composite (Standard Score)
Early Learning Composite (Standard Score)
AOSI Total Score
ADOS Calibrated Severity Score
Measures
Adaptive Behavior
The Vineland Adaptive Behavior Scales- II, Survey Form (Sparrow et al., 2005), is a semi-structured caregiver interview that measures current adaptive behavior functioning in four domains, Communication, Socialization, Daily Living Skills and Motor Skills. Individual items are scored on the frequency with which the individual completes the behavior independently (usually (2), sometimes (1), or never (0)). Higher scores indicate higher levels of adaptive skill development. Raw scores are utilized in all growth curve analyses given that standard scores are corrected for time (i.e. standardization by age), making true growth in skills more difficult to measure in a linear growth model. Standard scores (M = 100, SD = 15) will be utilized in the profile analysis to improve interpretability, given that raw scores cannot be directly compared across domains. The Vineland has been validated for individuals from birth to 99 years of age including 470 infants between 0 to 2 years. Mean reliability scores in the standardization sample on the four domains for this age group are reported as follows: Communication= .91, Daily Living skills = .84, Socialization = .92, motor skills = .93.
Autism Symptomatology in Infancy
The Autism Observation Scale for Infants (AOSI) (Bryson, Zwaigenbaum, McDermott, Rombough, & Brian, 2008) is a direct observation scale designed to identify behaviorally observed symptoms of autism in infants 6 to 18 months of age. Throughout the 20-minute measure, infants are engaged in two free play sessions, and behavioral presses from the examiner designed to target specific behaviors indicative of autism risk. Behaviors are rated on a scale from 0 to 3 (0 = typical response/absence of atypical response, 3 = great atypicality) and a total score is calculated. Total scores of 9 or more denote a behavioral presentation that signifies autism risk and has been found to be predictive of a best estimate diagnosis of autism at 3 years of age (Bryson, 2005). Total scores on the AOSI at 12 months are used in the analysis of research question 3 as a measure of autism symptom severity as a level 2 time-invariant predictor.
Autism Symptomatology at 24 months
The ADOS-2 is a play based semi-structured assessment designed to press for social interaction to rate the presence of behaviors consistent with a diagnosis of autism spectrum disorder. Five modules are available (Toddler, 1-4) which differ based on the child's age and language level. Behaviors are generally rated on a 0-3 scale (0 = typical response/absence of atypical response, 3 = great atypicality), and a total score is calculated. To compare scores across modules, a calibrated severity score can be obtained from the total score on each module. Calibrated severity scores are used in the analysis of research question 3 as a measure of autism symptom severity as a level 2 time-invariant predictor. A subset of 19 infants with FXS and 22 ASIB infants received an ADOS at the 24-month time point, consistent with the study design. The remaining participants (5 FXS, 4 ASIB) have not yet aged to 24 months so the ADOS-2 and Vineland data have not yet been collected at that age point. There were two participants (1 FXS, 1 ASIB) who were not administered the ADOS-2 at their 24-month-assessment due to behavioral compliance or data collection error.
Developmental Level
The Mullen Scales of Early Learning (Mullen) is a standardized developmental assessment for children ages 0-60 months that measures skills in five areas of development, expressive language, receptive language, fine motor, gross motor and visual reception. Each domain has a T-score of 50 and a standard deviation of 10. A summary standard score, the early learning composite (ELC), is generated from the domains (with the exclusion of gross motor). The ELC has a mean of 100, and standard deviation of 15. ELC was used to rule out developmental delays in the TD group. Developmental level was not controlled for in the analyses given that we were interested in uncontrolled parameter estimates that represented the true measured differences between groups in adaptive behavior.
Procedure
All procedures were conducted in compliance with the USC Institutional Review Board. At the 6 and 12-month visits, infants and their families came to lab at the University of South Carolina. To minimize travel burden on the families, research staff traveled to the family's homes for the 9 and 24 month visits where procedures were identical to those administered in the lab environment. AOSIs were administered by research staff who obtained official administration and coding reliability (>80%) with the developers of the measure. In lieu of the AOSI at the 24-month visit, participants were administered an ADOS-2 by research reliable administrators. The ADOS-2 was not included in the study design at the 12-month time point given that it requires a minimum mental age of 12 months, which is not achieved in the FXS sample. After the 24-month assessment, a clinical best estimate diagnosis was determined by a team of at least 3 members of the research staff who were all research reliable on the ADOS, one of whom was a licensed psychologist. All available clinical information including the Mullen, Vineland and ADOS, were used to determine whether the child met criteria for a diagnosis of Autism Spectrum Disorder. Consistent with the literature, about 20% of our ASIB (23%) and about 60% of the FXS sample met criteria for ASD (58%). A sample of 20% of all AOSI and ADOS administration were scored from tapes of the administrations for inter-rater reliability, which were 80.9% and 83.3% respectively. Participants were compensated for participation.
