Abstract
Study Objectives:
To investigate adherence to continuous positive airway pressure (CPAP) therapy and identify barriers to CPAP use among patients with obstructive sleep apnea (OSA) in India.
Methods:
A self-devised semistructured questionnaire (which collected patients' demographic information, socioeconomic position, and information about disease status, symptoms, and complications) was administered to consecutive patients with moderate to severe OSA from June 2015 to August 2016. Patients were grouped according to CPAP device buying behavior (buyers versus nonbuyers) and CPAP compliance behavior (compliant versus noncompliant).
Results:
Out of 187 patients with moderate-severe OSA, 79 patients were enrolled for this study. The overall adherence rate (usage > 4 hours per night on > 70% nights) was 30.3%. Among the patients in the buyer group, adherence was 82.7%. Fifty patients did not buy a CPAP device; 30 of these 50 patients (60%) said financial constraints were the most important reason for not buying a CPAP device. Patients without financial constraints had higher chances—odds ratio (95% confidence interval) = 4.85 (1.6–16.1)—of buying a CPAP device than patients with financial constraints. Patients with more severe disease (ie, lower nadir oxygen saturation during sleep, higher apnea-hypopnea index, or presence of obesity hypoventilation syndrome) were more likely to buy and use a CPAP device.
Conclusions:
The main cause of nonuse of CPAP in India is the inability to buy a CPAP device. In patients who are able to buy a CPAP device, adherence was significantly higher (82.7%) compared to adherence in the study's overall population (30.3%). Furthermore, patients with more severe OSA were more likely to buy a device and adhere to CPAP. Patients' behaviors and attitudes are also important barriers in using CPAP. There needs to be increased awareness of the benefits of CPAP therapy among patients.
Citation:
Goyal A, Agarwal N, Pakhare A. Barriers to CPAP use in India: an exploratory study. J Clin Sleep Med. 2017;13(12):1385–1394.
Keywords: adherence, continuous positive airway pressure, cost, CPAP, obstructive sleep apnea
INTRODUCTION
The first-line treatment for obstructive sleep apnea (OSA) is continuous positive airway pressure (CPAP). CPAP has been proven to reduce daytime sleepiness, improve quality of sleep and fatigability, and decrease the cardiovascular complications of OSA such as hypertension, coronary arterial disease, and cerebrovascular disease.1 Unfortunately, poor adherence to CPAP therapy reduces its effectiveness and thereby also limits its beneficial outcomes.2
OSA is highly prevalent in the Indian population with a prevalence of 13.74% in snorers and 3.57% in nonsnorers.3 Many studies have investigated the use of CPAP by patients with OSA in Western countries, and nonadherence to CPAP is high—in the range of 46% to 83%.4 In most of the Western countries, the cost of a CPAP device is either reimbursed or provided by the medical insurance companies; cost does not play a major role in CPAP adherence. The main reason for non-adherence is nonacceptance on the part of the patient. Conditions are different in most of the third-world countries, where insurance access is minimal, and insurance companies usually do not cover the cost of a CPAP device. In India, CPAP is not covered by any private insurance companies. Only some government employees are able to be reimbursed for CPAP therapy, and that too ranges from 30% to 100% depending upon the reimbursement rules of various government offices. CPAP is generally an out-of-pocket expense for most of the Indian population. As such, socioeconomic factors play a major role in usage of CPAP.
BRIEF SUMMARY
Current Knowledge/Study Rationale: To our knowledge, this is the first study to report adherence rates to continuous positive airway pressure (CPAP) therapy in India. Furthermore, the barriers preventing the use of CPAP in third world countries need to be identified.
Study Impact: This study shows that cost is the most important barrier to CPAP uptake in patients with obstructive sleep apnea in India. If a patient is able to buy a CPAP device, her adherence is significantly better compared to the rate of CPAP adherence reported in Western countries.
In India, awareness of OSA and CPAP is low as sleep medicine is still in its infancy. Most often patients are not convinced of the need for this therapy for various reasons, but the most important of which is financial burden. The current study shows that if a patient is able to buy a CPAP device, then she usually adheres to the therapy.
To our knowledge, this is the first study to report CPAP adherence rates and barriers to CPAP use in India. Although it is a general perception among Indian physicians that patients do not buy a CPAP device due to its high cost, no study has been done to confirm this belief. The objectives of the current study are to report the proportion of patients in India who do not use CPAP despite therapeutic indication, and to understand the reasons and barriers for the nonuse of CPAP in this patient population.
METHODS
Study Setting and Population
The population for this cross-sectional study was consecutive patients in whom OSA was diagnosed in the authors' sleep laboratory from June 2015 to August 2016. This sleep laboratory is the only level 1 polysomnography laboratory in central India. The laboratory caters to referred patients as well as walk-in patients. Patients with OSA who were older than 18 years of age, with an apnea-hypopnea index (AHI) > 15 (moderate to severe OSA), and were advised to use CPAP therapy were included. In this sleep laboratory, patients with mild OSA are not advised to use CPAP therapy. Patients who did not give consent to be a part of the study were excluded.
Procedure
All eligible patients were invited to participate in the study and written informed consent was obtained from willing patients. Patients with OSA who were advised to use CPAP therapy attended a one-on-one counseling session with a sleep physician along with at least one family member. These patients were provided with information about OSA and CPAP. At no cost to the patient, CPAP or bilevel PAP devices were distributed for a 1-week trial. After 1 week, the devices were reviewed along with the downloaded compliance data. At least 1 month after prescribing CPAP, these patients were called and asked to schedule an in person interview. The interviews took place at AIIMS Bhopal Sleep Medicine OPD.
Study Instrument
A self-devised semistructured questionnaire (Hindi and English language) was developed after reviewing existing literature. It included details regarding patients' demographic information, socioeconomic position, and information about disease status, symptoms, and complications. Data regarding routine clinical examinations, anthropometry, Epworth Sleepiness Scale (ESS), STOP-BANG assessment, and routine laboratory investigations was also gathered. Patients' understanding of the disease and its severity, perceived barriers, benefits, and self-efficacy for CPAP usage were assessed. This was done through open-ended questions and probes. Patients were asked to provide the number of hours of CPAP usage per night in the past month, and this was cross-referenced with downloaded compliance data. Patients were labeled complaint if they were using CPAP for at least 4 hours per night. ESS was used to assess daytime sleepiness.
