Abstract
Study Objectives:
Continuous positive airway pressure (CPAP) therapy is considered the front-line treatment for moderate-severe obstructive sleep apnea (OSA). However, nonuse rates are very high, such that adherence to CPAP has become a major concern. Although the literature on CPAP use is vast, further research is required to understand patients' experiences of CPAP use and nonuse. This is the goal of this study.
Methods:
This study draws on in-depth interviews with 61 Jewish-Israeli patients with OSA who received a recommendation to use a CPAP device. The sample includes both patients who started using CPAP devices as well as patients who rejected this course of treatment. It follows principles of constructivist-grounded theory in both sampling and analysis.
Results:
The study shows that regardless of patients' status of adherence, their attitudes toward CPAP devices are characterized by ambivalence. Users of CPAP expressed ambivalent adherence, pondering whether they should stop using the device; and patients who rejected the CPAP expressed ambivalent nonadherence, wondering whether they should give the CPAP another chance. This study identifies the experiences involved in using, as well as not using, CPAP devices that produce patients' ambivalence.
Conclusions:
Both adherence and nonadherence to CPAP are dynamic processes that are characterized by patients' ambivalence and contingent upon diverse factors. These findings have practical implications as they suggest that all patients, regardless of their initial adherence status, would benefit from a close follow-up.
Citation:
Zarhin D, Oksenberg A. Ambivalent adherence and nonadherence to continuous positive airway pressure devices: a qualitative study. J Clin Sleep Med. 2017;13(12):1375–1384.
Keywords: adherence, ambivalence, compliance, continuous positive airway pressure devices/CPAP therapy, obstructive sleep apnea, qualitative research methods
INTRODUCTION
Obstructive sleep apnea (OSA) is a prevalent chronic condition characterized by intermittent partial or complete collapse of the upper airway during sleep. Symptoms may include loud snoring, snorting, gasping, choking, frequent awakenings, insomnia, and excessive daytime sleepiness. In addition to these symptoms, patients with untreated moderate to severe OSA may suffer from long-term harmful health consequences.1 The treatment of choice for patients with moderate to severe OSA is continuous positive airway pressure (CPAP), which has become widespread since its introduction in 1981.2,3 There is much evidence that CPAP therapy is the most effective treatment option, decreasing breathing disturbance, alleviating symptoms, and restoring impaired daytime function.4,5 Some research suggests that CPAP reduces cardiovascular mortality and morbidity, but highlights the importance of adherence in achieving such results.6,7 Furthermore, compared to some of the other therapeutic alternatives such as oral devices or diverse surgeries, CPAP treatment has a significant advantage because it is both reversible, and can be provided to patients for a trial period with no out-of-pocket expense. Nonetheless, CPAP adherence, usually defined as at least 4 hours of nightly use, is quite low, with nonadherence often reaching 71%8 and even 83% of patients.9
BRIEF SUMMARY
Current Knowledge/Study Rationale: Further research is needed to understand patients' experiences with CPAP use and nonuse. This study contributes to the literature by drawing on in-depth interviews with Jewish-Israeli patients with OSA to examine patients' adherence and nonadherence to CPAP use during the first 18 months after diagnosis.
Study Impact: This study shows that both adherence and nonadherence to CPAP are dynamic processes characterized by patients' ambivalence. Understanding patients' perspectives will help improve the practice of sleep medicine, as it will allow medical practitioners to address patients' concerns directly, and offer useful guidance and assistance. This study highlights the importance of establishing a close long-term follow-up mechanism of all patients regardless of their initial status of CPAP adherence.
Hence, clinicians and researchers make efforts to understand as well as improve CPAP adherence, which is recognized as a multifactorial complex clinical issue. Although the literature on CPAP use is vast, further research is needed to understand patients' experience of CPAP use and nonuse. The majority of studies on CPAP use are quantitative, examining reasons for adherence or for abandoning use, or exploring the effect of various interventions. In these studies, the use or nonuse of CPAP emerges as an outcome of various variables, such as CPAP side effects (eg, mask leaks, dry throat, blocked nose, and uncomfortable mask pressure), personal or professional support, and perceived beneficial effects.10–14 Most of these studies use predetermined categories that have not been derived from users' accounts, thereby imposing certain responses on participants, and limiting capture of all aspects of their experiences. In contrast, qualitative research methods allow for the exploration of patients' experiences inductively, letting patients themselves conceptualize how they see and feel about using CPAP. Existing qualitative research focuses primarily on factors that either increase or decrease willingness to use CPAP as well as ways to promote CPAP use,11,15,16 difficulties upon CPAP initiation,17–19 or perceptions of OSA and beliefs about treatment.20,21 Thus, some important components in patients' experiences and processes of adherence and nonadherence do remain underexplored and require further clarification. This study sheds light on these processes by drawing on in-depth interviews with patients with OSA who received a recommendation to use CPAP devices. Additionally, whereas most qualitative studies examined adherence among patients who started using CPAP devices, this study also includes patients who rejected this course of treatment.
METHODS
There is increasing recognition of the value of qualitative research methods in sleep medicine, as these methods allow researchers to understand patients' point of view.11,22 This study contributes to this growing literature by drawing on the sociological perspective of symbolic interactionism (SI), and by using grounded theory methods. According to the SI approach, people's actions are guided by the socially created meanings that they impart to them.23 According to this approach, to understand patients' actions, researchers must explore the meanings patients ascribe to these actions, and the processes through which these meanings are created. SI differs from positivistic perspectives in that it is an interpretive perspective that allows for the agency in human behavior and supports a methodology to study this behavior without demanding that it be definitively explained or predicted. Thus, rather than relying on quantitatively derived data, symbolic interactionists primarily collect and analyze qualitative data from people's experiences.24 An important qualitative tradition that emerged from SI is grounded theory, developed originally by Barney Glaser and Anselm Strauss.25 This inductive method was designed to key in on the social processes through which meaning is derived.26 Because we are interested in understanding the processes of adherence and nonadherence to CPAP use, we chose constructivist grounded theory method to guide both the collection and analysis of the qualitative data.26 Constructivist grounded theory sees knowledge as socially produced and acknowledges multiple standpoints of both the research participants and the researcher. This approach also takes a reflexive stance toward the research (ie, it requires that researchers continuously reflect on their decisions and actions throughout the research process, maintaining awareness of how they may have influenced their research project).27 Reflexivity also allows for the establishment of trustworthiness, which is the central criterion used to judge the quality of qualitative research.28,29 As we clarify in the next paragraphs, additional strategies we used to ensure trustworthiness include peer debriefing and prolonged engagement in the field, which involved conducting a large number of lengthy and detailed interviews over an extended period of time. This prolonged engagement allowed for the establishment of rapport with respondents and the achievement of theoretical saturation, as well as the provision of thick description that is deep, dense, and detailed in a way that contributes to reliability.28
Data Collection
This study is part of a large qualitative research project that explored the experiences of patients diagnosed with or suspected of having OSA. The parent study examined various topics including patients' management of symptoms, their experiences of the diagnosis of OSA (for those who received such a diagnosis), reasons for delaying and for seeking care, and views and use of treatment options. Overall interview response rate for this study was 75% (78 out of 104). However, in the current study, we include the accounts of the 61 patients who received both an OSA diagnosis and a recommendation to use a CPAP device.