Data Analysis
Statistical Analysis was completed using R (R Core Team, 2013). To address the study's primary aims of examining trajectories of adaptive skill development, multilevel modeling was used. Multilevel modeling is ideal for these analyses given its robustness to uneven time points and missing data. Age was centered at 9 months so that the intercept is interpreted as the average predicted adaptive behavior functioning at 9 months of age. Age was centered at 9 months, rather than the earliest time point of 6 months, given the smaller sample of data available at 6 months. Slopes and intercepts were allowed to vary randomly. Separate models were estimated for each of the 4 Vineland domains.
In subsequent models of FXS males only, autism symptom severity scores were included as level-2 time invariant predictors of adaptive behavior growth trajectories. In addition to examining the impact of autism symptomatology on adaptive behavior growth trajectories, follow up analyses were conducted to compare mean standard scores based on a clinical best estimate diagnosis of ASD at 24 months. T-tests were used to examine these relationships. Due to small sample sizes, these comparisons within FXS and ASIB participants are to be considered as preliminary.
Trajectories of all domains on the Vineland were compared between males and female infants with FXS with multilevel models. Given the small sample sizes for females (n=12) and greater missing data, those results are presented as preliminary. However, given the lack of research with females with FXS, we include these results. Dependent variables in the growth models are Vineland domain raw scores. Assumptions of homogeneity of variance and multivariate normality were examined visually with no violations identified. All parameter estimates without accompanying p-values reported in the text are statistically significant at a .05 alpha level.
To examine profiles across domains, a one sample Hotelling's T-square profile analysis was conducted at the 24-month time point using Vineland domain standard scores. Due to different sample sizes across time points a repeated measures ANOVA would have required the use of equal groups across all time points reducing the sample to only 6 in the FXS group. Therefore, the 24 month time point was selected for the profile analysis given the larger number of skills expected at this age allowing for a more robust examination of strengths and weaknesses and the larger sample size.
Results
Research Question 1: Do adaptive behavior trajectories differ between infants with FXS, ASIBs and a typically developing control group?
At 9 months of age, infants with FXS evidenced lower adaptive Socialization skills compared to both comparison groups, scoring on average 7 points lower than TD infants (β =7.13, SE = 1.29) and 6 points lower than ASIBs (β = 5.73, SE = 1.28). These differences become greater with time, as TD (β = 0.95, SE = 0.26) and ASIBs (β = 0.52, SE = 0.25) gained adaptive Socialization skills at a faster rate than FXS infants.
Differences in adaptive Communication skills are also evident by 9 months in FXS infants. On average, FXS infants scored 7 points lower than TD infants (β = 6.62, SE = 1.03) and 5 points lower than ASIBs (β = 4.70, SE = 1.02). Growth rates also differed, with TD (β = 1.84, SE = 0.31) and ASIB (β = 1.03, SE = 0.29) infants gaining adaptive Communication skills at a faster rate than infants with FXS.
Differences in Daily Living skills were also evident by 9 months of age in FXS infants, who scored on average 3 points lower than both TD (β = 3.42, SE = 0.70) and ASIBs (β = 2.85, SE = 0.69). Growth rates also differed, with TD (β = 0.88, SE = 0.15) and ASIB (β =0.52, SE = 0.14) infants gaining Daily Living skills at a faster rate than infants with FXS.
Adaptive Motor skills were lower in FXS infants at 9 months of age, with FXS infants scoring on average 11 points lower than TD infants (β = 10.69, SE = 1.91), and 6 points lower than ASIBs (β = 6.49, SE = 1.88). FXS infants gained skills at a slower rate than both TD (β = 0.72, SE = 0.19) and ASIBs (β = 0.91, SE = 0.18). Model results are presented in Figure 1.
Figure 1.

Average linear growth trajectories of raw adaptive behavior scores by risk group.
TD = Typically Developing, ASIB = Infant Siblings of Children with Autism, FXS = Fragile X Syndrome
Research Question 2: Do infants with FXS or ASIBs show specific strengths or weaknesses across adaptive behavior domains at 24 months of age?
A one-sample profile analysis was run to examine the hypothesis of flatness across domains of adaptive functioning using Hotelling's T-square. Results of the profile analyses for both groups indicated that the profile was flat, suggesting that at 24 months neither infants with FXS or ASIBs show a distinct profile of strengths or weaknesses across the four domains of adaptive functioning. Means and standard deviations across the four domains are presented in Figure 2a and Figure 2b.
Figure 2.

a. Mean standard score values at 24 months across Vineland domains in males with FXS graphed with sample standard deviations.
b. Mean standard score values at 24 months across Vineland domains in ASIB males graphed with sample standard deviations.
