Abstract
Rift Valley fever (RVF) is a mosquito-borne zoonotic disease endemic to Africa and the Arabian Peninsula that affects sheep, cattle, goats, camels, and humans. Effective vaccination of susceptible ruminants is important for the prevention of RVF outbreaks. Live-attenuated RVF vaccines are in general highly immunogenic in ruminants, whereas residual virulence might be a concern for vulnerable populations. It is also important for live-attenuated strains to encode unique genetic markers for the differentiation from wild-type RVFV strains. In this study, we aimed to strengthen the attenuation profile of the MP-12 vaccine strain via the introduction of 584 silent mutations. To minimize the impact on protective efficacy, codon usage and codon pair bias were not de-optimized. The resulting rMP12-GM50 strain showed 100% protective efficacy with a single intramuscular dose, raising a 1:853 mean titer of plaque reduction neutralization test. Moreover, outbred mice infected with one of three pathogenic reassortant ZH501 strains, which encoded rMP12-GM50 L-, M-, or S-segments, showed 90%, 50%, or 30% survival, respectively. These results indicate that attenuation of the rMP12-GM50 strain is significantly attenuated via the L-, M-, and S-segments. Recombinant RVFV vaccine strains encoding similar silent mutations will be also useful for the surveillance of reassortant strains derived from vaccine strains in endemic countries.
Keywords: Rift Valley fever phlebovirus, MP-12 vaccine, attenuation, silent mutation, protective efficacy, reverse genetics
1. Introduction
Rift Valley fever (RVF) is a mosquito-borne zoonotic disease that affects sheep, cattle, goats, camels, and humans [1]. The causative agent, Rift Valley fever phlebovirus (RVFV) belongs to the genus Phlebovirus within the family Phenuiviridae, in the order Bunyavirales. The RVFV genome is comprised of three negative-sense or ambi-sense RNA: the Large (L)-, Medium (M)-, and Small (S)-segments. The L-segment encodes RNA-dependent RNA polymerase (L protein), whereas the M-segment encodes envelope glycoproteins Gn and Gc, as well as 78kD and NSm proteins. The S-segment encodes nucleoprotein (N protein) and nonstructural S (NSs) protein. Following RVFV infection, abortions and fetal malformations occur in most pregnant ruminants, whereas newborn lambs and goat kids show high mortalities due to acute viral hepatitis. RVFV infection in humans occurs via a bite from an infected mosquito or exposure to bodily fluid of infected animals [2]. Typically, RVF patients show a biphasic fever followed by spontaneous recovery, whereas severe cases suffer from hemorrhagic fever, encephalitis, or retinitis [3]. Due to the grave consequences of RVF outbreaks upon introduction into non-endemic countries, RVFV is classified as a Category A Priority Pathogen, and an overlap select agent via the U.S. Department of Health and Human Services, and Agriculture [4]. Since the first reported RVF outbreak in Kenya in 1930, the geographical distribution of RVFV has expanded into Saudi Arabia and Yemen, and many countries in Africa [5–8]. Effective vaccination of susceptible animals and humans at high risk of viral exposure is one of the most important approaches to minimizing the impact of RVF outbreaks [9, 10]. In endemic countries, both live-attenuated vaccines (Smithburn or Clone 13 vaccine) and inactivated vaccines are commercially available for veterinary use [11, 12]. Preparation of a national vaccine stockpile is also important for non-endemic countries. In the U.S., a live-attenuated MP-12 vaccine was conditionally licensed for veterinary use upon RVF outbreaks based on the protective efficacy and demonstrated safety in ruminants [13–19]. There are currently no licensed RVF vaccines or therapeutics available for humans.
Live-attenuated RVF vaccines show strong protective efficacies in ruminants following a single dose without adjuvants. Since those vaccine strains replicate in vaccinated animals, residual virulence might be a concern for vulnerable populations, including pregnant or newborn animals [13, 20]. Although subunit vaccines, DNA vaccines, viral vectors, and single-cycle RVF replicons are highly safe in animals due to a lack of viral spread, the vaccine immunogenicity of these novel candidates is not as high as traditional live-attenuated vaccines, and a booster dose and/or the use of adjuvant might be required to induce a long-term protective immunity [21–24]. Recently, we created a recombinant MP-12 strain, which encodes hundreds of silent mutations throughout the open reading frame (ORF) of genomic RNA (rMP12-GM50 strain)[25]. The rMP12-GM50 strain is potentially valuable as a novel candidate vaccine, because silent mutations might strengthen the attenuation profile of MP-12 strain via the L-, M-, and S-segments, and also serve as genetic markers to be distinguished from other RVFV strains. In this study, we aimed to characterize the attenuation profile and protective efficacy of rMP12-GM50 strain compared to those of parental MP-12 strain.
2. Materials and Methods
2.1. Media, cells, and viruses
BHK/T7-9 cells stably expressing T7 RNA polymerase [26] were cultured at 37°C with5% CO2 in minimum essential medium (MEM)-alpha containing 10% fetal bovine serum (FBS), penicillin (100 U/ml), streptomycin (100 μg/ml), and hygromycin B (600 μg/ml). MRC-5 cells (ATCC CCL-171), Vero cells (ATCC CCL-81), and VeroE6 cells (ATCC CRL-1586) were cultured at 37°C with 5% CO2 in Dulbecco’s modified MEM containing 10% FBS, penicillin (100 U/ml), and streptomycin (100 μg/ml). BHK/T7-9, MRC-5, Vero, and Vero E6 cells were verified to be mycoplasma free (UTMB Tissue Culture Core Facility), and the identity of MRC-5 cells was authenticated via Short Tandem Repeat analysis (UTMB Molecular Genomics Core Facility). The MP-12 vaccine Lot 7-2-88 was amplified once in MRC-5 cells and used in this study. Recombinant MP-12 (rMP-12) or ZH501 (rZH501) strains was recovered from BHK/T7-9 cells via reverse genetics, and passaged once in VeroE6 cells [27, 28]. A rMP-12 variant encoding a total of 584 silent mutations within the N, NSs, M, and L ORFs (the rMP12-GM50 strain) was also recovered via reverse genetics (GenBank Accession No. MF593928, MF593929, MF593930) as described previously [25]. Reassortant rZH501 strains encoding either rMP12-GM50 L-segment (RST-GM50-L), rMP12-GM50 M-segment (RST-GM50-M), or rMP12-GM50 S-segment (RST-GM50-S) were generated via reverse genetics. Rescued viruses were amplified in Vero cells after recovery from BHK/T7-9 cells, and stock viruses were titrated via a plaque assay using Vero E6 cells [28].