We commenced recruitment of interviewees after receiving ethical approval from both the Institutional Review Board at Brandeis University (#10059) and the Helsinki Committee at the hospital (#0019-09LOE-1). Most of the respondents (59 out of 61) were recruited through a sleep center located in the Tel Aviv metropolitan area, whereas the other 2 respondents were contacted through social networks. In January 2010 and from October 2010 to January 2011, the first author conducted face-to-face individual interviews at various locations including coffee shops, the sleep center, and respondents' homes or workplaces, based on the preferences of the interviewees.
Sampling was done in 2 stages. The first stage, based on a purposeful sampling design, aimed to include Israeli patients with OSA and a wide range of sociodemographic backgrounds, such as sex, age, family status, and occupation.30 We deemed these variables analytically important, and therefore intended to make sure the sample was heterogeneous with respect to these variables. Nevertheless, to facilitate saturation, we had to make sure the sample was homogenous in other respects.31 Thus, we excluded adults older than 66 years because some research has indicated that sleep apnea in the elderly may be a different “disease entity,”32,33 which requires a separate study. We initially intended to include non-Jewish patients as well as nonheterosexual ones. However, this proved difficult as the sleep center does not keep records of either religion or sexual orientation, and we could not ask patients to answer personal questions over the phone (before presenting them with a consent form). All patients turned out to be heterosexual and Jewish, and therefore the sample was homogenous with respect to religion and sexual orientation (see endnote A). The second stage of sampling included theoretical sampling, which aimed to seek and collect relevant data to elaborate and refine categories in the emerging theory.26 For example, the categories of ambivalent adherence and ambivalent nonadherence have emerged from the first set of interviews, but the sample included few individuals who continued to use a CPAP device, such that the category of ambivalent adherence and its properties needed further refinement. We therefore continued conducting interviews, aiming to find patients who were still using their CPAP devices. Data collection continued until theoretical saturation was reached, meaning until the data derived provided detailed and thick description, properties of categories were developed, and additional interviews did not generate novel insights about the concepts that had emerged or produce a change to the codebook.31,34,35 Thick description provided an opportunity for seeking replication in the data in a way that contributed to reliability.36
All respondents were asked a specific set of questions about their reasons for arriving at the sleep center, their experiences at the sleep center (from their meeting with a sleep specialist through the diagnostic test to their trial night of CPAP), and their thoughts about and experiences with the CPAP device (at the laboratory, during the trial period, and after purchase) (see interview guide in the supplemental material). In addition, the interviewer probed and asked supplementary questions to sharpen and deepen participants' responses. Following grounded theory principles, the first author gathered and analyzed data simultaneously, identifying categories, which were investigated further by appending questions to the interview guide.
Prior to each interview, the participants signed a consent form to affirm they understood the intent of the research and the voluntary nature of the interview. The interviews lasted between 40 minutes and 2.5 hours, with an average of 76.44 minutes. These interviews were intentionally long to establish trust and to allow respondents to provide rich and detailed data, thereby facilitating thick description.36 All interviews, except for one, were conducted in Hebrew. They were tape-recorded, with participants' consent, and field notes were written soon after each interview. Throughout this article, pseudonyms are used to protect the anonymity of respondents. Status of adherence, sex, and age are mentioned in parentheses following respondents' pseudonyms.
Participants
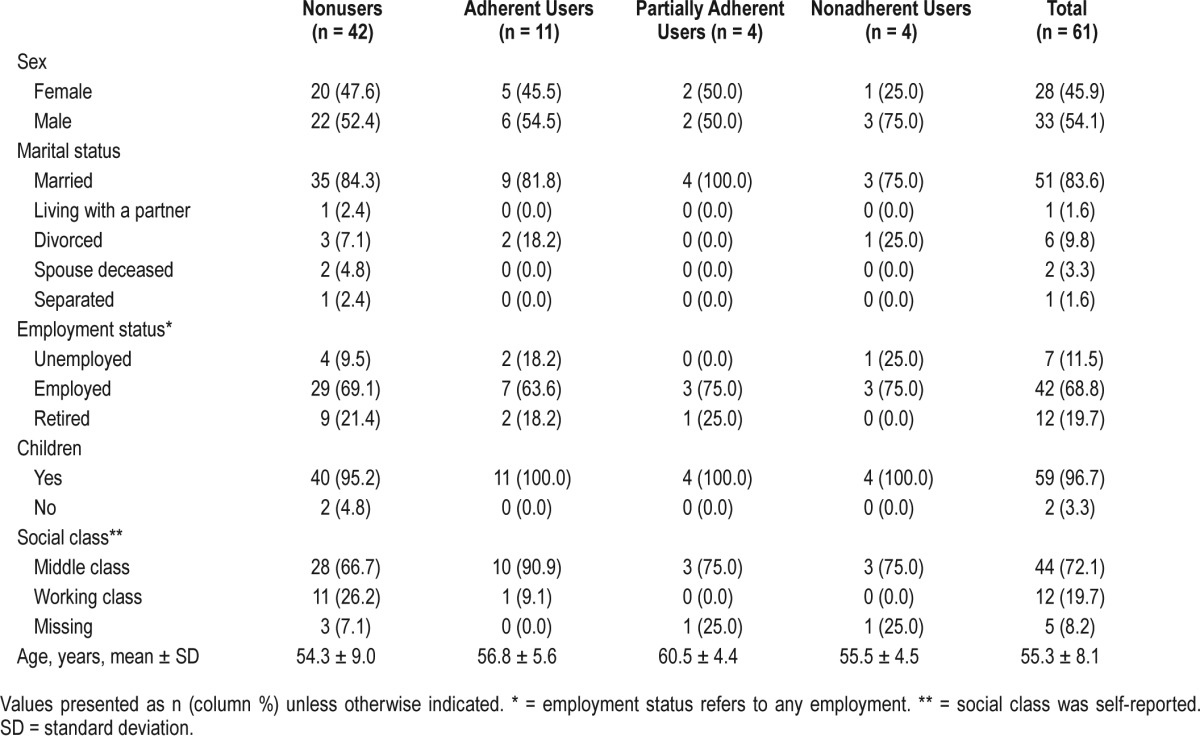
The sample comprises 61 Jewish-Israeli patients (28 women and 33 men) who received an OSA diagnosis sometime in the 18 months prior to the interview (see endnote B). This period of time is close enough to diagnosis to allow for good recollection of what happened since then and far enough to examine what happens to adherence. Apnea-hypopnea index (AHI) was available for 60 respondents. AHI average was 48.6 ± 28 (range 13–129.4). Scores of Epworth Sleepiness Scale were available for only 48 of the respondents, with an average of 9.6 ± 5.3 (range 0–23). Most of the participants (n = 51) were married at the time of the interview and 1 respondent was living with a partner. The rest were either divorced (n = 6), separated (n = 1), or widowers (n = 2). Except for 2 men, all respondents had children. Although most participants were employed (n = 42), approximately one-third were either unemployed (n = 7) or retired (n = 12). The majority of respondents reported that they belong to the middle class (n = 44), but a few (n = 12) said they belong to the working class. Information about social class is missing for 5 of the respondents. Participants' ages ranged from 30 to 66 years, with a mean age of 53.1 among men and 57.7 among women. The intention here was not to comprise a “representative” sample, as this qualitative study does not presume to be generalizable to all patients with OSA. Rather, the aim was to create a sample that is driven by theoretical concerns37 in order to shed some light on underexplored aspects of patients' processes of adherence and nonadherence to CPAP use.
