Abstract
Introduction
Higher sedentary time (ST) and lower moderate to vigorous intensity physical activity (MVPA) have each been associated with greater adiposity, but most studies are cross-sectional and measure ST and MVPA by self-report. This study evaluated associations between objective ST and MVPA with current and 5-year changes in BMI and waist circumference.
Methods
The Coronary Artery and Risk Development in Young Adults longitudinal cohort study recruited black or white young adults from four U.S. cities. This analysis (conducted in 2016) used data from 2005 to 2006 as baseline and 2010 to 2011 as 5-year follow-up. Accelerometers measured baseline ST (total and prolonged in bouts of ≥10 minutes) and MVPA (bouts of ≥10 minutes). BMI and waist circumference were assessed at baseline and repeated 5 years later. Regression models included sedentary time and MVPA simultaneously with adjustment for demographics and lifestyle factors.
Results
Participants (n=1,826) were 57% female, 40% black, aged 38–50 years, and had BMI of 28.7 (SD=6.3) kg/m2. At baseline, total and prolonged ST were directly associated with BMI and waist circumference, whereas MVPA was inversely related (all p<0.05). Longitudinally, only prolonged ST (per hour/day) was associated with greater increases in BMI (0.077 kg/m2, p=0.033) and waist circumference (0.198 cm, p=0.028). Associations between ST and adiposity were more apparent in less active participants. Risk of ≥5% increase in BMI across assessments increased by 8%–10% (p<0.05) per hour/day of ST.
Conclusions
Time spent sedentary was associated with increases in adiposity over time. Reducing sedentary time may be a novel strategy for weight control.
INTRODUCTION
Obesity affects one third of the U.S. adult population,1 increases the risk of diabetes, cardiovascular disease, and some cancers,2 and decreases life expectancy.3 Central adiposity, often measured by waist circumference (WC), may be more strongly associated with premature mortality as compared with overall adiposity (i.e., BMI).4 Though treatment for obesity can be successful in the short-term, effective strategies for long-term weight loss maintenance remain elusive.5 Thus, identifying strategies to prevent weight gain and obesity are a major public health priority.
Consistent engagement in moderate to vigorous intensity physical activity (MVPA) has been associated with attenuated weight and WC gains over time.6,7 Sedentary behavior has been established as a behavior distinct from inactivity or a lack of MVPA.8 Yet, whether sedentary behavior is a risk factor for weight or WC gains is less clear.
If sedentary behavior replaces tasks with slightly higher metabolic costs (i.e., light intensity activities)9 throughout the day, this could lead to less daily energy expenditure, a state of positive energy balance, and weight gain. However, some studies suggest a reverse direction of association where obesity leads to increased sedentary behavior over time.10,11 Though greater sedentary behavior has been associated with higher BMI and WC,12–17 most studies are cross-sectional and therefore cannot establish a temporal relationship. Another limitation is that most studies measure sedentary time (ST) by self-report, which can be poorly correlated to objectively measured ST9,17,18 and cannot evaluate patterns of sedentary behavior (such as prolonged bouts) which may be more closely related to adverse outcomes.16,19 Recent research also suggests that the risks of sedentary behavior may be attenuated among individuals who are more active,20,21 though whether relationships between sedentary behavior and adiposity differ in active versus inactive individuals remains unclear. Thus, longitudinal studies using objectively measured ST (from which prolonged ST can be extracted) and evaluating effects within higher and lower MVPA strata are needed to evaluate whether higher amounts of sedentary behavior are related to greater adiposity over time.
This study investigated whether accelerometer-measured ST and MVPA are associated with cross-sectional and 5-year changes in BMI and WC in a large, biracial cohort of middle-aged adults. Further, associations of ST with adiposity outcomes within strata of higher and lower MVPA, race and gender interactions, and associations with clinically meaningful 5-year adiposity gains are evaluated.
METHODS
Study Population
The Coronary Artery Risk Development in Young Adults (CARDIA) cohort study enrolled 5,115 black and white young men and women in four U.S. cities in 1985–1986 to longitudinally study determinants of cardiovascular disease.22 The current study uses data collected in 2005–2006 as baseline and 2010–2011 as 5-year follow-up. Each of these follow-up examinations included 72% of the surviving cohort. Of n=2,047 with valid accelerometry data, participants with missing anthropometric data (n=172), history of bariatric surgery (n=38), or pregnancy/breastfeeding at exams (n=11) were excluded, resulting in n=1,826. IRBs at each field center and the coordinating center approved the study annually.