2.2. Plasmids
Plasmids expressing positive-sense RNA of rMP12-GM50 L, M-, and S-segments via the T7 promoter, i.e. pProT7-vL(+)-GM50, pProT7-vM(+)-GM50, and pProT7-vS(+)-GM50, respectively, were described previously [25]. Briefly, silent mutations of the rMP12-GM50 strain were manually designed one by one, so as not to disturb the codon pair bias and codon usage, at least in humans [29, 30]. One or more silent mutations were introduced every 50 nucleotides; this could serve as a gene marker of this strain and was thus designated as gene marker 50 (GM50).
2.3. Growth kinetics of rMP-12 or rMP12-GM50 in culture cells
Vero or MRC-5 cells in 12-well culture plates were infected with the rMP-12 or rMP12-GM50 strain at 0.01 multiplicity of infection (MOI) at 37°C for 1 hour. After washing cells three times with media, culture supernatants at 1 hour post infection (hpi) were collected. Cells were further incubated at 37°C, and culture supernatants were collected at 24, 48, 72, 96, and 144 hpi. Experiments were performed three times independently.
2.4. Mouse challenge experiments with rZH501 and the reassortant strains
Five-week-old female outbred CD1 mice (Charles River, North Franklin, CT) were inoculated with 1×103 plaque forming units (PFU) of parental rZH501 (control, n = 5 per group), RST-GM50-L, RST-GM50-M, or RST-GM50-S (n = 10 per group) via the intraperitoneal route (i.p.). Clinical signs of disease were observed daily, and individual body weights were measured daily for seven days, and then subsequently every three days until termination of the experiment at 21 days post challenge. Mice showing more than 20% body weight loss and/or showing clinical signs such as viral encephalitis or severe lethargy were humanely euthanized, and all surviving mice were euthanized at 21 days post challenge. All work with infectious rZH501 was performed at the Robert E. Shope BSL-4 laboratory or Galveston National Laboratory at UTMB.
2.5. Protective efficacy experiments
Protective efficacy experiment 1
Five-week-old female outbred CD1 mice (Charles River) were inoculated subcutaneously (s.c.) with PBS (mock, n = 5), or 1×104 or 1×105 PFU of parental MP-12 or the rMP12-GM50 strain (n = 10 per group). Serum samples were collected via the retro-orbital vein at 43 days post vaccination (dpv). Mice were then subsequently challenged with 1×103 PFU of pathogenic rZH501 strain via i.p. route at 45 dpv. Mice were observed daily for 21 days after challenge, and individual body weights were measured daily for seven days, and then subsequently every three days until termination of the experiment at 21 days post challenge. Sera were then collected from surviving mice at 21 days post rZH501 challenge via the cardiac puncture. Survival curves of mice (Kaplan-Meyer method) were analyzed using the GraphPad Prism 6.05 program (GraphPad Software Inc, La Jolla, CA.).
Protective efficacy experiment 2
Five-week-old female outbred CD1 mice were inoculated s.c. or intramuscularly (i.m.) with PBS (s.c.: n = 5; i.m.: n = 5), or 5×105 PFU of parental MP-12 or the rMP12-GM50 strain (s.c.: n = 10 per group; i.m.: n = 10 per group). Serum samples were collected via the retro-orbital vein at 42 dpv. Mice were then subsequently challenged with 1×103 PFU of pathogenic rZH501 strain (i.p.) at 45 dpv as described above.
2.6. Plaque Reduction Neutralization Test
The plaque reduction neutralization test (PRNT80) titer was determined as described previously [31]. Briefly, each 20-μl aliquot of mouse serum, serially diluted four-fold, was transferred into flat-bottom 96-well plates containing MP-12 virus, in which 50 plaques were formed per well (final dilutions of sera mixed with viral input were 1:10, 1:40, 1:160, 1:640, 1:2,560, and 1:10,240). After incubation at 37°C for 1 hour, 150 μl of DMEM with 10% FBS was added to each well. Next, 150 μl of the mixture was transferred into a 24-well plate with subconfluent VeroE6 cells, and the plate was further incubated at 37°C for 1 hour. After removal of inocula, cells were covered with an overlay containing 0.3% tragacanth gum, 1xMEM, 5% FBS, 5% triphosphate broth, streptomycin, and penicillin, and then further incubated for 72 hours. Cells were fixed with 25% formalin and 5% ethanol containing crystal violet. The average number of plaques from at least five different wells that had mock-immunized mice sera was used to set the cut-off number of 80% reduction. The highest dilution of sera that inhibited the plaque formation below the cut-off number was used for the PRNT80.
2.7. Statistical analysis
Statistical analyses were conducted using the GraphPad Prism 6.05 program (GraphPad Software Inc.). Arithmetic means of log10 values of virus titers were analyzed by one-way ANOVA followed by Tukey’s multiple comparison test.
2.8. Ethics statement
Experiments using the RVFV ZH501 strain, MP-12 strain, recombinant MP-12 strains, and rMP12-GM50 strain were performed with the approval of the Notification of Use by the Institutional Biosafety Committee at UTMB. Mouse experiments were conducted in facilities accredited by the Association for Assessment and Accreditation of Laboratory Animal Care, in accordance with the Animal Welfare Act, NIH guidelines, and U.S. federal law. Animal protocols were approved via the UTMB Institutional Animal Care and Use Committee, Protocol number 1007038A.