A modified Kuppuswami scale was used as a socioeconomic scale.5 It is currently the most common validated scale for socioeconomic stratification in the Indian population. This scale includes the education and occupation of the head of the family and monthly family income. Education of the head of the family has a score ranging from 1 (for illiterate) to 7 (for honors). Occupation of the head of the family has a score ranging from 1 (unemployed) to 10 (professional). Similarly, monthly family income (according to 2014 update) has a score of 1 (< 1,865 Indian rupee [INR] which is approximately 28 United States dollars [USD]) to 12 (> 36,997 INR or approximately 560 USD). The sum of these 3 scores classifies a family into 5 different socioeconomic classes (lower class < 5; upper-lower class 5–10; lower-middle class 11–15; upper-middle class 16–25; and upper class 26–29).
Polysomnography Analysis
Level 1 polysomnography (PSG) with manual titration was done in all patients. Alice 6 (Koninklijke Philips N.V., Amsterdam, Netherlands) was used for PSG. Scoring was done first by a sleep technician, then by a resident doctor posted in the sleep laboratory, and then finally by a treating sleep physician. Results of titration done in PSG were classified as “optimal,” “good” and “adequate.” A titration was considered “optimal” if it reduced the AHI to less than 5 events/h for an at least a 15-minute duration, and if it included supine REM sleep at the selected pressure that was not continually interrupted by spontaneous arousals or awakenings. A titration was considered “good” if it reduced the AHI to less than or equal to 10 events/h or by 50% from the baseline AHI, and included supine REM sleep that was not continually interrupted by spontaneous arousals or awakenings at the selected pressure. A titration was considered “adequate” if it did not reduce the AHI to 10 events/h or lower, but did reduce the AHI by 75% from the baseline AHI (especially in patients with severe OSA). Also, those titrations that met the criteria for “optimal” or “good” but supine REM sleep did not occur at the selected pressure were considered “adequate.”6 Patients were asked about their experience during the in-hospital titration PSG, and the responses were classified as “good,” “nothing different,” and “difficult.” Patients were also asked whether they had difficulty tolerating the mask or CPAP pressure during the titration PSG.
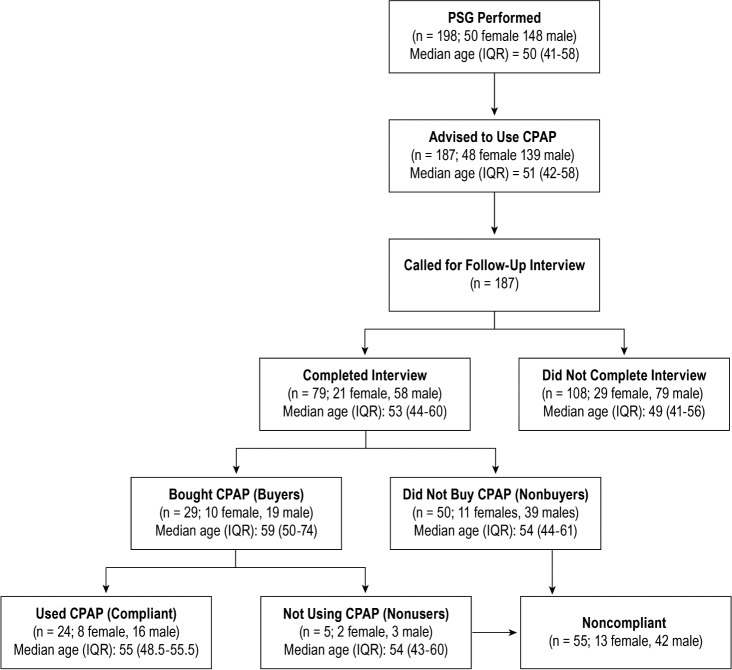
Patients were divided into groups based on whether or not they purchased a CPAP device in accordance with their physician's recommendation. These groups were labeled buyers and nonbuyers. Those in the buyers group were further classified as compliant or nonusers. Compliance was defined as the usage of CPAP for > 4 hours per night on > 70% nights. Patients categorized into the nonbuyer and nonuser groups were also grouped into the noncompliant group (Figure 1). We assessed CPAP buying behavior of the buyers versus nonbuyers groups and CPAP compliance behavior of the compliant versus non-compliant groups.
Figure 1. Flowchart depicting study algorithm.
CPAP = continuous positive airway pressure, IQR = interquartile range, PSG = polysomnography.
Data Analysis
Data entry and analysis were performed using Epi Info version 7.2.0.1 software (Centers for Disease Control and Prevention, Atlanta, Georgia, United States). Numerical variables were summarized as median and interquartile range. For categorical variables, count and proportion were used for summarization, and prevalence was estimated in proportion and in 95% confidence intervals. Chi-square was used to find an association between compliance and buying behavior with various categorical variables; t tests were also used when independent variables were numerical. We used binary logistics regression analysis to identify independent determinants of noncompliance. A data-driven approach was used to select independent factors to be entered in the regression model, wherein those variables with values of P < .1 were selected. Also, if 2 or more variables were highly correlated, then 1 was selected from the group. For the qualitative analysis of open-ended questions or semiopen questions, patients' statements were recorded verbatim by the interviewer. Then these statements were translated in English and content analysis was done. Frequency charting of themes was presented.
Ethical Concern
An approval from All India Institute of Medical Sciences Bhopal Institutional Human Ethical Committee was obtained for conducting the study.
RESULTS
Study Population (Figure 1)
During the study period, PSG was done in 198 patients; 187 patients had moderate to severe OSA and were prescribed PAP therapy and were called for this study. Out of these, 79 patients were followed in the sleep clinic after a mean duration of 160.97 ± 99.12 days after CPAP prescription. Fifty patients did not buy a CPAP device; 29 patients bought a CPAP device and 24 patients were finally using CPAP. The adherence rate was 30.3% (24 of 79) among total patients and 82.7% (24 out of 29) among patients who bought CPAP.
Socioeconomic and Demographic Characteristics (Table 1)
Table 1.
Socioeconomic and demographic characteristics.