Measures
Activity was measured by an ActiGraph uniaxial accelerometer (model 7164) at baseline only. Participants were asked to wear the accelerometer during all waking hours (except water activities) for 7 days. Movement was captured in 1-minute epochs. Wear time was calculated as 24 hours minus nonwear time, defined as time intervals with 0 counts per minute (cpm) for ≥60 consecutive minutes, but allowing ≤2 minutes at <100 cpm.23 Accelerometry data were considered valid with ≥4 days of monitoring with ≥10 hours/day and <20,000 average cpm. Importantly, ST was measured as the total duration of time spent in limited movement (0–99 cpm); posture and the definition of ST that includes posture were not measured.8 Freedson cutpoints classified total duration of MVPA (≥1,952 cpm).24
Daily ST was calculated as hours accumulated in 1-minute (total) and ≥10-minute (prolonged) bouts. The threshold for prolonged ST reflects research reporting that the direct relationship between ST and adiposity begins at a minimum bout length of 10 minutes.16 Weekly MVPA was calculated by averaging minutes/day of MVPA accumulated in bouts of ≥10 minutes, with allowance for 2 minutes with <1,952 cpm, over valid days and multiplying by 7 days/week.24 Weekly vigorous physical activity was similarly calculated with the cutpoint ≥5,725 cpm. Based on guidelines,25 participants were classified as sufficiently active (“sufficient”) if they achieved ≥150 minutes/week of bouted MVPA or ≥75 minutes/week of bouted vigorous physical activity. Otherwise, they were classified as “insufficient.”
Height and weight were measured in light clothing without shoes. WC was averaged over duplicate measurements by trained research personnel at the narrowest point of the torso. Clinically meaningful BMI or WC gains were defined as 5-year increases of ≥5%.26 Demographic characteristics, smoking, and alcohol were measured at baseline by standardized questionnaires. Energy intake was estimated from the CARDIA diet history at baseline.27
Statistical Analysis
Baseline characteristics were related to overall ST in linear regression models and compared across MVPA categories. Spearman’s correlations assessed relationships between measures of ST and MVPA. Linear regression models estimated cross-sectional associations with BMI and WC. Because 5-year changes in adiposity were of interest, longitudinal models used 5-year change in adiposity as the dependent variable with adjustment for baseline value. Model fit was assessed by visual plots evaluating linear relationships and examining residuals. Logistic regression estimated the odds of clinically meaningful increases (≥5%) in BMI or WC.28 All models included simultaneous adjustment for ST (total or prolonged) and MVPA, gender, race, center, alcohol, education, smoking, dietary energy intake, height (WC only), and accelerometer wear time. Analyses were repeated after stratification by MVPA category, and, reflecting the design of CARDIA, by gender and race. Data analyses were conducted using Stata, version 14 in 2016.
RESULTS
Age, race, gender, education, alcohol, and smoking were all significantly associated with total ST. Participants classified as sufficiently active were more likely to be white and had higher education and alcohol intake (Table 1). Mean total ST was 8.2 (SD=1.7) hours/day and prolonged ST was 4.5 (SD=1.7) hours/day. Median (25th, 75th percentile) MVPA was 43 (0, 130) minutes/week. MVPA was not related to total (rspearman = −0.03, p=0.160) or prolonged ST (rspearman =0.01, p=0.60). Total and prolonged ST were highly correlated (rspearman =0.92, p<0.001).
Table 1.
Baseline Participant Characteristics Overall and by Physical Activity Group in the CARDIA Study
| Characteristic | Overall (n=1,826) | R2a (p-value) | Sufficient MVPAb (n=417) | Insufficient MVPAb (n=1,409) | p-valuec |
|---|---|---|---|---|---|
| Age, years | 45.4 (3.5) | 0.5% (0.002) | 45.5 (3.4) | 45.3 (3.6) | 0.242 |
| Race | 0.9% (<0.001) | <0.001 | |||
| White | 1,102 (60%) | 309 (74%) | 793 (56%) | ||
| Black | 724 (40%) | 108 (26%) | 616 (44%) | ||
| Gender | 0.6% (0.001) | 0.330 | |||
| Male | 781 (43%) | 187 (45%) | 594 (42%) | ||
| Female | 1,045 (57%) | 230 (55%) | 815 (57%) | ||
| Education | 4.2% (<0.001) | <0.001 | |||
| <12 years | 54 (3%) | 10 (2%) | 44 (3%) | ||
| High school | 794 (43%) | 133 (32%) | 661 (47%) | ||
| College | 515 (28%) | 120 (29%) | 395 (28%) | ||
| Masters, PhD, etc. | 463 (25%) | 154 (37%) | 309 (22%) | ||
| Alcohol, mL/d | 2.4 [0, 13.6] | 0.2% (0.029) | 7.2 [0, 19.1] | 2.4 [0, 13.6] | <0.001 |
| Smokingd | 1.6% (<0.001) | 0.108 | |||
| Never | 1,148 (63%) | 274 (66%) | 874 (62%) | ||
| Former | 383 (21%) | 88 (21%) | 295 (21%) | ||
| Current | 281 (15%) | 50 (12%) | 231 (16%) | ||
| Energy intake, kcals/dd | 2,146 [1,638, 2,782] | 0.2% (0.111) | 2,144 [1,663, | 2,147 [1,663, 2,776] | 0.936 |
Notes: Data presented as mean ± SD, median [25th percentile, 75th percentile] or n (%). Boldface indicates statistical significance (p<0.05).
