Abstract
Continuous positive airway pressure (CPAP) is currently the reference treatment for obstructive sleep apnea (OSA). The use of a face mask, although sometimes necessary, is often associated with increased airway obstruction due to mandibular retrusion. We report a small group of patients in whom addition of a cervical collar to a face mask allowed correction of obstructive events.
Citation:
Prigent A, Grassion L, Guesdon S, Gonzalez-Bermejo J. Efficacy of the addition of a cervical collar in the treatment of persistent obstructive apneas despite continuous positive airway pressure. J Clin Sleep Med. 2017;13(12):1473–1476.
Keywords: cervicomandibular support collar, face mask, noninvasive ventilation, sleep apnea
INTRODUCTION
Obstructive sleep apnea (OSA) is a common disorder that has been associated with an increased risk of cardiovascular disease.1 Continuous positive airway pressure (CPAP) is frequently prescribed in patients with OSA and is effective in reversing hypoxemia and upper airway obstruction.
A face mask is commonly used to deliver CPAP in the case of mouth leaks, but at the price of decreased comfort and poorer quality of sleep. Moreover, because of the larger surface area of contact of the face mask, a higher leak rate around the face mask has been reported compared to nasal masks, thereby requiring tighter strapping,2 which can sometimes increase obstructive events, a phenomenon that has been reported increasingly frequently.2,3 Mandibular retrusion induced by wearing the face mask also induces retrusion of the tongue, especially when the patient lies on his or her back.4
We report 5 cases of patients treated by CPAP using a face mask, who presented with a large number of residual respiratory events despite a high positive expiratory pressure (PEP), in whom addition of a cervical collar allowed complete resolution of respiratory events with a lower PEP.
REPORT OF CASES
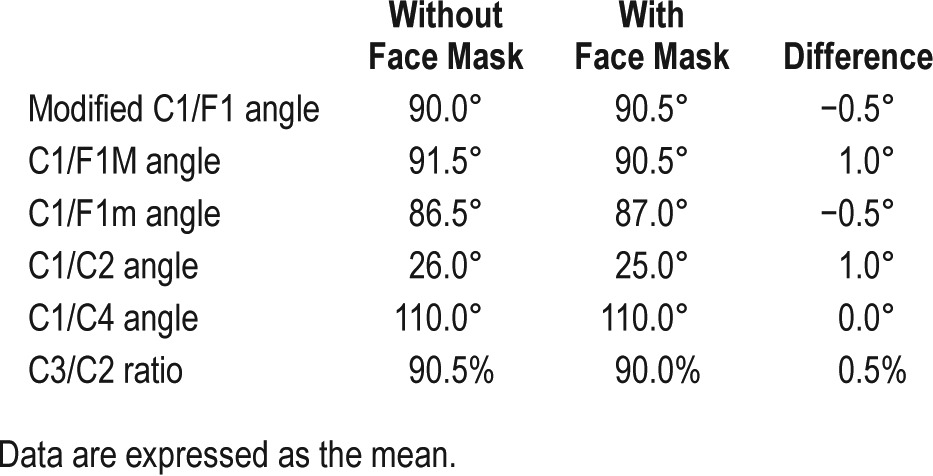
The 5 patients presented with either severe OSA requiring CPAP or hypercapnic respiratory failure requiring noninvasive ventilation (NIV). Patient characteristics are summarized in Table 1. Ear, nose, and throat examination was normal in these patients, although endoscopy was not performed. Cephalometry, performed for patients 1 and 2, did not show any mandibular retrusion in the sitting position with or without a full face mask (Table 2).
Table 1.
Patients' clinical characteristics, sleep data, and ventilator settings.