Analysis
The interviews were transcribed verbatim and uploaded onto ATLAS.ti. (Scientific Software Development GmbH, Berlin, Germany), a program for qualitative data analysis, where the interviews were coded and analyzed based on constructivist grounded theory principles, including systematic conceptualization, constant comparisons, coding, and memo-writing.26 The first author conducted the comparison process through an elaborate and careful process of coding and grouping the codes into concepts in a hierarchical manner.26,38 Specifically, coding comprised 3 stages. During the initial coding stage, the first author used open coding, giving temporary labels to phrases and incidents in the interviews to capture their meanings and content, and exploring all the theoretical possibilities in the data. The second stage of coding included focused coding in which the first author used codes that were more frequent and significant. Codes that endured this process were densified into categories, moving from a descriptive level to a more abstract theoretical level. In the third stage, the author moved on to theoretical coding in which she specified how the substantive codes related to one another, and then arranged the concepts that emerged into theoretical propositions.
As part of the constant comparison method of analysis, the first author made comparisons at each level of analytic work to establish analytic distinctions. Specifically, comparisons were made between data, codes, and categories, as well as concepts both within and across interviews, searching for similarities and differences. All the while, the first author wrote memos to detail these comparisons further, and to reflect on the analytic process. In addition, the first and second author met for peer debriefing once a week during which they discussed excerpts from interviews, the codes attached to these excerpts, as well as the emerging categories and concepts. These discussions as well as additional consults with other colleagues helped ensure reliability and allowed for further refinement of the coding and analysis, additional reflection, transparency, and a systematic approach for the development of the categories and the emerging theory. The sections that follow depict this theory and the data in which it is grounded.
RESULTS
Respondents arrived at this sleep center (see endnote C) looking for and hoping to obtain a satisfactory medical solution. They experienced diverse symptoms with varying degrees of severity, but all of them indicated that their symptoms had some effect on both their daily and nightly lives. Respondents' snoring interrupted the sleep of bed partners as well as other household members in a way that deteriorated the quality of filial relationships.39 Daytime somnolence and fatigue impaired respondents' performance at work and home, as respondents struggled to fulfill their various duties. Tired and sleepy respondents also became more irritable and impatient, finding it difficult to interact with others. Three respondents even fell asleep at the wheel and were involved in car crashes due to drowsy driving.
Yet, all but two respondents were disappointed to learn that the recommended treatment was CPAP therapy, citing the following reasons: Respondents said they had hoped for a solution that would “cure” their OSA, rather than a device they would have to use nightly for the rest of their lives. They also criticized the discomfort involved in using the device as well as its unaesthetic appearance, and expressed concern about travel restrictions. In addition, respondents argued the device had affected their self-perception, as it made them feel “disabled.”40 Furthermore, approximately one-third of the respondents were skeptical about the accuracy of their own OSA diagnosis.41 Interviewees mentioned that the out-of-pocket payment for CPAP devices was quite large, but no respondent saw the financial expense as a reason, in and of itself, not to purchase the device.
For these reasons, some respondents chose not to adhere to this course of treatment. The group of nonusers consists of 42 respondents who either refused to try the device or rejected it after trying it for 1 night at the sleep center or for a few days at home. The group of users, which includes 19 participants, can be divided into 3 subgroups according to their levels of adherence. The first subgroup, termed “adherent users,” includes 11 respondents who purchased the device and used it on a nightly basis. The second subgroup, “partially adherent users” includes 4 respondents who despite purchasing the device used it only occasionally. The third group includes 4 “nonadherent users,” who purchased the device and used it on a nightly basis for a period of time and then decided to stop using it altogether. No sociodemographic differences were found between these subgroups (see Table 1).
Table 1.
Sociodemographic characteristics of participants.
This variety indicates that even individuals who purchased the device and used it for a while did not necessarily continue to adhere to its use. Therefore, initial adherence is not necessarily indicative of long-term use. Yet, the group of adherent users includes 2 men who had previously rejected CPAP, but adhered to its use after receiving a diagnosis again years later. This finding indicates that nonusers may change their minds about CPAP as well (see endnote D). As the following discussion will show, patients' views and use or nonuse of CPAP devices are characterized by ongoing ambivalence, such that their level of adherence and nonadherence keeps fluctuating.
Ambivalent Adherence: Users' Experiences
Feeling uncertain about the role of CPAP in improving symptoms and quality of life
The 11 adherent CPAP users were generally pleased with the device's effects on their daytime and nighttime symptoms. They felt more rested and energetic during the day and experienced fewer awakenings at night. Respondents addressed the improvement in symptoms and quality of life as one of the major benefits of the device. However, they did not credit the improvement in their condition solely to the device. Rather, they kept pondering whether other factors, such as reduced stress due to retirement or reduction in workload, as well as weight loss and exercise, contributed to their recuperation. In other words, in spite of the benefits they obtained, they were ambivalent about the exact role of CPAP in what they called their “recovery” or “improvement.”