From unadjusted linear regression models predicting total sedentary time.
Sufficient MVPA defined as ≥150 minutes/week of MVPA or ≥75 minutes/week of VPA.
p-value compares values in the sufficient and insufficiently active groups.
Missing data for smoking (0.8%) and dietary intake (10%).
MVPA, moderate-to-vigorous intensity physical activity
At baseline, mean BMI was 28.6 (SD=6.3) kg/m2 and WC was 90.4 (SD=14.5) cm. Cross-sectionally (Table 2), both total and prolonged ST were associated with a higher BMI. Similar patterns were observed for WC. Higher MVPA was related to lower adiposity.
Table 2.
Cross-sectional and Longitudinal Associations of Prolonged and Total Sedentary Time, and MVPA With Adiposity
| Variable | Sedentary time (per hour/day) | MVPA (per 30 minutes/week) | ||
|---|---|---|---|---|
| β | p-value | β | p-value | |
| Cross-sectional | ||||
| BMI, kg/m2 | ||||
| Total | 0.20 | 0.047 | −0.15 | <0.001 |
| Prolonged | 0.23 | 0.013 | −0.18 | <0.001 |
| WC, cm | ||||
| Total | 0.67 | 0.003 | −0.46 | <0.001 |
| Prolonged | 0.73 | <0.001 | −0.47 | <0.001 |
| 5-year change | ||||
| BMI, kg/m2 | ||||
| Total | 0.065 | 0.108 | 0.004 | 0.750 |
| Prolonged | 0.077 | 0.033 | 0.003 | 0.811 |
| WC, cm | ||||
| Total | 0.151 | 0.130 | 0.006 | 0.851 |
| Prolonged | 0.198 | 0.028 | 0.004 | 0.898 |
Notes: Boldface indicates statistical significance (p<0.05). All β coefficients adjusted for sedentary time (separate models include either total or prolonged), MVPA, age, race, gender, center, education, alcohol, smoking, energy intake, height (waist only), wear time, and baseline value (5-year change models only).
MVPA, moderate-to-vigorous intensity physical activity; WC, waist circumference.
Over the 5-year follow-up, mean BMI increased by 1.8% (0.53 [SD=2.37] kg/m2) and WC by 2.6% (2.38 [SD=5.85] cm). Higher total ST at baseline was not associated with 5-year BMI gain. However, each hour of prolonged ST at baseline was associated with an additional BMI gain of 0.077 kg/m2 (p=0.033). Associations between 5-year changes in WC and baseline total ST were not significant, but each additional hour of baseline prolonged ST was associated with an additional 0.198 cm (p=0.028) gain in WC. Baseline MVPA was not significantly related to 5-year changes in adiposity.
Participants with sufficient (n=417, 23%) versus insufficient (n=1,409, 77%) MVPA had lower mean total ST (8.01 [SD=1.7] vs 8.23 [SD=1.7] hours per day, p=0.018) but not prolonged ST (4.41 [SD=1.65] vs 4.49 [SD=1.72] hours per day, p=0.414). Participants with sufficient and insufficient MVPA had mean baseline BMI of 26.5 (SD=4.9) kg/m2 and 29.3 (SD=4.9) kg/m2 (p<0.001), respectively and baseline WC of 85.7 (SD=13.1) cm and 91.8 (SD=14.6) cm (p<0.001), respectively. Cross-sectional associations between ST and adiposity were more pronounced and only retained statistical significance among participants with insufficient activity (Table 3). Participants with sufficient versus insufficient baseline MVPA had similar mean 5-year changes in BMI (0.34 [SD=1.96] kg/m2 vs 0.58 [SD=2.47] kg/m2, p=0.074) and WC (2.10 [SD=5.00] cm vs 2.46 [SD=6.08] cm, p=0.278). In longitudinal models evaluating associations between baseline ST and 5-year changes in adiposity, only prolonged ST in participants with insufficient MVPA was related to change in BMI (0.087 kg/m2 per hour/day, p=0.042).
Table 3.