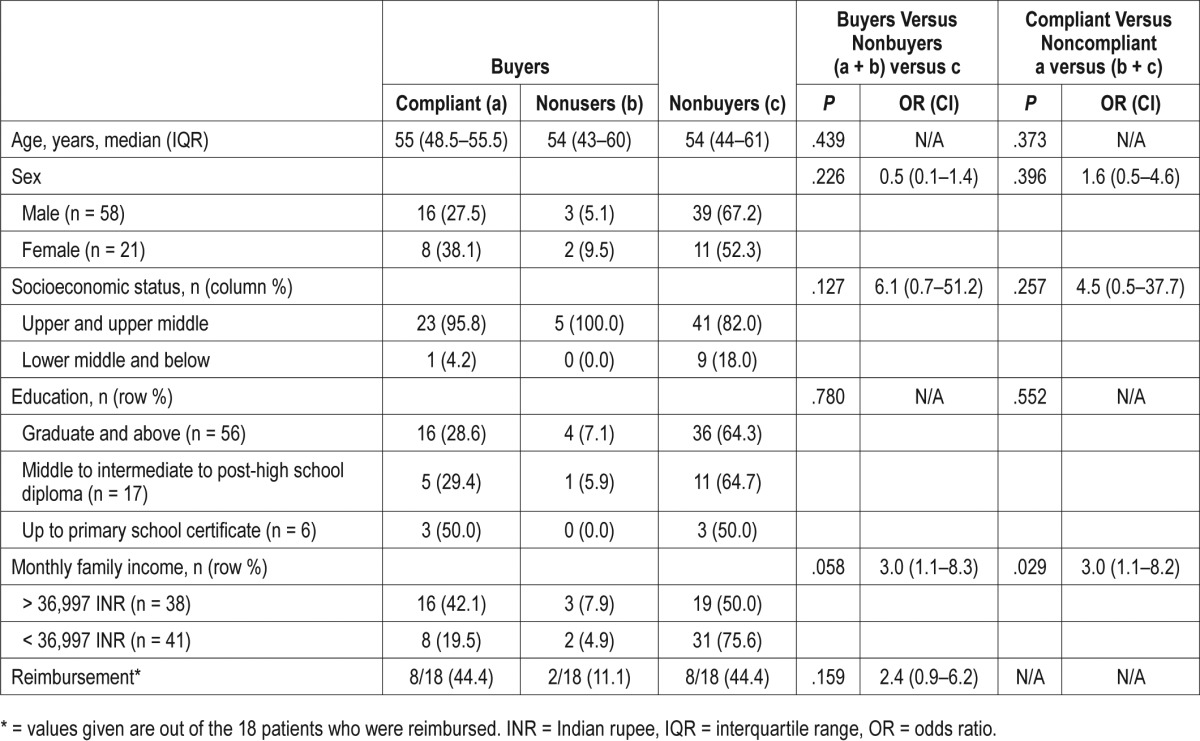
The median (interquartile range) age of the 79 patients who followed up was found to be 53 years (44–60). The only variable found to have significant results was average monthly income when cross-tabulated with adherence to treatment (P = .029).
The 7 categories of income defined by the modified Kuppuswami socioeconomic scale were combined into 2 because we had a small sample size (ie, income less than and above 36,997 INR [approximately 550 USD]). There was a nearly significant difference found between these 2 groups in CPAP device buying behavior (P = .058) and a significant difference when compliance to treatment was compared (P = .029). Patients with higher income were more compliant with CPAP.
To find out the possible effect of socioeconomic status, we combined the upper 2 and the lower 3 classes of the modified Kuppuswami scale (due to small sample size) and formed 2 groups (upper class and lower class). No significant difference was found with compliance behavior or buying behavior between these 2 groups.
Of 79 patients, only 18 (22.7%) could receive reimbursement for CPAP. There was no significant difference seen in compliance or buying behavior in patients with reimbursement versus patients without reimbursement (P = .159).
Smoking and alcohol had no significant relation with CPAP adherence.
Baseline Characteristics (Table 2)
Table 2A.
Baseline characteristics.
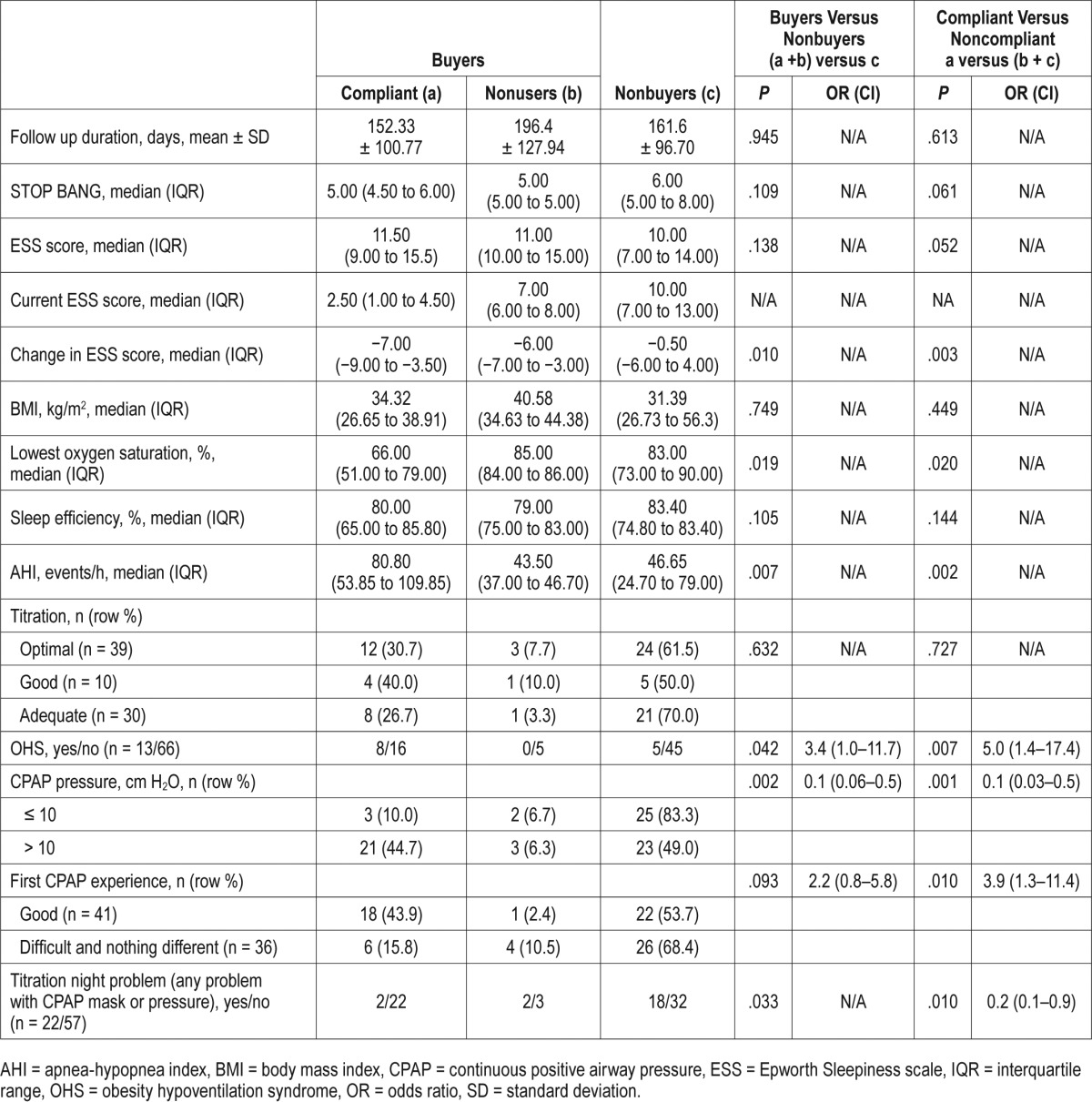
There was also a nearly significant difference found in adherence behavior with baseline ESS (P = .052). Patients who were more sleepy were more adherent to CPAP. A significant difference was seen between change in ESS and adherence to CPAP. Patients who were using CPAP had significant reduction in sleepiness (P = .003). A significant difference was also seen between buying behavior and adherence with respect to nadir oxygen saturation during sleep, AHI, and obesity hypoventilation syndrome. Patients with more severe disease were more eager to buy CPAP and were more adherent to therapy.