Experiencing difficulties with CPAP use, expecting a cure
With one exception, all of the patients who used CPAP on a regular basis also expressed substantial reservations and resentment toward this device. They criticized medicine for not improving PAP therapy, arguing that developers should attempt to make the device “more elegant” and “user friendly.” They were also highly critical of “medicine's failure” to provide them with better alternative solutions, or better yet, a cure for OSA. With the exception of 1 patient, all respondents appreciated and respected the sleep specialists they saw, mentioning both their competency and compassion as factors that contributed to their motivation to try the CPAP. Still, they contended that the lack of better alternative treatments highlighted the incompetence of the medical profession. Thus, even adherent users expressed ambivalence toward their CPAP device, with all except 1 being only partially satisfied.
Comparing home to hospital
Participants also discussed the differences in their experiences of using CPAP at the sleep center versus their home setting. In the home setting, they began experiencing problems and challenges they had not necessarily encountered at the center. At home, respondents do not necessarily assume the patient role. Instead, social expectations demand that they return to their regular role obligations as caregivers, workers, etc. However, as respondents attested, wearing “an external,” “ugly” and uncomfortable device is commensurate with people's expectations for being at a hospital, a setting that requires individuals to relinquish some control over their bodies and subject themselves to inspection and bodily manipulation. In their own homes, however, individuals expect to maintain bodily control. Even respondents who felt very refreshed after their trial night with CPAP said this experience did not recur at home. Their nights at home were not as “peaceful” and “restful” compared to their trial night. Rather, it was filled with additional struggles and difficulties due to the CPAP. Thus, although users expressed gratitude for the “healing prospects” of the CPAP, they resented how it made them feel physically and emotionally. Avner explained:
“ Maybe it [the device] does not bother everyone, but it does bother me. I cannot tell you that I am happy with it. I cannot tell you that I enjoy going to bed, putting this on, and sleeping with this. That's not how I feel. I try to be tired first. Sometimes I fall half-asleep and only then do I put it on and actually fall asleep. I am not happy with it. It is good for me; it saved me. But, on the other hand, it's not. If you take a scale of 1 to 100, I would give it 85.” (male adherent user, 63 years old)
Avner thought the CPAP “saved” him, as it eliminated his daytime sleepiness and fatigue, but he was still unhappy with the device. Avner repeatedly mentioned how he wished he could stop using this device and replace it with another “solution.” He adhered to the recommended therapy, but did it half-heartedly.
As with Avner, Rina (female adherent user, 55 years old) reflected frequently on how refreshing her trial night at the sleep unit was. Nonetheless, she emphasized that she continued to experience persistent difficulties, which often enhanced her inner resistance to using the device. She explained how she tried to overcome this resistance and to motivate herself to wear the mask at night by thinking about the benefits of the device. Throughout her interview, Rina discussed the downsides and upsides of the CPAP simultaneously, describing her own ambivalent adherence:
Rina: It really has a positive effect. It's just a shame that it is not aesthetic. Then again, you can't have it all.
Interviewer: You say it bothers you, not your husband--
Rina: Well, he never said anything. He doesn't complain. I try to, look, I wake up at around 4:00, 4:30 AM and I don't put it back on. I usually put it only when we go to sleep, when it's dark. I do it quietly. It's not like he doesn't see me, but I avoid putting it back on for my own good feeling.
Five additional users said that they wore the mask in darkened rooms and added that they did not put the CPAP mask back on if they woke up in the middle of the night (usually to urinate). As with Rina, these participants used the device in these particular ways both to minimize chances that their partners would see them with the mask and because it allowed them to get a few hours in which they were “free” of this machinery. Three respondents also did not wear the CPAP masks near their grandchildren to avoid scaring them. Hence, if their grandchildren slept over (which was a frequent occurrence at their household), respondents either closed their own bedroom doors or did not wear their masks at all. Additionally, all but 2 adherent users refrained from taking their CPAP with them on trips and long travels. Although patients knew they were supposed to use the device every night, they sometimes avoided doing so. Thus, as these examples clarify, even the adherence of adherent users is incomplete and expresses the ambivalence surrounding CPAP use.
Reducing adherence
Four respondents stopped using the device (nonadherent users) and 4 more started using it only occasionally (partially adherent users). The partially adherent users insinuated they might stop using the device altogether. Two of these respondents grappled with the question of adherence every evening, wondering whether they should use the CPAP or not, whereas the other 2 respondents reached an agreement with their spouses that they use it only on specific nights. Yoram (male partially adherent user, 55 years old), for example, stopped using the device on a nightly basis after returning from a long trip abroad during which he did not use the CPAP. He kept the device by his bed and used it on an “SOS basis” on nights in which his wife said she could not tolerate his snoring any longer. Five of the nonadherent as well as partially adherent users experienced some recurrence of symptoms, but at the time of the interview, they nonetheless did not consider returning to nightly use of CPAP. They explained that they had experienced difficulties with the device, as it interrupted their sleep and breathing, as well as their self-perception as attractive and independent individuals, and therefore decided to reduce or to stop CPAP use. Nonusers mentioned similar difficulties as reasons for rejecting CPAP use.
Ambivalent Nonadherence: Nonusers' Experiences
Experiencing worsened symptoms, reconsidering potential benefits from CPAP use
Of the 42 nonusers, 35 had scruples or second thoughts about not using the CPAP. Those who had not tried CPAP therapy said they often wondered whether they should try the device, whereas those who tried it mulled over whether they should make greater efforts to adjust to it, expressing ambivalence toward their decision. Erica (female nonuser, 65 years old), for example, thought that her adverse symptoms were getting worse and contemplated trying the CPAP:
“ Maybe I'll sleep better with it. Maybe the 4 hours I do sleep will be of better quality. But again, I have a problem with all of this construction [referring to the CPAP mask]. I don't know what to do. I don't know. I am still thinking about it. My husband said, ‘Do what you think is best. I don't mind. Maybe it'll be good for you; why wouldn't you try it?’”
The thought of sleeping while being attached to a device deterred Erica. Yet, she began to ponder the potential benefits of CPAP, wondering if it could improve the quality of her sleep. Her husband encouraged her to try the device; her resistance to doing so was self-induced. Similarly, respondents said their family members, and especially their partners, had frequently requested that they “do something” to treat their OSA and encouraged CPAP use. Erica said the thought of trying the CPAP arose nightly, whenever she woke up due to her repeated awakenings, feeling bored and alone. As with Erica, other respondents remarked that experiencing OSA symptoms, including fatigue and sleepiness, interrupted sleep, choking episodes, and even snoring, reminded them of the need to “do something” about their OSA.