Associations of Prolonged and Total Sedentary Time With Adiposity by Sufficient and Insufficient MVPA Category
| Variable | Sufficient MVPA (n=417) | Insufficient MVPA (n=1,409) | ||
|---|---|---|---|---|
| β | p-value | β | p-value | |
| Cross-sectional | ||||
| BMI, kg/m2 | ||||
| Total | −0.05 | 0.777 | 0.25 | 0.042 |
| Prolonged | 0.03 | 0.822 | 0.25 | 0.019 |
| WC, cm | ||||
| Total | −0.22 | 0.577 | 0.86 | 0.001 |
| Prolonged | 0.12 | 0.736 | 0.84 | <0.001 |
| 5-year change | ||||
| BMI, kg/m2 | ||||
| Total | 0.032 | 0.666 | 0.074 | 0.116 |
| Prolonged | 0.039 | 0.553 | 0.087 | 0.042 |
| WC, cm | ||||
| Total | 0.338 | 0.081 | 0.104 | 0.372 |
| Prolonged | 0.260 | 0.134 | 0.180 | 0.086 |
Notes: Boldface indicates statistical significance (p<0.05). Total and prolonged sedentary time were included in separate models. All β coefficients adjusted for MVPA, age, race, gender, center, education, alcohol, smoking, energy intake, height (waist only), wear time, and baseline value (5-year change models only).
Sufficient activity defined as ≥150 minutes/week of MVPA or ≥75 minutes/week of VPA
MVPA, moderate-to-vigorous intensity physical activity; WC, waist circumference.
Results stratified by race and gender are presented in Appendix Tables 1 and 2. In general, ST was more often associated with adiposity in men than women. ST was cross-sectionally associated with adiposity only in whites, whereas longitudinal associations were only observed in blacks. Associations between MVPA and adiposity were similar by race and gender.
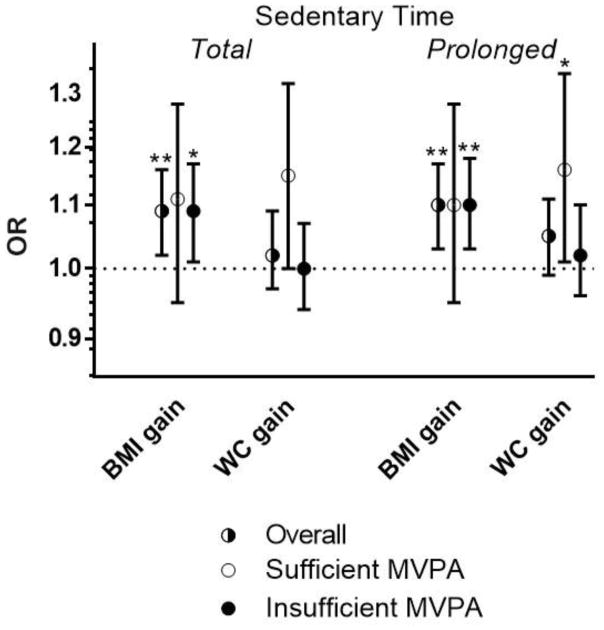
Thirty percent (n=548) and 34% (n=662) of participants had clinically meaningful (≥5%) weight and WC gains over the 5-year follow-up, respectively. These proportions were similar in participants with sufficient and insufficient baseline MVPA (weight gain: 31% vs 27%, p=0.175; WC gain: 35% vs 31%, p=0.160). The adjusted odds of clinically meaningful BMI (weight) gain over 5 years were elevated with each additional hour/day of baseline total ST (OR=1.09, 95% CI=1.02, 1.16) and prolonged ST (1.10, 95% CI=1.03, 1.17). Though the OR estimates were almost identical in participants with sufficient or insufficient MVPA, wide CIs among the sufficiently active resulted in significantly increased odds occurring only in the insufficient MVPA group (Figure 1 and Appendix Table 3). Total ST was not associated with increased odds of WC gain. Interestingly, prolonged ST was associated with higher odds of clinically meaningful WC gain among participants with sufficient (OR=1.16, 95% CI=1.01, 1.34), but not insufficient MVPA (OR=1.02, 95% CI=0.96, 1.10). Baseline MVPA was not associated with clinically meaningful adiposity gains.
Figure 1.
Adjusted odds of clinically meaningful (≥5%) 5-year gains in BMI and waist circumference (WC) with each 1-hour increase in total or prolonged sedentary time.
Notes: Data are presented overall (split circle, n=1,826) and stratified into participants with sufficient (white circle, n=417) and insufficient (solid black circle, n=1,409) moderate-to-vigorous physical activity. ORs are adjusted for moderate-to-vigorous physical activity, age, gender, race, center, education, alcohol, smoking, energy intake, height (waist only), and baseline value. *p<0.05; **p<0.01
MVPA, moderate-to-vigorous intensity physical activity
DISCUSSION
The primary findings of this study were that having greater objectively measured ST at baseline, particularly greater prolonged ST accumulated in bouts of >10 minutes, was related to higher current BMI and WC, but also greater 5-year increases in these adiposity measures. MVPA at baseline was associated with lower adiposity in cross-sectional analyses but not 5-year changes. Associations with BMI, WC, and 5-year BMI change were present only in participants that did not meet recommendations for MVPA (insufficiently active). The risk of clinically meaningful 5-year changes in BMI, reflecting a failure to maintain weight, was elevated with increased total and prolonged ST and risk estimates were similar after stratification into sufficient and insufficient MVPA groups. Risk of clinically meaningful gains in WC was not related to ST, except for an increased risk observed with prolonged ST among sufficiently active participants.