Titration (Table 2)
Patients who had been advised to use CPAP at a pressure > 10 cm H2O were more likely to purchase a CPAP device (odds ratio [CI] = 5.2 [1.7–15.9]; P = .002) and adhering to therapy (odds ratio [CI] = 7.2 [1.9–27.3]; P = .001) when compared to those advised to undergo CPAP at a pressure ≤ 10 cm H2O. Patients who had a higher CPAP pressure requirement were more likely to buy and use a CPAP device.
Patient responses to the experience during in-hospital titration were classified as “good,” “nothing different,” and “difficult.” This experience on analysis was found to have a significant effect on CPAP adherence (odds ratio [CI] = 3.9 [1.3–11.4]; P = .010). If the patient had any difficulty in tolerating CPAP pressure or had mask intolerance, then she was more likely to buy and use a CPAP device.
Comorbidities (Table 3)
Table 3.
Comorbidities.
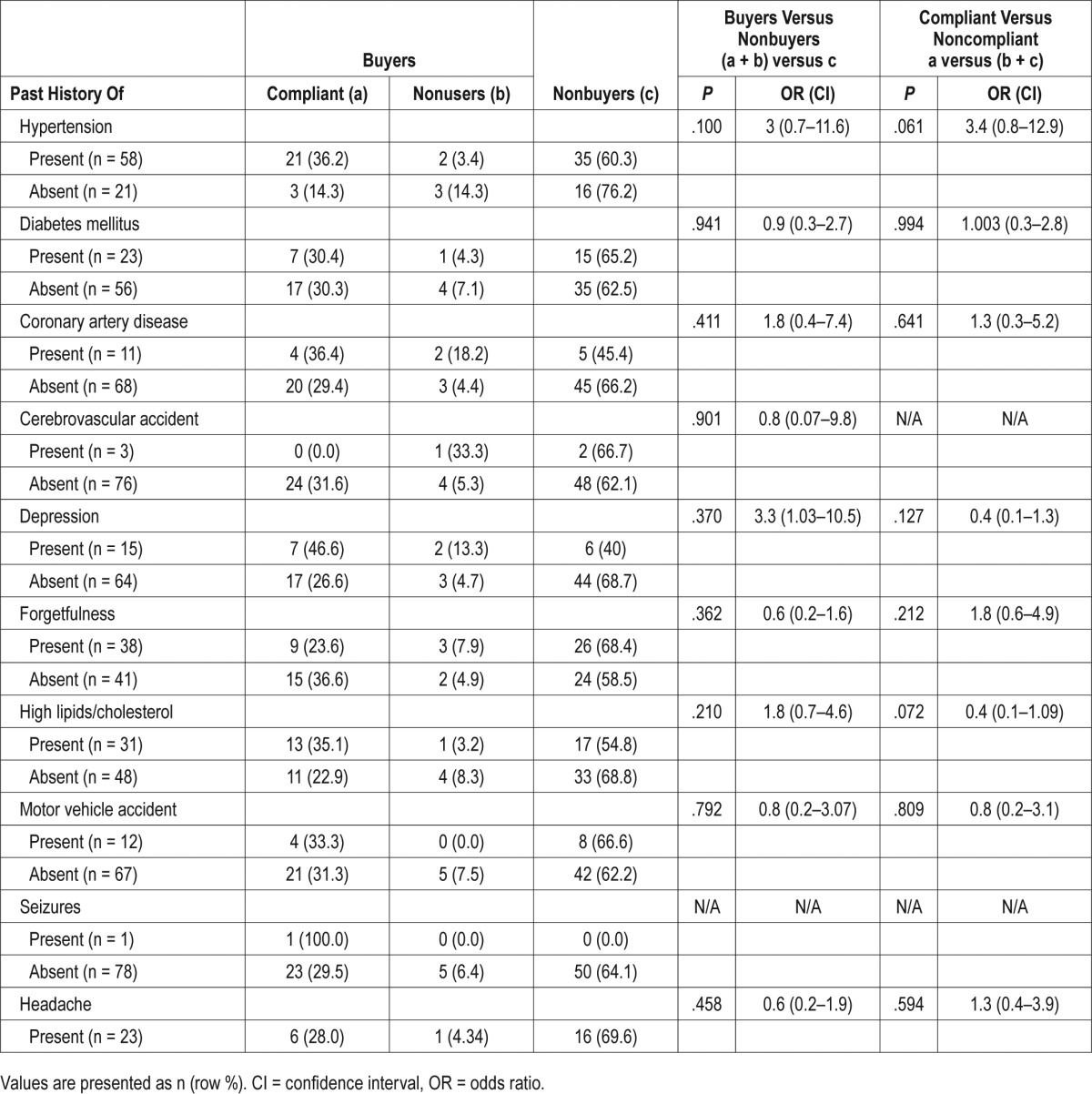
There were no significant differences found in the buyers versus nonbuyers groups nor the adherent versus nonadherent groups in any of the comorbid conditions except hypertension, which showed a nearly significant correlation with compliance behavior (odds ratio [CI] = 3.4 [0.8–12.9]; P = .061). Patients with hypertension were relatively more adherent to CPAP.