Research Question 3: What is the relationship of autism symptom severity and sex to growth in adaptive behavior skills across the first two years of life in infants with FXS syndrome?
Growth models were run to examine the relationship between autism symptomatology and adaptive behavior growth trajectories. Two separate models were run using AOSI Total Scores at 12 months (n=17) and ADOS-2 Calibrated Severity Scores at 24 months (n=19) as predictors of the adaptive behavior growth trajectories, respectively. Across all domains, AOSI scores were not related to adaptive behavior scores at 9 months or adaptive skill growth rates. Across all domains, average adaptive behavior scores at 9 months were not related to autism symptom severity at 24 months. However, symptom severity at 24 months was related to growth in adaptive behavior for the domains of Socialization (β = -0.11, SE = 0.05), Communication (β = -0.15, SE = 0.06) and approaching statistical significance in Daily Living (β = -0.06, SE = 0.03, p = .06). Across these three domains, higher autism severity scores at 24 months were related to slower rates of growth in adaptive skills. Autism symptom severity at 24 months was not related to growth rates in the adaptive Motor skills domain (p = 0.82).
Given the findings that autism symptom severity at 24 months impacted adaptive skill growth, follow up analyses were conducted to examine group differences based on autism diagnostic status in the FXS group, compared to the ASIB group at 24 months. Clinical best estimate diagnoses were given to all participants in the ASIB and FXS groups to determine if they met criteria for ASD. Welch's two sample T-tests were used to compare Vineland domain standard scores within each risk group, based on autism status (i.e. FXS + ASD and FXS − ASD, ASIB + ASD, ASIB − ASD). Given the multiple comparisons across the 5 Vineland standard scores (domain scores and the Adaptive Behavior Composite), a Bonferroni correction was applied (.05/5) and the alpha level was set at p<.01. In the Communication domains, FXS+ASD infants evidenced lower scores (M=70.09 SD=13.04) than the FXS-ASD group (M=84.75, SD=8.08) t(16.69) = 3.02. In the ASIB group, ASIB's with ASD evidenced lower scores in the Daily Living Skills (M=80.40, SD=4.22) t(9.67) = 5.89, and Adaptive Behavior Composite domains (M=81.80, SD=4.21) t(10.85) = 5.05, than ASIBs without ASD (Daily Living; M=94.59, SD=6.18) (Adaptive Behavior Composite; M=94.41, SD=6.77). The means and standard deviations are presented in Table 3.
Table 3. Vineland Adaptive Behavior Standard Scores at 24 Months of Age Across the FXS and ASIB Groups Based On Clinical Best Estimate Diagnosis of Autism Spectrum Disorder.
| FXS+ASD n = 11 | FXS-ASD n = 8 | ASIB+ASD n = 5 | ASIB-ASD n = 17 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| M | SD | M | SD | t-test | M | SD | M | SD | t-test | |
| Communication | 70.09 | (13.04) | 84.75 | (8.08) | 3.02* | 81.20 | (9.26) | 96.71 | (8.39) | 3.36 |
| Socialization | 73.91 | (8.41) | 84.25 | (7.72) | 2.78 | 82.00 | (8.46) | 92.29 | (6.69) | 2.50 |
| Daily Living | 72.55 | (15.08) | 81.12 | (6.06) | 1.71 | 80.40 | (4.22) | 94.59 | (6.18) | 5.89* |
| Motor | 79.91 | (10.61) | 80.88 | (6.75) | 0.24 | 96.20 | (4.92) | 99.06 | (8.61) | 0.94 |
| Adaptive Behavior Composite | 71.09 | (10.61) | 79.62 | (5.07) | 2.33 | 81.80 | (4.21) | 94.41 | (6.77) | 5.05* |
p<.01.
Note. M = Mean. SD = Standard Deviation. ASD diagnoses were determined by a clinical best estimate procedure.
To examine sex differences in FXS, a sample of 12 female infants with FXS was added to the sample of 25 males with FXS. Growth trajectories were compared for males and females with FXS across all domains of adaptive functioning. At 9 months of age, females were found to have higher scores in the domains of Socialization (β = − 8.13, SE =2.84) and Motor (β =-9.90, SE = 3.23). Rates of change for both of these domains were not significant. Different relationships were found in the Communication and Daily Living domains, where initial scores at 9 months did not differ between the sexes, however females gained skills at faster rates than males in both Communication (β = -0.60, SE = 0.27) and Daily Living (β = -0.43, SE = 0.15) leading to greater discrepancies in scores as the infants got older. These trajectories are presented in Figure 3.
Figure 3.