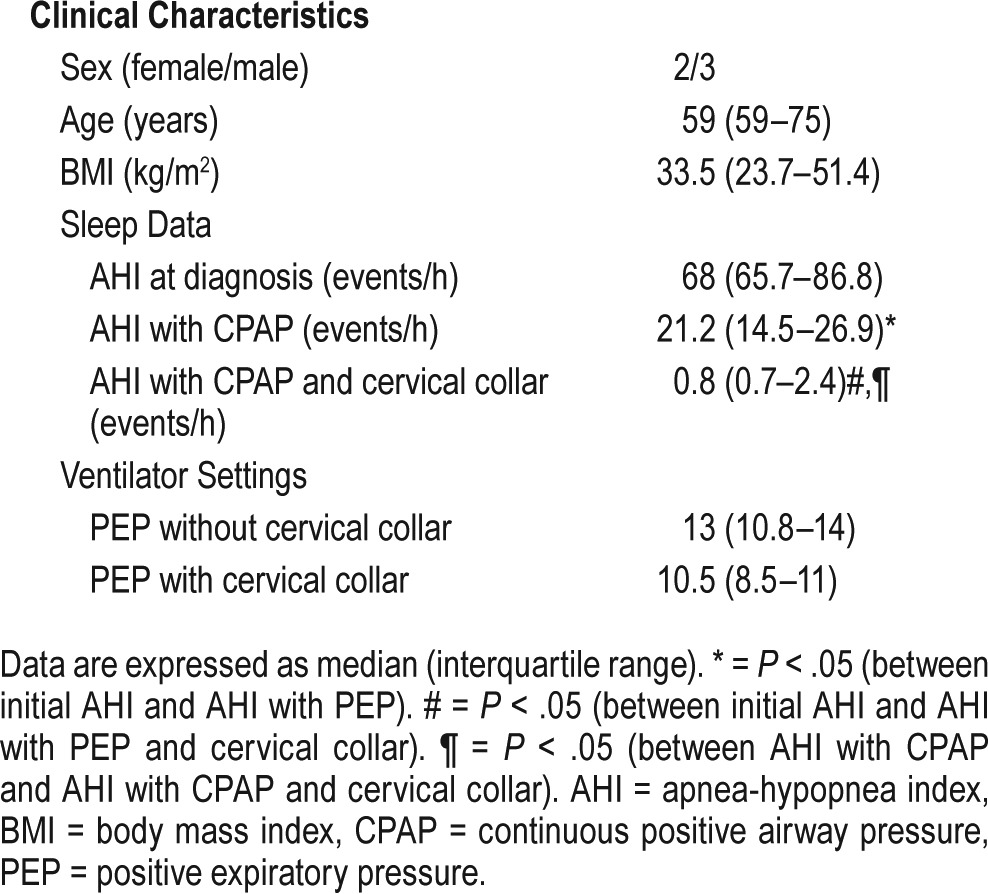
Table 2.
Delaire cephalometric analysis in patients 1 and 2.
Treatment with CPAP or NIV with full face mask was initiated in these patients who failed to tolerate a nasal mask and who experienced mouth leaks. All patients presented had a large number of residual obstructive respiratory events and failed to respond to increasing PEP up to more than 18 cm H2O.
Follow-up polygraphy on CPAP demonstrated the obstructive nature of the residual apneas. In the presence of residual events despite PEP and the normal ear, nose, and throat examination, a harmful effect of the face mask was suspected. To prevent posterior retrusion of the mandible related to the use of the face mask, addition of a cervical collar was tested (Figure 1).
Figure 1. Patient with cervical collar and continuous positive airway pressure face mask.
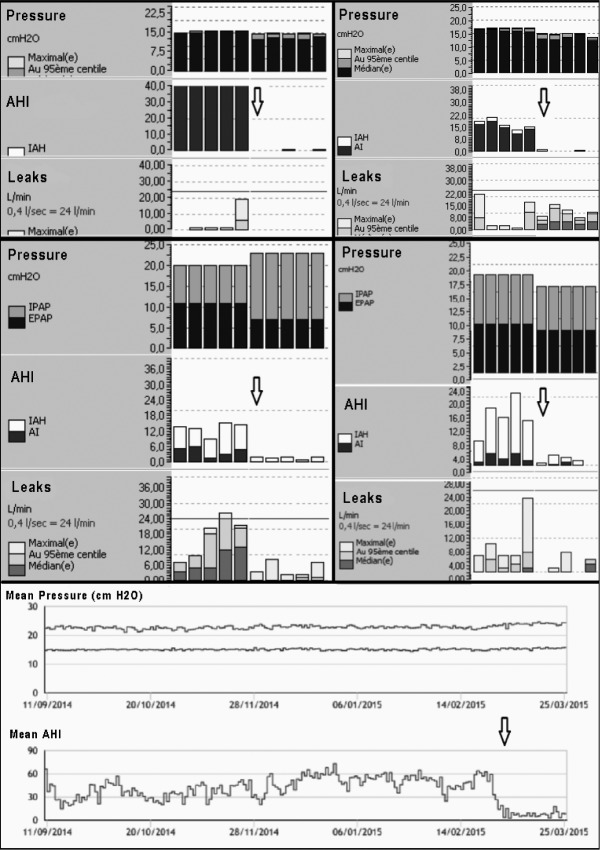
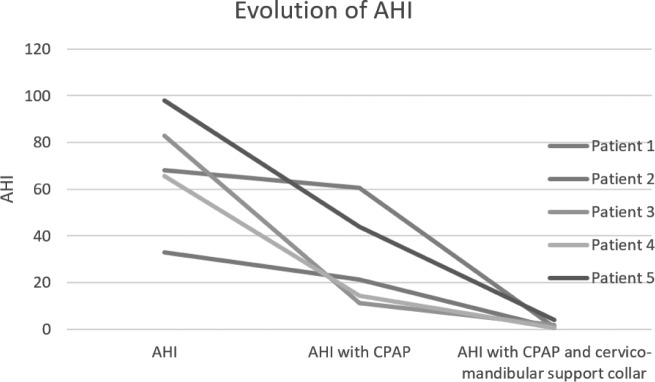
The course of respiratory parameters with the various treatments showed a reduction of the median apnea-hypopnea index (AHI) from 68 events/h at diagnosis to 21 events/h with PEP and face mask (P = .043) and to 0.8 events/h with PEP and cervical collar (P = .043), Furthermore we were able to reduce the median PEP from 13 to 10.5 cm H2O (Table 1, Figure 2, and Figure 3). All patients continued to use the cervical collar at 12 months.
Figure 2. Data obtained from continuous positive airway pressure machine software.
The arrow indicates the data obtained after introduction of the cervical collar. AHI = apnea-hypopnea index, AI = apnea index.
Figure 3. Course of AHI according to the CPAP modalities.
AHI = apnea-hypopnea index, CPAP = positive continuous airway pressure.
DISCUSSION
These 5 cases had residual obstructive respiratory events occurring with the use of a face mask and, for the first time to our knowledge, illustrate the efficacy of addition of a cervical collar, although unsuccessful use of a cervical collar has been described with NIV.5
Skinner et al.6 showed that use of a cervical collar alone was not sufficient to treat sleep apnea. Choi et al.7 showed that the position of the head influenced upper airway resistance. Neck flexion and, to a lesser extent, neck extension induce increased upper airway resistance. This mechanism could explain the efficacy of the cervical collar in the cases described here. Hiyama et al.8 reported that use of a cervical collar decreased mouth opening without inducing any anteroposterior displacement of the mandible. The sagittal dimension of the upper airway is reduced by wearing a cervical collar, with no change in the vertical dimension. The hyoid bone and third vertebra are displaced anteriorly when wearing a cervical collar.