Reasons for Not Buying (Nonbuyers, n = 50)
The individuals in the nonbuyers group were asked for reasons (one or more) for not purchasing a CPAP device (Table 4, Figure 2). Although the most common reason was financial constraints (34/50, 68%), there were also a fair number of other reasons reported. These patients were also asked to identify the most important reason for not purchasing. Again, most of the patients (30/50, 60%) said cost was the biggest prohibitory factor. Some patients reported some other unique reasons as the most important for not being able to buy a CPAP device; these responses included:
“I feel too lazy to use the machine every day”
“I have not been taught how to use the machine properly”
“I want to use the machine not on a regular basis but on and off”
“I am an Army soldier and I am always on the move in difficult areas, so I can't carry the machine every time”
“I want my other family members to undergo PSG as they have the same symptoms and then I want them to use as well, only then will I also start using”
“Administrative delay in procuring from government”
Table 4.
Reasons for not buying/using CPAP.
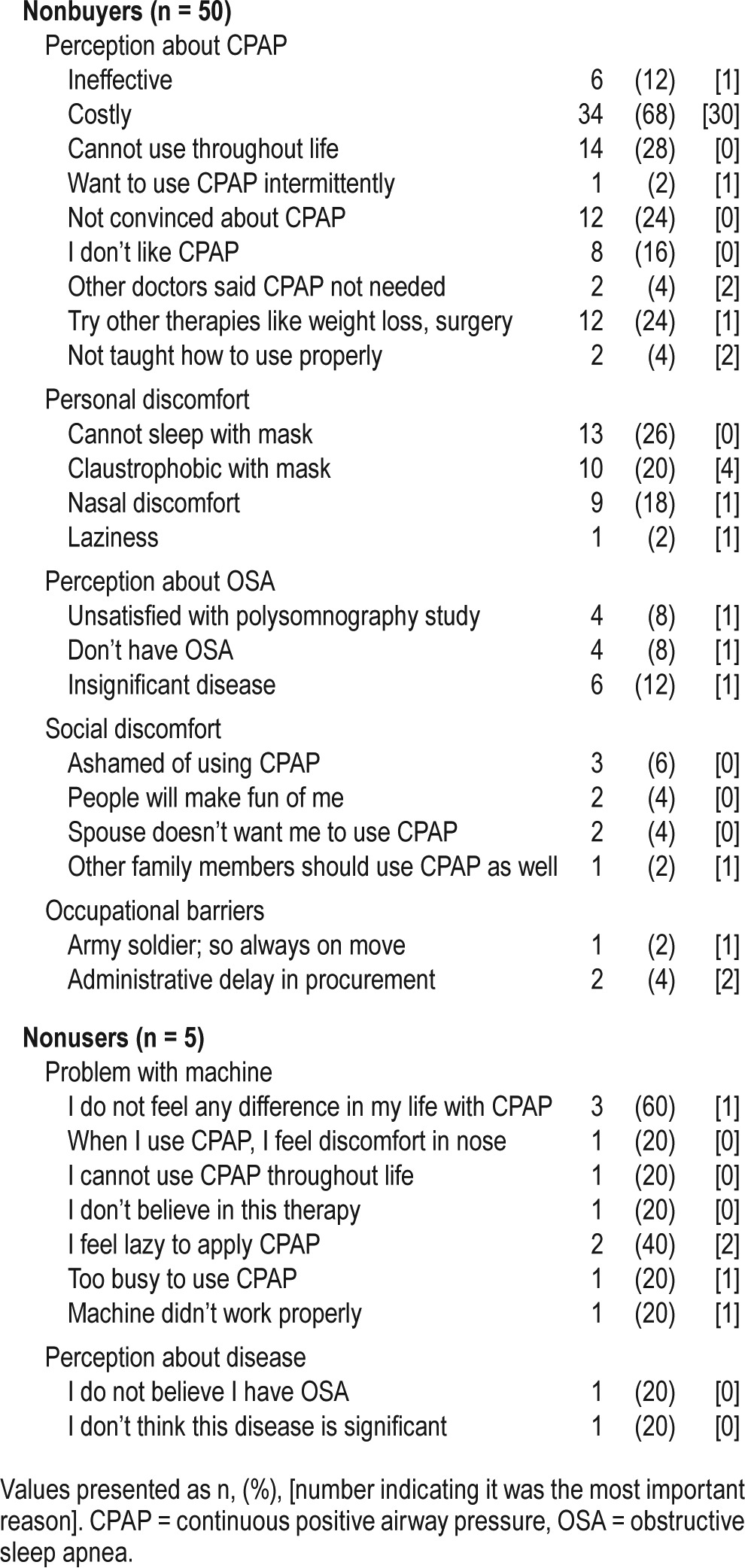
Figure 2. Word cloud showing reasons for not buying CPAP.
CPAP = continuous positive airway pressure.
Reasons for Buying but Not Using (Nonusers, n = 5)
Five patients were not using CPAP despite buying a CPAP device. Most of these patients gave “no difference in their lives after using CPAP” as the most important reason for not adhering to CPAP. Other responses included “I feel too lazy to use CPAP,” “I feel discomfort in nose on using CPAP,” and “I am too busy to use CPAP” (Table 4).