Because American adults spend an average 97% of waking hours engaging in sedentary or light intensity activities,29 and sedentary behavior has slightly lower energy costs than light intensity activities,30 it is plausible that excessive sedentary behavior might disrupt energy balance and contribute to obesity and weight gain. Some,13–16,19 but not all,16,17,31 studies with objective measurement of ST have found direct associations with overall or central adiposity. This current study’s cross-sectional findings are similar to results from the National Health and Nutrition Examination Survey (NHANES; 2003–2006) where objectively measured ST across (as ST quartiles,14 continuous ST, or prolonged ST bouts16) was related to greater central adiposity. The NHANES analysis also found that prolonged ST was associated with BMI (β=0.002, p=0.024) whereas total ST was not (BMI: β=0.001, p=0.521).16 Further, shorter-bout ST (1–9 minutes) was inversely related to BMI. The current study found that both prolonged and total ST were cross-sectionally related to BMI; the different results may be due in part to age-related differences between study populations.
To the authors’ knowledge, the current study is the largest to date examining longitudinal associations between objectively measured ST and adiposity over time, and the only to evaluate prolonged sedentary behavior. In the few studies that measured sitting time by self-report, most have found that higher sitting time did not predict changes in weight10,32–34 and some have found a reverse direction of effect whereby greater adiposity at baseline was associated with increased ST at follow-up.10,34 The authors are aware of only two studies with longitudinal assessment of both objectively measured total ST and adiposity. Among 393 healthy adults in the Medical Research Council Ely Study, ST (by heart rate monitor) was not associated with weight gain; however, baseline BMI was associated with increased ST over the 5.6-year follow-up.11 In the ProActive Study, 6-year changes in accelerometer-measured ST and WC were not associated among 171 adults with metabolic risk factors.35 The current study similarly found that total ST was not associated with 5-year changes in BMI and WC, but uniquely identified that prolonged ST was associated with 5-year increases in BMI and WC. These findings underscore the need to extract prolonged ST from objective monitors when evaluating the health risks associated with sedentary behavior. These findings also inform interventions that seek to reduce sedentary behavior.
The results of the current study stratified by MVPA level are also comparable to other research. In NHANES, more ST was associated with an increased risk of mortality in low active but not high active individuals.20 A recent meta-analysis found that associations between ST and cardiometabolic outcomes or mortality were of greater magnitude in the lowest versus highest MVPA groups.21 The current study found that cross-sectional relationships between sedentary behavior and adiposity were indeed only apparent among insufficiently active participants. For 5-year changes, only associations with prolonged sedentary behavior among participants with insufficient activity remained after stratification. Thus, sedentary behavior may be a risk factor for weight gain, particularly among less active individuals.
Though most associations between ST and adiposity were in the same direction across race or gender strata, statistically significant associations were more often observed in men, in whites cross-sectionally, and in blacks longitudinally. The reasons for these race and gender differences are not clear and an area for further research.
This analysis also considered a dichotomous outcome of whether individuals had clinically meaningful gains in adiposity over the 5-year follow-up defined as an increase of ≥5%.28 This outcome gives consideration to any clinically meaningful adiposity gain as a negative health outcome, rather than allowing large adiposity gains to potentially have more influence on estimated associations in a continuous variable analysis. Approximately a third of the participants had such gains as they progressed through middle age. Each additional hour/day of total or prolonged ST was associated with an 8%–10% increased risk of clinically meaningful weight gain and this estimate was similar among participants with sufficient and insufficient MVPA (though the risk estimate was not significant in the sufficiently active participants, likely a result of the small sample size). Thus, lowering ST may be a strategy for maintaining weight. Only prolonged ST in sufficiently active participants was associated with a 16% increase in the odds of clinically meaningful WC gains. Though the reasons for this stronger effect in the presence of sufficient MVPA are not clear, one explanation could be the lower WC at baseline in the sufficiently active group. Overall, lower ST appears to be helpful for maintaining weight and WC, regardless of activity level.