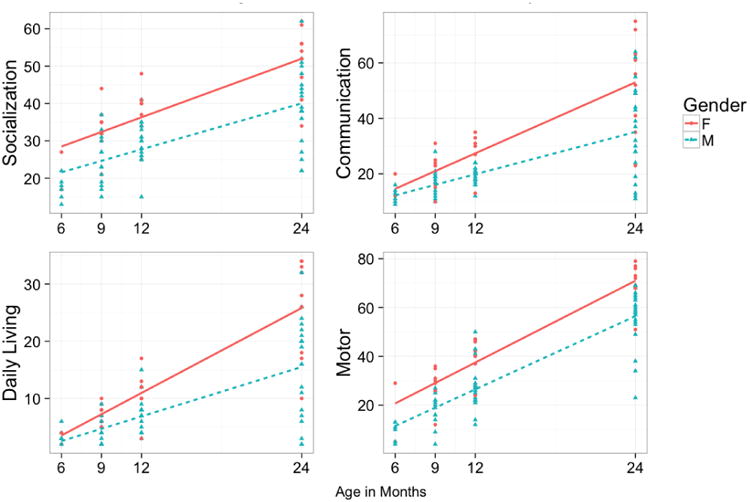
Average linear growth trajectories of raw adaptive behavior scores by sex.
F = Female, M = Male
Discussion
This paper is the first prospective longitudinal study to examine adaptive skills in infants with FXS less than 12 months of age and the first to include an etiologically distinct comparison group of infants at high risk for ASD. Given the importance of adaptive skills for independent functioning and optimal outcomes across social, cognitive and health domains, understanding the presentation and growth of adaptive behavior skills during infancy can inform targets for treatment and provide prognostic indicators beginning in infancy. This is particularly salient given evidence that early intervention can improve adaptive skills in young children with ASD which may then generalize to other domains of functioning with cascading effects (Estes, Munson, et al., 2015).
Adaptive Behavior Trajectories
Consistent with our hypothesis, infants with FXS possessed adaptive skill deficits across all domains compared to both ASIB and TD infants that emerged at 9 months of age. The rate of growth across all adaptive domains was slower for the group with FXS than both the ASIB and TD groups resulting in a greater magnitude of discrepancy and increased severity of impairment for infants with FXS with age. The difference in the rate of growth was largest in the Communication domain where the FXS infants gained skills at about half the rate of TD infants. Of interest, adaptive skills in infants with FXS were lower and developed more slowly over time than the ASIB group which displayed adaptive skills that were somewhat lower, but not significantly so, from the TD group. Given that the ASIB group shares risk with the FXS group for ASD, developmental delays and adaptive skill deficits, albeit to a reduced degree of risk (Charman et al., 2016; Ozonoff et al., 2011), our study is the first to provide evidence of etiological specificity in adaptive behavior profiles across two populations at high risk for ASD. While one assumption for the lower adaptive skills in infants with FXS contrasted to the ASIB group might be attributed to the lower developmental level in the FXS group, the relationship between Mullen and Vineland composite scores in the FXS and ASIB groups varies with age ranging from .44 to .71 at the 12 and 24-month age intervals for the FXS and from .48 to .46 at the 12 and 24-month age intervals for the ASIB group. Our findings are generally consistent with a recent large-scale study (n=859) indicating that only 33% of 36-month-old ASIBS who did not meet criteria for ASD had impairments on both the VABS and MSEL (Charman et al., 2016). These data suggest that developmental delays likely contribute to the presence of adaptive skill impairments but do not fully account for their presence.
The adaptive behavior findings presented here, are highly parallel to other work that has reported significant and pervasive delays in Communication, Motor and Visual Reception domains on the Mullen Scales of Early Learning in FXS that emerged at 6 months of age (Roberts, McCary, Shinkareva, & Bailey, 2016). Likewise, the rate of growth for developmental skills was also significantly slower across all domains than the ASIB and TD comparison groups. Thus, this study contributes to the refinement of the infant phenotype of FXS and also to addressing the heterogeneity of ASD by documenting the presence of early emerging and pervasive adaptive skill deficits during infancy.
While direct comparison of these findings to previous research is challenging given the limited published work on adaptive skill development in FXS before the age of 2, our findings are consistent with the positive growth identified by studies that include a handful of children below 2 years-of-age (Dykens et al., 1996; Hahn et al., 2015; Hatton et al., 2003), suggesting that although growth rates may be slower than TD peers, infants with FXS are showing overall growth in adaptive skills beginning in infancy. This is a promising finding providing evidence of aptitude for growth early on in development in this population, even if rates are below age expectations.