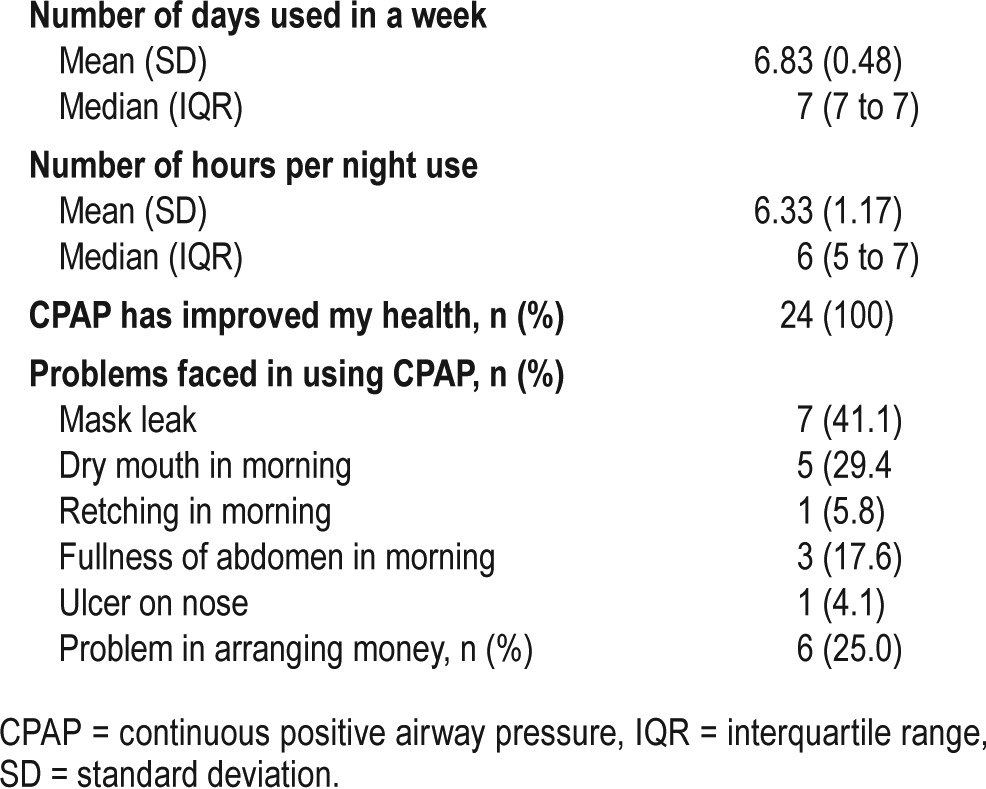
Compliant Group (n = 24)
Patients who used CPAP more than 4 hours per night for more than 70% of nights were categorized into the compliant group. All 24 patients in this group said that they had a significant improvement in their health. Patients were asked an open-ended question regarding improvement in their health; analysis of the responses was done qualitatively. The most common response was that they had a decrease in daytime sleepiness. Other responses included a reduction in sleep during the day, better control of hypertension, decreased nocturia, better sleep during the night, controlled weight, better lifestyle, decreased forgetfulness, and better efficiency at work. One patient who had uncontrolled nocturnal seizures had resolution of seizures after starting CPAP. In previous studies, resolution of snoring, better sleep, reduced daytime sleepiness, feeling of wellness, better memory, decreased headaches, and better control of comorbidities were found to be the most important reasons for CPAP compliance.7–9
Some patients also reported problems using the CPAP machine, the most common being mask leakage (41.1%). Six patients (25%) reported problems in obtaining money for purchasing the machine (Table 5).
Table 5.
CPAP usage in compliant group.
Comparing Groups With Financial Constraints (Table 6)
Table 6.
Perceived money problem
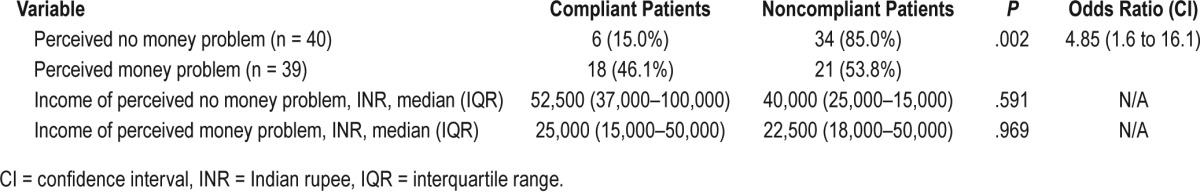
Because income was found to be one of the major determinants of CPAP device buying behavior, we divided the total sample population into 2 groups: those who said they had financial constraints and those who did not have financial constraints in buying CPAP. Patients who said they did not have financial constraints in buying a CPAP device were more likely (odds ratio [CI] = 4.85 [1.6–16.1]) to buy a CPAP device than patients who said they had financial constraints.
When we compared the income of patients who said that money was one of the primary reasons for not being able to buy a CPAP device with those who said they bought a CPAP device despite financial constraints, we found no difference in income in these 2 groups. This shows that the attitude of patients toward their disease is also an important factor apart from cost of a CPAP device.
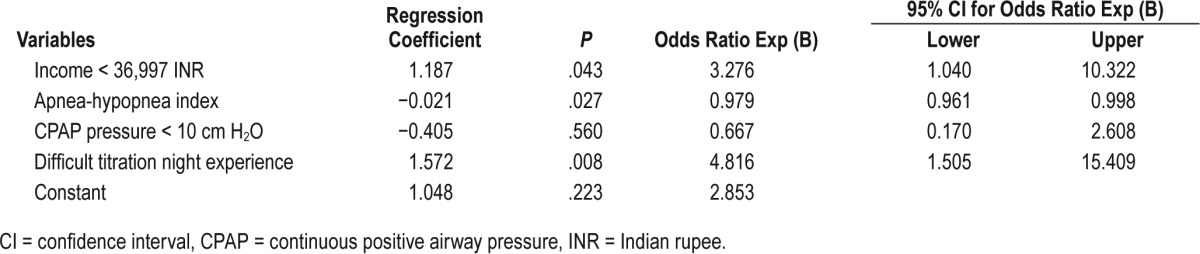
Binary logistic regression analysis was performed by entering all variables with P < .1 at the same time in the model. Selected independent variables were CPAP pressure, titration night experience, AHI, and family income. AHI, nadir oxygen, and presence of obesity hypoventilation syndrome were highly correlated or interdependent on each other; therefore, only AHI was entered. On multivariate analysis, family income < 36,997 INR and difficult titration night experience were significant predictors of nonadherence. Higher values of AHI were associated with better compliance (negative regression coefficient) (Table 2B).
Table 2B.
Binary logistic regression analysis for predictors of noncompliance.
DISCUSSION
CPAP is an unorthodox treatment for most patients, in which the patient does not simply take a pill, but instead she has to use a machine that pushes air under pressure to keep the airway open. Only 17% to 54% of patients remain adherent to CPAP.4 Most of the data for adherence available are from Western countries where cost is not a major barrier to obtaining CPAP because most of the population is covered by insurance, and CPAP is covered by private insurance companies. In contrast, CPAP in India is currently not covered by private insurance companies, and only some government employees receive reimbursement for CPAP costs.
