Abstract
Study Objectives:
REM sleep behavior disorder (RBD) is a parasomnia that is commonly associated with neurodegenerative disorders. We aimed to validate the Hong Kong version of the self-reported RBD questionnaire (RBDQ-HK) with the Korean version (RBDQ-KR) and to investigate its clinical usefulness.
Methods:
One-hundred five patients with RBD and 105 age- and sex-matched controls were enrolled. Thirty were randomly selected for a retest with the questionnaire after 2 to 4 weeks without any treatment. Receiver operating characteristic curve and exploratory factor analysis were used to evaluate the scale, which had a score ranging from 0 to 100.
Results:
There was no difference in mean age and sex in patients with RBD and control subjects. Patients with RBD had a significantly higher total RBDQ-KR score than the control group (P < .001). The RBDQ-KR demonstrated high sensitivity (93.3%), specificity (89.5%), positive predictive value (89.9%), and negative predictive value (93.1%). Cronbach α coefficient for internal consistency of the total score of the RBDQ-KR was 0.9, which shows high reliability. Exploratory factor analysis showed two components, dream-related and behavioral factors, consistent with the main clinical features of RBD. Based on the results, the best cutoff for the total score ranging from 0 to 100 was at 18/19 and for factor 2 ranging from 0 to 75 was at 11.
Conclusions:
This study showed RBDQ-KR is a valid and reliable questionnaire for RBD symptoms and severity in Korea. It serves as an effective tool to identify patients with RBD and to facilitate future clinical and research studies.
Citation:
You S, Moon HJ, Do SY, Wing YK, Sunwoo JS, Jung KY, Cho YW. The REM sleep behavior disorder screening questionnaire: validation study of the Korean version (RBDQ-KR). J Clin Sleep Med. 2017;13(12):1429–1433.
Keywords: Korean, questionnaire, RBD, reliability, validity
INTRODUCTION
Rapid eye movement (REM) sleep behavior disorder (RBD) shows direct connections to abnormal movements occurring during REM sleep. Evidence can be seen from clinical studies involving REM sleep without atonia and dream enactment.1 These movements include various audible responses, uncontrollable limb twitching, and vigorous physical reactions such as kicking, punching, walking, or rolling onto the floor; therefore, the sequelae of such prominent motor activities were often associated with various sleep-related injuries in not only the patients, but also their bed partners.
Polysomnography (PSG) is generally used for the diagnosis of RBD, representing loss of REM-related muscle atonia and increased muscle tone, associated with dream-related behaviors during REM sleep.2 RBD is present in various studies with results showing a prevalence in the range of 0.38% to 0.5%.3,4 One such study specifically discussed the senior citizen population of Korea and their RBD symptoms. This study showed RBD prevalence of 2.01%, which was higher than that found in previous Western studies.5
The pathophysiology of RBD is still unclear. Evidence suggests that the first sign of possible future alpha-synucleinopathy, such as Parkinson disease,6,7 multiple system atrophy,8,9 and dementia with Lewy bodies10 is RBD. However, in non-synucleinopathy, such as Alzheimer disease,11 and frontotemporal dementia,12 RBD may rarely occur. In synucleinopathy cases, the use of disease-modifying therapies allows researchers to have a chance to analyze how RBD leads the way to identifying neurodegenerative disorders, such as Parkinson disease.13
BRIEF SUMMARY
Current Knowledge/Study Rationale: Several studies have investigated the validity of the Hong Kong version of the rapid eye movement sleep behavior disorder questionnaire (RBDQ-HK) which has been translated into other languages. This study evaluated the usefulness of the Korean version (RBDQ-KR) as a screening tool.
Study Impact: Results of this study demonstrate that RBDQ-KR is a reliable and effective screening tool for diagnosis of rapid eye movement sleep behavior disorder. This study contributes to future research into the sleep disorders and neurodegenerative disease in Korea.
The relatively high prevalence of RBD in Korea and the clinical importance of RBD as prelude to neurodegenerative disease could prompt the use of a suitable and easy-to-administer screening tool for RBD. Questionnaires are used globally in identifying the status of RBD, such as Hong Kong's development of the RBD questionnaire (RBDQ-HK). Unlike the Mayo sleep questionnaire, the RBDQ-HK contains items for checking previous 1-year frequency; therefore, this questionnaire does not neglect currency, frequency, and severity.14,15
The RBDQ-HK has been translated and validated into various languages, such as Japanese and Chinese,16,17 but not Korean. The purpose of this study was to standardize and validate the Korean version of the questionnaire and to investigate its clinical usefulness.