3. Results
3.1. Introduction of silent mutations into N, NSs, M, and L ORFs of the RVFV MP-12 strain
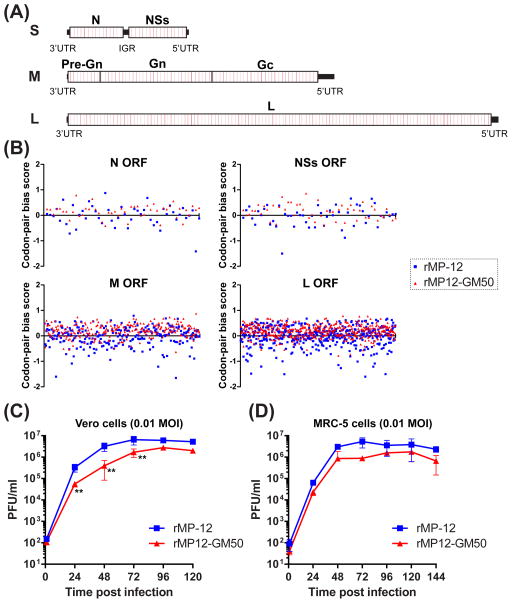
To introduce additional attenuations and gene markers into the MP-12 vaccine strain without changing the functions of viral proteins, a total of 584 silent mutations were introduced into the ORFs of the MP-12 strain. Specifically, 326 mutations were introduced in the L-segment, 185 mutations in the M-segment, and 73 mutations in the S-segment (Fig. 1A). The MP-12 variant was successfully rescued via the reverse genetics system, and the resulting virus was designated as rMP12-GM50. Each silent mutation was designed to not disturb codon-pair bias (Fig. 1B) and codon usage in order to retain the capability of viral replication in host cells [29]. The codon pair bias represents the bias of the pairing frequency of two neighboring codons within the species [32, 33]. The biological role of codon pair bias was previously studied via calculating the codon pair bias score using annotated human genes: i.e., the underrepresented pair and overrepresented pair were shown as scores of <0 and >0, respectively [29]. The average codon pair bias scores (humans) of parental rMP-12 and rMP12-GM50 were −0.018 and 0.189, respectively, whereas the codon adaptation index (humans) of parental rMP-12 and rMP12-GM50 were 0.72 and 0.73, respectively (data not shown) [30, 34]. The nucleotide homology between the parental MP-12 strain and the rMP12-GM50 strain was 94.9% (L-segment), 95.2% (M-segment), and 96.0% (S-segment). The replication efficiencies of rMP-12 and rMP12-GM50 were evaluated in Vero and MRC-5 cells. Replication of the rMP12-GM50 strain was less efficient than that of the parental rMP-12 strain in Vero cells at 24, 48, and 72 hpi, yet the viral titers at 96 and 120 hpi had no significant difference from those of the parental strain (Fig. 1C). Replication kinetics of the rMP12-GM50 strain were not statistically significantly different from those of the parental rMP-12 strain in MRC-5 cells (Fig. 1D), indicating that the rMP12-GM50 strain retains the ability to replicate in mammalian cells.
Fig. 1. Generation of the rMP12-GM50 strain of Rift Valley fever phlebovirus.
(A) Schematics of the genomic structure of the rMP12-GM50 strain. Silent mutations (red lines) were introduced every 50 nucleotides within each open reading frame (ORF). (B) The codon-pair bias scores in humans [29] at each codon within the ORFs for N, NSs, M, and L were individually plotted onto graphs. The X-axis represents the nucleotide position numbers. Blue square = rMP-12; red triangle = rMP12-GM50. (C) Replication kinetics of rMP-12 and rMP12-GM50 in Vero cells (left panel) and MRC-5 cells (right panel) at 0.01 MOI. Graph represents the means +/− standard deviations of three independent experiments. Blue square = rMP-12; red triangle = rMP12-GM50.
3.2. Attenuation of pathogenic recombinant ZH501 strain through the L, M-, or S-segments of the rMP12-GM50 strain
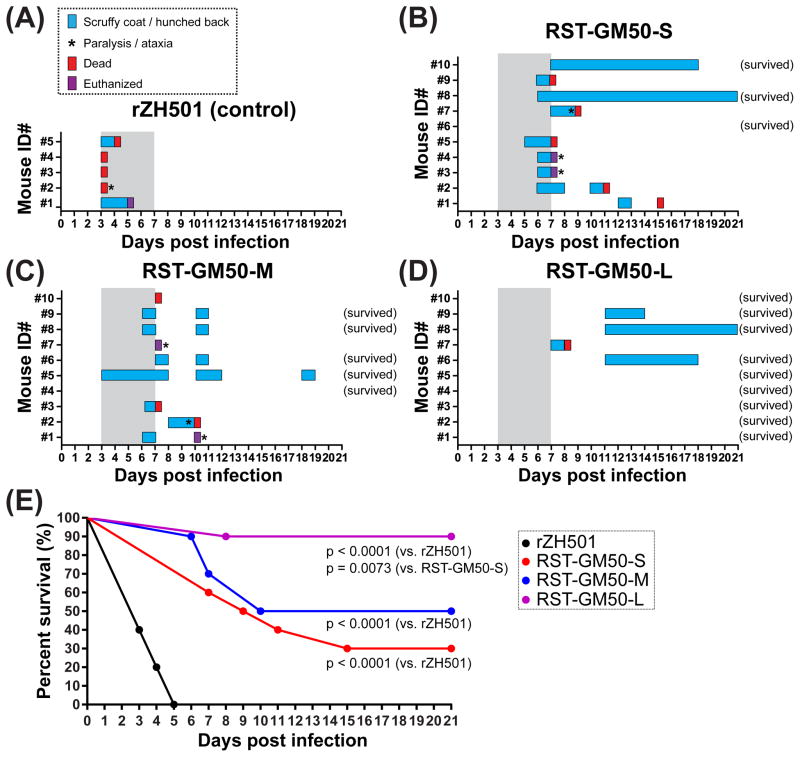
Although the parental MP-12 strain encodes attenuation mutations in the L-, M-, and S-segments, each segment only partially contributes to the attenuation of RVFV [35]. Previous study showed 20%, 40%, and 0% survival of mice via an i.p. challenge with 1×103 PFU of reassortant rZH501 strain encoding either the L-, M-, or S-segment of the parental MP-12 strain (RST-MP12-L, RST-MP12-M, and RST-MP12-S), respectively (Table 1) [35]. To evaluate the attenuation via each segment, reassortant rZH501 strains encoding either the L-, M-, or S-segment of the rMP12-GM50 strain were generated in this study (Table 1). In the challenge experiment of outbred mice with rZH501 or reassortant strains, all mice infected with parental rZH501 strain died or euthanized due to severe clinical signs within 5 days post infection (dpi) (Fig. 2A). Nine out of ten mice infected with RST-GM50-S showed scruffy coat or hunched back starting at 5 – 12 dpi, and three mice also showed neurological signs such as paralysis or ataxia at 7 or 8 dpi (Fig. 2B). Similarly, nine out of ten mice infected with RST-GST-M showed scruffy coat or hunched back starting at 3 – 8 dpi, and three mice showed paralysis or ataxia at 7, 9, or 10 dpi (Fig. 2C). In contrast, three out of ten mice infected with RST-GM50-L showed scruffy coat or hunched back starting at 11 dpi, and one mouse died at 8 dpi (Fig. 2D). Survival rates of mice infected with rZH501, RST-L, RST-M, and RST-S over 21 days were 0%, 90%, 50%, and 30%, respectively (Fig. 2E, Table 1). Survival curves RST-GM50-L, RST-GM50-M, or RST-GM50-S groups were significantly different from that of control rZH501 group (Log-rank test, p < 0.0001). Moreover, the survival curves of RST-GM50-L and RST-GM50-S groups were also significant different (Log-rank test, p = 0.0073).