Strengths and Weaknesses in Adaptive Behavior Domains
Flat profiles across adaptive behavior domains were found across both the FXS and ASIB groups at the 24-month time point. In contrast to previous research in older individuals with FXS that reports profiles of adaptive strengths and weaknesses, our study did not identify any differences in standard scores across the four domains of adaptive functioning at 24 months. The flat profile at 24 months may represent global delays across areas of adaptive functioning, consistent with findings of global delays across all areas of developmental/cognitive functioning in FXS (Roberts, Hatton, & Bailey, 2001; Roberts, McCary, Shinkareva, & Bailey, 2016; Roberts et al., 2009). Alternatively, our finding of a flat profile could reflect various developmental issues. First, given that the range of adaptive skills is more limited in younger children, the emergence of variation across domains could reflect constriction due to measurement. Second, the more varied profile reflecting relative strengths and weaknesses in adaptive skills in older children with FXS may be the result of focused intervention in a particular adaptive skill area resulting in improvements, while others remain untreated, therefore appearing to be “weaknesses” in these individuals. Third, children with FXS may gain adaptive skills at an uneven rate across development, evidencing different profiles of strengths and weaknesses at specific periods of development. Given that no differences were found in the ASIB group across domains, this may also provide evidence that differences at these early time points may be challenging to identify in risk groups with varying developmental outcomes, and that other variables may need to be explored to better understand patterns of strengths and weaknesses that may emerge with time.
Adaptive Behavior and Autism Symptomatology
Measures of autism symptom severity at both 12 and 24 months were not related to adaptive behavior functioning at 9 months of age, suggesting that early adaptive skill acquisition is generally consistent across all infants with FXS, regardless of their later presentation of autism symptomatology. Surprisingly, autism symptomatology at 12 months was not related to trajectories of adaptive development in any domain. In contrast, increasing symptom severity at 24 months was related to decreases in growth rates in the domains of Socialization, Communication and Daily Living skills. These findings are consistent with previous work that reported higher levels of autism symptomatology were related to slower adaptive skill growth (Hahn et al., 2015; Hatton et al., 2003). Trajectories of the Motor skills domain in FXS were not related to either measure of autism symptom severity.
The relationship between early motor skills and autism symptomatology in young children with FXS is complex. Recent work has identified that atypical motor behaviors measured by the Autism Observation Scale for Infants differentiate infants with FXS from ASIBs; however, 80% of infants with FXS display poor motor control at 12 months, regardless of autism outcomes at 24 months (Roberts et al., 2016) suggesting that atypicalities in this domain may be almost universal in infants with FXS. Other work has shown a strong relationship between fine motor development on the Mullen and autism symptomatology (Roberts et al., 2016; Roberts et al., 2009) in young children with FXS. This finding may be related to the imitation burden required of early fine motor tasks on the Mullen, which has been found to be a significant deficit in young children with autism and infants with FXS with elevated autism symptomatology (Rogers, Hepburn, Stackhouse, & Wehner, 2003). In contrast, the motor skills captured on the Vineland have less to do with immediate imitation; rather they measure the use of hands and fingers when completing common activities (e.g., taking items out of a container, turning pages in a book). Of note, previous work has not considered gross motor development in these relationships, which is combined with fine motor to create the Motor domain on the Vineland. Future work may focus on teasing apart the relationships between the subdomains of gross and fine motor adaptive skills, and autism symptomatology in FXS as they may help identify a specific risk phenotype in FXS.
Given that no work has been published examining adaptive behavior in infants with FXS based on a diagnostic outcome of ASD, rather than symptom severity, we presented preliminary comparisons of Vineland domain scores at 24 months based on autism diagnostic status for the FXS and ASIB groups. When participants in the FXS and ASIB groups were dichotomized based on their clinical best estimate diagnosis at 24 months, all domains with the exception of the Motor Skills domain were lower in participants with a diagnosis of ASD, although only the Communication domain met stringent significance criteria in the FXS group. These findings support the results of the longitudinal models presented in this paper that autism symptoms have a negative impact on adaptive behavior skills with means differences of almost 1 standard deviation on some domains.
In the ASIB group, the Daily Living and Adaptive Behavior Composite were lower in participants with ASD. These findings in the ASIB group are consistent with differences identified in larger samples by Estes and colleagues (Estes, Zwaigenbaum, et al., 2015), however previous work identified differences across all Vineland domains. Given the small samples in our study when ASIB participants are categorized based on ASD diagnosis, the lack of statistical findings across more domains is not surprising and we expect that they would likely parallel previous work given a larger sample.
Sex Differences in Adaptive Skill Development
The final aim of this paper was to present preliminary findings on the differences in adaptive skill development between male and female infants with FXS. While preliminary, findings suggest that females with FXS evidence higher scores in the domains of adaptive Socialization and Motor Skills at 9 months of age. Rates of growth were not different in these domains, suggesting that both sexes gained skills at a similar rate therefore maintaining the discrepancy of higher scores in females through 24 months. In direct contrast, differences in initial scores were not identified between sexes in the Communication and Daily Living domains, yet growth rates differed, resulting in a greater discrepancy with age favoring females. Across all domains, these trajectories result in higher skill acquisition in females with FXS by 24 months of age. While these results are limited by the small sample size of females with FXS in the analysis, they are consistent with previous work showing greater skills, and faster rates of growth in females with FXS (Hahn et al., 2015; Klaiman et al., 2014).