Meeting adherent CPAP users
Another factor that made respondents reassess CPAP use was meeting adherent CPAP users:
“ I have a friend who sleeps with it [a CPAP device] […] He enjoys sleeping with the device; he really does. It is good for him and he sleeps well with it. Now, it has reached a point that when they go on trips, he takes it with him. He does not separate from it. It [the thought of trying CPAP] comes up occasionally. It comes up that maybe I should talk to my doctor and we should think about which kind of CPAP I should get.”
Seeing the benefits her friend gained by adhering to CPAP use reminded Erica of this treatment option and made her reconsider her decision to reject the device. Similarly, respondents mentioned the effect of meeting other CPAP users or nonusers. The data indicate that people who know CPAP users that are pleased with the device and use it regularly are more likely to try the device whereas people who only know nonusers are less likely to try it. Still, as the previous section described, although knowing adherent CPAP users may influence people's willingness to try PAP therapy, it does not ensure long-term adherence.
Finding other treatment options to be unsatisfactory
Forty respondents said they rejected the CPAP because they wanted to exhaust other treatment options first. As Ana (female nonuser, 37 years old) explained:
“ I said I would try other options first and then we'll see. If I have no choice, I will go for the CPAP, but… I really don't want to sleep with an oxygen mask my whole life.”
Indeed, these nonusers tried alternative treatment options, including dental appliances, various types of surgeries, laser therapy, positional therapy, exercise, and weight loss, as well as breathing workshops (see endnote E). Although 8 respondents found some relief by using these alternative options, the rest said that at the time of the interview, they did not yet find an effective treatment. These respondents stated that “the next step” would be to try (or retry) the CPAP. As Yoel (male nonuser, 36 years old) stated:
“ Look, the next step would be trying the CPAP. There will be no choice at some point because dragging it on and on like that is [impossible].”
Hence, for patients who tried other treatment options and found them to be unsatisfactory, the CPAP became a viable alternative again.
DISCUSSION
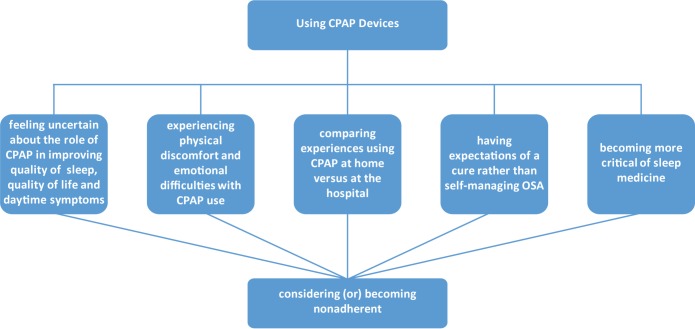
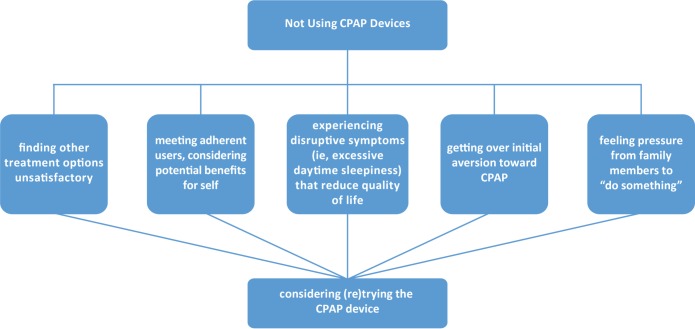
Although the literature on compliance/adherence to CPAP use is immense, a comparatively small body of work uses qualitative methods to understand patients' experiences of CPAP use and nonuse. This study contributes to this literature by drawing on in-depth interviews with OSA patients and highlighting the processual, mutable, and ambiguous nature of CPAP adherence and nonadherence. This paper shows that using the CPAP device entails experiences that produce ambivalence toward adherence, whereas not using it entails other experiences that produce ambivalence toward nonadherence (see Figure 1 and Figure 2). Such ambivalence is hard to capture in quantitative studies that use predetermined categories. Specifically, respondents who used CPAP exhibited ambivalent adherence, considering whether they should stop using the device and try other treatment options instead. Indeed, some patients who used to adhere to CPAP use started using the device only occasionally, and others abandoned the CPAP device altogether. Nonusers expressed ambivalent nonadherence as they kept pondering whether they should try the device or put greater efforts into adjusting to it. These respondents continued to deliberate whether they could and should do something different to mend their condition. As this research indicates, both adherence and nonadherence to CPAP are therefore dynamic processes rather than fixed statuses. These processes involve changes and are contingent upon diverse factors.
Figure 1. Ambivalent adherence.
CPAP = continuous positive airway pressure, OSA = obstructive sleep apnea.
Figure 2. Ambivalent nonadherence.
CPAP = continuous positive airway pressure.
Thus, whereas some studies have examined adherence in the first few weeks or months after initiation, contending that adherence is established within this time period,10,42 this study suggests that initial adherence or nonadherence may not necessarily be indicative of long-term use or nonuse. Indeed, studies that have used a longitudinal approach, tracking patients' long-term adherence, have found that patients may start using their device only intermittently or even stop using it.43,44 Still, these studies do not provide in-depth analysis of why such changes in the status of adherence occur.
Patients' accounts in this research shed light on this topic. As the data show, patients who purchased and used the CPAP experienced physical and emotional difficulties and began to consider discontinuing its use. Even if patients felt improvement in symptoms and quality of life, they did not necessarily ascribe it to the use of CPAP. Having to self-manage their condition displeased them as well, as they were hoping for a cure, or at least a better solution to their OSA. Bringing a “hospital-like device” into their home was not an easy experience for them. As a result, their criticism of sleep medicine only enhanced.
Yet, patients who did not use the CPAP reconsidered their decision as well. Many of the patients who rejected the treatment did so because they wanted to try other solutions first. If they found those to be ineffective, they began to consider trying or retrying the CPAP. For other patients, symptoms persisted or intensified, leading to the deterioration of their quality of life and functioning, such that they began to think that intervention was necessary. Furthermore, in some cases, family members' pressure to “do something” motivated nonusers to try or retry the device whereas in other cases patients' social networks changed and expanded, such that they encountered CPAP users who were satisfied with their device, and began to consider the potential benefits they could gain from using the device as well.