METHODS
This study was approved by the Institutional Ethics Committee in two regional university hospitals.
REM Sleep Behavior Disorder Questionnaire-Korean (RBDQ-KR)
The objectives of this study were explained to the patent owner of the original version of the RBDQ-HK15 and approval was given to translate the English version (questionnaire was originally developed in Chinese) into Korean to establish the first RBDQKR. For the linguistic validation process, the original RBDQHK was translated into Korean and then translated back into English to check for accuracy. The original version of RBDQHK consists of 13 items, which are designed to assess the two dimensions of RBD: lifetime occurrence and previous 1-year frequency. Total score of RBDQ-HK is 0–100, consisting of the lifetime occurrence score (0–20) and recent past frequency score over the course of 1 year (0–80).15 Through comparison of the questionnaire after being translated to Korean and retranslated to English, we prepared the Korean version of the questionnaire, the RBDQ-KR, as an original document.
Procedure and Subjects
In total, 210 subjects (105 patients with RBD and 105 age- and sex-matched controls) who visited the outpatient clinic of two university hospitals' sleep disorders centers between January 2014 and September 2016 were enrolled. Demographic factors remained consistent for the patients from the two university hospitals, Dongsan Medical Center (DSMC) and Seoul National University Hospital (SNUH). The two sleep disorder centers are located in two major cities in South Korea. Patients with RBD received a diagnosis from a sleep disorder expert in each university hospital (Y.W.C. and K.Y.J.) based on the results of PSG findings and clinical interviews according to the International Classification of Sleep Disorders, Third Edition (ICSD-3).2 The following criteria of ICSD-3 was used to diagnose RBD: (1) clinical history of problematic and harmful or potentially harmful sleep behaviors to self and/or sleep partner; and (2) polysomnographic evidence of RBD during REM sleep, including excessive augmentation of chin electro-myogram (EMG) tone or excessive chin or limb EMG phasic twitching and motor activities (eg, vocalization, simple, unclassified, or complex motor events).2
We administered the RBDQ-KR at the time of the first visit of all study participants before the PSG test. Any subject with preceding information from PSG was not evaluated by the RBDQ-KR.
The 105 controls had no previous history of sleep-related behavior episodes and overnight PSG confirmed the following sleep disorders: 69 patients with obstructive sleep apnea (OSA) (56 patients from DSMC and 18 patients from SNUH), 37 with periodic limb movement during sleep (PLMS) (31 patients from DSMC and 6 patients from SNUH), and 51 with insomnia (45 patients from DSMC and 6 patients from SNUH). In patients with OSA, 27 had severe OSA (apnea-hypopnea index [AHI] ≥ 30 events/h) (4 patients in the RBD group and 23 patients in the control group). Twenty-seven patients had severe PLMS (PLM index ≥ 50 events/h)18 (9 RBD and 18 controls).
No patient with suggestive features of RBD, non-REM parasomnia, or other neurodegenerative disorders was included as a control. Patients who were currently taking any psychotropic medications, such as antidepressants, were excluded.
An overnight polysomnography (Comet digital recording polysomnographic system, Grass-Telefactor, West Warwick, Rhode Island, United States) with video monitoring of patients' abnormal behavior during sleep, 6 electroencephalogram leads (C3-A2, C4-A1, F3-A2, F4-A1, O1-A2, and O2-A1 in the international 10–20 system), 3 EMG leads (submental and bilateral tibialis anterior), and bilateral electro-oculogram leads (ROC-A1 and LOC-A2) were tested on all of the patients in this study. In addition, several other tools were used, such as thermistors for air flow and electrocardiogram leads. In order to view nasal air pressure, an airflow pressure transducer was used. Thoracic and abdominal excursion was measured with strain gauges, snoring was recorded through the use of a microphone, and oxygen saturation was monitored with finger pulse oximetry (built-in Cometplus model, Nonin, Plymouth, Minnesota, United States). Each epoch was staged and scored according to the criteria of the 2007 American Academy of Sleep Medicine manual.19
All subjects completed the RBDQ-KR (self-reported on paper by the patient), overnight PSG study, and the Korean versions of sleep questionnaires (Insomnia Severity Index,20 Epworth Sleepiness Scale,21 and Pittsburgh Sleep Quality Index).22
We evaluated the reliability of RBDQ-KR based on results for factor 1 (dream-related factors questions 1–3, 5, and 13), factor 2 (behavioral factors questions 4 and 6–12), and the total score. In order to examine test-retest reliability, 30 of the 105 RBD subjects were randomly selected to undergo a retest at a 2- to 4-week interval without treatment.