Limitations and Future Directions
While this is the first longitudinal study to examine trajectories of adaptive behavior in infants with FXS, a few limitations exist. Although using raw scores in longitudinal models is ideal when attempting to measure true change over time, weaknesses exist in their use. Raw scores on the Vineland cannot be compared across domains given differing expectations in skill acquisition across domains with age. Therefore, clinical interpretation of some of the parameter estimates reported in this paper is limited. Additionally, this study is limited by the small number of data points at 6 months in FXS and the small overall sample size of females with FXS. While multilevel modeling is robust to missing data and uneven data collection over time, time points with fewer data points to estimate from will be inherently more biased. Future research in infants with FXS should aim to collect a larger sample size at 6 months of age to more fully understand the early anchors of these trajectories, while also focusing on collecting a larger sample of females. Given the rarity of FXS and the challenge of identifying children, especially females with the disorder in early infancy, we suspect this will continue to be a limitation in FXS infant research for the foreseeable future.
Implications
Infants with FXS show deficits across all domains of adaptive functioning as early as 9 months of age with slower rates of growth in these skills across the first two years of life compared to TD and ASIB age matched peers. Therefore, interventions for young children with FXS should target adaptive skills across all domains in the first year of life, capitalizing on their measured capacity for growth. Additional monitoring and targeted treatment for adaptive skills should be given to children who are exhibiting signs of ASD by the age of 2, given the more severe adaptive skills deficits found identified in those children with high levels of autism symptomatology at 24 months. While males with FXS show more severe delays in adaptive development than females, adaptive skill assessment should be an essential component of treatment planning for all children with FXS given its importance for long-term independence.
Highlights.
Infants with fragile X syndrome show adaptive skills deficits across all domains by 9 months of age.
Trajectories of these skills are delayed, albeit growing, before the age of 2.
Elevated autism symptomatology impairs adaptive skill growth in infants with fragile X syndrome.
All domains of adaptive skills should be targeted for intervention in infants with fragile X.
Acknowledgments
We thank the families who participated in this project. This work was funded by the National Institute of Mental Health (R01MH090194, F31MH095318).
Footnotes
Conflict of Interest: There are no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bailey DB, Raspa M, Bishop E, Holiday D. No change in the age of diagnosis for fragile X syndrome: Findings from a national parent survey. Pediatrics. 2009;124(2):527–533. doi: 10.1542/peds.2008-2992. [DOI] [PubMed] [Google Scholar]
- Bryson SE, Zwaigenbaum L, McDermott C, Rombough V, Brian J. The Autism Observation Scale for Infants: scale development and reliability data. Journal of Autism and Developmental Disorders. 2008;38(4):731–8. doi: 10.1007/s10803-007-0440-y. https://doi.org/10.1007/s10803-007-0440-y. [DOI] [PubMed] [Google Scholar]
- Charman T, Young GS, Brian J, Carter A, Carver LJ, Chawarska K, et al. Zwaigenbaum L. Non-ASD outcomes at 36 months in siblings at familial risk for autism spectrum disorder (ASD): A baby siblings research consortium (BSRC) study. Autism Research. 2016:1–10. doi: 10.1002/aur.1669. https://doi.org/10.1002/aur.1669. [DOI] [PMC free article] [PubMed]
- Coffee B, Keith K, Albizua I, Malone T, Mowrey J, Sherman SL, Warren ST. Incidence of Fragile X Syndrome by Newborn Screening for Methylated FMR1 DNA. American Journal of Human Genetics. 2009;85(4):503–514. doi: 10.1016/j.ajhg.2009.09.007. https://doi.org/10.1016/j.ajhg.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen IL. Behavioral profiles of autistic and nonautistic fragile X males. Developmental Brain Dysfunction 1995 [Google Scholar]
- Dykens E, Ort S, Cohen I, Finucane B, Spiridigliozzi G, Lachiewicz A, et al. O'Connor R. Trajectories and profiles of adaptive behavior in males with fragile X syndrome: Multicenter studies. Journal of Autism and Developmental Disorders. 1996 doi: 10.1007/BF02172475. https://doi.org/10.1007/BF02172475. [DOI] [PubMed]