Table 1.
Reassortant strains between rZH501 and either rMP-12 or rMP12-GM50
| Reassortant strains | L-segment | M-segment | S-segment | Mouse survival (%)* |
|---|---|---|---|---|
| RST-MP12-L | rMP-12 | rZH501 | rZH501 | 20** |
| RST-MP12-M | rZH501 | rMP-12 | rZH501 | 40** |
| RST-MP12-S | rZH501 | rZH501 | rMP-12 | 0** |
| RST-GM50-L | rMP12-GM50 | rZH501 | rZH501 | 90 |
| RST-GM50-M | rZH501 | rMP12-GM50 | rZH501 | 50 |
| RST-GM50-S | rZH501 | rZH501 | rMP12-GM50 | 30 |
Survival of outbred CD1 mice with 1×103 PFU dose via intraperitoneal inoculation
Cited from [35].
Fig. 2. Survival of mice infected with the parental rZH501 strain of Rift Valley fever phlebovirus or its reassortants with the rMP12-GM50 strain.
Outbred CD1 mice were intraperitoneally mock-infected with PBS or infected with 1×103 PFU of parental rZH501 (n = 5), or the reassortant strains RST-GM50-L, RST-GM50-M, or RST-GM50-S (n = 10 per group). (A – D) Clinical signs of disease observed in each mouse infected with rZH501 (A), RST-GM50-S (B), RST-GM50-M (C), or RST-GM50-L are shown. Blue = scruffy coat and/or hunched back; red = dead; purple = euthanized; asterisk = paralysis and/or ataxia; gray shadowing = typical period of disease in parental rZH501-infected mice [35]. (F) The Kaplan-Meier survival curve of infected mice. Statistically significant differences based on log-rank testing among groups are also shown.
3.3. Protective efficacy of the rMP12-GM50 strain via the subcutaneous route
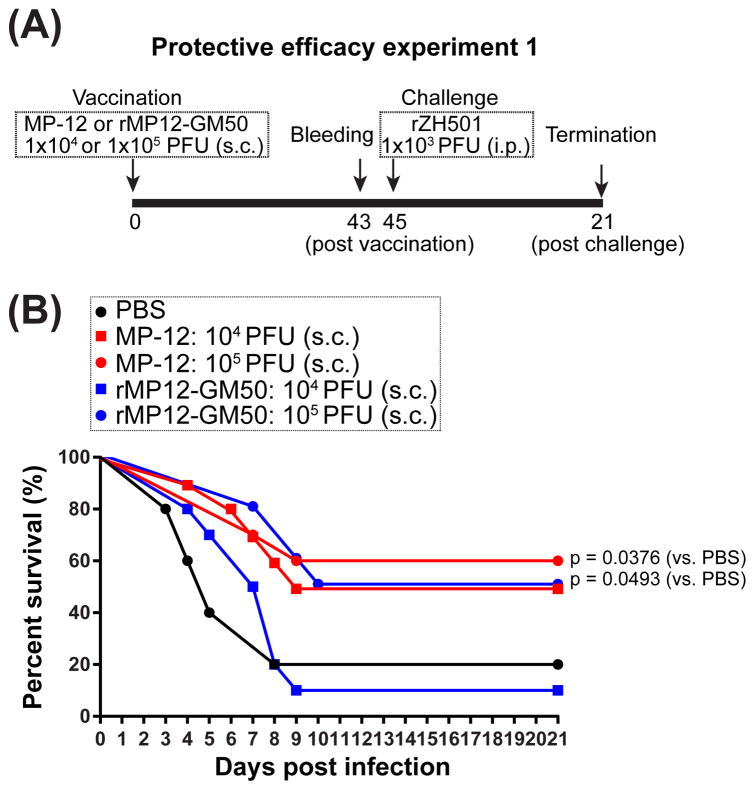
Next, the protective efficacy of the rMP12-GM50 strain was tested in comparison with that of the parental MP-12 strain. Since previous efficacy experiments using the MP-12 strain were performed via s.c. route [16, 17, 19, 31, 36], the protective efficacy of the MP-12 and rMP12-GM50 strains were first tested via s.c. using 1×104 and 1×105 PFU doses (protective efficacy experiment 1) (Fig. 3A). Vaccination with 1×104 or 1×105 PFU doses parental MP-12 strain resulted in an increase of PRNT80 neutralizing antibody titers to 1:40 or higher in 20% or 40% of vaccinated mice, respectively, at 43 days post vaccination (Figs. S1A and S1C). Similarly, vaccination with 1×104 or 1×105 PFU doses rMP12-GM50 strain resulted in an increase of PRNT80 titers to 1:40 or higher in 10% or 50% of vaccinated mice, respectively (Figs. S1B and S1D). Followed by a challenge with pathogenic rZH501 strain at 45 days post vaccination, four of five (80%) mock (PBS)-vaccinated mice died within 8 days post rZH501 strain challenge (Fig. 3B). Vaccination with 1×104 or 1×105 PFU of parental MP-12 strain resulted in 50% or 60% survival of mice after rZH501 challenge, respectively (Fig. 3B). Mice vaccinated with 1×104 or 1×105 PFU of rMP12-GM50 strain resulted in 10% or 50% survival after rZH501 challenge, respectively (Fig. 3B). The survival curves of MP-12 1×105 PFU dose group and rMP12-GM50 1×105 PFU dose group showed marginal differences from that of mock-vaccinated group (Log-rank test, p = 0.0376 and p = 0.0493, respectively).
Fig. 3. Protective efficacy experiment 1: vaccination with subcutaneous route.
(A) Schematic representation of vaccination and challenge schedule for the protective efficacy experiment 1. Outbred CD1 mice mock-vaccinated via subcutaneous route (s.c.) with PBS (n = 5), or vaccinated via s.c. with 1×104 PFU or 1×105 PFU of MP-12 (n = 10 per group) or rMP12-GM50 (n = 10 per group). (B) The Kaplan-Meier survival curve of infected mice is shown. Statistically significant differences based on log-rank testing between mock-vaccinated group and vaccinated group are also shown.