Statistical Analysis
The results of the RBD and control groups' scores led to the reassurance of using the RBDQ-KR questionnaire in place of the ICSD-3 as a preferable and more accurate form of diagnosis. The comparison of demographic and clinical data between RBD and control groups was performed by independent t test and χ2. The psychometric properties of the questionnaire were assessed by calculating the sensitivity, specificity, positive predictive value, and negative predictive value for each threshold with a 95% confidence interval. Sensitivity and specificity were measured when considering the preferable cutoff score by using the receiver operating characteristic (ROC) curve.
Internal consistency was assessed by using Cronbach α coefficient. Test-retest reliability was analyzed by Pearson correlation coefficients and paired t test. The structural validity of the scale was confirmed through utilization of exploratory factor analysis. Data analysis was performed using SPSS version 22.0 (IBM Corp, Armonk, New York). Values of P < .05 were considered statistically significant.
RESULTS
The mean age and sex in patients with RBD [67.3 ± 6.4 years; male 57.1%] and control subjects [65.8 ± 5.7 years, male 46.7%] showed no difference. Demographic and clinical characteristics of the subjects are shown in Table 1.
Table 1.
Demographic features and clinical data.
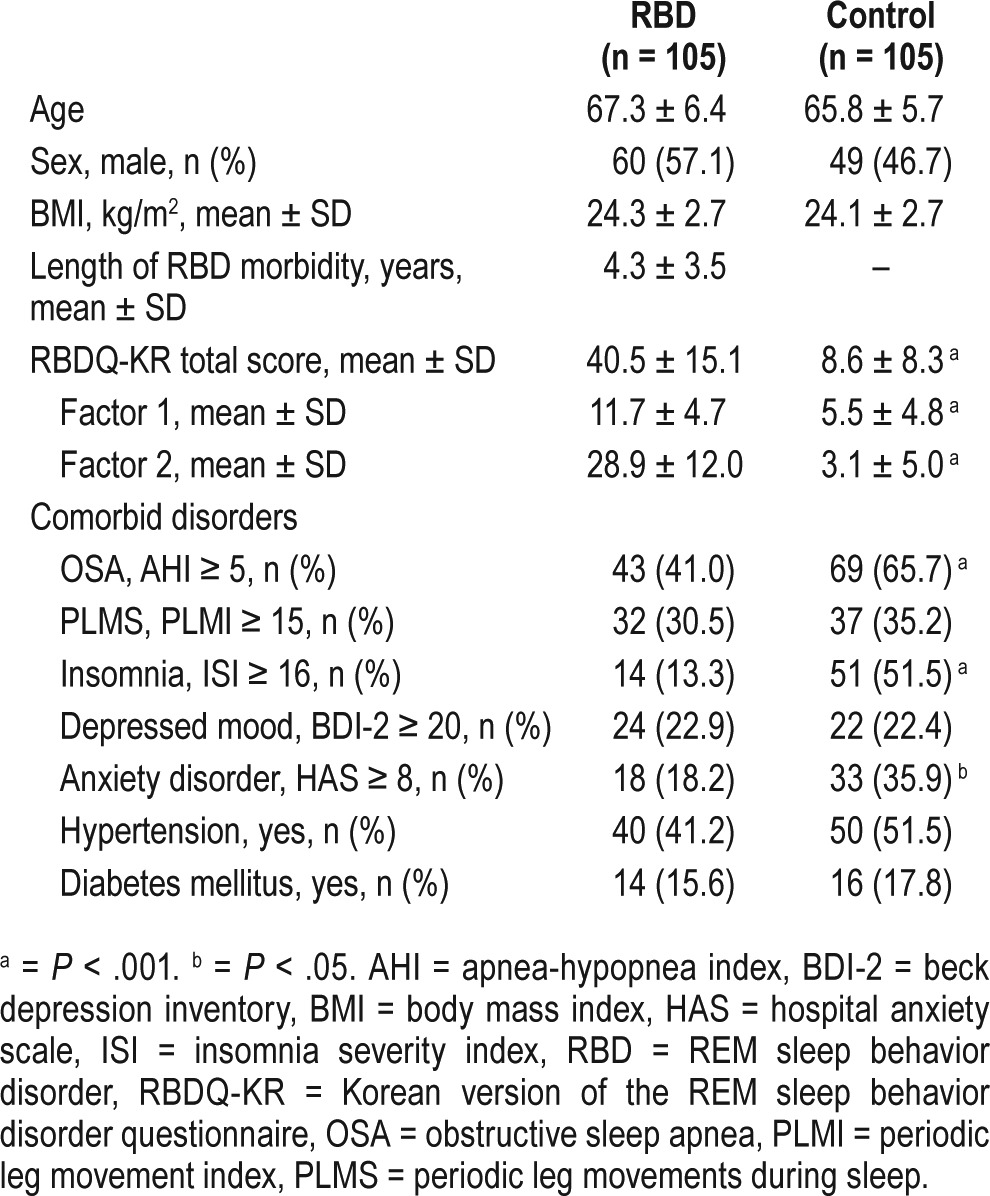
The mean duration of RBD morbidity was 4.3 ± 3.5 years. The RBD group had a significantly higher score for the RBDQKR total score (40.5 ± 15.1 versus 8.6 ± 8.3), factor 1 (11.7 ± 4.7 versus 5.5 ± 4.8), and factor 2 (28.9 ± 12.0 versus 3.1 ± 5.0) (P < .001) than the control group (Table 1). Average value of AHI was significantly lower in the RBD group than in the control group (7.1 ± 9.7 versus 15.7 ± 15.6, P < .001).
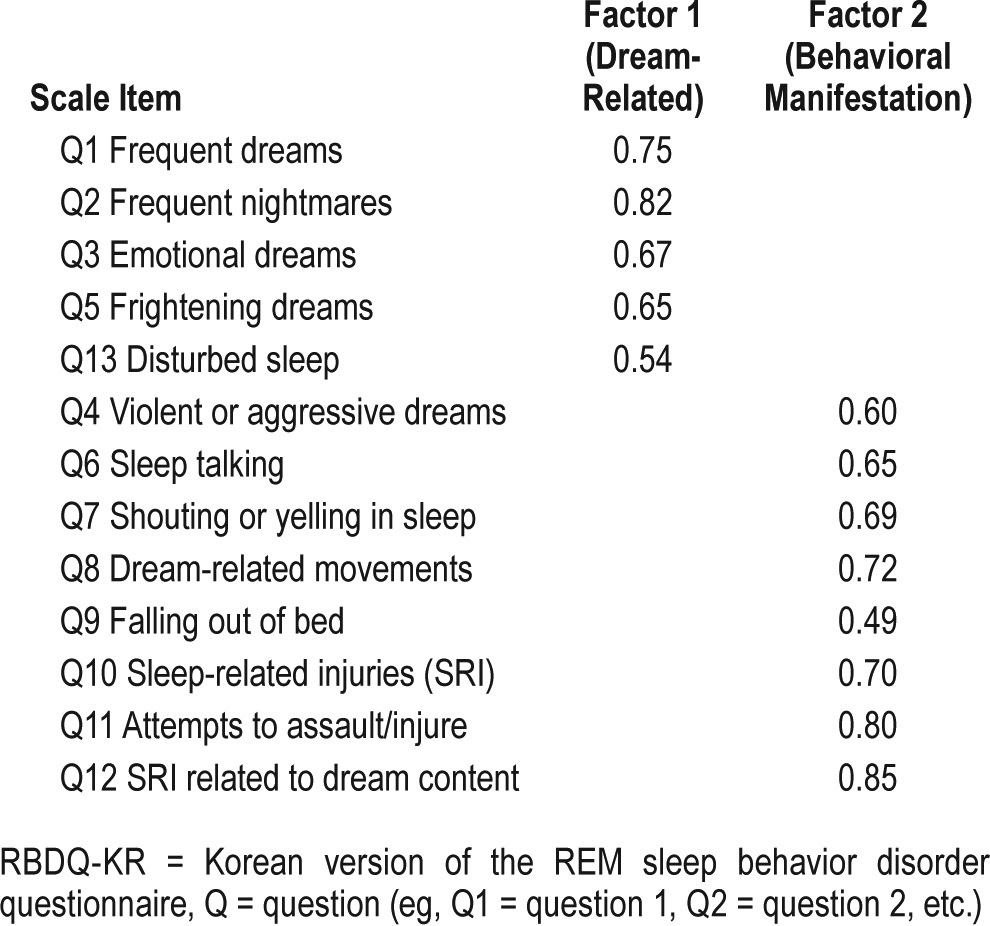
The exploratory factor analysis was deemed appropriate for the RBDQ-KR questionnaire through a 0.90 margin of error using the Kaiser-Meyer-Olkin method of measurement. Sleep symptoms were analyzed using Varimax-rotated two-factor solution as seen in Table 2, resulting in the two-factor model showing a scale variance (ie, 59.3%), with the item loading ranging from 0.49 to 0.85. Questions 1–3, 5, and 13 for factor 1 evaluated the patients' dreams while the remaining questions, 4 and 6–12, for factor 2 specified the behavioral audible and physical reactions of RBD.