Though higher baseline MVPA was related to lower adiposity cross-sectionally, the lack of longitudinal associations differs from existing studies showing that MVPA protects against weight gain.7,36,37 Over the first 20-years of the CARDIA Study (prior to these analyses), participants with consistently high versus low self-reported MVPA gained less weight and WC.7 In another study of 421 young adults over 1 year, those in the lowest objectively measured MVPA quintile at baseline gained the most fat mass and were 3.8 times more likely to increase their weight by ≥3% as compared with those in the middle MVPA quintile.37 Baseline MVPA may not have associated with 5-year changes in adiposity in the current study for two reasons. First, though controversial, the National Academy of Medicine38 (formerly known as the Institute of Medicine) recommends that as much as 420 minutes/week of MVPA may be necessary to maintain a healthy weight. Only 2.1% (n=39) of participants achieved >420 minutes/week of MVPA. It is possible that the scarcity of participants achieving these levels of MVPA may have limited the ability to detect an association. Another possibility is that the single assessment of MVPA, with no additional measures to account for changes in behavior over follow-up, may have resulted in misclassification and attenuation of relationships between MVPA and changes in adiposity.
The public health and clinical significance of these findings are that time spent in sedentary behavior, particularly when accumulated in prolonged bouts, might be a new behavioral target to decrease weight gain and obesity during midlife. Though significant associations were more consistently observed among inactive individuals, there was also a suggestion that active individuals could benefit from lower ST. Though the U.S. does not currently have sedentary behavior guidelines,25 generally reducing sedentary behavior is part of the Australian physical activity guidelines. An expert statement commissioned by Public Health England and the Active Working Community Interest Company recently concluded that desk-based employees should accumulate 2–4 hours of standing or other light activity in each 8-hour workday. 39 The current study informs potential sedentary behavior guidelines, though evidence of a health benefit from natural experiments (e.g., demonstrated health improvements with large-scale sit-stand desk implementation) and randomized trials that experimentally decrease sedentary time long-term will provide further support for such recommendations.
Limitations
This study is strengthened by the large sample size, objective measurements, longitudinal follow-up of obesity outcomes, and inclusion of other relevant confounders (e.g., energy intake, smoking) in CARDIA. One limitation was the inability to study some temporal relationships because of the single assessment of objective activity at baseline. Another limitation is that the objective monitor used measures time spent in limited movement (0–99 cpm), which some may refer to as “stationary time,”40 rather than time spent in low intensity and a seated or reclining posture, the more commonly accepted definition of sedentary behavior.9 Though free-living ST measured by accelerometer have been shown to be highly correlated (e.g., R2=70%28) with ST measured by devices also capable for measuring posture, interpretation of the results should acknowledge ST as “limited movement” rather than “sitting at low intensity” in this study.
CONCLUSIONS
Greater time spent in objectively measured ST and lower levels of MVPA were associated with higher levels of adiposity, but only ST was associated with greater increases in BMI and WC and elevated the risk of clinically meaningful adiposity gains over 5 years. These results suggest that lowering ST, or time spent with limited movement, may be protective against obesity and a novel strategy for weight control.
Supplementary Material
Acknowledgments
The authors would like to thank the participants, staff, and investigators of the Coronary Artery Risk Development in Young Adults Study (CARDIA) study. CARDIA is supported by contracts HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, and HHSN268200900041C from the National Heart, Lung, and Blood Institute (NHLBI), the Intramural Research Program of the National Institute on Aging, and an intra-agency agreement between National Institute on Aging and NHLBI (AG0005). The CARDIA Fitness Study was supported by grant R01-HL-078972 from the NHLBI and is registered on ClinicalTrials.gov (NCT00005130). The CARDIA Young Adults Longitudinal Trends in Antioxidants was supported by a grant 1RO1-HL53560–01A1 from the NHLBI. Dr. Barone Gibbs was supported by the Tomayko Foundation. Dr. Siddique was supported by grant K07 CA154862 from the National Cancer Institute and R01 HL131606 from NHLBI. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the NHLBI, NIH, or U.S. DHHS.
Preliminary analyses of these data were presented at the American Heart Association Epi|Lifestyle conference in March 2016.