3.4. Protective efficacy of the rMP12-GM50 strain via the intramuscular route
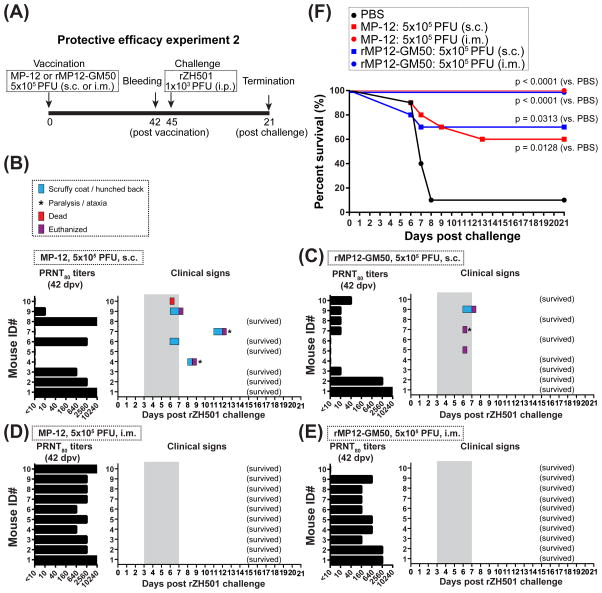
Since the vaccinations with 1×105 PFU of the parental MP-12 or rMP12-GM50 strains were not very efficacious via the s.c. route, a higher dose (5×105 PFU) via the s.c. or intramuscular (i.m.) route was next tested for its protective efficacy (protective efficacy experiment 2: Fig. 4). At 42 days post vaccination, the neutralizing antibodies with PRNT80 1:40 or higher were detected in 50% or 20% of mice vaccinated via s.c. with 5×105 PFU of the parental MP-12 or rMP12-GM50 strains, respectively (Figs. 4B and C). The mean neutralizing antibody titers of responders (PRNT80 titers of 1:10 or higher) were 1:4,375 and 1:1,840 against the parental MP-12 or rMP12-GM50 strains, respectively. In contrast, the vaccination via i.m. route showed an improved immunogenicity of those vaccine strains. The neutralizing antibodies with PRNT80 1:40 or higher were detected in 100% and 90% of mice vaccinated i.m. with the parental MP-12 or rMP12-GM50 strains, respectively, and none of mice in those groups showed detectable clinical signs of disease over a 21-day period after a rZH501 challenge. (Figs. 4D and E). The mean neutralizing antibody titers of those responders via i.m. vaccination were 1:3,712 and 1:853 against the parental MP-12 or rMP12-GM50 strains, respectively. Those vaccinated mice were challenged with pathogenic rZH501 strain at 45 days post vaccination. Mice vaccinated with 5×105 PFU of the parental MP-12 or rMP12-GM50 strains via s.c. route resulted in 60% or 70% survival, respectively, and all dead or euthanized mice did not have neutralizing antibody with PRNT80 1:40 or higher (Fig. 4F). Survival curves of those s.c. groups were marginally significant compared to that of mock-vaccinated group (Log-rank test, p = 0.0128 or p = 0.0313, respectively). In contrast, mice vaccinated with 5×105 PFU of the parental MP-12 or rMP12-GM50 strains via i.m. route showed 100% survival, and those survival curves were significantly different from that of mock-vaccinated group (Log-rank test, p < 0.0001) (Fig. 4F). Overall, these results showed that the i.m. route is more suitable than the s.c. route for universally inducing protective immunity in mice vaccinated with the MP-12 or rMP12-GM50 strains.
Fig. 4. Protective efficacy experiment 1: vaccination with either subcutaneous or intramuscular route.
(A) Schematic representation of vaccination and challenge schedule for the protective efficacy experiment 2. Outbred CD1 mice mock-vaccinated via s.c. or intramuscular (i.m.) route with PBS (n = 5 per route), or vaccinated via s.c. or i.m. with 5×105 PFU of MP-12 (n = 10 per group) or rMP12-GM50 (n = 10 per group). (B – E) Titers of Plaque Reduction Neutralization Test 80 and clinical signs of disease observed in each mouse infected with 5×105 PFU of MP-12 (B and D) or rMP12-GM50 (C and E) are shown. Blue = scruffy coat and/or hunched back; red = dead; purple = euthanized; asterisk = paralysis and/or ataxia; gray shadowing = typical period of disease in parental rZH501-infected mice [35]. (F) The Kaplan-Meier survival curve of infected mice is shown. Statistically significant differences based on log-rank testing between mock-vaccinated group and vaccinated group are also shown.
4. Discussion
The MP-12 vaccine has been conditionally licensed for veterinary use in the U.S. [15], and infectious clones can be genetically manipulated via reverse genetics for further improvement [13, 27]. The MP-12 strain was originally generated via serial viral passages of the parental ZH548 strain in MRC-5 cells with a chemical mutagen, 5-fluorouracil [14]. As a result, 23 mutations were introduced into its L-, M-, and S-segments. Two amino acid substitutions (Gn-Y259H and Gc-R1182G) in the M-segment are independently responsible for the attenuation [35]. Those two mutations in the M-segment and two other amino acid substitutions (V172A and M1244I) in the L-segments display a temperature-sensitive phenotype, which restricts viral replication at 38°C and above [37]. The attenuation strength of each L-, M-, and S-segment was previously determined as M > L > S, based on the virulence of reassortant ZH501 strains that encode one of either the MP-12 L-, M-, or S-segments. Namely, 20%, 40%, or 0% of mice were able to survive the infection (i.p.) following a dose of 1×103 PFU of RST-MP12-L, RST-MP12-M, or RST-MP12-S, respectively [35]. Although the attenuation of MP-12 strain via the S-segment was not evident based on the survival rate, pathogenic RVFV strains encoding MP-12 S-segment showed prolonged survivals of mice [35, 38]. Past attempts aimed to strengthen the attenuation profile of MP-12 strain via reverse genetics. Attenuation through the S-segment could be achieved via the truncation of the NSs gene (rMP12-ΔNSs16/198) [27, 31]. Alternatively, the NSs gene of the MP-12 strain could be replaced with other phlebovirus NSs to modestly attenuate via the S-segment [36, 39]. Attenuation via the M-segment could be partly successful via the truncation of the 78kD/NSm gene (rMP12-ΔNSm21/384) [40–42]; the pathogenic RVFV ZH501 strain encoding the 78kD/NSm deletion (rZH501-ΔNSm21/384) was shown to be 100% lethal in mice, whereas the onset of disease was delayed in both mice and rats [39, 43], indicating that the truncation of the 78kD/NSm gene attenuates the ZH501 strain weakly. Modification of the L-segment has not been evaluated, partly due to a lack of rationale for any approach to altering L protein functions. In this study, mice infected with the RST-GM50-L or RST-GM50-S showed 90% or 30% survival. Since the survival curves of the RST-GM50-L and RST-GM50-S groups were significantly different each other, and also different from that of parental rZH501 group, the results suggest that silent mutations could strengthen the attenuation profile of MP-12 L- and S-segments.