Table 2.
Rotated factor loadings for the RBDQ-KR.
ROC analysis revealed that both the total score (score range of 0–100) and factor 2 (score range of 0–75) of RBDQ-KR had reliable diagnostic accuracy in all subjects (Table 3). The best cutoff values for the RBDQ-KR total score were determined to be located at 18/19 with a sensitivity of 93.3% and specificity of 89.5% (area under the curve = 0.971) in all subjects (Figure 1). The cutoff score of total score was the same at 18.5 whether the severe OSA group or PLMS group was included or excluded. In ROC analysis of total score, positive likelihood ratio was 8.909 and negative likelihood ratio was 0.074.
Table 3.
Sensitivity, specificity, PPV, and NPV at the cutoff point for the RBDQ-KR total score and factor 2.
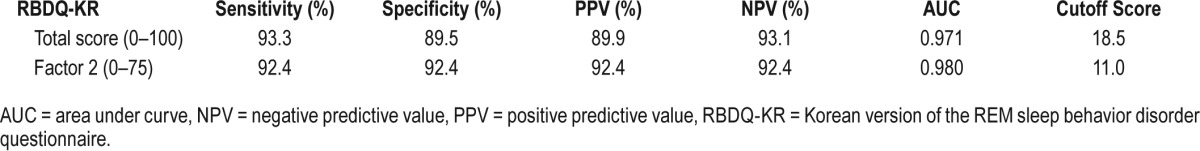
Figure 1. ROC curve for all respondents of the RBDQ-KR.
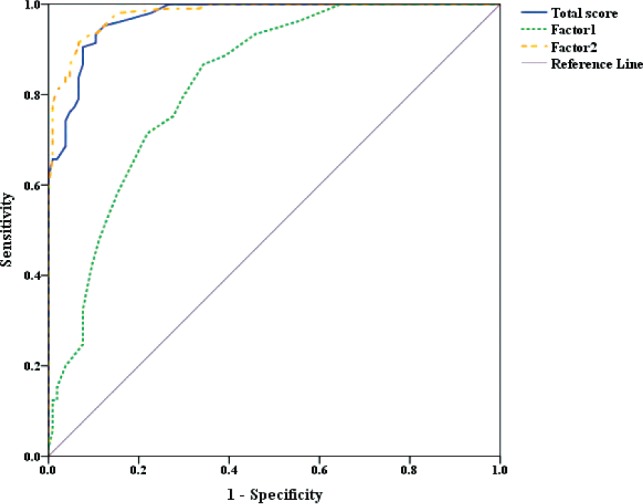
The best cutoff for total score (blue line) was located at 18.5 with a sensitivity of 93.3%, specificity of 89.5%, positive predictive value of 89.9%, and negative predictive value of 93.1% (area under the curve = 0.971). RBDQ-KR = Korean version of the REM sleep behavior disorder questionnaire, ROC = receiver operating characteristic.
For internal consistency, Cronbach α coefficient for total score was 0.90, for factor 1 (dreams-related) was 0.79, and factor 2 (behavioral manifestations) was 0.89, showing that RBDQ-KR was reliable.
Thirty patients were retested with the questionnaire (28.6%) over the course of 1 month. Reliability of the first and second rounds of tests had a total score of 0.86 (P < .001) for the RBD patients using RBDQ-KR. There were no significant differences between the scores of the test subjects at the time of the first and second tests (44.5 [15.2] and 46.3 [13.4], respectively) using the paired t test.