Dr. Barone Gibbs reports grant funding to her institution from Humanscale. Dr. Jakicic reports grant funding to his institution from Weight Watchers, Jawbone, and Humanscale, and personal payment for serving on the Scientific Advisory Board for Weight Watchers. No other financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. https://doi.org/10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kopelman P. Health risks associated with overweight and obesity. Obes Rev. 2007;8(s1):13–17. doi: 10.1111/j.1467-789X.2007.00311.x. https://doi.org/10.1111/j.1467-789X.2007.00311.x. [DOI] [PubMed] [Google Scholar]
- 3.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861–1867. doi: 10.1001/jama.293.15.1861. https://doi.org/10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 4.Sahakyan KR, Somers VK, Rodriguez-Escudero JP, et al. Normal-Weight Central Obesity: Implications for Total and Cardiovascular Mortality. Ann Intern Med. 2015;163(11):827–835. doi: 10.7326/M14-2525. https://doi.org/10.7326/M14-2525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dombrowski SU, Knittle K, Avenell A, Araujo-Soares V, Sniehotta FF. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ. 2014;348:g2646. doi: 10.1136/bmj.g2646. https://doi.org/10.1136/bmj.g2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donnelly JE, Blair SN, Jakicic JM, et al. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–471. doi: 10.1249/MSS.0b013e3181949333. https://doi.org/10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 7.Hankinson AL, Daviglus ML, Bouchard C, et al. Maintaining a high physical activity level over 20 years and weight gain. JAMA. 2010;304(23):2603–2610. doi: 10.1001/jama.2010.1843. https://doi.org/10.1001/jama.2010.1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sedentary Behavior Research Network. Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab. 2012;37(3):540–542. doi: 10.1139/h2012-024. https://doi.org/10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 9.Gibbs BB, Hergenroeder AL, Katzmarzyk PT, Lee IM, Jakicic JM. Definition, measurement, and health risks associated with sedentary behavior. Med Sci Sports Exerc. 2015;47(6):1295–1300. doi: 10.1249/MSS.0000000000000517. https://doi.org/10.1249/MSS.0000000000000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pedisic Z, Grunseit A, Ding D, et al. High sitting time or obesity: Which came first? Bidirectional association in a longitudinal study of 31,787 Australian adults. Obesity (Silver Spring) 2014;22(10):2126–2130. doi: 10.1002/oby.20817. https://doi.org/10.1002/oby.20817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ekelund U, Brage S, Besson H, Sharp S, Wareham NJ. Time spent being sedentary and weight gain in healthy adults: reverse or bidirectional causality? Am J Clin Nutr. 2008;88(3):612–617. doi: 10.1093/ajcn/88.3.612. [DOI] [PubMed] [Google Scholar]
- 12.Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am J Prev Med. 2011;41(2):207–215. doi: 10.1016/j.amepre.2011.05.004. https://doi.org/10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 13.Drenowatz C, Jakicic JM, Blair SN, Hand GA. Differences in correlates of energy balance in normal weight, overweight and obese adults. Obes Res Clin Pract. 2015;9(6):592–602. doi: 10.1016/j.orcp.2015.03.007. https://doi.org/10.1016/j.orcp.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 14.Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in U.S. adults: NHANES 2003–06. Eur Heart J. 2011;32(5):590–597. doi: 10.1093/eurheartj/ehq451. https://doi.org/10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31(2):369–371. doi: 10.2337/dc07-1795. https://doi.org/10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 16.Kim Y, Welk GJ, Braun SI, Kang M. Extracting objective estimates of sedentary behavior from accelerometer data: measurement considerations for surveillance and research applications. PLoS One. 2015;10(2):e0118078. doi: 10.1371/journal.pone.0118078. https://doi.org/10.1371/journal.pone.0118078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stamatakis E, Hamer M, Tilling K, Lawlor DA. Sedentary time in relation to cardio-metabolic risk factors: differential associations for self-report vs accelerometry in working age adults. Int J Epidemiol. 2012;41(5):1328–1337. doi: 10.1093/ije/dys077. https://doi.org/10.1093/ije/dys077. [DOI] [PubMed] [Google Scholar]
- 18.Barone Gibbs B, King WC, Davis KK, et al. Objective vs. Self-report Sedentary Behavior in Overweight and Obese Young Adults. J Phys Act Health. 2015;12(12):1551–1557. doi: 10.1123/jpah.2014-0278. https://doi.org/10.1123/jpah.2014-0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.King WC, Chen J-Y, Courcoulas AP, et al. Objectively-measured sedentary time and cardiometabolic health in adults with severe obesity. Prev Med. 2016;84:12–18. doi: 10.1016/j.ypmed.2015.12.007. https://doi.org/10.1016/j.ypmed.2015.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matthews CE, Keadle SK, Troiano RP, et al. Accelerometer-measured dose-response for physical activity, sedentary time, and mortality in U.S. adults. Am J Clin Nutr. 2016;104(5):1424–1432. doi: 10.3945/ajcn.116.135129. https://doi.org/10.3945/ajcn.116.135129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–132. doi: 10.7326/M14-1651. https://doi.org/10.7326/M14-1651. [DOI] [PubMed] [Google Scholar]