In the current study, the MP-12 genome was modified via 584 artificial silent mutations (4.9% nucleotide differences from the parental MP-12). Silent mutations could alter (i) the codon usage bias, (ii) the codon pair bias, and (iii) the frequency of CpG or UpA dinucleotides, which potentially affect the fitness of RNA viruses [29, 44–48]. To avoid over-attenuation of the MP-12 strain, which decreases the protective efficacy, each silent mutation was manually designed to not deoptimize the codon-pair bias in the context of humans [29]. Clusters of mutations were introduced at 50-nucleotide intervals so that the strain could also be used for other studies, such as the analysis of viral homologous recombination, or reassortants between MP-12 strains. The rMP12-GM50 strain showed (i) a codon adaptation index (a codon usage score) of 0.73, compared to the 0.72 of parental MP-12 in humans [34]; (ii) a codon pair bias score of 0.189, compared to the −0.018 of parental MP-12 in humans [29]; and (iii) a total of 133 CpG and 480 UpA dinucleotide motifs, compared to the 130 CpG and 549 UpA dinucleotide motifs in parental MP-12. The silent mutations introduced in this study were thus expected not to alter viral replication capability in human cells. Analysis of viral replication kinetics of the rMP12-GM50 strain, however, showed significant reduction in Vero cells early in infection. Although not statistically significant, a slight decrease of rMP12-GM50 replication also occurred in MRC-5 cells. Those results indicated that silent mutations had detectable impact on viral replication kinetics.
This study showed that vaccination routes significantly affect protective efficacy outcomes of MP-12 and rMP12-GM50 vaccinations: i.e., MP-12 (100% protective: 5×105 PFU via i.m., 60% protective: 5×105 PFU via s.c.), rMP12-GM50 (100% protective: 5×105 PFU via i.m., 70% protective: 5×105 PFU via s.c.). Previous experiments using the same outbred mouse model consistently detected poor responders via s.c. route vaccinations [31, 36]. It remains unknown how the i.m. vaccination with MP-12 strain could reduce poor responders. Although s.c. route is traditionally used for live-attenuated vaccines, there are evidences of better immune responses via i.m. route vaccination [49, 50]. Further evaluation of i.m. route vaccination will be thus important for MP-12 and next generation RVF vaccines.
The mean PRNT80 titer of responders vaccinated parental MP-12 were higher than that vaccinated with rMP12-GM50: i.e., MP-12 (PRNT80 titer 1:3,712 by 5×105 PFU via i.m., PRNT80 titer 1:4,375 by 5×105 PFU via s.c.), rMP12-GM50 (PRNT80 titer 1:853 by 5×105 PFU via i.m., PRNT80 titer 1:1,840 by 5×105 PFU via s.c.). This indicates that a reduction of viral replication led to a decrease in viral antigen expression.
Our previous study showed a random creation of genetic reassortant strains between rMP-12 and rMP12-GM50 strain in co-infected mosquito C6/36 cells [25]. Since MP-12 strain does not induce high titers of viremia in ruminants, it is considered unlikely that rMP12-GM50 strain can transmit from vaccinated animals to mosquitoes [51, 52]. If rMP12-GM50 strain and wild-type RVFV strains co-circulate in mosquitoes by any reasons, it is assumed that reassortant RVFV strains between two strains can be created. It will be, however, unlikely that reassortant RVFV strains encoding any of L-, M-, or S-segments derived from rMP12-GM50 will be more pathogenic than wild-type RVFV strains due to attenuation via each RNA segment. Silent mutations of rMP12-GM50 will also serve as a genetic marker to distinguish rMP12-GM50 strain from wild-type RVFV strain for the surveillance of vaccine strains after the vaccination in endemic countries. A similar approach will be applicable to an effective vaccination strategy for RVF in endemic countries.
Supplementary Material
Highlights.
The rMP12-GM50 strain shows 100% protective efficacy in mice.
Silent mutations strengthen attenuation profiles of the MP-12 strain.
For the MP-12 strain, intramuscular vaccination is more immunogenic than subcutaneous vaccination.
Acknowledgments
We thank the staff in the Animal Resource Center at UTMB for their support with the mouse experiment.
Funding
This study was made possible by the generous support of NIH grant R01 AI08764301-A1, the United States Agency for International Development (USAID, AID-OAA-A-13-00084), and the funding from the Sealy Center for Vaccine Development at the University of Texas Medical Branch at Galveston. The contents do not necessarily reflect the views of the United States Government. SN was supported by the James W. McLaughlin Postdoctoral Fellowship at UTMB.