DISCUSSION
The RBDQ-KR questionnaire showed validity and reliability as a measure of clinical RBD symptoms and severity in Korea. The factor analysis of our RBDQ-KR questionnaire revealed a highly stable two-factor structure. Both factors corresponded to the essential clinical features as suggested by ICSD-3. Factor 1 (dream-related) identified the subjects whose dreams led to frequent dream enactment with vigorous nocturnal behaviors and sleep disruptions. Factor 2 (behavioral manifestation) revealed the behavioral aspects of a patient's sleep disorder. In this study, the compositions of the two factors were similar to the result of the original version (RBDQ-HK), but different in the Japanese version (RBDQ-JP). Compared to the Japanese version,16 our RBDQ-KR questionnaire showed higher internal consistency (coefficient alpha for the total score: 0.74 versus 0.90) and lower test-retest reliability (correlation coefficient for total score: 0.92 versus 0.86). In the case of the Japanese version, categorization of the two factors (factor 1: dream/dream-related, factor 2: violent/complex behavior) depended on the differences of complexity or strength of the behavior during sleep.16 An interesting finding was regarding the “Falling out of bed” item in factor 2 of the questionnaire showing the lowest loading in our study. This result might be caused by the low rate of the Korean elderly using beds. In fact, socioculturally, most elderly people in Korea sleep on the floor.
RBDQ-KR questionnaire had a total cutoff score of 18/19. This shows high sensitivity (93.3%), specificity (89.5%), positive predictive value (89.9%), and negative predictive value (93.1%). A previous study reported that specialized interviews for identifying RBD clinically was successful in patients without Parkinson disease with high sensitivity (100%) and specificity (99.6%).23 Unlike the results of the previous 3 studies,15–17 our study population showed similar sex proportion in the group of patients with RBD. Several reports described a higher proportion of male patients with RBD.24–26 According to one previous study, male patients with RBD mainly felt anger in dreams and had aggressive behavior, but female patients mainly experienced fear and did not act violently during dreams.27 It is possible that patients who experience less violent or nonviolent behaviors during sleep receive less attention in clinical interviews, which might lead to overlooking RBD detection in females.28 We need to consider this point when interviewing patients with RBD in clinics. Certainly, to clarify these differences between the sexes in patients with RBD, further studies are needed.
Unfortunately, RBD is easily overlooked and misdiagnosed due to the costly tests and extended periods of time needed for PSG in order to confirm its presence clinically. Interviews are a solution to these obstacles; however, those conducting such interviews require experienced clinicians to exclude other sleep-related movement disorders. To make an accurate diagnosis, the scale should be supplemental to additional clinical interviews according to the results of the high specificity and positive predictive value of the RBDQ-KR as well as PSG assessments. The questionnaire can be a reliable tool for screening, evaluation, and follow-up methods in patients with RBD symptoms with varying currency, frequency, and severity. Further validation using the Modified REM Sleep Behavior Disorder Questionnaire (RBDQ 3-month version) is preferable in providing more accurate monitoring of progress in respect to treatment.29
There are some limitations to this study. First, all participants came to the sleep clinics with sleep complaints; thus, the results might not reflect the general population. Second, incorrect information for spousal input was a potential problem because this was not included as an item in the original questionnaire, as well as differentiating the severity of RBD within that group. Third, our study included patients with severe OSA (AHI ≥ 30 events/h)30–32 and PLMS,33 who could reveal nonspecific limb movements, mimicking RBD. However, when we excluded the severe OSA group or severe PLMS group, the results were not significantly different. Fourth, this study did not include patients with non-REM parasomnia as controls; therefore, the RBDQ-KR could not demonstrate a sensibility to differentiate RBD from non-REM parasomnia. In addition, we did not calculate the amount of REM sleep without atonia and extra EMG placements were not used. Further studies will be needed to validate the RBDQ-KR in the community-based population.
The RBDQ-KR was shown to be a reliable and valid questionnaire for the use of screening and quantifying the severity of RBD in South Korea. This is useful as a screening tool to identify patients with RBD.