- Ebrahim S, Singh S, Hutchison JS, Kulkarni AV, Sananes R, Bowman KW, Parshuram CS. Adaptive Behavior, Functional Outcomes, and Quality of Life Outcomes of Children Requiring Urgent ICU Admission*. Pediatric Critical Care Medicine. 2013;14(1):10–18. doi: 10.1097/PCC.0b013e31825b64b3. https://doi.org/10.1097/PCC.0b013e31825b64b3. [DOI] [PubMed] [Google Scholar]
- Estes A, Munson J, Rogers SJ, Greenson J, Winter J, Dawson G. Long-Term Outcomes of Early Intervention in 6-Year-Old Children With Autism Spectrum Disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54(7):580–587. doi: 10.1016/j.jaac.2015.04.005. https://doi.org/10.1016/j.jaac.2015.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estes A, Zwaigenbaum L, Gu H, St John T, Paterson S, Elison JT, et al. Piven J. Behavioral, cognitive, and adaptive development in infants with autism spectrum disorder in the first 2 years of life. Journal of Neurodevelopmental Disorders. 2015;7(1):24. doi: 10.1186/s11689-015-9117-6. https://doi.org/10.1186/s11689-015-9117-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farley MA, McMahon WM, Fombonne E, Jenson WR, Miller J, Gardner M, et al. Coon H. Twenty-year outcome for individuals with autism and average or near-average cognitive abilities. Autism Research. 2009;2(2):109–118. doi: 10.1002/aur.69. https://doi.org/10.1002/aur.69. [DOI] [PubMed] [Google Scholar]
- Frolli A, Piscopo S, et al. Conson M. Developmental changes in cognitive and behavioural functioning of adolescents with fragile-X syndrome. Journal of Intellectual Disability Research. 2014 Jul;59:n/a-n/a. doi: 10.1111/jir.12165. https://doi.org/10.1111/jir.12165. [DOI] [PubMed] [Google Scholar]
- Hagerman RJ, Rivera SM, Hagerman PJ. The Fragile X Family of Disorders: A Model for Autism and Targeted Treatment. Current Pediatric Reviews. 2008;(4):40–52. [Google Scholar]
- Hahn LJ, Brady NC, Warren SF, Fleming KK. Do Children With Fragile X Syndrome Show Declines or Plateaus in Adaptive Behavior? American Journal on Intellectual and Developmental Disabilities. 2015;120(5):412–432. doi: 10.1352/1944-7558-120.5.412. https://doi.org/10.1352/1944-7558-120.5.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris SW, Hessl D, Goodlin-Jones B, Ferranti J, Bacalman S, Barbato I, et al. Hagerman RJ. Autism profiles of males with fragile X syndrome. Journal Information. 2008;113(6) doi: 10.1352/2008.113:427-438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley SL, Malick Seltzer M, Raspa M, Olmstead M, Bishop E, Bailey DB. Exploring the Adult Life of Men and Women with Fragile X Syndrome: Results From a National Survey. American Journal on Intellectual and Developmental Disabilities. 2011;116(1):316–35. doi: 10.1352/1944-7558-116.1.16. https://doi.org/10.1080/01944360903212087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatton DD, Sideris J, Skinner M, Mankowski J, Bailey DB, Roberts J, Mirrett P. Autistic Behavior in Children With Fragile X Syndrome : Prevalence, Stability, and the Impact of FMRP. American Journal of Medical Genetics. 2006;1813(140A):1804–1813. doi: 10.1002/ajmg.a.31286. https://doi.org/10.1002/ajmg.a. [DOI] [PubMed] [Google Scholar]
- Hatton DD, Wheeler AC, Skinner ML, Bailey DB, Sullivan KM, Roberts JE, et al. Clark RD. Adaptive behavior in children with fragile X syndrome. American Journal of Mental Retardation: AJMR. 2003;108(6):373–90. doi: 10.1352/0895-8017(2003)108<373:ABICWF>2.0.CO;2. https://doi.org/10.1352/0895-8017(2003)108<373:ABICWF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Huddletson LB, Visootsak J, Sherman SL. Cognitive Aspects of Fragile X syndrome. Wiley Interdisciplinary Reviews: Cognitive Science. 2014;5(4):501–508. doi: 10.1002/wcs.1296. https://doi.org/10.1126/scisignal.2001449.Engineering. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hustyi KM, Hall SS, Quintin EM, Chromik LC, Lightbody AA, Reiss AL. The Relationship Between Autistic Symptomatology and Independent Living Skills in Adolescents and Young Adults with Fragile X Syndrome. Journal of Autism and Developmental Disorders. 2014;45(6):1836–1844. doi: 10.1007/s10803-014-2342-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanne SM, Gerber AJ, Quirmbach LM, Sparrow SS, Cicchetti DV, Saulnier Ca. The role of adaptive behavior in autism spectrum disorders: implications for functional outcome. Journal of Autism and Developmental Disorders. 2011;41(8):1007–18. doi: 10.1007/s10803-010-1126-4. https://doi.org/10.1007/s10803-010-1126-4. [DOI] [PubMed] [Google Scholar]