Most importantly, a cervical collar induces counterclockwise rotation of the mandible, which decreases mouth opening and stabilizes the mandible anteroposteriorly, maintaining the head of the mandible deep in the mandibular fossa, which could explain why mandibular retrusion is not observed in this position when wearing a face mask. This is the main reason why we chose to use a cervical collar rather than a chin strap, which would certainly be more comfortable, reduces mouth leaks, and is associated with better adherence,9 but, to our knowledge, does not induce this counterclockwise rotation of the mandible. Moreover, a chin strap was tried unsuccessfully in a patient treated with NIV.
This study presents a number of limitations. Apart from the small number of cases in this series, we were unable to demonstrate why addition of a cervical collar eliminated the residual obstructive apneas.
A previous study has shown that the position of the mandible varies during the various stages of sleep.10 However, the radiographies performed in our patients, in the sitting position and while awake, did not demonstrate any signs of mandibular retrusion induced by the face mask, but this may not have been the best examination to elucidate the mechanism. Cine magnetic resonance imaging examinations could be useful in this setting.11
Another possible mechanism is epiglottic obstruction, which may be avoided by wearing the cervical collar by maintaining the neck in neutral position. Endoscopy with and without a face mask and with and without a cervical collar in awake and sleeping patients could help determine underlying mechanisms.
The side effects of wearing a cervical collar at night were not evaluated in this study. Georges et al.5 reported that the use of a cervical collar associated with a face mask was poorly tolerated in the long term, but their study concerned patients with neuromuscular disease with associated head and neck disease treated with NIV. All patients in our series continued to use the cervical collar and face mask after 12 months of follow-up.