Abbreviations
- FBS
fetal bovine serum
- i.m
intramuscular route
- i.p
intraperitoneal route
- MEM
minimum essential medium
- MOI
multiplicity of infection
- ORF
open reading frame
- PFU
plaque forming units
- PRNT80
Plaque Reduction Neutralization Test 80
- RVF
Rift Valley fever
- RVFV
Rift Valley fever phlebovirus
- s.c
subcutaneous route
Footnotes
Competing Interests
The authors declare no conflict of interest. The founding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
Author Contributions
H.J.L. and T.I. conceived and designed the experiments; H.J.L., N.L., S.N., J.K.S., L.Z., D.P., T.L.J., A.N.F., and T.I. performed the experiments; H.J.L. and T.I. analyzed the data; H.J.L. and T.I. wrote the paper. Authorship must be limited to those who have contributed substantially to the work reported.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Swanepoel R, Coetzer JAW. Rift Valley fever. In: Coetzer JAW, Tustin RC, editors. Infectious diseases of livestock with special reference to southern Africa. 2. Cape Town, South Africa: Oxford University Press; 2004. pp. 1037–1070. [Google Scholar]
- 2.Pepin M, Bouloy M, Bird BH, Kemp A, Paweska J. Rift Valley fever virus (Bunyaviridae: Phlebovirus): an update on pathogenesis, molecular epidemiology, vectors, diagnostics and prevention. Vet Res. 2010;41:61. doi: 10.1051/vetres/2010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ikegami T, Makino S. The Pathogenesis of Rift Valley Fever. Viruses. 2011;3:493–519. doi: 10.3390/v3050493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jonsson CB, Cole KS, Roy CJ, Perlin DS, Byrne G. Challenges and Practices in Building and Implementing Biosafety and Biosecurity Programs to Enable Basic and Translational Research with Select Agents. J Bioterror Biodef. 2013;(Suppl 3):12634. doi: 10.4172/2157-2526.S3-015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daubney R, Hudson JR. Enzootic hepatitis or Rift Valley fever: An undescribed virus disease of sheep cattle and man from east Africa. J Path Bact. 1931;34:545–79. [Google Scholar]
- 6.Bird BH, Khristova ML, Rollin PE, Ksiazek TG, Nichol ST. Complete genome analysis of 33 ecologically and biologically diverse Rift Valley fever virus strains reveals widespread virus movement and low genetic diversity due to recent common ancestry. J Virol. 2007;81:2805–16. doi: 10.1128/JVI.02095-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carroll SA, Reynes JM, Khristova ML, Andriamandimby SF, Rollin PE, Nichol ST. Genetic evidence for Rift Valley fever outbreaks in Madagascar resulting from virus introductions from the East African mainland rather than enzootic maintenance. J Virol. 2011;85:6162–7. doi: 10.1128/JVI.00335-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Madani TA, Al-Mazrou YY, Al-Jeffri MH, Mishkhas AA, Al-Rabeah AM, Turkistani AM, et al. Rift Valley fever epidemic in Saudi Arabia: epidemiological, clinical, and laboratory characteristics. Clin Infect Dis. 2003;37:1084–92. doi: 10.1086/378747. [DOI] [PubMed] [Google Scholar]
- 9.Ikegami T, Makino S. Rift valley fever vaccines. Vaccine. 2009;27(Suppl 4):D69–72. doi: 10.1016/j.vaccine.2009.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kortekaas J. One Health approach to Rift Valley fever vaccine development. Antiviral Res. 2014;106:24–32. doi: 10.1016/j.antiviral.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 11.Alhaj M. Safety and Efficacy Profile of Commercial Veterinary Vaccines against Rift Valley Fever: A Review Study. Journal of immunology research. 2016;2016:7346294. doi: 10.1155/2016/7346294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO. The use of veterinary vaccines for prevention and control of Rift Valley fever: memorandum from a WHO/FAO meeting. Bull World Health Organ. 1983;61:261–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Ikegami T. Rift Valley fever vaccines: An overview of the safety and efficacy of the live-attenuated MP-12 vaccine candidate. Expert Rev Vaccines. 2017;16:601–11. doi: 10.1080/14760584.2017.1321482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caplen H, Peters CJ, Bishop DH. Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J Gen Virol. 1985;66(Pt 10):2271–7. doi: 10.1099/0022-1317-66-10-2271. [DOI] [PubMed] [Google Scholar]
- 15.Hills RE. Issuance of a conditional license for Rift Valley fever vaccine, modified live virus. Center for Veterinary Biologics; Ames, IA: 2013. Notice no. 13–12. [Google Scholar]
- 16.Morrill JC, Carpenter L, Taylor D, Ramsburg HH, Quance J, Peters CJ. Further evaluation of a mutagen-attenuated Rift Valley fever vaccine in sheep. Vaccine. 1991;9:35–41. doi: 10.1016/0264-410x(91)90314-v. [DOI] [PubMed] [Google Scholar]
- 17.Morrill JC, Jennings GB, Caplen H, Turell MJ, Johnson AJ, Peters CJ. Pathogenicity and immunogenicity of a mutagen-attenuated Rift Valley fever virus immunogen in pregnant ewes. Am J Vet Res. 1987;48:1042–7. [PubMed] [Google Scholar]
- 18.Morrill JC, Mebus CA, Peters CJ. Safety of a mutagen-attenuated Rift Valley fever virus vaccine in fetal and neonatal bovids. Am J Vet Res. 1997;58:1110–4. [PubMed] [Google Scholar]
- 19.Morrill JC, Mebus CA, Peters CJ. Safety and efficacy of a mutagen-attenuated Rift Valley fever virus vaccine in cattle. Am J Vet Res. 1997;58:1104–9. [PubMed] [Google Scholar]
- 20.Botros B, Omar A, Elian K, Mohamed G, Soliman A, Salib A, et al. Adverse response of non-indigenous cattle of European breeds to live attenuated Smithburn Rift Valley fever vaccine. J Med Virol. 2006;78:787–91. doi: 10.1002/jmv.20624. [DOI] [PubMed] [Google Scholar]
- 21.Indran SV, Ikegami T. Novel approaches to develop Rift Valley fever vaccines. Front Cell Infect Microbiol. 2012;2:131. doi: 10.3389/fcimb.2012.00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Terasaki K, Tercero BR, Makino S. Single-cycle replicable Rift Valley fever virus mutants as safe vaccine candidates. Virus Res. 2016;216:55–65. doi: 10.1016/j.virusres.2015.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Warimwe GM, Gesharisha J, Carr BV, Otieno S, Otingah K, Wright D, et al. Chimpanzee Adenovirus Vaccine Provides Multispecies Protection against Rift Valley Fever. Scientific reports. 2016;6:20617. doi: 10.1038/srep20617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Faburay B, Wilson WC, Gaudreault NN, Davis AS, Shivanna V, Bawa B, et al. A Recombinant Rift Valley Fever Virus Glycoprotein Subunit Vaccine Confers Full Protection against Rift Valley Fever Challenge in Sheep. Scientific reports. 2016;6:27719. doi: 10.1038/srep27719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ly HJ, Lokugamage N, Nishiyama S, Ikegami T. Risk analysis of inter-species reassortment through a Rift Valley fever phlebovirus MP-12 vaccine strain. PLoS ONE. 2017;12:e0185194. doi: 10.1371/journal.pone.0185194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ito N, Takayama-Ito M, Yamada K, Hosokawa J, Sugiyama M, Minamoto N. Improved recovery of rabies virus from cloned cDNA using a vaccinia virus-free reverse genetics system. Microbiol Immunol. 2003;47:613–7. doi: 10.1111/j.1348-0421.2003.tb03424.x. [DOI] [PubMed] [Google Scholar]
- 27.Ikegami T, Won S, Peters CJ, Makino S. Rescue of infectious rift valley fever virus entirely from cDNA, analysis of virus lacking the NSs gene, and expression of a foreign gene. J Virol. 2006;80:2933–40. doi: 10.1128/JVI.80.6.2933-2940.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kalveram B, Lihoradova O, Indran SV, Ikegami T. Using reverse genetics to manipulate the NSs gene of the Rift Valley fever virus MP-12 strain to improve vaccine safety and efficacy. J Vis Exp. 2011:e3400. doi: 10.3791/3400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Coleman JR, Papamichail D, Skiena S, Futcher B, Wimmer E, Mueller S. Virus attenuation by genome-scale changes in codon pair bias. Science. 2008;320:1784–7. doi: 10.1126/science.1155761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.GenScript Rare Codon Analysis Tool [database on the Internet] Available from: https://www.genscript.com/tools/rare-codon-analysis.