Limitations
Whereas many studies measure CPAP use by downloading the data from patients' CPAP machines, this study relies on patients' accounts of CPAP use time. This method poses some limitations, as patients' reports may differ from the actual CPAP run time, as measured by hidden monitors.45 Therefore, it is possible that patients would have been classified differently if such objective measures were available and that the comparison between objective versus subjective data would have provided interesting results that have therapeutic implications. Still, these limitations do not detract from the conclusions or significance of this research, as this study aims to investigate patients' experiences inductively, and explore their own point of view, a feat that has been called for46 and is required in order to reach a more thorough understanding of patients' experiences of adherence and nonadherence to CPAP. To achieve this aim, patients' understanding of how (and how much) they use the CPAP is more important than their actual use time. Additionally, since this study was conducted in patients younger than 66 years, its findings and implications may be relevant primarily to patients in midlife. Nonetheless, because the mean age of CPAP users in most studies is between 40 to 50 years,47 our study may apply to most CPAP users.
Implications for Clinical Practice and Research
Understanding patients' perspectives will help improve the practice of sleep medicine, as it will allow medical practitioners to address patients' concerns directly, and offer useful guidance and assistance. The findings of this paper suggest that sleep centers should implement a long-term follow-up mechanism. Currently, there is no consensus regarding the modality or the frequency of long-term follow-up48 and in many places, including in most Israeli sleep centers, there is no follow-up mechanism. Nonetheless, this paper highlights the need in a long-term follow-up of all patients. As the study shows, patients who exhibit good adherence at the beginning may abandon treatment after a period of time. Sleep clinicians should follow up to check whether patients' commitment to using the device has wavered or whether they are experiencing difficulties that could be remedied. Such instrumental and emotional support could assist patients and prevent them from discontinuing use of this device. Simultaneously, sleep clinicians should bear in mind that patients who rejected the CPAP or stopped using it after a short period may change their minds, too. Hence, it is worthwhile to follow up with these patients as well to determine whether they have reached a point in which they would be open to trying or retrying CPAP.
By showing that adherence and nonadherence to CPAP are frequently accompanied by dynamic ambivalence, this paper sends a clear message to sleep clinicians: “Be close to your patients.” Therefore, a mechanism that will ensure close contact with the patient is imperative. This message is simple but significant and has clinical implications. The specific mechanism chosen should be developed and adapted to the realities of the particular context in which it is implemented. Further research should assess which mechanism is optimal to provide detailed recommendations for its parameters. For some sleep centers, the new available telemedicine platform could be the ideal operative answer to keeping patients as close as possible. Yet, in other centers, a follow-up mechanism can include setting up follow-up meetings with patients or, alternatively, follow-up phone calls. In any case, the mechanism should also include a well-organized and effective assessment of the patient's data for a long-term evaluation. We recommend a close follow-up of all patients in the first month and then additional follow-ups at least every 3 months.
Patients who arrive at their follow-up meetings will be able to share their experiences and raise issues that bother them. During these meetings, practitioners can address these issues and try to assist patients in dealing with them, but they can also reiterate the importance of an adequate use of CPAP, thereby reinvigorating patients' commitment to using the device. Additionally, practitioners can inform patients about any technological improvement in CPAP machines, masks, and accessories that could ease their difficulties. If the patients' refusal seems to be non-negotiable, practitioners may suggest other applicable alternatives, such as weight loss, positional therapy, dental appliances, or surgery (for selected patients who could benefit from them).
Alternatively, patients can be contacted via phone. Phone calls can be made not only by sleep medicine practitioners, as these practitioners may not have the time to make such calls, but also by physician assistants, nurses, or sleep technicians. The point of these calls is to identify patients who may be having second thoughts about CPAP, and assist them with finding useful treatment. As the study findings indicate, knowing adherent CPAP users plays a significant role in respondents' decision to try the CPAP device. We would, therefore, recommend that practitioners encourage patients to seek out and discuss CPAP use with other users. Internet forums are a good platform for this purpose. Practitioners may also ask that sleep partners be involved in the follow-up process because, as the study shows, sleep partners are usually supportive of CPAP use, and patients should be aware of the effect CPAP use or nonuse has on not only their own lives, but also their families' lives.
Future longitudinal research should investigate the effectiveness of such mechanisms in the long run, examining whether and how they increased CPAP adherence rates among patients. Further research should also explore how to identify and characterize patients who develop ambivalence toward their CPAP use versus those who do not. Additional research is also needed to investigate whether and how elderly patients develop and exhibit ambivalence adherence and nonadherence toward CPAP use.
Implementing a follow-up mechanism is not an easy feat, as time and resources are limited and often scarce in many health care systems. However, we believe that close follow-up mechanisms are crucial for the success of sleep medicine in treating OSA patients, thereby improving the quality of their lives. Furthermore, because adherence rates to CPAP use are so low, OSA diagnosis risks becoming an “empty diagnosis,” meaning a futile diagnosis that provides little meaning to patients and carries no good treatment.49 Such an empty diagnosis may lead to the deterioration of the status of sleep medicine, as individuals would refrain from using its services. In the case of OSA, large numbers of untreated diagnosed patients send the message that there is no point in getting an OSA diagnosis. If cuts have to be made in sleep medicine, it is best that they are made elsewhere. The blanket is short, but it should cover this side of OSA treatment.
ENDNOTES
We hope to expand our research in the future to include these populations by using alternative recruitment strategies.
Polysomnographic recordings were performed with Embla (Embla, Amsterdam, The Netherlands), and included conventional parameters.50 Sleep studies were staged and scored according to American Academy of Sleep Medicine criteria51 using Remlogic software (Embla, Amsterdam, The Netherlands) by the same polysomnography technicians during the entire study period. Apnea was defined as an episode of complete breathing cessation of 10 seconds or longer, and hypopnea as a reduction in oral/nasal airflow lasting 10 seconds or longer, accompanied by arousal or by a drop of at least 3% in oxygen saturation. The apnea-hypopnea index (AHI)—number of apnea plus hypopnea events per hour of sleep—was calculated and severity of OSA was defined as mild for AHI ≥ 5 and < 15, moderate for AHI ≥ 15 and ≤ 30 and severe for AHI > 30 events/h.
According to the Israeli National Health Insurance Law, all Israeli citizens must choose 1 of the 4 health plans in Israel. These health plans are obliged to provide patients with medications and health services included in the “health basket” with minimal out-of-pockets payments, including a polysomnography study. The participants in this study are insured by Clalit health plan, which provides medical services to about 60% of the Israeli population. Patients' out-of-pocket payments for polysomnography study is 30 NIS (approximately 8 US dollars). The referral to a sleep unit originates mainly from an ear, nose, and throat physician, a neurologist, or a pulmonologist after a recommendation from the family physician.
Time since diagnosis was not related to or factored into group assignment.