Finally, the number of patients in whom this treatment was a failure cannot be determined in the absence of a prospective study. A randomized controlled trial would be necessary to address these issues, but in view of the major public health problem of OSA, the low cost and completely noninvasive and simple nature of a trial of cervical collar, we believe that our results should be sufficient to propose a cervical collar in the OSA treatment algorithm in the case of failure of high PEP, requiring the use of a face mask. We have now integrated this step into our routine management.
CONCLUSIONS
Although we have not fully elucidated the mechanism, we report, for the first time, that the use of a cervical collar can constitute a useful contribution to reduce obstructive events in patients requiring the use of a face mask for CPAP or NIV. We believe that a cervical collar should now be proposed to all patients requiring a face mask with persistent obstructive apneas despite high PEP.
DISCLOSURE STATEMENT
AP, LG, SG, and JGB all declare to have no conflicts of interest. The authors declare that they have obtained informed consent from the patient who is identifiable in Figure 1.
ACKNOWLEDGMENTS
The authors thank the GAV (Groupe Ventilatoire Assistance) of the Société de Pneumologie de Langue Française for funding the English translation of this article and Anthony Saul for the translation. Author contributions: AP, LG, and JGB contributed to writing of the manuscript. AP and SG contributed to data collection. All authors participated in data analysis and final approval of the manuscript.
REFERENCES
- 1.Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3(4):310–318. doi: 10.1016/S2213-2600(15)00043-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bakker JP, Neill AM. Nasal versus oronasal continuous positive airway pressure masks for obstructive sleep apnea: a pilot investigation of pressure requirement, residual disease, and leak. Sleep Breath. 2012;16(3):709–716. doi: 10.1007/s11325-011-0564-3. [DOI] [PubMed] [Google Scholar]
- 3.Bettinzoli M, Taranto-Montemurro L, Messineo L, et al. Oronasal masks require higher levels of positive airway pressure than nasal masks to treat obstructive sleep apnea. Sleep Breath. 2014;18(4):845–849. doi: 10.1007/s11325-014-0954-4. [DOI] [PubMed] [Google Scholar]
- 4.Nascimento JA, de Santana Carvalho T, Moriya HT, et al. Body position may influence oronasal CPAP effectiveness to treat OSA. J Clin Sleep Med. 2016;12(3):447–448. doi: 10.5664/jcsm.5602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Georges M, Attali V, Golmard JL, et al. Reduced survival in patients with ALS with upper airway obstructive events on non-invasive ventilation. J Neurol Neurosurg Psychiatry. 2016;87(10):1045–1050. doi: 10.1136/jnnp-2015-312606. [DOI] [PubMed] [Google Scholar]
- 6.Skinner MA, Kingshott RN, Jones DR, Taylor DR. Lack of efficacy for a cervicomandibular support collar in the management of obstructive sleep apnea. Chest. 2004;125(1):118–126. doi: 10.1378/chest.125.1.118. [DOI] [PubMed] [Google Scholar]
- 7.Choi J-K, Goldman M, Koyal S, Clark G. Effect of jaw and head position on airway resistance in obstructive sleep apnea. Sleep Breath. 2000;4(4):163–168. doi: 10.1007/s11325-000-0163-1. [DOI] [PubMed] [Google Scholar]
- 8.Hiyama S, Tsuiki S, Ono T, Kuroda T, Ohyama K. Effects of mandibular advancement on supine airway size in normal subjects during sleep. Sleep. 2003;26(4):440–445. doi: 10.1093/sleep/26.4.440. [DOI] [PubMed] [Google Scholar]
- 9.Knowles SR, O'Brien DT, Zhang S, Devara A, Rowley JA. Effect of addition of chin strap on PAP compliance, nightly duration of use, and other factors. J Clin Sleep Med. 2014;10(4):377–383. doi: 10.5664/jcsm.3608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hiyama S, Ono T, Ishiwata Y, Kuroda T. Changes in mandibular position and upper airway dimension by wearing cervical headgear during sleep. Am J Orthod Dentofac Orthop. 2001;120(2):160–168. doi: 10.1067/mod.2001.113788. [DOI] [PubMed] [Google Scholar]
- 11.Chan ASL, Sutherland K, Schwab RJ, et al. The effect of mandibular advancement on upper airway structure in obstructive sleep apnoea. Thorax. 2010;65(8):726–732. doi: 10.1136/thx.2009.131094. [DOI] [PubMed] [Google Scholar]