Data from India—or any other third-world country—on CPAP adherence and the economical barriers for obtaining CPAP are scarce in the existing literature. The objectives of the current study were to report adherence rates to CPAP and identify reasons for nonadherence to CPAP in Indian patients with OSA. In our study, we found resistance at the very first step (ie, purchasing/acquiring the CPAP device) as the most important reason for nonadherence. This is evident from the fact that 24 of 29 patients who purchased CPAP were using CPAP for approximately 6 hours per night every day (82.7% CPAP buyers were adherent). Overall adherence was 30.3% (24 of 79 patients).
Because cost was the most important barrier in purchase of a CPAP device in our study, we compared the income of buyers and nonbuyers. The patients with monthly family income more than 36,997 INR (approximately 550 USD) were three times more likely to buy and comply with CPAP compared to the group with lower income. These results are consistent with those from Somers et al. who found that patients with higher income were more likely to purchase of CPAP.9 Similarly, Simon-Tuval et al. has shown a 140% increase in acceptance of CPAP therapy with each increase in income level.8
Because we had approximately 25% of CPAP device buyers who said that they had difficulty obtaining money for a CPAP device, we compared their income with those who did not buy a CPAP device due to financial constraints. We found that there was no difference in the income of these 2 groups. This suggests that the patient's attitude and mindset could also be seen as a hindrance in CPAP device purchase. OSA is a neglected disorder in India; people see it as a disease of only “snoring.” Knowledge about its complications is poor among patients as well as doctors, perhaps contributing to the patients' belief that CPAP treatment is not worth purchasing.
CPAP in India is currently not insured by private insurance companies, and only some government employees are reimbursed for CPAP costs. There was no difference in buying behavior in those patients who had access to CPAP device reimbursement when compared to others. This might be due to lack of awareness about OSA as a disease in society and also due to the attitude of patients toward this disease.
Tarasiuk et al. studied the role of financial incentive on uptake of CPAP. Patients in a financial incentive group were provided CPAP at a subsidized rate of $55 and controls had to pay the entire amount ($330–$660) themselves. They found that CPAP acceptance was 43% higher in the financial incentive group compared to the control group.10 This shows that if patients are given support to buy a CPAP device, acceptance of CPAP significantly increases.
We did not find sex or socioeconomic status (according to the modified Kuppuswami scale) to affect compliance or buying behavior of CPAP. In a study conducted to find predictors of long-term CPAP use in Israel, female sex was found to be a barrier in CPAP acceptance.11 Although in India, unfortunately, the health of females is often neglected, surprisingly in our study, we did not find any effect of sex on CPAP acceptance.
Increased CPAP acceptance with increasing age has been previously reported,8 but in our study age was not found to be a significant factor determining adherence or purchase of a CPAP device.
Education has been previously shown to affect adherence to CPAP therapy.8,9 It has been shown that patients living in areas with a higher percentage of graduates were more likely to be adherent to treatment. Whereas in some other studies,12 and the one conducted by us, we did not find adherence to depend on education status of the patient. In our study, smoking and drinking alcohol were not found to have any influence on adherence, but some studies found a negative effect of smoking or alcohol on overall adherence to CPAP therapy.11–13
As expected there was great decline in ESS in the adherent group. It was also seen that change in sleepiness after using CPAP has a great effect on adherence with CPAP. We also observed that the adherent group had a higher baseline sleepiness score than the nonadherent group, which implies that patients with higher baseline sleepiness are more likely to be adherent to CPAP; similar results were shown by McArdle et al. where most of the patients with ESS score higher than 10 were found to be adherent even after 3 years of prescription compared to lower ESS scores.11
Obesity hypoventilation syndrome is often associated with severe OSA. Patients with obesity hypoventilation syndrome were 3.4 times more likely to buy a CPAP device and 5 times more likely to adhere to CPAP therapy than patients without obesity hypoventilation syndrome. This means that the more severe the disease, the more likely the patients are to undergo therapy.
Similarly, patients who had more severe OSA (ie, higher AHI, lower nadir oxygen saturation) were more likely to buy and use a CPAP device as compared to those with less severe OSA. This finding is in agreement with other studies where severity of the disease was one of the most important factors for determining adherence.8,11,12,14 Similarly, it was observed that patients with CPAP pressure of more than 10 cm H2O are 5 times more likely to buy and 7.2 times more likely to comply with treatment. CPAP pressures > 10 cm H2O have been shown to be associated with CPAP adherence.15 A possible reason for this could be that usually more severe OSA requires higher pressure, so patients with more severe OSA who require higher pressure are more adherent than patients with a lower CPAP requirement.
Many studies done in the past have shown a positive correlation with experience with CPAP during in-hospital titration. Drake et al. report that improvement in sleep on the titration night is a major predictor of future compliance of the patient with CPAP.16 Likewise in our study, the patients who did not face any problems relating to the CPAP pressure or mask were 3.9 times more likely to be adherent to the therapy and 2.2 times more likely to purchase a CPAP device. High satisfaction levels on the morning after in-hospital titration was also a positive influence, both on buying and compliance behavior. So, if a patient is comfortable with PSG titration, he or she is more likely to adhere to treatment. This again highlights the importance of having a written protocol for titration and having a good sleep technician so that titration is done satisfactorily and patients are more likely to use CPAP.
Although another study has shown a relationship between hypertension and increased compliance in the form of increase in number of days of use, our study failed to find any relationship between hypertension or any other comorbidity associated with OSA.13
Identifying the barriers to CPAP uptake in Indian patients was one of the main objectives of our study. There have been very few studies conducted in the past where cost as a barrier was studied. In a study done in Israel (where CPAP therapy is not covered under reimbursement), cost of a CPAP device was found to be one of the major factors along with side effects of CPAP, failure to adapt to therapy, and patients wanting to try other therapies.8 In a study done in Canada (where health insurance covered cost of CPAP), poor titration night experience was the most important factor.7
In India, many people do not have insurance coverage, and even those who do, they do not have insurance that covers CPAP therapy. In our study, financial constraints were the most significant barrier to CPAP therapy. Out of 50 nonbuyers 34 (68%) patients reported it to be one of the reasons and 30 (54.5%) patients called it the most important reason for not being able to purchase CPAP (Table 4). In our study, only 5 patients left treatment after buying a CPAP device. Reasons for stopping CPAP were “no difference in sleep quality” or discomfort with the mask or laziness to use the CPAP device. In a study done at Mount Sinai Hospital Sleep Clinic in Montreal, the main reason for nonadherence was found to be the tendency of patients to switch over to dental devices. Other reasons were preference of surgery over noninvasive CPAP, noise of the apparatus, and mask issues (especially claustrophobia).7 As dental sleep medicine is still not developed in India, alternate treatment options are very limited to patients with OSA at our center. This might be the reason for the difference in responses in 2 studies.