DISCLOSURE STATEMENT
Work for this study was performed at Dongsan Medical Center, Keimyung University School of Medicine and Seoul National University Hospital, Seoul National University College of Medicine. All authors have seen and approved the manuscript. This work was supported by the National Research Foundation of Korea (NRF) Grant funded by the Korea Government (MSIP) (No. 2014R1A5A2010008 and 2014R1A2A2A04003858). The sponsor had no role in the design or conduct of this research. The authors report no conflicts of interest.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- EMG
electromyogram
- ICSD
International Classification of Sleep Disorders
- OSA
obstructive sleep apnea
- PLMS
periodic limb movement during sleep
- PSG
polysomnography
- REM
rapid eye movement
- RBD
REM sleep behavior disorder
- RBDQ-KR
Korean version of the RBD questionnaire
- RBDQ-HK
Hong Kong version of the RBD questionnaire
- ROC
receiver operating characteristic
REFERENCES
- 1.Mahowald MW, Schenck CH. REM sleep parasomnias. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 5th ed. Philadelphia, PA: Elsevier-Saunders; 2011. pp. 1083–1097. [Google Scholar]
- 2.American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 3.Chiu HF, Wing YK, Lam LC, et al. Sleep-related injury in the elderly--an epidemiological study in Hong Kong. Sleep. 2000;23(4):513–517. [PubMed] [Google Scholar]
- 4.Ohayon MM, Caulet M, Priest RG. Violent behavior during sleep. J Clin Psychiatry. 1997;58(8):369–376. quiz 77. [PubMed] [Google Scholar]
- 5.Kang SH, Yoon IY, Lee SD, Han JW, Kim TH, Kim KW. REM sleep behavior disorder in the Korean elderly population: prevalence and clinical characteristics. Sleep. 2013;36(8):1147–1152. doi: 10.5665/sleep.2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adler CH, Hentz JG, Shill HA, et al. Probable RBD is increased in Parkinson's disease but not in essential tremor or restless legs syndrome. Parkinsonism Relat Disord. 2011;17:456–458. doi: 10.1016/j.parkreldis.2011.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Comella CL, Tanner CM, Ristanovic RK. Polysomnographic sleep measures in Parkinson's disease patients with treatment-induced hallucinations. Ann Neurol. 1993;34(5):710–714. doi: 10.1002/ana.410340514. [DOI] [PubMed] [Google Scholar]
- 8.Palma JA, Fernandez-Cordon C, Coon EA, et al. Prevalence of REM sleep behavior disorder in multiple system atrophy: a multicenter study and meta-analysis. Clin Auton Res. 2015;2(1):5, 69–75. doi: 10.1007/s10286-015-0279-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Plazzi G, Corsini R, Provini F, et al. REM sleep behavior disorders in multiple system atrophy. Neurology. 1997;48(4):1094–1097. doi: 10.1212/wnl.48.4.1094. [DOI] [PubMed] [Google Scholar]
- 10.Boeve BF, Silber MH, Ferman TJ, et al. REM sleep behavior disorder and degenerative dementia: an association likely reflecting Lewy body disease. Neurology. 1998;51(2):363–370. doi: 10.1212/wnl.51.2.363. [DOI] [PubMed] [Google Scholar]
- 11.Wang P, Wing YK, Xing J, et al. Rapid eye movement sleep behavior disorder in patients with probable Alzheimer's disease. Aging Clin Exp Res. 2016;28(5):951–957. doi: 10.1007/s40520-015-0382-8. [DOI] [PubMed] [Google Scholar]
- 12.McCarter SJ, St Louis EK, Boeve BF. Sleep disturbances in frontotemporal dementia. Curr Neurol Neurosci Rep. 2016;16(9):85. doi: 10.1007/s11910-016-0680-3. [DOI] [PubMed] [Google Scholar]
- 13.Howell MJ, Schenck CH. Rapid eye movement sleep behavior disorder and neurodegenerative disease. JAMA Neurol. 2015;72(6):707–712. doi: 10.1001/jamaneurol.2014.4563. [DOI] [PubMed] [Google Scholar]
- 14.Boeve BF, Molano JR, Ferman TJ, et al. Validation of the Mayo Sleep Questionnaire to screen for REM sleep behavior disorder in an aging and dementia cohort. Sleep Med. 2011;12(5):445–453. doi: 10.1016/j.sleep.2010.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li SX, Wing YK, Lam SP, et al. Validation of a new REM sleep behavior disorder questionnaire (RBDQ-HK) Sleep Med. 2010;11(1):43–48. doi: 10.1016/j.sleep.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 16.Sasai T, Matsuura M, Wing YK, Inoue Y. Validation of the Japanese version of the REM sleep behavior disorder questionnaire (RBDQ-JP) Sleep Med. 2012;13(7):913–918. doi: 10.1016/j.sleep.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 17.Chang Y, Gu Z, Zhan S, et al. Validation of the Beijing version of the REM sleep behavior disorder questionnaire (RBDQ-Beijing) in a mainland Chinese cohort. Tohoku J Exp Med. 2014;234(1):7–15. doi: 10.1620/tjem.234.7. [DOI] [PubMed] [Google Scholar]