Respondents reported undergoing laser surgery performed by ear, nose, and throat physicians. During the procedure, performed under local anesthesia, a laser beam is sent to burn and remove parts of the palate, especially the soft palate, the amber, and tonsils. Some respondents also tried breathing workshops using a Buteyko method, which is said to help manage breathing-related problems.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. The authors received no financial support for the research, authorship, and/or publication of this article. The authors report no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ACKNOWLEDGMENTS
The authors thank Professor Peter Conrad and Dr. Ofir Abu for providing valuable feedback on earlier drafts. We are also grateful to the anonymous reviewers and editors of Journal of Clinical Sleep Medicine for their helpful comments and suggestions. We owe special thanks to the interviewees who participated in our research and generously shared their thoughts and experiences with us.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- CPAP
continuous positive airway pressure
- OSA
obstructive sleep apnea
- SI
symbolic interactionism
REFERENCES
- 1.Kendzerska T, Mollayeva T, Gershon AS, Leung RS, Hawker G, Tomlinson G. Untreated obstructive sleep apnea and the risk for serious long-term adverse outcomes: a systematic review. Sleep Med Rev. 2014;18(1):49–59. doi: 10.1016/j.smrv.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Sullivan CE, Berthonjones M, Issa FG, Eves L. Reversal of obstructive sleep-apnea by continuous positive airway pressure applied through the nares. Lancet. 1981;1(8225):862–865. doi: 10.1016/s0140-6736(81)92140-1. [DOI] [PubMed] [Google Scholar]
- 3.Epstein LJ, Kristo D, Strollo PJ, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263–276. [PMC free article] [PubMed] [Google Scholar]
- 4.Teri B, D'Ambrosio C, Mohsenin V. Quality of life in patients with obstructive sleep apnea - effect of nasal continuous positive airway pressure - a prospective study. Chest. 1999;115(1):123–129. doi: 10.1378/chest.115.1.123. [DOI] [PubMed] [Google Scholar]
- 5.Ferini-Strambi L, Baietto C, Di Gioia MR, et al. Cognitive dysfunction in patients with obstructive sleep apnea (OSA): partial reversibility after continuous positive airway pressure (CPAP) Brain Res Bull. 2003;61(1):87–92. doi: 10.1016/s0361-9230(03)00068-6. [DOI] [PubMed] [Google Scholar]
- 6.Peker Y, Glantz H, Eulenburg C, Wegscheider K, Herlitz J, Thunstrom E. Effect of positive airway pressure on cardiovascular outcomes in coronary artery disease patients with nonsleepy obstructive sleep apnea the riccadsa randomized controlled trial. Am J Respir Crit Care Med. 2016;194(5):613–620. doi: 10.1164/rccm.201601-0088OC. [DOI] [PubMed] [Google Scholar]
- 7.McEvoy RD, Antic NA, Heeley E, et al. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med. 2016;375(10):919–931. doi: 10.1056/NEJMoa1606599. [DOI] [PubMed] [Google Scholar]
- 8.Lindberg E, Berne C, Elmasry A, Hedner J, Janson C. CPAP treatment of a population-based sample - what are the benefits and the treatment compliance? Sleep Med. 2006;7(7):553–560. doi: 10.1016/j.sleep.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy. Proc Am Thorac Soc. 2008;5(2):173–178. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aloia MS, Arnedt JT, Stanchina M, Millman RP. How early in treatment is PAP adherence established? Revisiting night-to-night variability. Behav Sleep Med. 2007;5(3):229–240. doi: 10.1080/15402000701264005. [DOI] [PubMed] [Google Scholar]
- 11.Brostrom A, Nilsen P, Johansson P, et al. Putative facilitators and barriers for adherence to CPAP treatment in patients with obstructive sleep apnea syndrome: A qualitative content analysis. Sleep Med. 2010;11(2):126–130. doi: 10.1016/j.sleep.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Brostrom A, Arestedt KF, Nilsen P, Stromberg A, Ulander M, Svanborg E. The side-effects to CPAP treatment inventory: the development and initial validation of a new tool for the measurement of side-effects to CPAP treatment. J Sleep Res. 2010;19(4):603–611. doi: 10.1111/j.1365-2869.2010.00825.x. [DOI] [PubMed] [Google Scholar]
- 13.Moroni L, Neri M, Lucioni AM, Filipponi L, Bertolotti G. A new means of assessing the quality of life of patients with obstructive sleep apnea: the MOSAS questionnaire. Sleep Med. 2011;12(10):959–965. doi: 10.1016/j.sleep.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 14.Galetke W, Puzzo L, Priegnitz C, Anduleit N, Randerath WJ. Long-term therapy with continuous positive airway pressure in obstructive sleep apnea: Adherence, side effects and predictors of withdrawal - a ‘real-life’ study. Respiration. 2011;82(2):155–161. doi: 10.1159/000322838. [DOI] [PubMed] [Google Scholar]
- 15.Ayow TM, Paquet F, Dallaire J, Purden M, Champagne KA. Factors influencing the use and nonuse of continuous positive airway pressure therapy: a comparative case study. Rehabil Nurs. 2009;34(6):230–236. doi: 10.1002/j.2048-7940.2009.tb00255.x. [DOI] [PubMed] [Google Scholar]
- 16.Dickerson SS, Kennedy MC. CPAP devices: encouraging patients with sleep apnea. Rehabil Nurs. 2006;31(3):114–122. doi: 10.1002/j.2048-7940.2006.tb00015.x. [DOI] [PubMed] [Google Scholar]
- 17.Dickerson SS, Akhu-Zaheya L. Life changes in individuals diagnosed with sleep apnea while accommodating to continuous positive airway pressure (CPAP) devices. Rehabil Nurs. 2007;32(6):241–250. doi: 10.1002/j.2048-7940.2007.tb00181.x. [DOI] [PubMed] [Google Scholar]
- 18.Veale D, Poussin G, Benes F, Pepin JL, Levy P. Identification of quality of life concerns of patients with obstructive sleep apnoea at the time of initiation of continuous positive airway pressure: a discourse analysis. Qual Life Res. 2002;11(4):389–399. doi: 10.1023/a:1015599326110. [DOI] [PubMed] [Google Scholar]
- 19.Matthias MS, Chumbler NR, Bravata DM, et al. Challenges and motivating factors related to positive airway pressure therapy for post-TIA and stroke patients. Behav Sleep Med. 2014;12(2):143–157. doi: 10.1080/15402002.2013.778200. [DOI] [PubMed] [Google Scholar]