- 22.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41(11):1105–1116. doi: 10.1016/0895-4356(88)90080-7. https://doi.org/10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 23.Tudor-Locke C, Camhi SM, Troiano RP. A catalog of rules, variables, and definitions applied to accelerometer data in the National Health and Nutrition Examination Survey, 2003–2006. Prev Chronic Dis. 2012;9:110332. doi: 10.5888/pcd9.110332. https://doi.org/10.5888/pcd9.110332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Freedson P, Bowles HR, Troiano R, Haskell W. Assessment of physical activity using wearable monitors: recommendations for monitor calibration and use in the field. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S1–4. doi: 10.1249/MSS.0b013e3182399b7e. https://doi.org/10.1249/MSS.0b013e3182399b7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Physical Activity Guidelines Advisory Committee Report, 2008. Nutr Rev. 2009;67(2):114–120. doi: 10.1111/j.1753-4887.2008.00136.x. https://doi.org/10.1111/j.1753-4887.2008.00136.x. [DOI] [PubMed] [Google Scholar]
- 26.Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34(7):1481–1486. doi: 10.2337/dc10-2415. https://doi.org/10.2337/dc10-2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mcdonald A, Vanhorn L, Slattery M, et al. The Cardia Dietary History - Development, Implementation, and Evaluation. J Am Diet Assoc. 1991;91(9):1104–1112. [PubMed] [Google Scholar]
- 28.Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34(7):1481–1486. doi: 10.2337/dc10-2415. https://doi.org/10.2337/dc10-2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Buman MP, Winkler EA, Kurka JM, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am J Epidemiol. 2014;179(3):323–334. doi: 10.1093/aje/kwt292. https://doi.org/10.1093/aje/kwt292. [DOI] [PubMed] [Google Scholar]
- 30.Judice PB, Hamilton MT, Sardinha LB, Zderic TW, Silva AM. What is the metabolic and energy cost of sitting, standing and sit/stand transitions? Eur J Appl Physiol. 2016;116(2):263–273. doi: 10.1007/s00421-015-3279-5. https://doi.org/10.1007/s00421-015-3279-5. [DOI] [PubMed] [Google Scholar]
- 31.Henson J, Yates T, Biddle SJ, et al. Associations of objectively measured sedentary behaviour and physical activity with markers of cardiometabolic health. Diabetologia. 2013;56(5):1012–1020. doi: 10.1007/s00125-013-2845-9. https://doi.org/10.1007/s00125-013-2845-9. [DOI] [PubMed] [Google Scholar]
- 32.De Cocker KA, van Uffelen JG, Brown WJ. Associations between sitting time and weight in young adult Australian women. Prev Med. 2010;51(5):361–367. doi: 10.1016/j.ypmed.2010.07.009. https://doi.org/10.1016/j.ypmed.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 33.van Uffelen JG, Watson MJ, Dobson AJ, Brown WJ. Sitting time is associated with weight, but not with weight gain in mid-aged Australian women. Obesity (Silver Spring) 2010;18(9):1788–1794. doi: 10.1038/oby.2009.511. https://doi.org/10.1038/oby.2009.511. [DOI] [PubMed] [Google Scholar]
- 34.Pulsford RM, Stamatakis E, Britton AR, Brunner EJ, Hillsdon MM. Sitting behavior and obesity: evidence from the Whitehall II study. Am J Prev Med. 2013;44(2):132–138. doi: 10.1016/j.amepre.2012.10.009. https://doi.org/10.1016/j.amepre.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wijndaele K, Orrow G, Ekelund U, et al. Increasing objectively measured sedentary time increases clustered cardiometabolic risk: a 6 year analysis of the ProActive study. Diabetologia. 2014;57(2):305–312. doi: 10.1007/s00125-013-3102-y. https://doi.org/10.1007/s00125-013-3102-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee IM, Djousse L, Sesso HD, Wang L, Buring JE. Physical activity and weight gain prevention. JAMA. 2010;303(12):1173–1179. doi: 10.1001/jama.2010.312. https://doi.org/10.1001/jama.2010.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shook RP, Hand GA, Drenowatz C, et al. Low levels of physical activity are associated with dysregulation of energy intake and fat mass gain over 1 year. Am J Clin Nutr. 2015;102(6):1332–1338. doi: 10.3945/ajcn.115.115360. https://doi.org/10.3945/ajcn.115.115360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Trumbo P, Schlicker S, Yates AA, Poos M Food, Nutrition Board of the Institute of Medicine. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J Am Diet Assoc. 2002;102(11):1621–1630. doi: 10.1016/s0002-8223(02)90346-9. https://doi.org/10.1016/S0002-8223(02)90346-9. [DOI] [PubMed] [Google Scholar]
- 39.Buckley JP, Hedge A, Yates T, et al. The sedentary office: an expert statement on the growing case for change towards better health and productivity. Br J Sports Med. 2015;49:1357–1362. doi: 10.1136/bjsports-2015-094618. https://doi.org/10.1136/bjsports-2015-094618. [DOI] [PubMed] [Google Scholar]
- 40.Tremblay MS, Aubert S, Barnes JD, et al. Sedentary Behavior Research Network (SBRN) – Terminology Consensus Project process and outcome. Int J Behav Nutr Phys Act. 2017;14:75. doi: 10.1186/s12966-017-0525-8. https://doi.org/10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.