- 18.Natarajan R. Review of periodic limb movement and restless leg syndrome. J Postgrad Med. 2010;56(2):157–162. doi: 10.4103/0022-3859.65284. [DOI] [PubMed] [Google Scholar]
- 19.Iber C, Ancoli-Israel S, Chesson AL, Jr, Quan SF for the American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology, and Technical Specifications. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 20.Cho YW, Song ML, Morin CM. Validation of a Korean version of the insomnia severity index. J Clin Neurol. 2014;10(3):210–215. doi: 10.3988/jcn.2014.10.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cho YW, Lee JH, Son HK, Lee SH, Shin C, Johns MW. The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath. 2011;15(3):377–384. doi: 10.1007/s11325-010-0343-6. [DOI] [PubMed] [Google Scholar]
- 22.Sohn SI, Kim DH, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012;16(3):803–812. doi: 10.1007/s11325-011-0579-9. [DOI] [PubMed] [Google Scholar]
- 23.Eisensehr I, Lindeiner H, Jager M, Noachtar S. REM sleep behavior disorder in sleep-disordered patients with versus without Parkinson's disease: is there a need for polysomnography? J Neurol Sci. 2001;186(1-2):7–11. doi: 10.1016/s0022-510x(01)00480-4. [DOI] [PubMed] [Google Scholar]
- 24.Wing YK, Lam SP, Li SX, et al. REM sleep behaviour disorder in Hong Kong Chinese: clinical outcome and gender comparison. J Neurol Neurosurg Psychiatry. 2008;79(12):1415–1416. doi: 10.1136/jnnp.2008.155374. [DOI] [PubMed] [Google Scholar]
- 25.Schenck CH, Hurwitz TD, Mahowald MW. Symposium: normal and abnormal REM sleep regulation: REM sleep behaviour disorder: an update on a series of 96 patients and a review of the world literature. J Sleep Res. 1993;2(4):224–231. doi: 10.1111/j.1365-2869.1993.tb00093.x. [DOI] [PubMed] [Google Scholar]
- 26.Olson EJ, Boeve BF, Silber MH. Rapid eye movement sleep behaviour disorder: demographic, clinical and laboratory findings in 93 cases. Brain. 2000;123(Pt 2):331–339. doi: 10.1093/brain/123.2.331. [DOI] [PubMed] [Google Scholar]
- 27.Borek LL, Kohn R, Friedman JH. Phenomenology of dreams in Parkinson's disease. Mov Disord. 2007;22(2):198–202. doi: 10.1002/mds.21255. [DOI] [PubMed] [Google Scholar]
- 28.Iranzo A, Santamaria J, Tolosa E. The clinical and pathophysiological relevance of REM sleep behavior disorder in neurodegenerative diseases. Sleep Med Rev. 2009;13(6):385–401. doi: 10.1016/j.smrv.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 29.Li SX, Lam SP, Zhang J, et al. A prospective, naturalistic follow-up study of treatment outcomes with clonazepam in rapid eye movement sleep behavior disorder. Sleep Med. 2016;21:114–120. doi: 10.1016/j.sleep.2015.12.020. [DOI] [PubMed] [Google Scholar]
- 30.Iranzo A, Santamaria J. Severe obstructive sleep apnea/hypopnea mimicking REM sleep behavior disorder. Sleep. 2005;28(2):203–206. doi: 10.1093/sleep/28.2.203. [DOI] [PubMed] [Google Scholar]
- 31.Schredl M. Snoring, breathing pauses, and nightmares. Percept Mot Skills. 2008;106(3):690–692. doi: 10.2466/pms.106.3.690-692. [DOI] [PubMed] [Google Scholar]
- 32.BaHammam AS, Al-Shimemeri SA, Salama RI, Sharif MM. Clinical and polysomnographic characteristics and response to continuous positive airway pressure therapy in obstructive sleep apnea patients with nightmares. Sleep Med. 2013;14(2):149–154. doi: 10.1016/j.sleep.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 33.Gaig C, Iranzo A, Pujol M, Perez H, Santamaria J. Periodic limb movements during sleep mimicking REM sleep behavior disorder: a new form of periodic limb movement disorder. Sleep. 2017;40(3) doi: 10.1093/sleep/zsw063. [DOI] [PubMed] [Google Scholar]