Among the CPAP-adherent patients, all of them agreed that CPAP has been helpful in improving their health and they were satisfied with the treatment and were eager to continue CPAP therapy. Among the patients who bought a CPAP device, 82.7% (24 of 29) were regularly using CPAP. This shows that in India the most important prohibitive factor for CPAP device usage is cost. If a patient is able to purchase a CPAP device, then she is more likely to adhere to CPAP compared to Western countries, where adherence is around 46% to 83%.4
Limitations
Limitations of this study include small sample size, and the fact that it was a single-center study done at a public hospital; this could lead to referral bias. Multicenter studies should be undertaken on a pilot basis in other parts of India to understand the main concerns underlying resistance of patients toward acquiring and complying with CPAP treatment. Another limitation of this study is that it does not report long-term adherence data of CPAP usage.
CONCLUSIONS
The main reason for not using CPAP in India is the inability to buy a CPAP device. In patients who are able to buy a CPAP device, adherence was significantly higher (82.7%) compared to adherence in the overall population (30.3%). Patient behaviors and attitudes are also important barriers to CPAP therapy. Awareness regarding benefits of CPAP needs to be increased among patients. Patients with more severe OSA are more likely to buy and adhere to CPAP therapy.
DISCLOSURE STATEMENT
Work for this study was performed at All India Institute of Medical Sciences (AIIMS Bhopal). All authors have seen and approved this manuscript. The authors report no conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the Indian Council of Medical Research for granting short-term student status to Namrata Agarwal.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- BMI
body mass index
- CI
confidence interval
- CPAP
continuous positive airway pressure
- ESS
Epworth Sleepiness Scale
- INR
Indian rupee
- IQR
interquartile range
- OHS
obesity hypoventilation syndrome
- OR
odds ratio
- OSA
obstructive sleep apnea
- PAP
positive airway pressure
- PSG
polysomnography
- REM
rapid eye movement
- SD
standard deviation
- USD
United States dollars
REFERENCES
- 1.Huang Z, Liu Z, Luo Q, et al. Long-term effects of continuous positive airway pressure on blood pressure and prognosis in hypertensive patients with coronary heart disease and obstructive sleep apnea: a randomized controlled trial. Am J Hypertens. 2015;28(3):300–306. doi: 10.1093/ajh/hpu147. [DOI] [PubMed] [Google Scholar]
- 2.Kang Y, Sawyer AM, Griffin PM, Prabhu VV. Modelling adherence behaviour for the treatment of obstructive sleep apnoea. Eur J Oper Res. 2016;249(3):1005–1013. doi: 10.1016/j.ejor.2015.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharma SK, Kumpawat S, Banga A, Goel A. Prevalence and risk factors of obstructive sleep apnea syndrome in a population of Delhi, India. Chest. 2006;130(1):149–156. doi: 10.1378/chest.130.1.149. [DOI] [PubMed] [Google Scholar]
- 4.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy the challenge to effective treatment. Proc Am Thorac Soc. 2008;5(2):173–178. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oberoi SS. Updating income ranges for Kuppuswamy's socio-economic status scale for the year 2014. Indian J Public Health. 2015;59(2):156–157. doi: 10.4103/0019-557X.157540. [DOI] [PubMed] [Google Scholar]
- 6.Kushida CA, Chediak A, Berry RB, et al. Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med. 2008;4(2):157–171. [PMC free article] [PubMed] [Google Scholar]
- 7.Wolkove N, Baltzan M, Kamel H, Dabrusin R, Palayew M. Long-term compliance with continuous positive airway pressure in patients with obstructive sleep apnea. Can Respir J. 2008;15(7):365–369. doi: 10.1155/2008/534372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simon-Tuval T, Reuveni H, Greenberg-Dotan S, Oksenberg A, Tal A, Tarasiuk A. Low socioeconomic status is a risk factor for CPAP acceptance among adult OSAS patients requiring treatment. Sleep. 2009;32(4):545–552. doi: 10.1093/sleep/32.4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Somers ML, Peterson E, Sharma S, Yaremchuk K. Continuous positive airway pressure adherence for obstructive sleep apnea. ISRN Otolaryngol. 2011;2011:943586. doi: 10.5402/2011/943586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tarasiuk A, Reznor G, Greenberg-Dotan S, Reuveni H. Financial incentive increases CPAP acceptance in patients from low socioeconomic background. PLoS One. 2012;7(3):e33178. doi: 10.1371/journal.pone.0033178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McArdle N, Devereux G, Heidarnejad H, Engleman HM, Mackay TW, Douglas NJ. Long-term use of CPAP therapy for sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med. 1999;159(4):1108–1114. doi: 10.1164/ajrccm.159.4.9807111. [DOI] [PubMed] [Google Scholar]
- 12.Gagnadoux F, Le Vaillant M, Goupil F, et al. Influence of marital status and employment status on long-term adherence with continuous positive airway pressure in sleep apnea patients. PLoS One. 2011;6(8):e22503. doi: 10.1371/journal.pone.0022503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim JH, Kwon MS, Song HM, Lee B-J, Jang YJ, Chung Y-S. Compliance with positive airway pressure treatment for obstructive sleep apnea. Clin Exp Otorhinolaryngol. 2009;2(2):90–96. doi: 10.3342/ceo.2009.2.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen YF, Hang LW, Huang CS, Liang SJ, Chung WS. Polysomnographic predictors of persistent continuous positive airway pressure adherence in patients with moderate and severe obstructive sleep apnea. Kaohsiung J Med Sci. 2015;31(2):83–89. doi: 10.1016/j.kjms.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dzierzewski JM, Wallace DM, Wohlgemuth WK. Adherence to continuous positive airway pressure in existing users: self-efficacy enhances the association between continuous positive airway pressure and adherence. J Clin Sleep Med. 2016;12(2):169–176. doi: 10.5664/jcsm.5478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Drake CL, Day R, Hudgel D, et al. Sleep during titration predicts continuous positive airway pressure compliance. Sleep. 2003;26(3):308–311. doi: 10.1093/sleep/26.3.308. [DOI] [PubMed] [Google Scholar]