- 20.Tyrrell J, Poulet C, Pepin JL, Veale D. A preliminary study of psychological factors affecting patients' acceptance of CPAP therapy for sleep apnoea syndrome. Sleep Med. 2006;7(4):375–379. doi: 10.1016/j.sleep.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 21.Sawyer AM, Deatrick JA, Kuna ST, Weaver TE. Differences in perceptions of the diagnosis and treatment of obstructive sleep apnea. Qual Health Res. 2010;20(7):873–892. doi: 10.1177/1049732310365502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheung JMY, Bartlett DJ, Armour CL, Glozier N, Saini B. Insomnia patients' help-seeking experiences. Behav Sleep Med. 2014;12(2):106–122. doi: 10.1080/15402002.2013.764529. [DOI] [PubMed] [Google Scholar]
- 23.Blumer H. Symbolic Interactionism: Perspective and Method. Englewood Cliffs, NJ: Prentice-Hall; 1969. [Google Scholar]
- 24.Given L. The Sage Encyclopedia of Qualitative Research Methods. Thousand Oaks, CA: Sage Publications; 2008. [Google Scholar]
- 25.Glaser BG, Strauss AL. The Discovery of Grounded Theory. Chicago, IL: Aldine; 1967. [Google Scholar]
- 26.Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. Thousand Oaks, CA: Sage Publications; 2006. [Google Scholar]
- 27.Charmaz K. Shifting the Grounds: Constructivist Grounded Theory Methods. In: Morse JM, Stern PN, Corbin J, Bowers B, Charmaz K, Clark AE, editors. Developing Grounded Theory: The Second Generation. Walnut Creek, CA: Left Coast Press; 2009. pp. 127–147. [Google Scholar]
- 28.Guba EG, Lincoln YS. Fourth Generation Evaluation. Newbury Park, CA: Sage Publications; 1989. [Google Scholar]
- 29.Rolfe G. Validity, trustworthiness and rigour: quality and the idea of qualitative research. J Adv Nurs. 2006;53(3):304–310. doi: 10.1111/j.1365-2648.2006.03727.x. [DOI] [PubMed] [Google Scholar]
- 30.Sandelowski M. Sample size in qualitative research. Res Nurs Health. 1995;18(2):179–183. doi: 10.1002/nur.4770180211. [DOI] [PubMed] [Google Scholar]
- 31.Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18:59–82. [Google Scholar]
- 32.Launois SH, Pepin JL, Levy P. Sleep apnea in the elderly: a specific entity? Sleep Med Rev. 2007;11(2):87–97. doi: 10.1016/j.smrv.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 33.Appleton SL, Vakulin A, McEvoy RD, et al. Undiagnosed obstructive sleep apnea is independently associated with reductions in quality of life in middle-aged, but not elderly men of a population cohort. Sleep Breath. 2015;19(4):1309–1316. doi: 10.1007/s11325-015-1171-5. [DOI] [PubMed] [Google Scholar]
- 34.Morse JM. The significance of saturation. Qual Health Res. 1995;5:147–149. [Google Scholar]
- 35.LaRossa R. Grounded theory methods and qualitative family research. J Marriage Fam. 2005;67(4):837–857. [Google Scholar]
- 36.Morse JM, Coulehan J. Maintaining confidentiality in qualitative publications. Qual Health Res. 2015;25(2):151–152. doi: 10.1177/1049732314563489. [DOI] [PubMed] [Google Scholar]
- 37.Clarke AE. Situational Analysis: Grounded Theory After the Postmodern Turn. Thousand Oaks, CA: SAGE; 2005. [Google Scholar]
- 38.Wasserman JA, Clair JM, Wilson KL. Problematics of grounded theory: innovations for developing an increasingly rigorous qualitative method. Qual Res. 2009;9:355–381. [Google Scholar]
- 39.Zarhin D. Sleep as a gendered family affair: Snoring and the ‘dark side’ of relationships. Qual Health Res. 2016;26(14):1888–1901. doi: 10.1177/1049732315583270. [DOI] [PubMed] [Google Scholar]
- 40.Zarhin D. “I don't want to see myself as a disabled person”: Continuous positive airway pressure devices and the emergence of (dis)ability as subjectivity. Science, Technology, & Human Values. Epub 2017 May 23. doi: 10.1177/0162243917711006. [Google Scholar]
- 41.Zarhin D. Contesting medicalisation, doubting the diagnosis: Israeli patients' ambivalence towards the diagnosis of obstructive sleep apnoea. Sociol Health Illn. 2015;37:715–730. doi: 10.1111/1467-9566.12229. [DOI] [PubMed] [Google Scholar]
- 42.Budhiraja R, Parthasarathy S, Drake CL, et al. Early CPAP use identifies subsequent adherence to CPAP therapy. Sleep. 2007;30(3):320–324. [PubMed] [Google Scholar]
- 43.Sarrell EM, Chomsky O, Shechter D. Treatment compliance with continuous positive airway pressure device among adults with obstructive sleep apnea (OSA): how many adhere to treatment? Harefuah. 2013;152(3):140–144. [PubMed] [Google Scholar]
- 44.Kohler M, Smith D, Tippett V, Stradling JR. Predictors of long-term compliance with continuous positive airway pressure. Thorax. 2010;65(9):829–832. doi: 10.1136/thx.2010.135848. [DOI] [PubMed] [Google Scholar]
- 45.Kribbs NB, Pack AI, Kline LR, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep-apnea. Am Rev Respir Dis. 1993;147(4):887–895. doi: 10.1164/ajrccm/147.4.887. [DOI] [PubMed] [Google Scholar]
- 46.Ward K, Hoare KJ, Gott M. What is known about the experiences of using CPAP for OSA from the users' perspective? A systematic integrative literature review. Sleep Med Rev. 2014;18(4):357–366. doi: 10.1016/j.smrv.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 47.Jonas DE, Amick HR, Feltner C, et al. Screening for obstructive sleep apnea in adults: Evidence report and systematic review for the us preventive services task force. JAMA. 2017;317(4):415–433. doi: 10.1001/jama.2016.19635. [DOI] [PubMed] [Google Scholar]
- 48.Avellan-Hietanen H, Bachour A, Brander P. Long-term CPAP therapy follow-up: reasons for patients' contacts with the sleep unit. Sleep Med. 2015;16(Suppl 1):S211. doi: 10.5664/jcsm.7568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Madden S, Sim J. Creating meaning in fibromyalgia syndrome. Soc Sci Med. 2006;63(11):2962–2973. doi: 10.1016/j.socscimed.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 50.Oksenberg A, Khamaysi I, Silverberg DS. Apnoea characteristics across the night in severe obstructive sleep apnoea: Influence of body posture. Eur Respir J. 2001;18(2):340–346. doi: 10.1183/09031936.01.00038101. [DOI] [PubMed] [Google Scholar]
- 51.Iber C, Ancoli-Israel S, Chesson A, Quan S for the American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.