- Klaiman C, Quintin EM, Jo B, Lightbody Aa, Hazlett HC, Piven J, et al. Reiss AL. Longitudinal profiles of adaptive behavior in fragile X syndrome. Pediatrics. 2014;134(2):315–24. doi: 10.1542/peds.2013-3990. https://doi.org/10.1542/peds.2013-3990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landa RJ, Gross AL, Stuart Ea, Bauman M. Latent class analysis of early developmental trajectory in baby siblings of children with autism. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2012;53(9):986–96. doi: 10.1111/j.1469-7610.2012.02558.x. https://doi.org/10.1111/j.1469-7610.2012.02558.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozonoff S, Young GS, Belding A, Hill M, Hill A, Hutman T, et al. Iosif AM. The Broader Autism Phenotype in Infancy: When Does It Emerge? - Accepted Manuscript. Journal of the American Academy of Child & Adolescent Psychiatry - Articles in Press. 2014;53(4):398–407. doi: 10.1016/j.jaac.2013.12.020. https://doi.org/10.1016/j.jaac.2013.12.020.The. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozonoff S, Young GS, Carter A, Messinger D, Yirmiya N, Zwaigenbaum L, et al. Stone WL. Recurrence risk for autism spectrum disorders: a Baby Siblings Research Consortium study. Pediatrics. 2011;128(3):e488–95. doi: 10.1542/peds.2010-2825. https://doi.org/10.1542/peds.2010-2825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JE, Hatton DD, Bailey DB. Development and Behavior of Male Toddlers With Fragile X Syndrome. Journal of Early Intervention. 2001;24(3):207–223. https://doi.org/10.1177/10538151010240030601. [Google Scholar]
- Roberts JE, Mankowski JB, Sideris J, Goldman BD, Hatton DD, Mirrett PL, et al. Bailey DB. Trajectories and predictors of the development of very young boys with fragile X syndrome. Journal of Pediatric Psychology. 2009;34(8):827–36. doi: 10.1093/jpepsy/jsn129. https://doi.org/10.1093/jpepsy/jsn129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JE, McCary LM, Shinkareva SV, Bailey DB. Infant Development in Fragile X Syndrome: Cross-Syndrome Comparisons. Journal of Autism and Developmental Disorders. 2016;46(6):1–12. doi: 10.1007/s10803-016-2737-1. https://doi.org/10.1007/s10803-016-2737-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts JE, Tonnsen BL, McCary LM, Caravella KE, et al. Shinkareva SV. Brief Report: Autism Symptoms in Infants with Fragile X Syndrome. Journal of Autism and Developmental Disorders. 2016:1–8. doi: 10.1007/s10803-016-2903-5. https://doi.org/10.1007/s10803-016-2903-5. [DOI] [PMC free article] [PubMed]
- Rogers SJ, Hepburn SL, Stackhouse T, Wehner E. Imitation performance in toddlers with autism and those with other developmental disorders. Journal of Child Psychology and Psychiatry. 2003;44(5):763–781. doi: 10.1111/1469-7610.00162. https://doi.org/10.1111/1469-7610.00162. [DOI] [PubMed] [Google Scholar]
- Rogers SJ, Wehner EA, Hagerman R. The Behavioral Phenotype in Fragile X : Symptoms of Autism in Very Young Children with Fragile X Syndrome, Idiopathic Autism, and Other Developmental Disorders. Developmetnal and Behavioral Pediatrics. 2001;22(6):409–417. doi: 10.1097/00004703-200112000-00008. [DOI] [PubMed] [Google Scholar]
- Tassé MJ, Schalock RL, Balboni G, Bersani H, Borthwick-Duffy SA, Spreat S, et al. Zhang D. The construct of adaptive behavior: Its conceptualization, measurement, and use in the field of intellectual disability. American Journal on Intellectual and Developmental Disabilities. 2012;117(4):291–303. doi: 10.1352/1944-7558-117.4.291. https://doi.org/10.1352/1944-7558-117.4.291. [DOI] [PubMed] [Google Scholar]
- Toth K, Dawson G, Meltzoff AN, Greenson J, Fein D. Early Social, Imitation, Play, and Language Abilities of Young Non- Autistic Siblings of Children with Autism. Journal of Autism and Developmental Disorders. 2007;37(1):145–147. doi: 10.1007/s10803-006-0336-2. https://doi.org/10.1016/j.micinf.2011.07.011.Innate. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay KN, Richer L, Lachance L, Côté A. Psychopathological manifestations of children with intellectual disabilities according to their cognitive and adaptive behavior profile. Research in Developmental Disabilities. 2010;31(1):57–69. doi: 10.1016/j.ridd.2009.07.016. [DOI] [PubMed] [Google Scholar]