- 31.Lihoradova O, Kalveram B, Indran SV, Lokugamage N, Juelich TL, Hill TE, et al. The dominant-negative inhibition of double-stranded RNA-dependent protein kinase PKR increases the efficacy of Rift Valley fever virus MP-12 vaccine. J Virol. 2012;86:7650–61. doi: 10.1128/JVI.00778-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gutman GA, Hatfield GW. Nonrandom utilization of codon pairs in Escherichia coli. Proc Natl Acad Sci U S A. 1989;86:3699–703. doi: 10.1073/pnas.86.10.3699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moura G, Pinheiro M, Silva R, Miranda I, Afreixo V, Dias G, et al. Comparative context analysis of codon pairs on an ORFeome scale. Genome Biol. 2005;6:R28. doi: 10.1186/gb-2005-6-3-r28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Puigbo P, Bravo IG, Garcia-Vallve S. CAIcal: a combined set of tools to assess codon usage adaptation. Biol Direct. 2008;3:38. doi: 10.1186/1745-6150-3-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ikegami T, Hill TE, Smith JK, Zhang L, Juelich TL, Gong B, et al. Rift Valley Fever Virus MP-12 Vaccine Is Fully Attenuated by a Combination of Partial Attenuations in the S, M, and L Segments. J Virol. 2015;89:7262–76. doi: 10.1128/JVI.00135-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lihoradova OA, Indran SV, Kalveram B, Lokugamage N, Head JA, Gong B, et al. Characterization of Rift Valley Fever Virus MP-12 Strain Encoding NSs of Punta Toro Virus or Sandfly Fever Sicilian Virus. PLoS Negl Trop Dis. 2013;7:e2181. doi: 10.1371/journal.pntd.0002181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nishiyama S, Lokugamage N, Ikegami T. The L-, M- and S-segments of Rift Valley fever virus MP-12 vaccine independently contribute to a temperature-sensitive phenotype. J Virol. 2016;90:3735–37644. doi: 10.1128/JVI.02241-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Billecocq A, Gauliard N, Le May N, Elliott RM, Flick R, Bouloy M. RNA polymerase I-mediated expression of viral RNA for the rescue of infectious virulent and avirulent Rift Valley fever viruses. Virology. 2008;378:377–84. doi: 10.1016/j.virol.2008.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nishiyama S, Slack OA, Lokugamage N, Hill TE, Juelich TL, Zhang L, et al. Attenuation of pathogenic Rift Valley fever virus strain through the chimeric S-segment encoding sandfly fever phlebovirus NSs or a dominant-negative PKR. Virulence. 2016:1–11. doi: 10.1080/21505594.2016.1195528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Won S, Ikegami T, Peters CJ, Makino S. NSm protein of Rift Valley fever virus suppresses virus-induced apoptosis. J Virol. 2007;81:13335–45. doi: 10.1128/JVI.01238-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morrill JC, Laughlin RC, Lokugamage N, Pugh R, Sbrana E, Weise WJ, et al. Safety and immunogenicity of recombinant Rift Valley fever MP-12 vaccine candidates in sheep. Vaccine. 2013;31:559–65. doi: 10.1016/j.vaccine.2012.10.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Morrill JC, Laughlin RC, Lokugamage N, Wu J, Pugh R, Kanani P, et al. Immunogenicity of a recombinant Rift Valley fever MP-12-NSm deletion vaccine candidate in calves. Vaccine. 2013;31:4988–94. doi: 10.1016/j.vaccine.2013.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bird BH, Albarino CG, Nichol ST. Rift Valley fever virus lacking NSm proteins retains high virulence in vivo and may provide a model of human delayed onset neurologic disease. Virology. 2007;362:10–5. doi: 10.1016/j.virol.2007.01.046. [DOI] [PubMed] [Google Scholar]
- 44.Burns CC, Campagnoli R, Shaw J, Vincent A, Jorba J, Kew O. Genetic inactivation of poliovirus infectivity by increasing the frequencies of CpG and UpA dinucleotides within and across synonymous capsid region codons. J Virol. 2009;83:9957–69. doi: 10.1128/JVI.00508-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Atkinson NJ, Witteveldt J, Evans DJ, Simmonds P. The influence of CpG and UpA dinucleotide frequencies on RNA virus replication and characterization of the innate cellular pathways underlying virus attenuation and enhanced replication. Nucleic Acids Res. 2014;42:4527–45. doi: 10.1093/nar/gku075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tulloch F, Atkinson NJ, Evans DJ, Ryan MD, Simmonds P. RNA virus attenuation by codon pair deoptimisation is an artefact of increases in CpG/UpA dinucleotide frequencies. eLife. 2014;3:e04531. doi: 10.7554/eLife.04531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Baker SF, Nogales A, Martinez-Sobrido L. Downregulating viral gene expression: codon usage bias manipulation for the generation of novel influenza A virus vaccines. Future Virol. 2015;10:715–30. doi: 10.2217/fvl.15.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang B, Yang C, Tekes G, Mueller S, Paul A, Whelan SP, et al. Recoding of the vesicular stomatitis virus L gene by computer-aided design provides a live, attenuated vaccine candidate. MBio. 2015:6. doi: 10.1128/mBio.00237-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cook IF. Evidence based route of administration of vaccines. Hum Vaccin. 2008;4:67–73. doi: 10.4161/hv.4.1.4747. [DOI] [PubMed] [Google Scholar]
- 50.Herzog C. Influence of parenteral administration routes and additional factors on vaccine safety and immunogenicity: a review of recent literature. Expert Rev Vaccines. 2014;13:399–415. doi: 10.1586/14760584.2014.883285. [DOI] [PubMed] [Google Scholar]
- 51.Turell MJ, Rossi CA. Potential for mosquito transmission of attenuated strains of Rift Valley fever virus. Am J Trop Med Hyg. 1991;44:278–82. doi: 10.4269/ajtmh.1991.44.278. [DOI] [PubMed] [Google Scholar]
- 52.Miller MM, Bennett KE, Drolet BS, Lindsay R, Mecham JO, Reeves WK, et al. Evaluation of the efficacy, potential for vector transmission, and duration of immunity of MP-12, an attenuated Rift Valley fever virus vaccine candidate, in sheep. Clin Vaccine Immunol. 2015;22:930–7. doi: 10.1128/CVI.00114-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.